Behavioral Factors Associated with COVID-19 Risk: A Cross-Sectional Survey in Japan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient and Public Involvement
2.2. Data Collection
2.3. Statistical Analysis
2.3.1. Outcome Variables
2.3.2. Explanatory Variables
- Pre-existing diseases;
- Behaviors to avoid contracting SARS-CoV-2;
- Average days and hours of exercise in a week;
- Main exercise type;
- Change in the amount of exercise compared with the same time last year;
- Frequency of going out;
- Frequency of working from home in the past one month.
2.3.3. Comparison of the Two Groups
2.3.4. Multivariate Analysis
2.3.5. Sensitivity Analysis
2.3.6. Ethical Considerations
3. Results
3.1. Background of the Responders
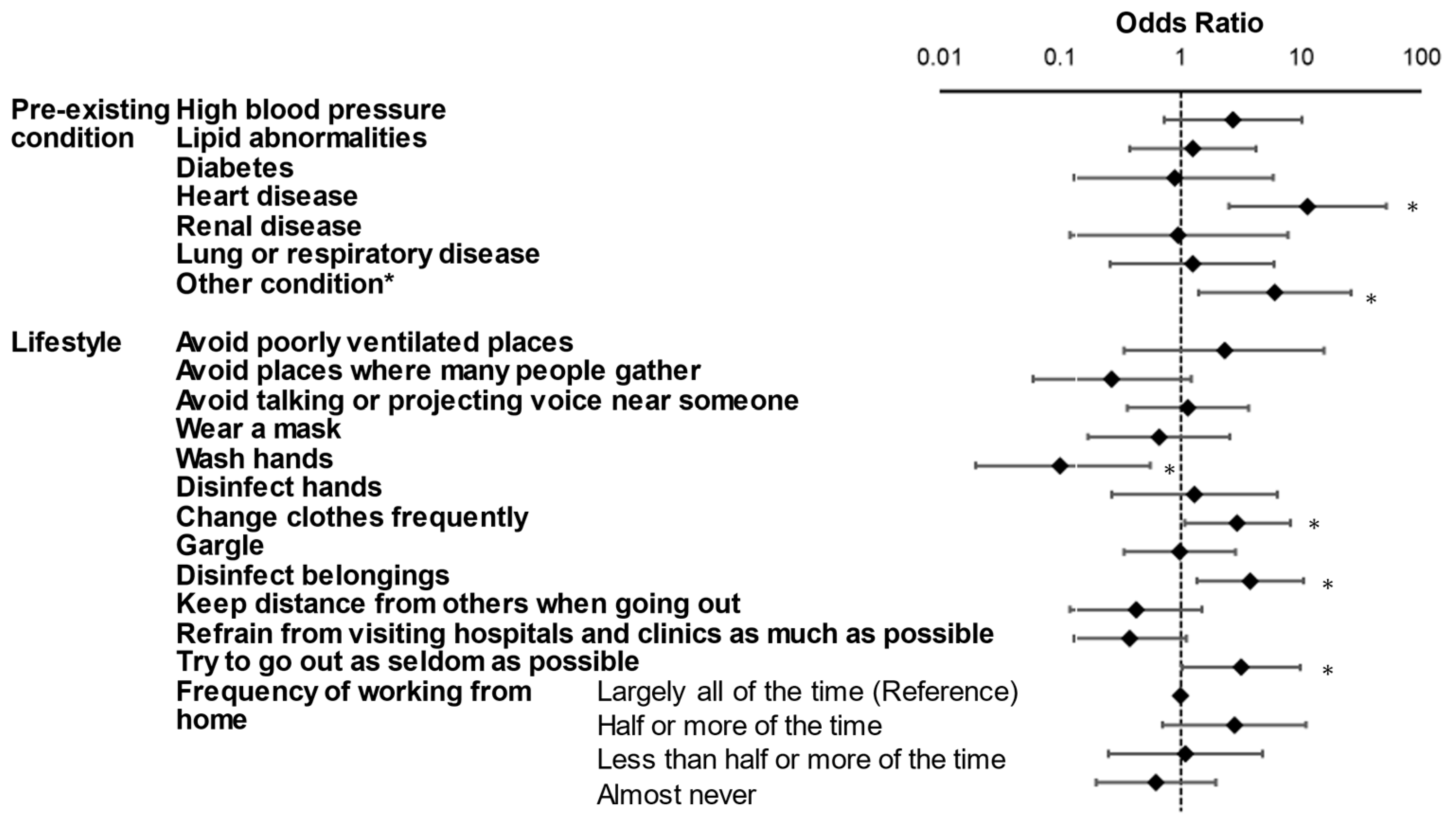
3.2. Multivariate Logistic Regression Analysis
3.3. Analysis Using Inverse Probability Weighting Method
3.4. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- CDC. The Possibility of COVID-19 after Vaccination: Breakthrough Infections. 9 November 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/effectiveness/why-measure-effectiveness/breakthrough-cases.html (accessed on 13 November 2021).
- Godlee, F. Covid-19: Vaccine woes highlight vital role of traditional public health. BMJ 2021, 373, n968. [Google Scholar] [CrossRef]
- Ganesan, B.; Al-Jumaily, A.; Fong, K.N.K.; Prasad, P.; Meena, S.K.; Tong, R.K. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak Quarantine, Isolation, and Lockdown Policies on Mental Health and Suicide. Front. Psychiatry 2021, 12, 565190. [Google Scholar] [CrossRef] [PubMed]
- Mulugeta, T.; Tadesse, E.; Shegute, T.; Desta, T.T. COVID-19: Socio-economic impacts and challenges in the working group. Heliyon 2021, 7, e07307. [Google Scholar] [CrossRef] [PubMed]
- Kithiia, J.; Wanyonyi, I.; Maina, J.; Jefwa, T.; Gamoyo, M. The socio-economic impacts of Covid-19 restrictions: Data from the coastal city of Mombasa, Kenya. Data Brief 2020, 33, 106317. [Google Scholar] [CrossRef] [PubMed]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Abdo, C.; Miranda, E.P.; Santos, C.S.; Junior, J.B.; Bernardo, W.M. Domestic violence and substance abuse during COVID19: A systematic review. Indian J. Psychiatry 2020, 62, S337–S342. [Google Scholar] [CrossRef] [PubMed]
- Wingfield-Hayes, R. Covid and Suicide: Japan’s Rise a Warning to the World? BBC News. 18 February 2021. Available online: https://www.bbc.com/news/world-asia-55837160 (accessed on 13 November 2021).
- Stuckler, D.; Reeves, A.; Loopstra, R.; Karanikolos, M.; McKee, M. Austerity and health: The impact in the UK and Europe. Eur. J. Public Health 2017, 27, 18–21. [Google Scholar] [CrossRef] [PubMed]
- WHO. Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions. 9 July 2020. Available online: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions (accessed on 13 November 2021).
- Zhou, L.; Ayeh, S.K.; Chidambaram, V.; Karakousis, P.C. Modes of transmission of SARS-CoV-2 and evidence for preventive behavioral interventions. BMC Infect. Dis. 2021, 21, 496. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, N.; Saito, E.; Kondo, N.; Inoue, M.; Ikeda, S.; Satoh, T.; Wada, K.; Stickley, A.; Katanoda, K.; Mizoue, T.; et al. What has made the population of Japan healthy? Lancet 2011, 378, 1094–1105. [Google Scholar] [CrossRef]
- Alfano, V.; Ercolano, S. The Efficacy of Lockdown Against COVID-19: A Cross-Country Panel Analysis. Appl. Health Econ. Health Policy 2020, 18, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Lau, H.; Khosrawipour, V.; Kocbach, P.; Mikolajczyk, A.; Schubert, J.; Bania, J.; Khosrawipour, T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Travel. Med. 2020, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harvey, A.P.; Fuhrmeister, E.R.; Cantrell, M.E.; Pitol, A.K.; Swarthout, J.M.; Powers, J.E.; Nadimpalli, M.L.; Julian, T.R.; Pickering, A.J. Longitudinal Monitoring of SARS-CoV-2 RNA on High-Touch Surfaces in a Community Setting. Environ. Sci. Technol. Lett. 2021, 8, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Li, F.; Fortunati, F.; Krystal, J.H. Association of a Prior Psychiatric Diagnosis with Mortality among Hospitalized Patients with Coronavirus Disease 2019 (COVID-19) Infection. JAMA Netw. Open 2020, 3, e2023282. [Google Scholar] [CrossRef] [PubMed]
- Haas, P.M. Introduction: Epistemic communities and international policy coordination. Int. Organ. 2009, 46, 1–35. [Google Scholar] [CrossRef] [Green Version]
- Eyles, J.; Robinson, K.; Elliott, S. An epistemic community comes and goes? Local and national expressions of heart health promotion in Canada. BMC Health Serv. Res. 2009, 9, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lebel, U. The immunized integration of Religious-Zionists within Israeli society: The pre-military academy as an institutional model. Soc. Identities 2016, 22, 642–660. [Google Scholar] [CrossRef]
| Variables | Categories | SARS-CoV-2 Group (N = 44) | Control Group (N = 13,277) | p | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Age group | 18–19 | 2 | 4.5 | 297 | 2.2 | <0.01 |
| 20–29 | 12 | 27.3 | 1270 | 9.6 | ||
| 30–39 | 8 | 18.2 | 1479 | 11.1 | ||
| 40–49 | 10 | 22.7 | 2698 | 20.3 | ||
| 50–59 | 7 | 15.9 | 2863 | 21.6 | ||
| 60–69 | 3 | 6.8 | 3076 | 23.2 | ||
| 70–74 | 2 | 4.5 | 1594 | 12.0 | ||
| Gender | Female | 16 | 36.4 | 6566 | 49.5 | 0.09 |
| Male | 28 | 63.6 | 6711 | 50.5 | ||
| BMI | <18.5 | 3 | 6.8 | 1736 | 13.1 | 0.39 |
| 18.5–25 | 31 | 70.5 | 9044 | 68.1 | ||
| 25–30 | 9 | 20.5 | 2097 | 15.8 | ||
| ≥30 | 1 | 2.3 | 400 | 3.0 | ||
| Pre-existing condition | High blood pressure | 11 | 25.0 | 2179 | 16.4 | 0.13 |
| Lipid abnormalities | 5 | 11.4 | 1242 | 9.4 | 0.65 | |
| Diabetes | 5 | 11.4 | 671 | 5.1 | 0.06 | |
| Heart disease | 5 | 11.4 | 299 | 2.3 | <0.01 | |
| Renal disease | 1 | 2.3 | 102 | 0.8 | 0.26 | |
| Cancer | 1 | 2.3 | 201 | 1.5 | 0.68 | |
| Lung or respiratory disease | 1 | 2.3 | 299 | 2.3 | 0.99 | |
| Other condition * | 2 | 4.5 | 184 | 1.4 | 0.08 | |
| Lifestyle | Avoid poorly ventilated places | 36 | 81.8 | 11,348 | 85.5 | 0.49 |
| Avoid places where many people gather | 29 | 65.9 | 11,570 | 87.1 | <0.01 | |
| Avoid talking or projecting voice near someone | 31 | 70.5 | 10,664 | 80.3 | 0.10 | |
| Wear a mask | 37 | 84.1 | 12,915 | 97.3 | <0.01 | |
| Wash hands | 34 | 77.3 | 12,808 | 96.5 | <0.01 | |
| Disinfect hands | 36 | 81.8 | 11,848 | 89.2 | 0.11 | |
| Change clothes frequently | 22 | 50.0 | 2820 | 21.2 | <0.01 | |
| Gargle | 28 | 63.6 | 9122 | 68.7 | 0.47 | |
| Disinfect belongings | 24 | 54.5 | 3743 | 28.2 | <0.01 | |
| Keep distance from others when going out | 30 | 68.2 | 10,937 | 82.4 | 0.01 | |
| Refrain from visiting hospitals and clinics as much as possible | 22 | 50.0 | 6572 | 49.5 | 0.59 | |
| Try to go out as seldom as possible | 30 | 68.2 | 8082 | 60.9 | 0.32 | |
| Frequency of working from home | Largely all of the time | 6 | 13.6 | 900 | 6.8 | <0.01 |
| Half or more of the time | 5 | 11.4 | 359 | 2.7 | ||
| Less than half or more of the time | 3 | 6.8 | 533 | 4.0 | ||
| Almost never | 18 | 40.9 | 5952 | 44.8 | ||
| Variables | Multiple Regression | IPW | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | p | ATE (%change) | 95%CI | p | |||
| Age | 0.94 | 0.91 | 0.98 | <0.01 | N.A. | |||
| Male gender | 0.96 | 0.87 | 1.06 | 0.47 | ||||
| BMI | 0.91 | 0.43 | 1.92 | 0.81 | ||||
| Pre-existing condition | ||||||||
| High blood pressure | 2.72 | 0.73 | 10.15 | 0.14 | 195.0 | −78.7 | 468.6 | 0.16 |
| Lipid abnormalities | 1.27 | 0.38 | 4.25 | 0.69 | 107.2 | −118.3 | 332.7 | 0.35 |
| Diabetes | 0.89 | 0.13 | 5.86 | 0.90 | 194.8 | −107.6 | 497.2 | 0.21 |
| Heart disease | 11.33 | 2.50 | 51.25 | <0.01 | 2704.4 | −918.2 | 6327.0 | 0.14 |
| Renal disease | 0.95 | 0.12 | 7.78 | 0.96 | 912.9 | −964.4 | 2790.2 | 0.34 |
| Lung or respiratory disease | 1.26 | 0.26 | 5.99 | 0.77 | −62.1 | −140.8 | 16.5 | 0.12 |
| Other condition * | 6.03 | 1.41 | 25.77 | 0.02 | 152.4 | −336.5 | 641.3 | 0.54 |
| Lifestyle | ||||||||
| Avoid poorly ventilated places | 2.31 | 0.34 | 15.56 | 0.39 | 443.6 | −324.1 | 1211.2 | 0.26 |
| Avoid places where many people gather | 0.27 | 0.06 | 1.22 | 0.09 | −62.2 | −115.6 | −8.7 | 0.02 |
| Avoid talking or projecting voice near someone | 1.15 | 0.36 | 3.67 | 0.81 | −19.0 | −81.0 | 43.1 | 0.55 |
| Wear a mask | 0.66 | 0.17 | 2.55 | 0.54 | −86.4 | −175.4 | 2.6 | 0.06 |
| Wash hands | 0.10 | 0.02 | 0.56 | 0.01 | −84.8 | −155.8 | −13.7 | 0.02 |
| Disinfect hands | 1.30 | 0.27 | 6.38 | 0.74 | −44.0 | −117.8 | 29.9 | 0.24 |
| Change clothes frequently | 2.96 | 1.08 | 8.15 | 0.04 | 274.4 | 113.2 | 435.6 | <0.01 |
| Gargle | 0.98 | 0.34 | 2.85 | 0.97 | −16.3 | −74.3 | 41.7 | 0.58 |
| Disinfect belongings | 3.78 | 1.37 | 10.44 | 0.01 | 100.0 | 55.9 | 144.1 | <0.01 |
| Keep distance from others when going out | 0.43 | 0.12 | 1.51 | 0.19 | −43.8 | −102.4 | 14.8 | 0.14 |
| Refrain from visiting hospitals and clinics as much as possible | 0.38 | 0.13 | 1.12 | 0.08 | 2.1 | −59.5 | 63.7 | 0.95 |
| Try to go out as seldom as possible | 3.20 | 1.03 | 9.88 | 0.04 | 45.2 | −28.6 | 119.0 | 0.23 |
| Frequency of working from home | ||||||||
| Largely all of the time | 1 (Reference) | 0 (Reference) | ||||||
| Half or more of the time | 2.79 | 0.71 | 10.97 | 0.14 | 15.1 | −96.8 | 1.8 | 0.79 |
| Less than half or more of the time | 1.09 | 0.25 | 4.78 | 0.91 | −67.8 | −142.6 | 0.1 | 0.08 |
| Almost never | 0.62 | 0.20 | 1.97 | 0.42 | −77.1 | −143.4 | −0.2 | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ochi, S.; So, M.; Hashimoto, S.; Denda, K.; Sekizawa, Y. Behavioral Factors Associated with COVID-19 Risk: A Cross-Sectional Survey in Japan. Int. J. Environ. Res. Public Health 2021, 18, 12184. https://doi.org/10.3390/ijerph182212184
Ochi S, So M, Hashimoto S, Denda K, Sekizawa Y. Behavioral Factors Associated with COVID-19 Risk: A Cross-Sectional Survey in Japan. International Journal of Environmental Research and Public Health. 2021; 18(22):12184. https://doi.org/10.3390/ijerph182212184
Chicago/Turabian StyleOchi, Sae, Mirai So, Sora Hashimoto, Kenzo Denda, and Yoichi Sekizawa. 2021. "Behavioral Factors Associated with COVID-19 Risk: A Cross-Sectional Survey in Japan" International Journal of Environmental Research and Public Health 18, no. 22: 12184. https://doi.org/10.3390/ijerph182212184
APA StyleOchi, S., So, M., Hashimoto, S., Denda, K., & Sekizawa, Y. (2021). Behavioral Factors Associated with COVID-19 Risk: A Cross-Sectional Survey in Japan. International Journal of Environmental Research and Public Health, 18(22), 12184. https://doi.org/10.3390/ijerph182212184






