Refugee Children’s Social–Emotional Capacities: Links to Mental Health upon Resettlement and Buffering Effects on Pre-Migratory Adversity
Abstract
:1. Introduction
1.1. Multiple Levels of Adversity: Child, Parental, and Familial
1.2. Mental Health in Refugee Children: Internalizing and Externalizing Symptoms
1.3. Social–Emotional Capacities as Potential Sources of Protection Amidst Adversity
1.4. The Current Study
2. Materials and Methods
2.1. Study Participants
2.2. Procedure
2.3. Measures
2.3.1. Child, Parental, and Familial Pre-Migratory Adversities
2.3.2. Child Social–Emotional Capacities
2.3.3. Child Mental Health
2.4. Data Analytic Plan
3. Results
3.1. Descriptive Statistics
3.2. Regression Models Predicting Child Internalizing and Externalizing Symptoms
4. Discussion
4.1. Main Effects of Child, Parental, and Familial Pre-Migratory Adversities on Refugee Children’s Mental Health
4.2. Main Effects of Child Social–Emotional Capacities on Child Internalizing and Externalizing Symptoms
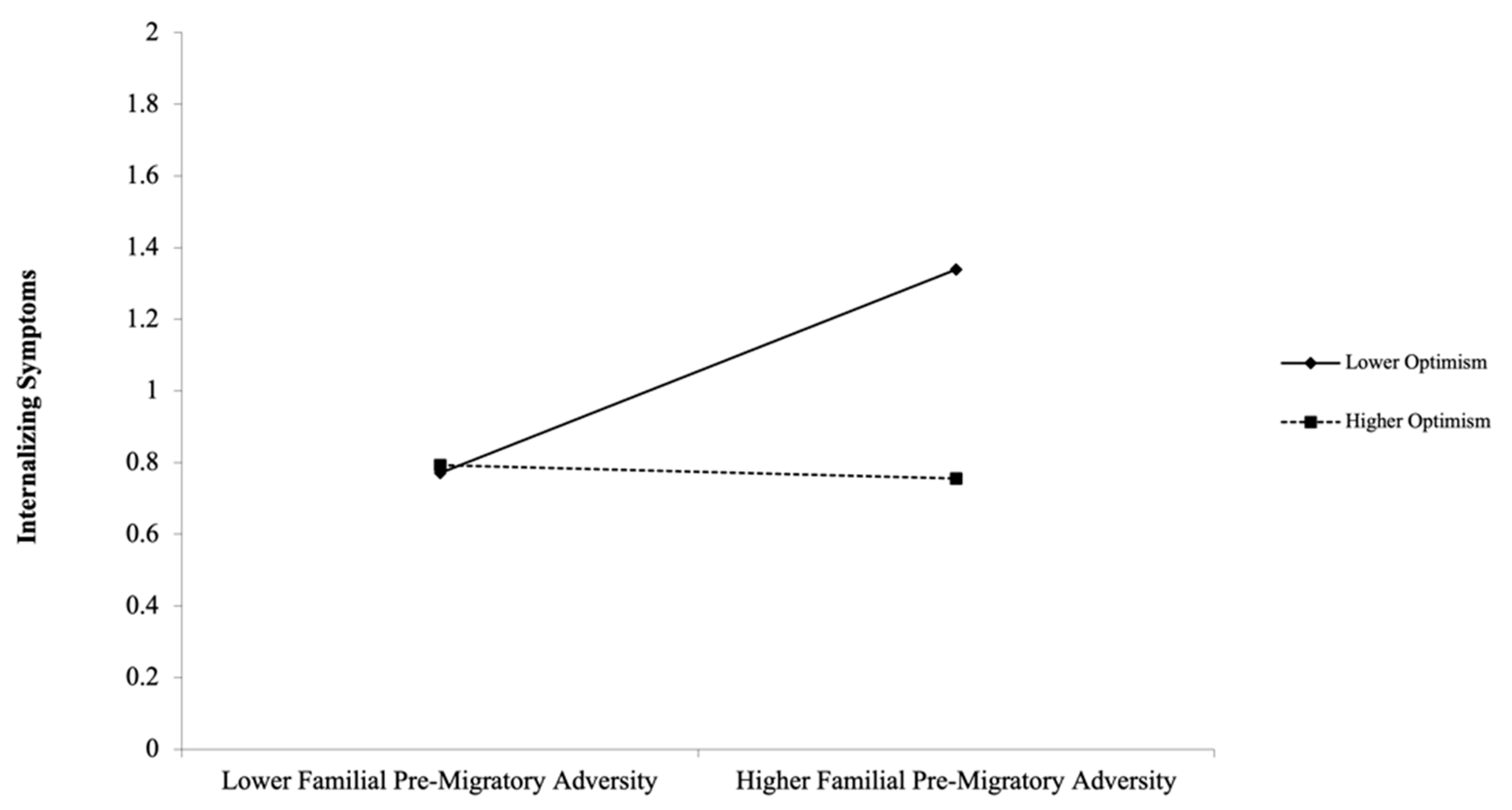
4.3. Moderating Effects of Child Social–Emotional Capacities
4.4. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations High Commissioner for Refugees [UNHCR]. Global Trends in Forced Displacement in 2020. 2021. Available online: https://www.unhcr.org/refugee-statistics/ (accessed on 15 September 2021).
- Flanagan, N.; Travers, A.; Vallières, F.; Hansen, M.; Halpin, R.; Sheaf, G.; Rottmann, N.; Johnsen, A.T. Crossing borders: A systematic review identifying potential mechanisms of intergenerational trauma transmission in asylum-seeking and refugee families. Eur. J. Psychotraumatol. 2020, 11, 1790283. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S. Resilience Theory and Research on Children and Families: Past, Present, and Promise. J. Fam. Theory Rev. 2018, 10, 12–31. [Google Scholar] [CrossRef] [Green Version]
- Fritz, J.; de Graaff, A.M.; Caisley, H.; van Harmelen, A.-L.; Wilkinson, P.O. A Systematic Review of Amenable Resilience Factors That Moderate and/or Mediate the Relationship Between Childhood Adversity and Mental Health in Young People. Front. Psychiatry 2018, 9, 230. [Google Scholar] [CrossRef] [Green Version]
- Yule, K.; Houston, J.; Grych, J. Resilience in Children Exposed to Violence: A Meta-analysis of Protective Factors across Ecological Contexts. Clin. Child Fam. Psychol. Rev. 2019, 22, 406–431. [Google Scholar] [CrossRef] [PubMed]
- Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design; Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
- Miller, K.E.; Rasco, L.M. An Ecological Framework for Addressing the Mental Health Needs of Refugee Communities. In The Mental Health of Refugees: Ecological Approaches to Healing and Adaptation; Miller, K.E., Rasc, L.M., Eds.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2004. [Google Scholar]
- East, P.L.; Gahagan, S.; Al-Delaimy, W. The Impact of Refugee Mothers’ Trauma, Posttraumatic Stress, and Depression on Their Children’s Adjustment. J. Immigr. Minor. Health 2017, 20, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Eltanamly, H.; Leijten, P.; Jak, S.; Overbeek, G. Parenting in Times of War: A Meta-Analysis and Qualitative Synthesis of War Exposure, Parenting, and Child Adjustment. Trauma Violence Abus. 2019, 22, 147–160. [Google Scholar] [CrossRef]
- Nielsen, M.B.; Carlsson, J.; Rimvall, M.K.; Petersen, J.H.; Norredam, M. Risk of childhood psychiatric disorders in children of refugee parents with post-traumatic stress disorder: A nationwide, register-based, cohort study. Lancet Public Health 2019, 4, e353–e359. [Google Scholar] [CrossRef] [Green Version]
- Chan, K.J.; Young, M.Y.; Sharif, N. Well-being after trauma: A review of posttraumatic growth among refugees. Can. Psychol. 2016, 57, 291–299. [Google Scholar] [CrossRef]
- Atzaba-Poria, N.; Pike, A.; Deater-Deckard, K. Do risk factors for problem behaviour act in a cumulative manner? An examination of ethnic minority and majority children through an ecological perspective. J. Child Psychol. Psychiatry 2004, 45, 707–718. [Google Scholar] [CrossRef]
- DeVries, J.M.; Gebhardt, M.; Voß, S. An assessment of measurement invariance in the 3- and 5-factor models of the Strengths and Difficulties Questionnaire: New insights from a longitudinal study. Personal. Individ. Differ. 2017, 119, 1–6. [Google Scholar] [CrossRef]
- Nelson, C.A.; Gabard-Durnam, L.J. Early Adversity and Critical Periods: Neurodevelopmental Consequences of Violating the Expectable Environment. Trends Neurosci. 2020, 43, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Blackmore, R.; Gray, K.M.; Boyle, J.A.; Fazel, M.; Ranasinha, S.; Fitzgerald, G.; Misso, M.; Gibson-Helm, M. Systematic Review and Meta-analysis: The Prevalence of Mental Illness in Child and Adolescent Refugees and Asylum Seekers. J. Am. Acad. Child Adolesc. Psychiatry 2019, 59, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Scoglio, A.A.J.; Salhi, C. Violence Exposure and Mental Health Among Resettled Refugees: A Systematic Review. Trauma Violence Abus. 2020. [Google Scholar] [CrossRef]
- Alsayed, A.; Wildes, V.J. Syrian Refugee Children: A Study of Strengths and Difficulties. J. Hum. Rights Soc. Work. 2018, 3, 81–88. [Google Scholar] [CrossRef]
- Morton, B.; Feng, H. Mental Health Effects of Premigration Trauma and Postmigration Discrimination on Refugee Youth in Canada. J. Nerv. Ment. Dis. 2016, 204, 464–470. [Google Scholar] [CrossRef]
- Mels, C.; Derluyn, I.; Broekaert, E.; Rosseel, Y. The psychological impact of forced displacement and related risk factors on Eastern Congolese adolescents affected by war. J. Child Psychol. Psychiatry 2010, 51, 1096–1104. [Google Scholar] [CrossRef]
- Vervliet, M.; Lammertyn, J.; Broekaert, E.; Derluyn, I. Longitudinal follow-up of the mental health of unaccompanied refugee minors. Eur. Child Adolesc. Psychiatry 2013, 23, 337–346. [Google Scholar] [CrossRef]
- Sapmaz, S.Y.; Tanrıverdi, B.U.; Öztürk, M.; Ülker, G.Y.; Özkan, Y. Immigration-related mental health disorders in refugees 5–18 years old living in Turkey. Neuropsychiatr. Dis. Treat. 2017, 13, 2813–2821. [Google Scholar] [CrossRef] [Green Version]
- Jensen, T.K.; Fjermestad, K.W.; Granly, L.; Wilhelmsen, N.H. Stressful life experiences and mental health problems among unaccompanied asylum-seeking children. Clin. Child Psychol. Psychiatry 2013, 20, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Rousseau, C.; Drapeau, A.; Rahimi, S. The complexity of trauma response: A 4-year follow-up of adolescent Cambodian refugees. Child Abus. Negl. 2003, 27, 1277–1290. [Google Scholar] [CrossRef]
- Bean, T.; Derluyn, I.; Eurelings-Bontekoe, E.; Broekaert, E.; Spinhoven, P. Comparing Psychological Distress, Traumatic Stress Reactions, and Experiences of Unaccompanied Refugee Minors with Experiences of Adolescents Accompanied by Parents. J. Nerv. Ment. Dis. 2007, 195, 288–297. [Google Scholar] [CrossRef]
- Lau, W.; Silove, D.; Edwards, B.; Forbes, D.; Bryant, R.; McFarlane, A.; Hadzi-Pavlovic, D.; Steel, Z.; Nickerson, A.; Van Hooff, M.; et al. Adjustment of refugee children and adolescents in Australia: Outcomes from wave three of the Building a New Life in Australia study. BMC Med. 2018, 16, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Hovil, L.; Gill, M.; Genovese, I.; Bueno, O.; Kaplan, J.; Subrahmanian, R. Reimagining Migration Responses: Learning from Children and Young People Who Move in the Horn of Africa; UNICEF Office of Research-Innocenti: Florence, Italy, 2021. [Google Scholar]
- Marley, C.; Mauki, B. Resilience and protective factors among refugee children post-migration to high-income countries: A systematic review. Eur. J. Public Health 2018, 29, 706–713. [Google Scholar] [CrossRef]
- Malti, T. Children and Violence: Nurturing Social-Emotional Development to Promote Mental Health. Soc. Policy Rep. 2020, 33, 1–27. [Google Scholar] [CrossRef]
- Malti, T.; Sette, S.; Dys, S.P. Social-Emotional Responding: A Perspective from Developmental Psychology. In Emerging Trends in the Social and Behavioral Sciences: An Interdisciplinary, Searchable, and Linkable Resource; 2015; pp. 1–15. [Google Scholar] [CrossRef]
- Robson, D.A.; Allen, M.S.; Howard, S.J. Self-regulation in childhood as a predictor of future outcomes: A meta-analytic review. Psychol. Bull. 2020, 146, 324–354. [Google Scholar] [CrossRef] [Green Version]
- Malti, T.; Krettenauer, T. The Relation of Moral Emotion Attributions to Prosocial and Antisocial Behavior: A Metaanalysis. Child Dev. 2013, 84, 397–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Awad, U.; Fathi, A.; Petermann, F.; Reinelt, T. Promoting Mental Health in Unaccompanied Refugee Minors: Recommendations for Primary Support Programs. Brain Sci. 2017, 7, 146. [Google Scholar] [CrossRef] [Green Version]
- Lee, F. Cultivating a Culture of Peace and Empathy in Young Children While Empowering Refugee Communities. Child. Educ. 2019, 95, 16–23. [Google Scholar] [CrossRef]
- Eisenberg, N.; Spinrad, T.L. Emotion-Related Regulation: Sharpening the Definition. Child Dev. 2004, 75, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.A. Emotion Regulation: A Theme in Search of Definition. Monogr. Soc. Res. Child Dev. 1994, 59, 25–52. [Google Scholar] [CrossRef]
- Compas, B.E.; Jaser, S.S.; Bettis, A.H.; Watson, K.H.; Gruhn, M.A.; Dunbar, J.P.; Williams, E.; Thigpen, J.C. Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychol. Bull. 2017, 143, 939–991. [Google Scholar] [CrossRef] [PubMed]
- Amone-P’Olak, K.; Garnefski, N.; Kraaij, V. Adolescents caught between fires: Cognitive emotion regulation in response to war experiences in Northern Uganda. J. Adolesc. 2007, 30, 655–669. [Google Scholar] [CrossRef]
- Lee, M.; Lee, E.-S.; Jun, J.Y.; Park, S. The effect of early trauma on North Korean refugee youths’ mental health: Moderating effect of emotional regulation strategies. Psychiatry Res. 2019, 287, 112707. [Google Scholar] [CrossRef]
- Flouri, E.; Mavroveli, S. Adverse Life Events and Emotional and Behavioural Problems in Adolescence: The Role of Coping and Emotion Regulation. Stress Health 2012, 29, 360–368. [Google Scholar] [CrossRef]
- Eisenberg, N. Emotion, Regulation, and Moral Development. Annu. Rev. Psychol. 2000, 51, 665–697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eisenberg, N.; Eggum-Wilkens, N.; Di Giunta, L. Empathy-Related Responding: Associations with Prosocial Behavior, Aggression, and Intergroup Relations. Soc. Issues Policy Rev. 2010, 4, 143–180. [Google Scholar] [CrossRef]
- Zuffianò, A.; Colasante, T.; Buchmann, M.; Malti, T. The codevelopment of sympathy and overt aggression from middle childhood to early adolescence. Dev. Psychol. 2018, 54, 98–110. [Google Scholar] [CrossRef] [Green Version]
- Dagan, Y.; Yager, J. Posttraumatic Growth in Complex PTSD. Psychiatry 2019, 82, 329–344. [Google Scholar] [CrossRef]
- Staub, E.; Vollhardt, J. Altruism born of suffering: The roots of caring and helping after victimization and other trauma. Am. J. Orthopsychiatry 2008, 78, 267–280. [Google Scholar] [CrossRef] [PubMed]
- Hartman, A.C.; Morse, B.S. Violence, Empathy and Altruism: Evidence from the Ivorian Refugee Crisis in Liberia. Br. J. Polit. Sci. 2018, 50, 731–755. [Google Scholar] [CrossRef] [Green Version]
- Taylor, L.K.; Hanna, J.R. Altruism born of suffering among emerging adults in Northern Ireland. J. Aggress. Confl. Peace Res. 2017, 10, 157–169. [Google Scholar] [CrossRef] [Green Version]
- Vollhardt, J.R.; Staub, E. Inclusive altruism born of suffering: The relationship between adversity and prosocial attitudes and behavior toward disadvantaged outgroups. Am. J. Orthopsychiatry 2011, 81, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Scheier, M.F. Dispositional optimism. Trends Cogn. Sci. 2014, 18, 293–299. [Google Scholar] [CrossRef] [Green Version]
- Nes, L.S.; Segerstrom, S. Dispositional Optimism and Coping: A Meta-Analytic Review. Pers. Soc. Psychol. Rev. 2006, 10, 235–251. [Google Scholar] [CrossRef]
- Pieloch, K.A.; McCullough, M.B.; Marks, A.K. Resilience of children with refugee statuses: A research review. Can. Psychol. 2016, 57, 330–339. [Google Scholar] [CrossRef]
- Sleijpen, M.; Haagen, J.; Mooren, T.; Kleber, R.J. Growing from experience: An exploratory study of posttraumatic growth in adolescent refugees. Eur. J. Psychotraumatol. 2016, 7, 28698. [Google Scholar] [CrossRef]
- Mahamid, F.; Berte, D.Z. Happiness, Sadness, and Hope for the Future in Narratives of Palestinian Refugee Children. Int. J. Ment. Health Addict. 2020, 18, 1638–1651. [Google Scholar] [CrossRef]
- Mohamed, S.; Thomas, M. The mental health and psychological well-being of refugee children and young people: An exploration of risk, resilience and protective factors. Educ. Psychol. Pract. 2017, 33, 249–263. [Google Scholar] [CrossRef]
- Veronese, G.; Castiglioni, M.; Tombolani, M.; Said, M. ‘My happiness is the refugee camp, my future Palestine’: Optimism, life satisfaction and perceived happiness in a group of Palestinian children. Scand. J. Caring Sci. 2011, 26, 467–473. [Google Scholar] [CrossRef]
- Yamagishi, T. Trust as Social Intelligence. In Trust. The Science of the Mind; Springer: Tokyo, Japan, 2011; pp. 107–131. [Google Scholar] [CrossRef]
- Grütter, J.; Gasser, L.; Zuffiano, A.; Meyer, B. Promoting Inclusion via Cross-Group Friendship: The Mediating Role of Change in Trust and Sympathy. Child Dev. 2017, 89, e414–e430. [Google Scholar] [CrossRef]
- Malti, T.; Averdijk, M.; Zuffiano, A.; Ribeaud, D.; Betts, L.R.; Rotenberg, K.J.; Eisner, M.P. Children’s trust and the development of prosocial behavior. Int. J. Behav. Dev. 2015, 40, 262–270. [Google Scholar] [CrossRef] [Green Version]
- Song, J.-H.; Colasante, T.; Malti, T. Helping yourself helps others: Linking children’s emotion regulation to prosocial behavior through sympathy and trust. Emotion 2018, 18, 518–527. [Google Scholar] [CrossRef] [PubMed]
- Lindert, J.; Schinina, G. Mental health of refugees and asylum-seekers. In Migration and Health in the European Union; Bernd, R., Mladovsky, P., Deville, W., Rijks, B., Petrova-Bendict, R., Eds.; McGraw-Hill, Open University Press: Maidenhead, UK, 2011; pp. 169–181. [Google Scholar]
- Betancourt, T.S.; Newnham, E.A.; Layne, C.M.; Kim, S.; Steinberg, A.M.; Ellis, H.; Birman, D. Trauma History and Psychopathology in War-Affected Refugee Children Referred for Trauma-Related Mental Health Services in the United States. J. Trauma. Stress 2012, 25, 682–690. [Google Scholar] [CrossRef]
- Eide, K.; Lidén, H.; Haugland, B.; Fladstad, T.; Hauge, H.A. Trajectories of ambivalence and trust: Experiences of unaccompanied refugee minors resettling in Norway. Eur. J. Soc. Work 2018, 23, 554–565. [Google Scholar] [CrossRef]
- Majumder, P.; O’Reilly, M.; Karim, K.; Vostanis, P. ‘This doctor, I not trust him, I’m not safe’: The perceptions of mental health and services by unaccompanied refugee adolescents. Int. J. Soc. Psychiatry 2014, 61, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Nickerson, A.; Liddell, B.J.; Keegan, D.; Edwards, B.; Felmingham, K.L.; Forbes, D.; Hadzi-Pavlovic, D.; McFarlane, A.C.; O’Donnell, M.; Silove, D.; et al. Longitudinal association between trust, psychological symptoms and community engagement in resettled refugees. Psychol. Med. 2018, 49, 1661–1669. [Google Scholar] [CrossRef] [Green Version]
- Rutter, M. Resilience as a dynamic concept. Dev. Psychopathol. 2012, 24, 335–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bontempo, R. Translation Fidelity of Psychological Scales. J. Cross-Cult. Psychol. 1993, 24, 149–166. [Google Scholar] [CrossRef]
- Bean, T.; Derluyn, I.; Eurelings-Bontekoe, E.; Broekaert, E.; Spinhoven, P. Validation of the multiple language versions of the Reactions of Adolescents to Traumatic Stress questionnaire. J. Trauma. Stress 2006, 19, 241–255. [Google Scholar] [CrossRef] [PubMed]
- Holmes, T.H.; Rahe, R.H. The social readjustment rating scale. Psychosomatics 1967, 11, 213–218. [Google Scholar] [CrossRef]
- Malti, T.; Zuffiano, A.; Noam, G.G. Knowing Every Child: Validation of the Holistic Student Assessment (HSA) as a Measure of Social-Emotional Development. Prev. Sci. 2017, 19, 306–317. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. The Strengths and Difficulties Questionnaire: A Research Note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Goodman, A.; Lamping, D.L.; Ploubidis, G.B. When to Use Broader Internalising and Externalising Subscales Instead of the Hypothesised Five Subscales on the Strengths and Difficulties Questionnaire (SDQ): Data from British Parents, Teachers and Children. J. Abnorm. Child Psychol. 2010, 38, 1179–1191. [Google Scholar] [CrossRef] [PubMed]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- Arakelyan, S.; Ager, A. Annual Research Review: A multilevel bioecological analysis of factors influencing the mental health and psychosocial well-being of refugee children. J. Child Psychol. Psychiatry 2020, 62, 484–509. [Google Scholar] [CrossRef] [PubMed]
- Scharpf, F.; Kaltenbach, E.; Nickerson, A.; Hecker, T. A systematic review of socio-ecological factors contributing to risk and protection of the mental health of refugee children and adolescents. Clin. Psychol. Rev. 2020, 83, 101930. [Google Scholar] [CrossRef]
- Domitrovich, C.E.; Durlak, J.A.; Staley, K.C.; Weissberg, R.P. Social-Emotional Competence: An Essential Factor for Promoting Positive Adjustment and Reducing Risk in School Children. Child Dev. 2017, 88, 408–416. [Google Scholar] [CrossRef]
- Malti, T.; Cheah, S.L. Towards Complementarity: Specificity and Commonality in Social-Emotional Development. Child Dev. 2021, 92, e1085–e1094. [Google Scholar] [CrossRef]
- Blewitt, C.; Fuller-Tyszkiewicz, M.; Nolan, A.; Bergmeier, H.; Vicary, D.; Huang, T.; McCabe, P.; McKay, T.; Skouteris, H. Social and Emotional Learning Associated with Universal Curriculum-Based Interventions in Early Childhood Education and Care Centers. JAMA Netw. Open 2018, 1, e185727. [Google Scholar] [CrossRef] [Green Version]
- Gillham, J.; Reivich, K. Cultivating Optimism in Childhood and Adolescence. Ann. Am. Acad. Polit. Soc. Sci. 2004, 591, 146–163. [Google Scholar] [CrossRef]
- Rotenberg, K.J.; Boulton, M.J.; Fox, C.L. Cross-Sectional and Longitudinal Relations Among Children’s Trust Beliefs, Psychological Maladjustment and Social Relationships: Are Very High as Well as Very Low Trusting Children at Risk? J. Abnorm. Child Psychol. 2005, 33, 595–610. [Google Scholar] [CrossRef]
- Rotenberg, K.J. The Psychology of Interpersonal Trust: Theory and Research; Routledge: London, UK, 2019. [Google Scholar] [CrossRef]
- Rotenberg, K.J.; Qualter, P.; Holt, N.L.; Harris, R.A.; Henzi, P.; Barrett, L. When Trust Fails: The Relation between Children’s Trust Beliefs in Peers and their Peer Interactions in a Natural Setting. J. Abnorm. Child Psychol. 2014, 42, 967–980. [Google Scholar] [CrossRef] [PubMed]
- Foka, S.; Hadfield, K.; Pluess, M.; Mareschal, I. Promoting well-being in refugee children: An exploratory controlled trial of a positive psychology intervention delivered in Greek refugee camps. Dev. Psychopathol. 2020, 33, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Reivich, K.; Gillham, J.E.; Chaplin, T.M.; Seligman, M.E.P. From Helplessness to Optimism: The Role of Resilience in Treating and Preventing Depression in Youth. In Handbook of Resilience in Children; Springer: Boston, MA, USA, 2013; pp. 201–214. [Google Scholar] [CrossRef]
- Zeman, J.; Shipman, K.; Suveg, C. Anger and Sadness Regulation: Predictions to Internalizing and Externalizing Symptoms in Children. J. Clin. Child Adolesc. Psychol. 2002, 31, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Immigration, Refugees and Citizenship Canada (IRCC). New Definition of Age of Dependants Now in Force. Government of Canada. 2017. Available online: https://www.canada.ca/en/immigration-refugees-citizenship/news/2017/10/new_definition_ofageofdependantsnowinforce.html (accessed on 21 July 2021).
- Immigration, Refugees and Citizenship Canada (IRCSS). Syrian Outcomes Report. Evaluation Division. Research and Evaluation. 2019. Available online: https://www.canada.ca/en/immigration-refugees-citizenship/corporate/reports-statistics/evaluations/syrian-outcomes-report-2019.html (accessed on 21 July 2021).
- McMurdo, A.M.B. Causes and consequences of Canada’s resettlement of Syrian refugees. Forced Migr. Rev. 2016, 52, 82–84. [Google Scholar]
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child pre-migratory adversity | — | |||||||||||
| 2. Parental pre-migratory adversity | −0.01 | — | ||||||||||
| 3. Familial pre-migratory adversity | 0.57 *** | 0.82 *** | — | |||||||||
| 4. Emotion regulation | 0.01 | −0.05 | −0.03 | — | ||||||||
| 5. Sympathy | −0.20 | 0.08 | −0.09 | −0.17 | — | |||||||
| 6. Optimism | −0.06 | 0.15 | 0.09 | 0.12 | 0.37 *** | — | ||||||
| 7. Trust | −0.21 * | 0.24 * | 0.12 | −0.30 ** | 0.29 ** | 0.29 ** | — | |||||
| 8. Internalizing | 0.02 | 0.14 | 0.16 | −0.53 *** | 0.11 | −0.28 ** | 0.23 * | — | ||||
| 9. Externalizing | 0.19 | 0.12 | 0.22 | −0.55 *** | −0.23 * | −0.27 ** | 0.02 | 0.57 *** | — | |||
| 10. Child age | 0.05 | 0.09 | 0.09 | −0.16 | 0.14 | −0.05 | 0.07 | 0.18 | −0.04 | — | ||
| 11. Child gender (male) | 0.16 | −0.23 * | −0.08 | −0.03 | −0.21 * | −0.22 * | −0.16 | 0.10 | 0.24 ** | 0.02 | — | |
| 12. Length of stay in Canada | −0.14 | −0.27 * | −0.29 ** | −0.12 | 0.15 | −0.06 | 0.02 | 0.04 | −0.02 | −0.23 * | 0.14 | — |
| Min | 0.00 | 0.00 | 0.00 | 0.00 | 0.75 | 1.25 | 0.00 | 0.00 | 0.20 | 5.00 | 0.00 | 3.00 |
| Max | 4.00 | 5.00 | 9.00 | 3.00 | 3.00 | 3.00 | 3.00 | 1.90 | 2.40 | 12.00 | 1.00 | 30.00 |
| M | 1.41 | 2.48 | 3.84 | 0.97 | 2.41 | 2.60 | 1.94 | 0.94 | 1.09 | 8.01 | — | 14.34 |
| SD | 0.99 | 1.44 | 1.76 | 0.72 | 0.58 | 0.46 | 0.75 | 0.46 | 0.52 | 2.26 | — | 6.30 |
| Internalizing | Externalizing | |||||
|---|---|---|---|---|---|---|
| Variable | β | SE | p | β | SE | p |
| Child age | 0.10 | 0.08 | 0.19 | −0.09 | 0.07 | 0.20 |
| Child gender (male) | 0.09 | 0.07 | 0.22 | 0.18 | 0.07 | 0.01 |
| Length of stay in Canada | 0.07 | 0.07 | 0.34 | −0.01 | 0.08 | 0.88 |
| Familial pre-migratory adversity | 0.29 | 0.11 | 0.006 | 0.20 | 0.08 | 0.009 |
| Emotion regulation | −0.39 | 0.07 | <0.001 | −0.60 | 0.07 | <0.001 |
| Optimism | −0.31 | 0.08 | <0.001 | −0.07 | 0.07 | 0.34 |
| Trust | 0.19 | 0.07 | 0.007 | - | - | - |
| Familial Pre-Migratory Adversity × Optimism | −0.26 | 0.12 | 0.03 | - | - | - |
| Sympathy | - | - | - | −0.27 | 0.08 | 0.001 |
| Familial Pre-Migratory Adversity × Emotion Regulation | - | - | - | −0.10 | 0.07 | 0.14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Speidel, R.; Galarneau, E.; Elsayed, D.; Mahhouk, S.; Filippelli, J.; Colasante, T.; Malti, T. Refugee Children’s Social–Emotional Capacities: Links to Mental Health upon Resettlement and Buffering Effects on Pre-Migratory Adversity. Int. J. Environ. Res. Public Health 2021, 18, 12180. https://doi.org/10.3390/ijerph182212180
Speidel R, Galarneau E, Elsayed D, Mahhouk S, Filippelli J, Colasante T, Malti T. Refugee Children’s Social–Emotional Capacities: Links to Mental Health upon Resettlement and Buffering Effects on Pre-Migratory Adversity. International Journal of Environmental Research and Public Health. 2021; 18(22):12180. https://doi.org/10.3390/ijerph182212180
Chicago/Turabian StyleSpeidel, Ruth, Emma Galarneau, Danah Elsayed, Shahdah Mahhouk, Joanne Filippelli, Tyler Colasante, and Tina Malti. 2021. "Refugee Children’s Social–Emotional Capacities: Links to Mental Health upon Resettlement and Buffering Effects on Pre-Migratory Adversity" International Journal of Environmental Research and Public Health 18, no. 22: 12180. https://doi.org/10.3390/ijerph182212180
APA StyleSpeidel, R., Galarneau, E., Elsayed, D., Mahhouk, S., Filippelli, J., Colasante, T., & Malti, T. (2021). Refugee Children’s Social–Emotional Capacities: Links to Mental Health upon Resettlement and Buffering Effects on Pre-Migratory Adversity. International Journal of Environmental Research and Public Health, 18(22), 12180. https://doi.org/10.3390/ijerph182212180






