Validity and Reliability of the Korean Version of the Self-Care of Diabetes Inventory (SCODI-K)
Abstract
1. Introduction
2. Materials and Methods
2.1. Aims
2.2. Study Design
2.3. Participants
2.4. Tools
2.4.1. Characteristics of Participants
2.4.2. Self-Care of Diabetes Inventory
2.4.3. The Summary of Diabetes Self-Care Activities (SDSCA) Questionnaire
2.4.4. Physiological Indicators
2.5. Development of the Korean Version of the SCODI
2.6. Data Collection
2.7. Ethical Consideration
2.8. Data Analysis
3. Results
3.1. Characteristics of Participants and Their Difference in the SCODI-K
3.2. Exploratory Factor Analysis of SCODI-K
3.2.1. Self-Care Maintenance
3.2.2. Self-Care Monitoring
3.2.3. Self-Care Management
3.2.4. Self-Care Confidence
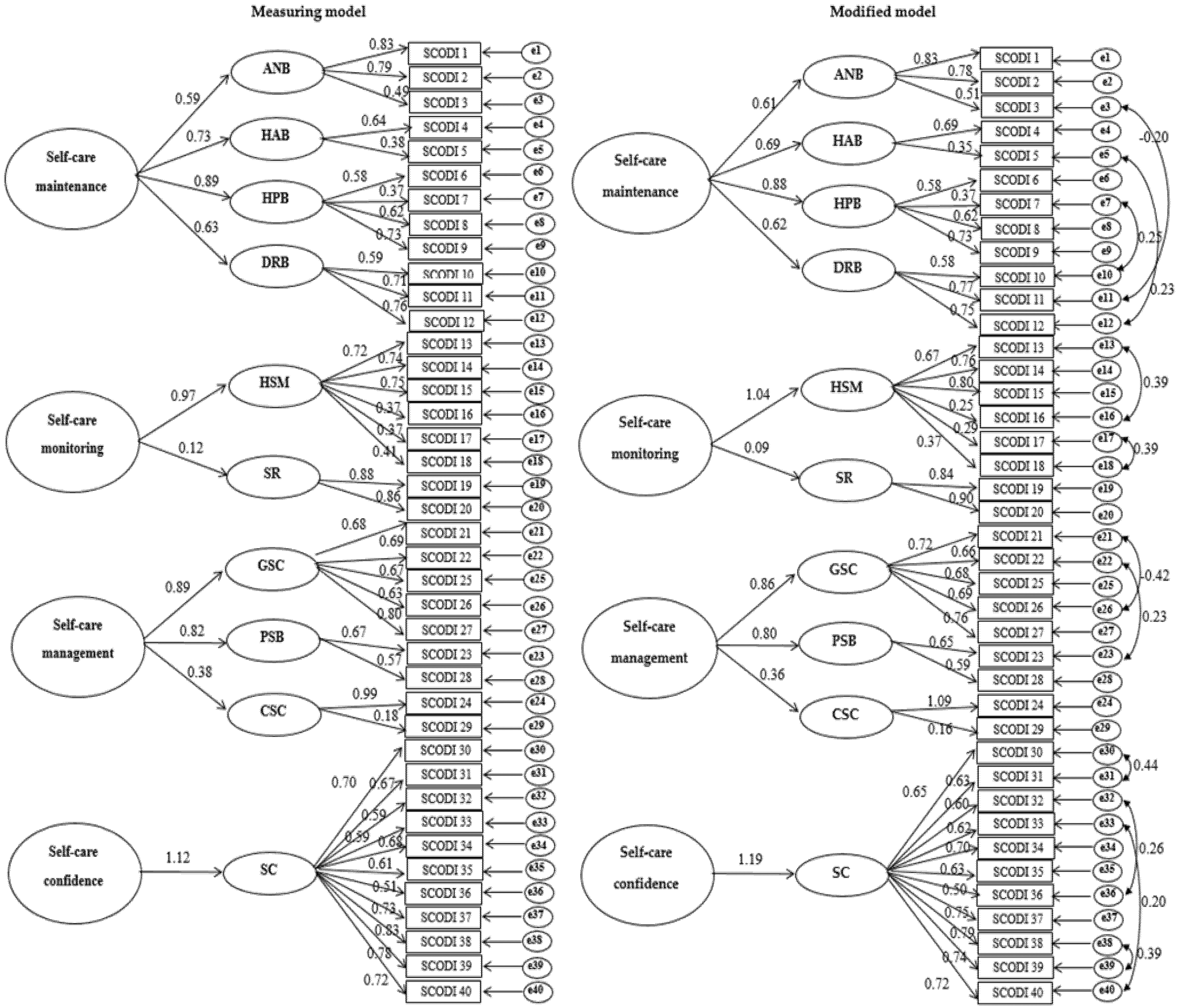
3.3. Confirmatory Factor Analysis of SCODI-K
3.4. Construct Validity of SCODI-K
3.5. Criterion-Related and Concurrent Validity of SCODI-K
3.6. Reliability of SCODI-K
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Korean Diabetes Association. Treatment Guidelines for Diabetes. Available online: https://www.diabetes.or.kr/pro/publish/guide.php?code=guide&mode=view&number=765 (accessed on 10 August 2021).
- International Diabetes Federation. IDF Diabetes Atlas Ninth Edition 2019. Available online: https://www.idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html (accessed on 10 August 2021).
- Korean Diabetes Association. Diabetes Fact Sheet in Korea 2018, Seoul; Korean Diabetes Association: Seoul, Korea, 2018; Available online: https://www.diabetes.or.kr/bbs/index.html?code=e_resource&number=381&mode=view (accessed on 12 April 2021).
- National Center for Chronic Disease Prevention and Heath Promotion. Disease Prevention and Health Promotion. National Diabetes Statistics Report; CDC: Atlanta, GA, USA, 2017. Available online: https://www.cdc.gov/diabetes/ (accessed on 10 August 2021).
- Sinclair, A.J.; Abdelhafiz, A.H.; Rodríguez-Mañas, L. Frailty and sarcopenia—Newly emerging and high impact complications of diabetes. J. Diabetes Complicat. 2017, 31, 1465–1473. [Google Scholar] [CrossRef]
- Basevi, V.; Di Mario, S.; Morciano, C.; Nonino, F.; Magrini, N. Comment on: American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care 2011, 34 (Suppl. S1), S11–S61. [Google Scholar] [CrossRef]
- Chrvala, C.A.; Sherr, D.; Lipman, R.D. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ. Couns. 2016, 99, 926–943. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.-Y.; Gu, M.-O. Comparative study on Self-care Behavior, Diabetes-related stress, and stress coping among Good, inadequate, and Poor glycemic control groups. J. Korean Acad. Fundam. Nurs. 2012, 19, 168–178. [Google Scholar] [CrossRef][Green Version]
- Devarajooh, C.; Chinna, K. Depression, distress and self-efficacy: The impact on diabetes self-care practices. PLoS ONE 2017, 12, e0175096. [Google Scholar] [CrossRef]
- Sittner, K.J.; Greenfield, B.L.; Walls, M.L. Microaggressions, diabetes distress, and self-care behaviors in a sample of American Indian adults with type 2 diabetes. J. Behav. Med. 2017, 41, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Al-Amer, R.; Ramjan, L.; Glew, P.; Randall, S.; Salamonson, Y. Self-Efficacy, depression, and self-care activities in Adult Jordanians with type 2 diabetes: The role of illness Perception. Issues Ment. Health Nurs. 2016, 37, 744–755. [Google Scholar] [CrossRef]
- Boren, S.A. AADE7™ self-care behaviors: Systematic reviews. Diabetes Educ. 2007, 33, 866–871. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Chew, B.H.; Vos, R.C.; Metzendorf, M.-I.; Scholten, R.J.P.M.; Rutten, G.E.H.M. Psychological interventions for diabetes-related distress in adults with type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2017, 9, CD011469. [Google Scholar] [CrossRef]
- Borhaninejad, V.; Shati, M.; Bhalla, D.; Iranpour, A.; Fadayevatan, R. A population-based survey to determine Association of perceived social support and Self-efficacy With self-care among elderly with diabetes mellitus (Kerman City, Iran). Int. J. Aging Hum. Dev. 2017, 85, 504–517. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.; Rocco, M. KDOQI clinical practice guidelines and clinical Practice recommendations for diabetes and chronic kidney disease. Am. J. Kidney Dis. 2007, 49, S12–S154. [Google Scholar] [CrossRef]
- Ausili, D.; Barbaranelli, C.; Rossi, E.; Rebora, P.; Fabrizi, D.; Coghi, C.; Luciani, M.; Vellone, E.; Di Mauro, S.; Riegel, B. Development and psychometric testing of a Theory-based tool to Measure self-care in diabetes patients: The Self-care of Diabetes inventory. BMC Endocr. Disord. 2017, 17, 66. [Google Scholar] [CrossRef] [PubMed]
- Caro-Bautista, J.; Martín-Santos, F.J.; Morales-Asencio, J.M. Systematic review of the psychometric properties and theoretical grounding of instruments evaluating self-care in people with type 2 Diabetes Mellitus. J. Adv. Nurs. 2014, 70, 1209–1227. [Google Scholar] [CrossRef] [PubMed]
- Toobert, D.J.; Hampson, S.E.; Glasgow, R.E. The summary of Diabetes self-care activities measure: Results from 7 studies and a Revised scale. Diabetes Care 2000, 23, 943–950. [Google Scholar] [CrossRef]
- Weinger, K.; Butler, H.A.; Welch, G.W.; La Greca, A.M. Measuring diabetes self-care: A psychometric analysis of the Self-Care Inventory-Revised with adults. Diabetes Care 2005, 28, 1346–1352. [Google Scholar] [CrossRef] [PubMed]
- Markle-Reid, M.; Ploeg, J.; Fraser, K.D.; Fisher, K.A.; Bartholomew, A.; Griffith, L.E.; Miklavcic, J.; Gafni, A.; Thabane, L.; Upshur, R. Community program improves quality of life and self-management in older adults with diabetes mellitus and comorbidity. J. Am. Geriatr. Soc. 2018, 66, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Powers, M.A.; Bardsley, J.; Cypress, M.; Duker, P.; Funnell, M.M.; Fischl, A.H.; Maryniuk, M.D.; Siminerio, L.; Vivian, E. Diabetes self-management education and support in type 2 diabetes: A joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Educ. 2017, 43, 40–53. [Google Scholar] [CrossRef]
- Nicolucci, A.; Kovacs Burns, K.; Holt, R.I.G.; Comaschi, M.; Hermanns, N.; Ishii, H.; Kokoszka, A.; Pouwer, F.; Skovlund, S.E.; Stuckey, H.; et al. Diabetes Attitudes, Wishes and Needs second study (DAWN2™): Cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet. Med. 2013, 30, 767–777. [Google Scholar] [CrossRef] [PubMed]
- Comrey, A.L.; Osborne, J. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 2005, 10, 7. [Google Scholar] [CrossRef]
- Comrey, A.L.; Lee, H.B. A First Course in Factor Analysis; Psychology Press: New York, NY, USA, 1992. [Google Scholar]
- Chang, S.J.; Song, M.S. The validity and reliability of a Korean version of the summary of diabetes self-care activities questionnaire for older patients with type 2 diabetes. Korean J. Adult Nurs. 2009, 21, 235–244. [Google Scholar]
- Self Care of Diabetes Inventory. Available online: http://self-care-measures.com/available-self-care-measures/self-care-of-diabetes-inventory/ (accessed on 12 May 2021).
- Chamberlain, J.J.; Rhinehart, A.S.; Shaefer, C.F., Jr.; Neuman, A. Diagnosis and management of diabetes: Synopsis of the 2016 American Diabetes Association Standards of Medical Care in Diabetes. Ann. Intern. Med. 2016, 164, 542–552. [Google Scholar] [CrossRef] [PubMed]
- Ebadi, A.; Ausili, D.; Albatineh, A.N.; Salarvand, S.; Ghanei Ghashlagh, R. Psychometric evaluation of the Farsi version of the Self-care of Diabetes inventory in Iranian patients with Diabetes. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 2775–2784. [Google Scholar] [CrossRef] [PubMed]
- Geldhof, G.J.; Preacher, K.J.; Zyphur, M.J. Reliability estimation in a multilevel confirmatory factor analysis framework. Psychol. Methods 2014, 19, 72–91. [Google Scholar] [CrossRef] [PubMed]
- Sousa, V.D.; Rojjanasrirat, W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J. Eval. Clin. Pract. 2011, 17, 268–274. [Google Scholar] [CrossRef] [PubMed]
- American Association of Diabetes Educators. An effective model of diabetes care and education: Revising the AADE7 Self-Care Behaviors®. Diabetes Educ. 2020, 46, 139–160. [Google Scholar] [CrossRef] [PubMed]
- Gere, J.; MacDonald, G. Assessing relationship quality across cultures: An examination of measurement equivalence. Pers. Relatsh. 2013, 20, 422–442. [Google Scholar] [CrossRef]
- Kong, S.-Y.; Cho, M.-K. Factors related to self-care in patients with type 2 diabetes. Open Nurs. J. 2020, 14, 64–73. [Google Scholar] [CrossRef]
| Characteristics | Categories | N (%) | Self-Care | |
|---|---|---|---|---|
| M ± SD | t or F (p) | |||
| Gender | Male | 118 (56.2) | 66.27 ± 16.77 | −3.75 (<0.001) |
| Female | 92 (43.8) | 74.27 ± 14.13 | ||
| Age (year) | <60 | 92 (43.8) | 63.88 ± 15.38 | −4.93 (<0.001) |
| ≥60 | 118 (56.2) | 74.37 ± 15.23 | ||
| Marital status | Married | 180 (85.7) | 70.04 ± 16.16 | 0.59 (0.556) |
| The others | 30 (14.3) | 68.17 ± 16.15 | ||
| Education | ≤Middle school | 60 (28.6) | 70.85 ± 17.52 | 0.61 (0.543) |
| ≥High school | 150 (71.4) | 69.35 ± 15.58 | ||
| Occupation | Unemployed | 114 (54.3) | 73.41 ± 14.50 | 3.66 (<0.001) |
| Employed | 96 (45.7) | 65.46 ± 16.96 | ||
| Economic status | Low | 33 (15.7) | 65.30 ± 14.19 | −1.74 (0.083) |
| ≥Middle | 177 (84.3) | 70.61 ± 16.37 | ||
| Care givers | No | 73 (34.8) | 68.27 ± 16.18 | −0.99 (.326) |
| Yes | 137 (65.2) | 70.58 ± 16.10 | ||
| Drinking | No | 121 (57.6) | 72.31 ± 14.94 | 2.70 (0.008) |
| Yes | 89 (42.4) | 66.33 ± 17.10 | ||
| Smoking | No | 178 (84.8) | 71.90 ± 15.06 | 4.72 (<0.001) |
| Yes | 32 (15.2) | 57.97 ± 17.00 | ||
| BMI (kg/m2) | <18.5 | 7 (3.3) | 71.71 ± 16.17 | 0.90 (0.914) |
| 18.5~22.9 | 48 (22.9) | 70.19 ± 19.03 | ||
| ≥23 | 154 (73.3) | 69.48 ± 15.25 | ||
| Duration of disease (year) | <10 | 108 (51.4) | 65.33 ± 16.91 | −4.27 (<0.001) |
| ≥10 | 102 (48.6) | 74.48 ± 13.85 | ||
| Complication of DM | No | 101 (48.1) | 69.19 ± 16.16 | −0.51 (0.612) |
| Yes | 109 (51.9) | 70.32 ± 16.16 | ||
| Experience of hospitalization with DM | No | 158 (75.2) | 69.69 ± 15.58 | −0.14 (0.893) |
| Yes | 52 (24.8) | 70.04 ± 17.86 | ||
| Family history | No | 128 (61.0) | 70.30 ± 16.05 | 0.58 (0.560) |
| Yes | 82 (39.0) | 68.96 ± 16.31 | ||
| Experience of DM education | No | 133 (63.3) | 68.72 ± 16.22 | −1.25 (0.214) |
| Yes | 77 (36.7) | 71.60 ± 15.91 | ||
| Treatment modality | OHA | 162 (77.1) | 69.04 ± 16.42 | 1.51 (0.222) |
| Insulin | 36 (17.1) | 70.61 ± 15.55 | ||
| OHA and insulin | 12 (5.7) | 77.25 ± 12.59 | ||
| Comorbidity | No | 37 (17.6) | 70.51 ± 15.89 | 0.31 (0.760) |
| Yes | 173 (82.4) | 69.62 ± 16.22 | ||
| HbA1c (%) | <6.5 | 46 (21.9) | 68.63 ± 15.90 | −0.54 (0.587) |
| ≥6.5 | 164 (78.1) | 70.10 ± 16.23 | ||
| FBG (mg/dL) | <130 | 98 (46.7) | 70.21 ± 15.81 | 0.37 (0.714) |
| ≥130 | 112 (53.3) | 69.39 ± 16.46 | ||
| Cholesterol (mg/dL) | <200 | 186 (88.6) | 69.53 ± 16.25 | −0.62 (0.534) |
| ≥200 | 24 (11.4) | 71.71 ± 15.36 | ||
| Exploratory Factor Analysis | Confirmatory Factor Analysis | ||||||
|---|---|---|---|---|---|---|---|
| Items | M ± SD | Factor Loadings | Factor Loadings | ||||
| 1 | 2 | 3 | 4 | ||||
| Self-care | 68.03 ± 15.92 | ||||||
| Self-care maintenance | 74.23 ± 16.47 | ||||||
| 1. Do you maintain an active lifestyle? (Examples: walking, going out, doing outdoor activities.) | 3.46 ± 1.40 | 0.83 | 0.83 | ||||
| 2. Do you exercise 2.5 h per week? (Examples: swimming, going to the gym, riding a bicycle, walking.) | 2.99 ± 1.60 | 0.80 | 0.79 | ||||
| 3. Do you eat a balanced diet containing carbohydrates (pasta, rice, sugars, bread), protein (meats, fish, beans), fruits, and vegetables? | 3.29 ± 1.32 | 0.64 | 0.49 | ||||
| 12. Many people do not properly take their prescribed medicine. Do you take all medicines prescribed by your doctor? | 4.74 ± 0.72 | 0.80 | 0.76 | ||||
| 11. Do you get your health check-ups on time? (Examples: blood test, urine test, ultrasound, eye check-up.) | 4.66 ± 0.87 | 0.79 | 0.71 | ||||
| 10. Do you keep your appointments with your doctor? | 4.87 ± 0.55 | 0.73 | 0.60 | ||||
| 7. Are you refraining from smoking? | 4.35 ± 1.44 | 0.74 | 0.37 | ||||
| 9. Do you maintain good oral hygiene? (Brush teeth at least twice a day. Use mouthwash and dental floss.) | 4.05 ± 1.21 | 0.72 | 0.73 | ||||
| 6. Are you managing your health? (Examples: washing hands, receiving recommended vaccines.) | 4.22 ± 1.12 | 0.60 | 0.58 | ||||
| 8. Do you care for your feet? (Apply moisturizer after washing and drying feet. Wear proper socks.) | 3.67 ± 1.45 | 0.58 | 0.62 | ||||
| 5. Are you limiting alcohol intake? (Allowable alcohol consumption is two shots of soju a day for men and one shot of soju a day for women.) | 4.12 ± 1.39 | 0.84 | 0.38 | ||||
| 4. Do you avoid salt and fats? (Example: cheese, cured meats, sweets, red meats.) | 3.18 ± 1.33 | 0.52 | 0.64 | ||||
| Eigenvalue | 2.36 | 2.03 | 1.91 | 1.25 | |||
| Explained variance (%) | 19.7 | 16.9 | 15.9 | 10.4 | CR | 0.9 | |
| Total explained variances (%) | 19.7 | 36.6 | 52.5 | 62.9 | AVE | 0.4 | |
| Self-care monitoring | 66.01 ± 19.56 | ||||||
| 13. Do you regularly measure your blood sugar? | 3.65 ± 1.44 | 0.80 | 0.72 | ||||
| 15. Do you take your blood pressure? | 3.31 ± 1.53 | 0.78 | 0.75 | ||||
| 14. Do you check your weight? | 3.91 ± 1.27 | 0.77 | 0.74 | ||||
| 16. Do you keep a record of your blood sugar in a diary or notebook? | 2.32 ± 1.62 | 0.52 | 0.37 | ||||
| 17. Do you check your feet every day for wounds, redness, or blisters? | 4.03 ± 1.37 | 0.48 | 0.37 | ||||
| 18. Are you paying attention to high-blood-sugar symptoms (thirst, frequent urination) and low-blood-sugar symptoms (weakness, perspiration, anxiety)? | 4.26 ± 1.15 | 0.47 | 0.41 | ||||
| 19. Did you recognize quickly that you have the above symptoms? | 3.52 ± 1.65 | 0.90 | 0.88 | ||||
| 20. Did you recognize quickly that the above symptoms were caused by diabetes? | 3.45 ± 1.71 | 0.90 | 0.86 | ||||
| Eigenvalue | 2.58 | 1.97 | |||||
| Explained variance (%) | 32.2 | 24.6 | CR | 0.9 | |||
| Total explained variances (%) | 32.2 | 56.8 | AVE | 0.5 | |||
| Self-care management | 56.56 ± 25.18 | ||||||
| 26. When you have high blood-sugar levels, do you lower your blood sugar by exercising? | 3.40 ± 1.56 | 0.82 | 0.63 | ||||
| 27. Do you check your blood sugar again to assess whether your actions to adjust the abnormal blood-sugar level were effective? | 3.03 ± 1.66 | 0.80 | 0.80 | ||||
| 21. Do you check your blood sugar when you feel you have symptoms (thirst, frequent urination, weakness, perspiration, anxiety)? | 3.10 ± 1.60 | 0.75 | 0.68 | ||||
| 25. When you have high blood-sugar levels, do you lower your blood sugar by adjusting your diet? | 3.69 ± 1.42 | 0.66 | 0.67 | ||||
| 22. When you have abnormal blood-sugar levels, do you keep a record of what caused it and what you did to address it? | 2.54 ± 1.56 | 0.51 | 0.69 | ||||
| 24. When you have low blood-sugar levels, do you solve the problem by eating sugary foods or drinks? | 3.83 ± 1.44 | 0.76 | 0.99 | ||||
| 29. When your blood-sugar levels are too high or low, do you adjust your insulin dose as per your doctor’s suggestion? * | 4.71 ± 0.65 | 0.75 | 0.18 | ||||
| 28. When your blood-sugar levels were too high or low, did you see your doctor? | 3.28 ± 1.58 | 0.84 | 0.57 | ||||
| 23. When you have abnormal blood-sugar levels, do you ask for advice from your family or friends? | 2.92 ± 1.59 | 0.69 | 0.67 | ||||
| Eigenvalue | 2.73 | 1.92 | 1.35 | ||||
| Explained variance (%) | 30.3 | 21.4 | 15.0 | CR | 0.9 | ||
| Total explained variances (%) | 30.3 | 51.6 | 66.6 | AVE | 0.5 | ||
| Self-care confidence | 79.15 ± 19.41 | ||||||
| 38. I can take actions to control my blood-sugar level and relieve symptoms. | 4.11 ± 1.15 | 0.83 | 0.83 | ||||
| 39. I can evaluate whether the actions taken to control blood-sugar levels and relieve symptoms were effective. | 3.90 ± 1.19 | 0.78 | 0.78 | ||||
| 37. I can continue self-care for diabetes no matter what. | 4.30 ± 1.01 | 0.76 | 0.73 | ||||
| 40. I can continue carrying out those actions to improve my blood-sugar levels in any situation. | 4.25 ± 0.94 | 0.75 | 0.72 | ||||
| 34. I can check my blood-sugar level as many times as ordered by my doctor. | 4.20 ± 1.12 | 0.73 | 0.68 | ||||
| 30. I can prevent high blood sugar or low blood sugar and their symptoms. | 3.82 ± 1.28 | 0.73 | 0.70 | ||||
| 31. I can adhere to the nutrition and physical activity guidelines. | 3.86 ± 1.18 | 0.71 | 0.67 | ||||
| 33. I can persist to the treatment plan in any situation. | 4.45 ± 0.89 | 0.67 | 0.61 | ||||
| 32. I can take my medicine correctly. (Including insulin, as prescribed.) | 4.53 ± 0.87 | 0.67 | 0.59 | ||||
| 35. When I check my blood-sugar levels, I understand whether it is under control. | 4.28 ± 1.07 | 0.66 | 0.61 | ||||
| 36. I can recognize low-blood-sugar symptoms. | 4.11 ± 1.28 | 0.58 | 0.51 | ||||
| Eigenvalue | 5.64 | ||||||
| Explained variance (%) | 51.2 | CR | 0.9 | ||||
| Total explained variances (%) | 51.2 | AVE | 0.5 | ||||
| Variable | Measuring Model | Modified Model | ||||||
|---|---|---|---|---|---|---|---|---|
| χ²/df | RMSEA | CFI | GFI | χ²/df | RMSEA | CFI | GFI | |
| SCODI | ||||||||
| Self-care maintenance | 2.214 | 0.076 | 0.896 | 0.919 | 1.875 | 0.065 | 0.930 | 0.937 |
| Self-care monitoring | 4.771 | 0.134 | 0.855 | 0.900 | 1.915 | 0.066 | 0.969 | 0.963 |
| Self-care management | 3.447 | 0.108 | 0.874 | 0.912 | 2.491 | 0.084 | 0.933 | 0.945 |
| Self-care confidence | 4.753 | 0.134 | 0.855 | 0.846 | 3.056 | 0.099 | 0.928 | 0.912 |
| Variables | SCODI | SDSCA | HbA1c | FBG |
|---|---|---|---|---|
| r (p) | ||||
| SDSCA | 0.75 (<0.001) | |||
| HbA1c | 0.04 (0.563) | 0.11 (0.109) | ||
| FBG | 0.01 (0.993) | 0.02 (0.757) | 0.56 (<0.001) | |
| Cholesterol | 0.02 (0.744) | −0.01 (0.921) | 0.20 (0.004) | 0.07 (0.293) |
| Variables | Items | M ± SD | Cronbach’s α | |
|---|---|---|---|---|
| Korean Version | Original | |||
| SCODI | 40 | 69.78 ± 16.13 | 0.92 | |
| Self-care maintenance | 12 | 74.23 ± 16.47 | 0.77 | 0.81 |
| Self-care monitoring | 8 | 66.01 ± 19.56 | 0.69 | 0.84 |
| Self-care management | 9 | 56.56 ± 25.18 | 0.81 | 0.86 |
| Self-care confidence | 11 | 79.15 ± 19.41 | 0.90 | 0.89 |
| SDSCA | 17 | 37.08 ± 14.44 | 0.79 | 0.68 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kong, S.-Y.; Cho, M.-K. Validity and Reliability of the Korean Version of the Self-Care of Diabetes Inventory (SCODI-K). Int. J. Environ. Res. Public Health 2021, 18, 12179. https://doi.org/10.3390/ijerph182212179
Kong S-Y, Cho M-K. Validity and Reliability of the Korean Version of the Self-Care of Diabetes Inventory (SCODI-K). International Journal of Environmental Research and Public Health. 2021; 18(22):12179. https://doi.org/10.3390/ijerph182212179
Chicago/Turabian StyleKong, Seung-Yeon, and Mi-Kyoung Cho. 2021. "Validity and Reliability of the Korean Version of the Self-Care of Diabetes Inventory (SCODI-K)" International Journal of Environmental Research and Public Health 18, no. 22: 12179. https://doi.org/10.3390/ijerph182212179
APA StyleKong, S.-Y., & Cho, M.-K. (2021). Validity and Reliability of the Korean Version of the Self-Care of Diabetes Inventory (SCODI-K). International Journal of Environmental Research and Public Health, 18(22), 12179. https://doi.org/10.3390/ijerph182212179






