Referral Patterns in Oral Medicine: A Retrospective Analysis of an Oral Medicine University Center in Southern Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
3.1. Patient Demographic Characteristics
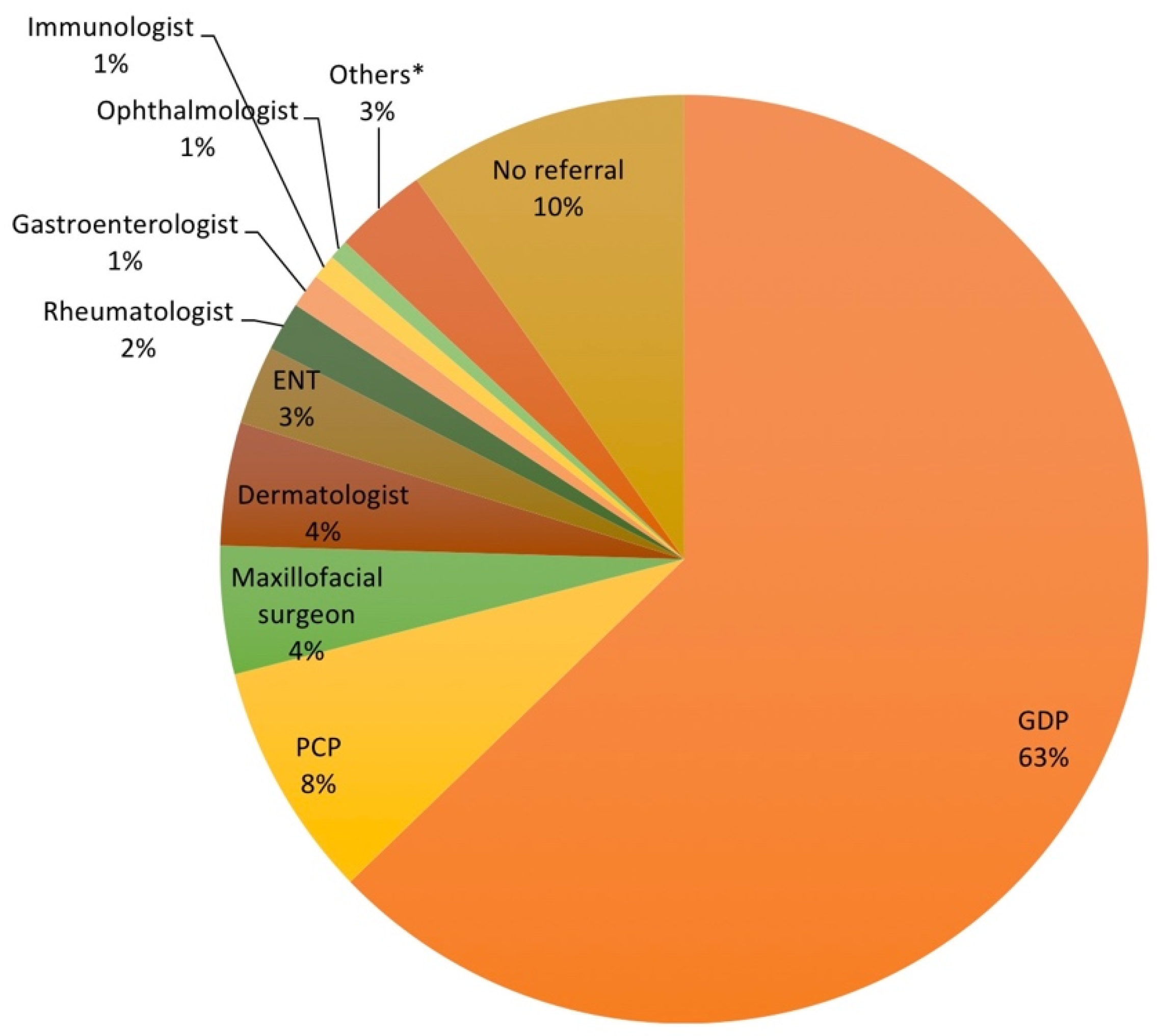
3.2. Referral Source
3.3. Diagnostic Procedures Ordered by Referral
3.4. Reasons for Referral
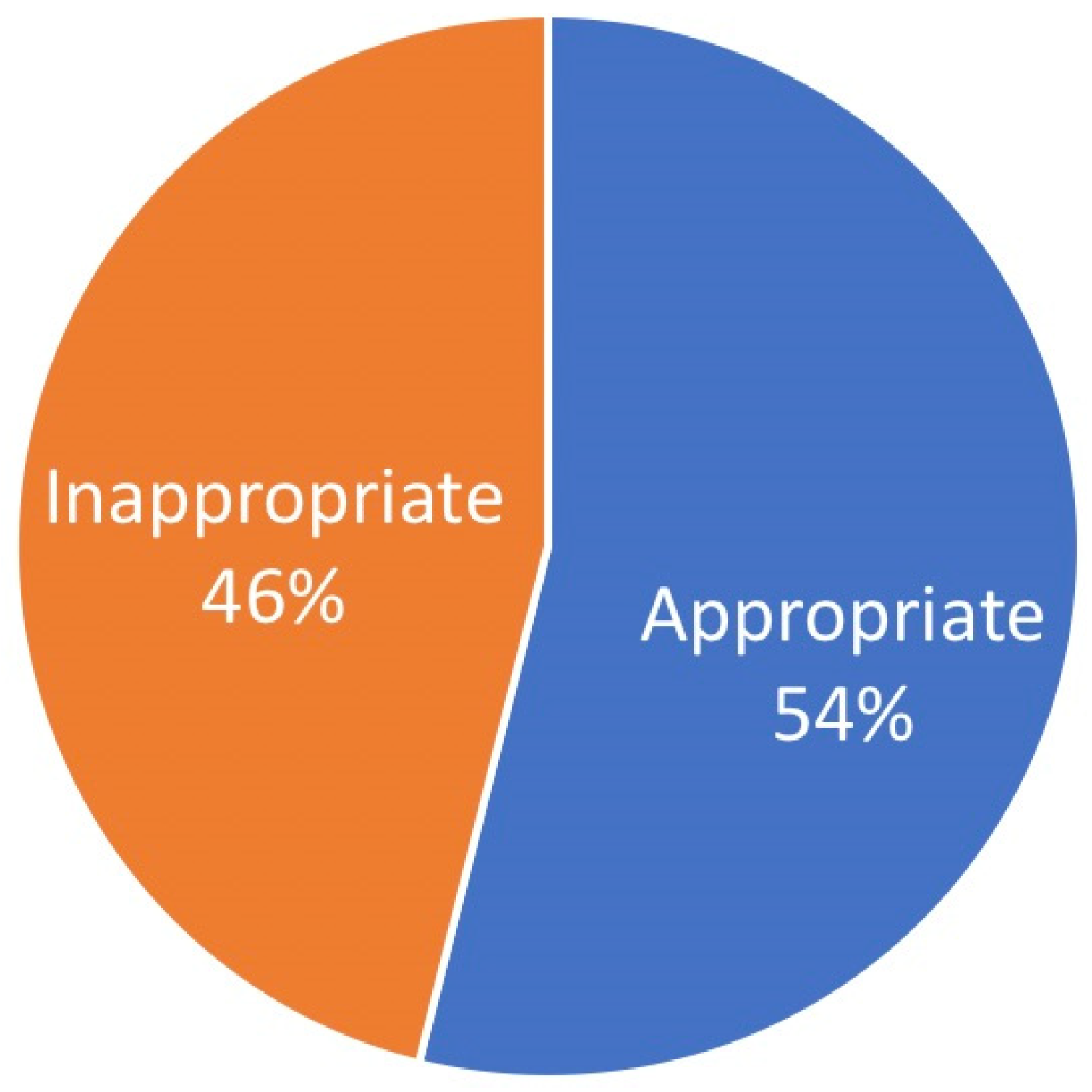
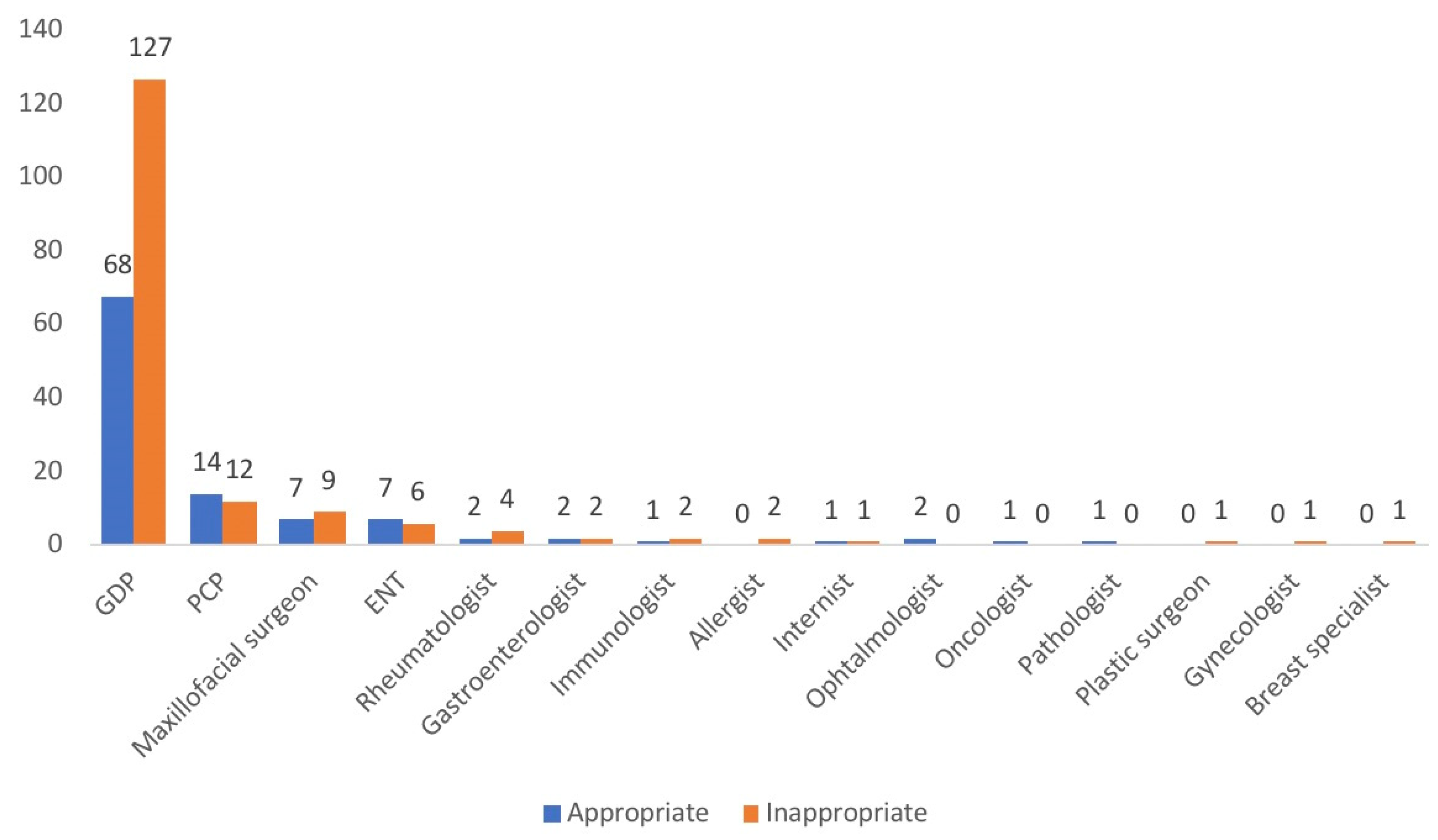
3.5. Accuracy of Referrals
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hensher, M.; Price, M.; Adomakoh, S. Referral hospitals. In Disease Control Priorities in Developing Countries, 2nd ed.; Chapter 66; Jamison, D.T., Breman, J.G., Measham, A.R., Alleyne, G., Claeson, M., Evans, D.B., Jha, P., Mills, A., Musgrove, P., Eds.; Oxford University Press and The World Bank: New York, NY, USA, 2006. [Google Scholar]
- Mehrotra, A.; Forrest, C.B.; Lin, C.Y. Dropping the baton: Specialty referrals in the United States. Milbank Q. 2011, 89, 39–68. [Google Scholar] [CrossRef]
- Guevara, J.P.; Hsu, D.; Forrest, C.B. Performance measures of the specialty referral process: A systematic review of the literature. BMC Heal. Serv. Res. 2011, 11, 168. [Google Scholar] [CrossRef] [PubMed]
- Dickie, J.A.; Ellwood, D.A.; Robertson, M. What’s in a referral letter: Does the detail matter? Australas. J. Ultrasound Med. 2011, 14, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Sampson, R.; Cooper, J.; Barbour, R.; Polson, R.; Wilson, P. Patients’ perspectives on the medical primary–secondary care interface: Systematic review and synthesis of qualitative research. BMJ Open 2015, 5, e008708. [Google Scholar] [CrossRef]
- Tobin-Schnittger, P.; O’Doherty, J.; O’Connor, R.; O’Regan, A. Improving quality of referral letters from primary to secondary care: A literature review and discussion paper. Prim. Health Care Res. Dev. 2017, 19, 211–222. [Google Scholar] [CrossRef]
- Tzartzas, K.; Oberhauser, P.-N.; Marion-Veyron, R.; Bourquin, C.; Senn, N.; Stiefel, F. General practitioners referring patients to specialists in tertiary healthcare: A qualitative study. BMC Fam. Pract. 2019, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Moore, K. Social Determinants of Health: Addressing Barriers Through Screening, Referrals, and Care Coordination. North Carol. Med. J. 2019, 80, 306–311. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Oral Medicine. Available online: http://www.aaom.com/ (accessed on 25 September 2021).
- Bez, C.; Sklavounou, A.; Carrozzo, M. Oral medicine in Europe: Past, present and future. Br. Dent. J. 2017, 223, 726–728. [Google Scholar] [CrossRef] [PubMed]
- Scully, C.; Miller, C.S.; Urizar, J.-M.A.; Alajbeg, I.; Almeida, O.P.; Bagan, J.V.; Birek, C.; Chen, Q.; Farah, C.; Figueirido, J.P.; et al. Oral medicine (stomatology) across the globe: Birth, growth, and future. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 121, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Spielman, A.I. The future of oral medicine. Oral Dis. 2018, 24, 285–288. [Google Scholar] [CrossRef]
- Available online: https://www.england.nhs.uk/south/wp-content/uploads/sites/6/2019/02/mcn-oral-medicine-referral-guidelines-for-gdps-jan-2019-v1.pdf (accessed on 5 November 2021).
- Riordain, R.; O’Sullivan, K.; McCreary, C. Retrospective evaluation of the referral pattern to an oral medicine unit in Ireland. Community Dent. Health 2011, 28, 107–110. [Google Scholar] [CrossRef]
- Villa, A.; Stock, S.; Aboalela, A.; Lerman, M.A.; Woo, S.-B.; Sonis, S.T.; Treister, N.S. Oral Medicine referrals at a hospital-based practice in the United States. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 119, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Farah, C.S.; Simanovic, B.; Savage, N.W. Scope of practice, referral patterns and lesion occurrence of an oral medicine service in Australia. Oral Dis. 2008, 14, 367–375. [Google Scholar] [CrossRef]
- ICD-11. International Classification of Diseases 11th Revision. Available online: https://icd.who.int/en. (accessed on 17 November 2021).
- Friesen, R.; McGaw, T.; Peters, E.; Lai, H. A retrospective analysis of referral patterns to a university oral medicine clinic. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 128, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Patterson, J.; Willis, A. Oral Medicine Considerations for Older Patients. Prim. Dent. J. 2020, 9, 45–53. [Google Scholar] [CrossRef]
- Coppola, N.; Mignogna, M.; Rivieccio, I.; Blasi, A.; Bizzoca, M.; Sorrentino, R.; Muzio, L.L.; Spagnuolo, G.; Leuci, S. Current Knowledge, Attitudes, and Practice among Health Care Providers in OSCC Awareness: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4506. [Google Scholar] [CrossRef]
- Vernon, L.T.; Teng, K.A.; Kaelber, D.C.; Heintschel, G.P.; Nelson, S. Time to integrate oral health screening into medicine? A survey of primary care providers of older adults and an evidence-based rationale for integration. Gerodontology 2021. [Google Scholar] [CrossRef]
- Guan, G.; Lau, J.; Yew, V.; Jiayun, U.; Qu, W.; Lam, J.; Mei, L. Referrals by general dental practitioners and medical practitioners to oral medicine specialists in New Zealand: A study to develop protocol guidelines. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 130, 43–51.e5. [Google Scholar] [CrossRef] [PubMed]
- Sardella, A.; Demarosi, F.; Lodi, G.; Canegallo, L.; Rimondini, L.; Carrassi, A. Accuracy of Referrals to a Specialist Oral Medicine Unit by General Medical and Dental Practitioners and the Educational Implications. J. Dent. Educ. 2007, 71, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Westhausen, A.M.; Bornstein, M.M. Orale Medizin: Interdisziplinäre Zusammenarbeit zwischen Medizin und Zahnmedizin [Oral medicine: A specialty placed between medicine and dentistry]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2011, 54, 1061–1065. [Google Scholar] [CrossRef]
- Benoliel, R.; May, A.; Svensson, P. International Classification of Orofacial Pain, 1st edition (ICOP). Cephalalgia 2020, 40, 129–221. [Google Scholar]
- Freilich, J.E.; Kuten-Shorrer, M.; Treister, N.S.; Woo, S.-B.; Villa, A. Burning mouth syndrome: A diagnostic challenge. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 129, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Klasser, G.D.; Epstein, J.B.; Villines, D.; Utsman, R. Burning mouth syndrome: A challenge for dental practitioners and patients. Gen. Dent. 2011, 59, 210–220. [Google Scholar] [PubMed]
- Mignogna, M.D.; Fedele, S.; Russo, L.L.; Leuci, S.; Muzio, L.L. The diagnosis of burning mouth syndrome represents a challenge for clinicians. J. Orofac. Pain 2005, 19, 168–173. [Google Scholar]
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Criqui, M.H. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar]
- Colloca, L.; Ludman, T.; Bouhassira, D.; Baron, R.; Dickenson, A.H.; Yarnitsky, D.; Freeman, R.; Truini, A.; Attal, N.; Finnerup, N.B.; et al. Neuropathic pain. Nature reviews. Dis. Primers 2017, 3, 17002. [Google Scholar] [CrossRef] [PubMed]
- Crocetto, F.; Coppola, N.; Barone, B.; Leuci, S.; Imbimbo, C.; Mignogna, M.D. The association between burning mouth syndrome and urologic chronic pelvic pain syndrome: A case-control study. J. Oral Pathol. Med. 2020, 49, 829–834. [Google Scholar] [CrossRef]
- Aslam, A.; Hamburger, J. Does the use of photography help to prioritise patients when referring to the oral medicine department? Br. Dent. J. 2010, 208, E16. [Google Scholar] [CrossRef]
- Petruzzi, M.; De Benedittis, M. WhatsApp: A telemedicine platform for facilitating remote oral medicine consultation and improving clinical examinations. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 121, 248–254. [Google Scholar] [CrossRef]
- Pentapati, K.C.; Smriti, K.; Gadicherla, S. WhatsApp: A telemedicine platform for facilitating remote oral medicine consultation and improving clinical examinations—a commentary. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 121, 573. [Google Scholar] [CrossRef][Green Version]
- Carrard, V.C.; Martins, M.A.T.; Molina-Bastos, C.G.; Gonçalves, M.R. WhatsApp: A telemedicine platform for facilitating remote oral medicine consultation and improving clinical examinations—some considerations. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 123, 408. [Google Scholar] [CrossRef] [PubMed][Green Version]
| N | (%) | |
|---|---|---|
| All patients | 583 | |
| Age, mean years ± SD | 56.6 ± 16.2 | |
| Gender | ||
| Male | 218 | 37.4 |
| Female | 365 | 62.6 |
| Risk factor | ||
| Smoking status | ||
| Never | 308 | 52.8 |
| <5 | 120 | 20.6 |
| 5–15 | 113 | 19.4 |
| >15 | 42 | 7.2 |
| Alcohol use | ||
| Never | 215 | 36.9 |
| Light drinker | 219 | 37.6 |
| Moderate drinker | 127 | 21.8 |
| Heavy drinker | 22 | 3.8 |
| Diagnostic Test | N |
|---|---|
| Blood examination | 80 |
| Biopsy | 56 |
| Orthopantomogram | 53 |
| Lingual swab | 42 |
| Computed tomography maxillo-facial | 26 |
| Gastroscopy | 10 |
| Maxillo-facial MRI | 8 |
| Brain MRI | 6 |
| General urine test | 2 |
| Others | 25 |
| Disease | N | (%) |
|---|---|---|
| Immune-mediated mucosal conditions | 231 | 39.6 |
| Oral lichen planus | 164 | 28.1 |
| Orofacial granulomatosis | 29 | 5 |
| Recurrent aphthous | 19 | 3.3 |
| Geographic tongue | 18 | 3.1 |
| Pemphigus disease | 13 | 2.2 |
| Plasma cell mucositis | 6 | 1 |
| Pemphigoid disease | 4 | 0.7 |
| Erythema multiforme | 3 | 0.5 |
| Behcet’s disease | 1 | 0.2 |
| Orofacial pain disorders | 147 | 25.2 |
| Burning mouth syndrome | 111 | 19 |
| Persistent idiopathic facial pain | 30 | 5.1 |
| Trigeminal neuralgia | 4 | 0.7 |
| Myofascial pain | 1 | 0.2 |
| Globus pharyngeus | 1 | 0.2 |
| Benign tumors or neoplasms | 32 | 5.5 |
| Fibroma | 20 | 3.4 |
| HPV-related lesions | 8 | 1.4 |
| Peripheral giant cell granuloma | 2 | 0.3 |
| Lipoma | 1 | 0.2 |
| Varix | 1 | 0.2 |
| Dysplasia and cancerous conditions | 81 | 13.9 |
| Leukoplakia | 51 | 8.7 |
| Oral carcinoma | 27 | 4.6 |
| Erythroplakia | 3 | 0.5 |
| Reactive keratosis | 12 | 2 |
| Salivary gland disorders | 11 | 1.9 |
| Sjogren’s syndrome | 6 | 1 |
| Mucocele | 3 | 0.5 |
| Sialadenitis | 5 | 0.9 |
| Infections (Oral candidiasis) | 15 | 2.6 |
| Osteonecrosis of the jaws | 13 | 2.2 |
| Other mucosal and gingival lesions | 22 | 3.8 |
| Others * | 16 | 2.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coppola, N.; Baldares, S.; Blasi, A.; Bucci, R.; Spagnuolo, G.; Mignogna, M.D.; Leuci, S. Referral Patterns in Oral Medicine: A Retrospective Analysis of an Oral Medicine University Center in Southern Italy. Int. J. Environ. Res. Public Health 2021, 18, 12161. https://doi.org/10.3390/ijerph182212161
Coppola N, Baldares S, Blasi A, Bucci R, Spagnuolo G, Mignogna MD, Leuci S. Referral Patterns in Oral Medicine: A Retrospective Analysis of an Oral Medicine University Center in Southern Italy. International Journal of Environmental Research and Public Health. 2021; 18(22):12161. https://doi.org/10.3390/ijerph182212161
Chicago/Turabian StyleCoppola, Noemi, Stefania Baldares, Andrea Blasi, Rosaria Bucci, Gianrico Spagnuolo, Michele Davide Mignogna, and Stefania Leuci. 2021. "Referral Patterns in Oral Medicine: A Retrospective Analysis of an Oral Medicine University Center in Southern Italy" International Journal of Environmental Research and Public Health 18, no. 22: 12161. https://doi.org/10.3390/ijerph182212161
APA StyleCoppola, N., Baldares, S., Blasi, A., Bucci, R., Spagnuolo, G., Mignogna, M. D., & Leuci, S. (2021). Referral Patterns in Oral Medicine: A Retrospective Analysis of an Oral Medicine University Center in Southern Italy. International Journal of Environmental Research and Public Health, 18(22), 12161. https://doi.org/10.3390/ijerph182212161









