The Magnitude and Directions of the Associations between Early Life Factors and Metabolic Syndrome Differ across Geographical Locations among Migrant and Non-Migrant Ghanaians—The RODAM Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Recruitment Procedures
2.2. Eligibility
2.3. Data Collection
2.4. Metabolic Syndrome (MetSyn)
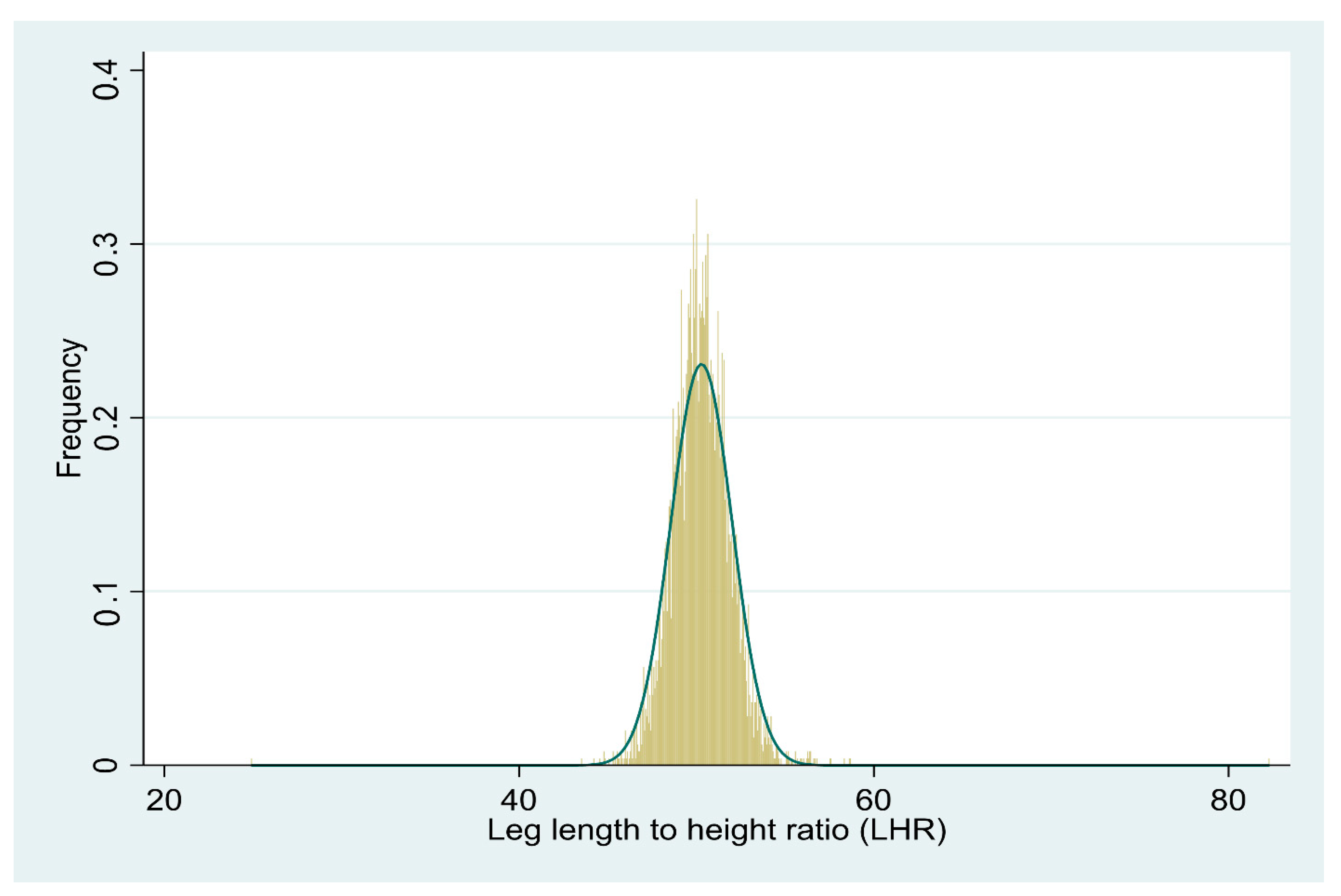
2.5. Early-Life Factors (ELFs)
2.6. Data Analysis
3. Results
3.1. Study Population
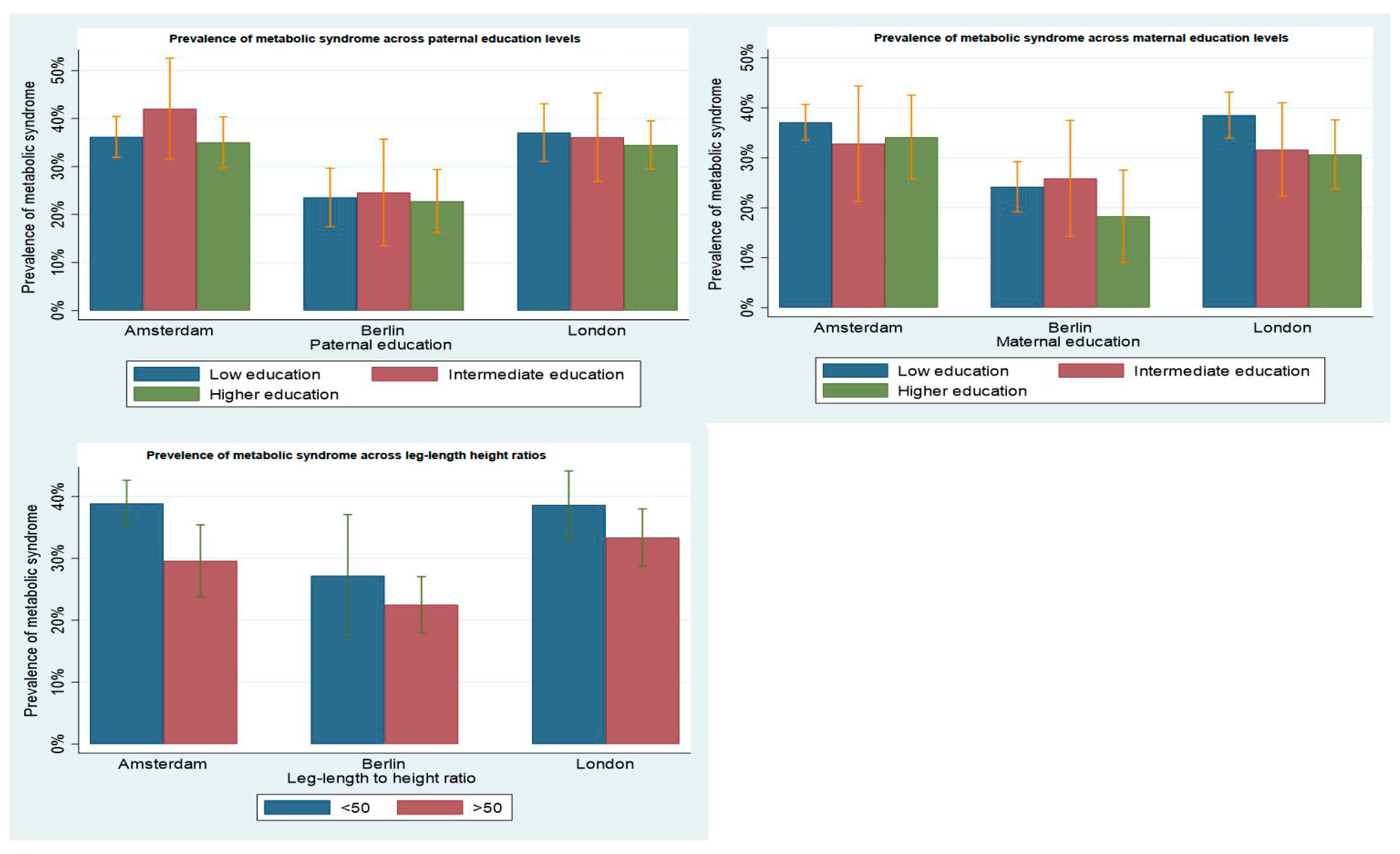
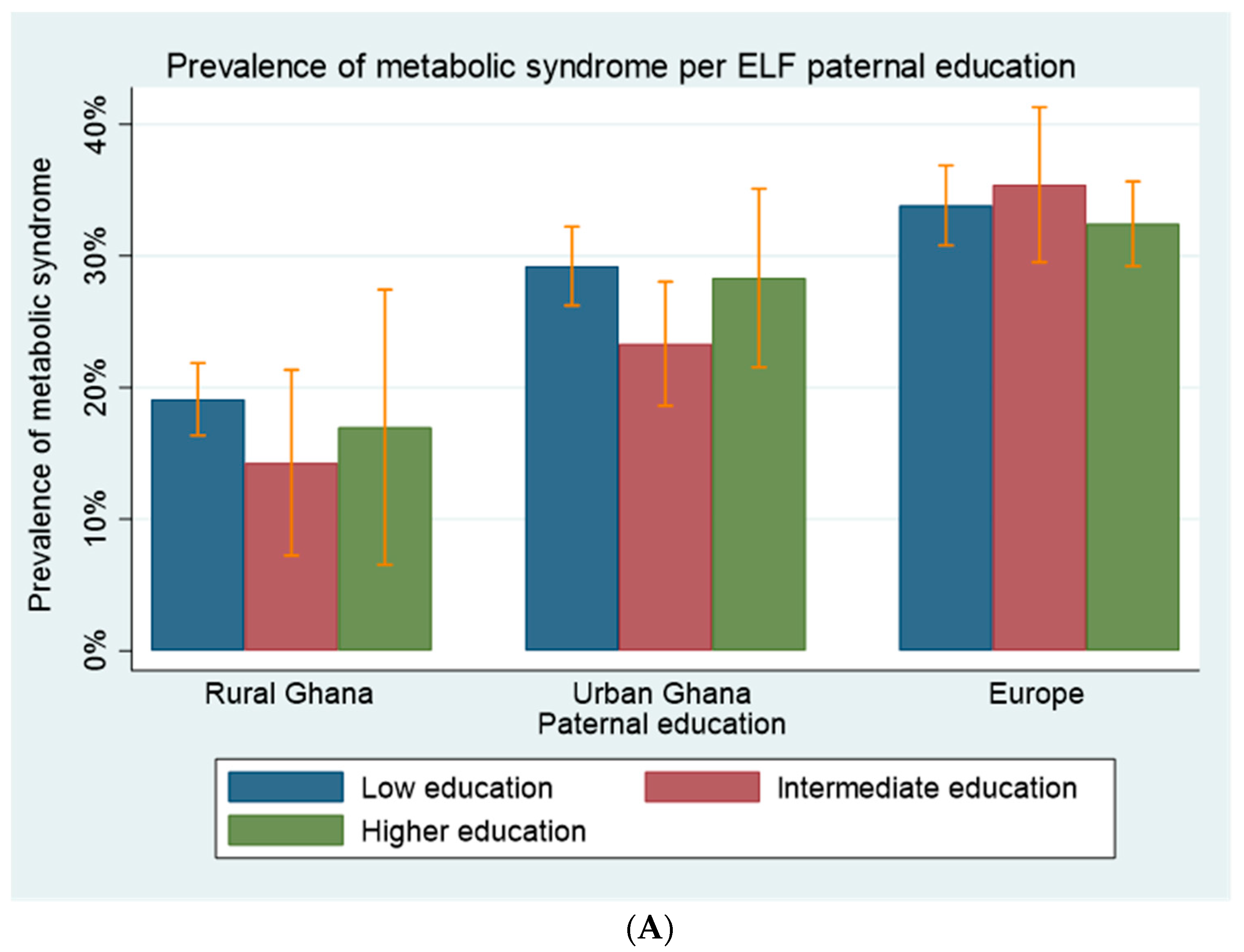
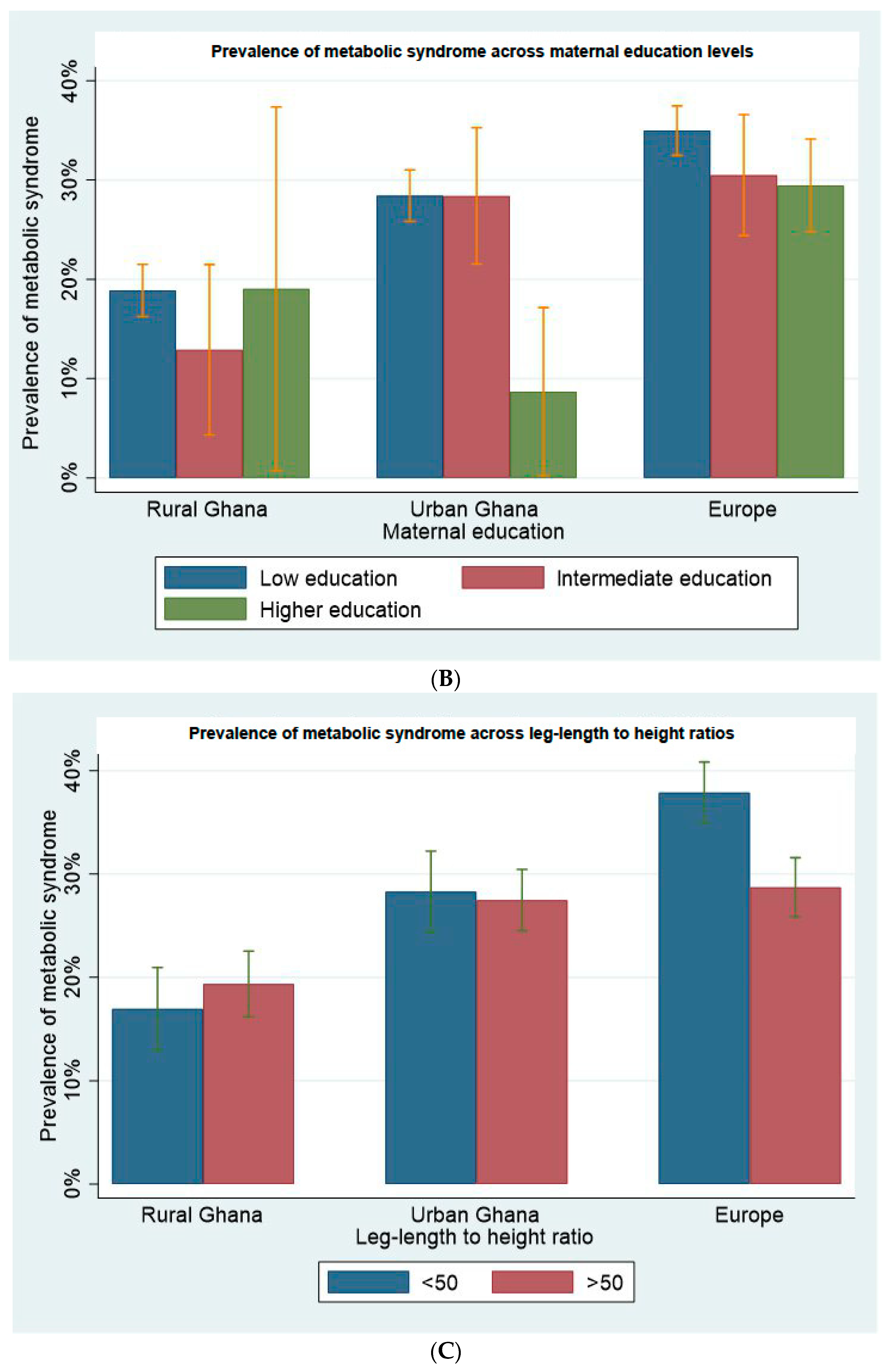
3.2. Proportions of MetSyn by Context across ELFs
3.3. Associations between ELFs and MetSyn
3.4. Stratified Analysis by Site in Europe
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ELFs | Early life factors |
| MetSyn | Metabolic syndrome |
| RODAM | Research on Obesity and Diabetes Among Migrants |
| HDL-cholesterol | High-density lipoprotein cholesterol |
| LDL-Cholesterol | Low-density lipoprotein cholesterol |
| AOR | Adjusted odds ratio |
Appendix A
Appendix B
Appendix C
| Variable | Amsterdam Ghanaians, OR (95% CI) | Berlin Ghanaians, OR(95% CI) | London Ghanaians, OR(95% CI) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | % MetSyn | Model 0 a | Model 1 b | Model 2 c | n (%) | % MetSyn | Model 0 a | Model 1 b | Model 2 c | n (%) | % MetSyn | Model 0 a | Model 1 b | Model 2 c | |
| Paternal education | |||||||||||||||
| Lower educataion | 492 (55.22) | 36.17 | 1.05 (0.78–1.41) | 0.88 (0.63–1.24) | 0.93 (0.66–1.32) | 191 (46.59) | 23.56 | 1.04 (0.63–1.72) | 0.60 (0.33–1.06) | 0.59 (0.33–1.06) | 251 (35.50) | 37.05 | 1.12 (0.80–1.57) | 0.70 (0.47–1.03) | 0.67 (0.44–1.00) |
| Intermediate education | 88 (9.88) | 42.05 | 1.34 (0.83–2.18) | 1.40 (0.84–2.35) | 1.22 (0.72–2.10) | 61 (14.88) | 24.59 | 1.11 (0.55–2.21) | 0.90 (0.43–1.87) | 0.89 (0.43–1.85) | 108 (15.28) | 36.11 | 1.07 (0.68–1.69) | 0.79 (0.48–1.29) | 0.74 (0.45–1.25) |
| Higher eduaction | 311 (34.90) | 35.05 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 158 (38.53) | 22.78 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 348 (49.22) | 34.48 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Maternal education | |||||||||||||||
| Lower educataion | 698 (78.34) | 37.11 | 1.14 (0.76–1.70) | 0.76 (0.48–1.19) | 0.78 (0.49–1.24) | 281 (68.54) | 24.20 | 1.42 (0.74–2.76) | 0.94 (0.45–1.95) | 0.97 (0.47–2.01) | 436 (61.67) | 38.53 | 1.42 (0.97–2.06) | 0.79 (0.51–1.22) | 0.80 (0.50–1.28) |
| Intermediate education | 67 (7.52) | 32.84 | 0.94 (0.50–1.77) | 0.84 (0.43–1.64) | 0.82 (0.41–1.63) | 58 (14.15) | 25.86 | 1.55 (0.67–3.61) | 1.74 (0.71–4.27) | 1.80 (0.73–4.43) | 98 (13.86) | 31.63 | 1.05 (0.61–1.79) | 0.87 (0.49–1.55) | 0.94 (0.52–1.70) |
| Higher eduaction | 126 (14.14) | 34.13 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 71 (17.31) | 18.31 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 173 (24.47) | 30.63 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Leg-Length to Height ratio (standardized values) | |||||||||||||||
| Leg-Length to Height ratio | 891 (100) | 36.36 | 0.88 (0.74–1.04) | 0.81 (0.67–0.97) | 0.86 (0.73–0.99) | 410 (100) | 23.41 | 1.00 (0.77–1.28) | 0.94 (0.72–1.24) | 0.95 (0.74–1.22) | 707 (100) | 35.64 | 0.99 (0.84–1.16) | 0.91 (0.76–1.09) | 0.96 (0.81–1.15) |
References
- Amuna, P.; Zotor, F.B. Epidemiological and nutrition transition in developing countries: Impact on human health and development. Proc. Nutr. Soc. 2008, 67, 82–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagner, K.H.; Brath, H. A global view on the development of non communicable diseases. Prev. Med. 2012, 54, S38–S41. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the Metabolic Syndrome. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [Green Version]
- Faijer-Westerink, H.J.; Kengne, A.P.; Meeks, K.A.C.; Agyemang, C. Prevalence of metabolic syndrome in sub-Saharan Africa: A systematic review and meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 547–565. [Google Scholar] [CrossRef]
- Van Der Linden, E.L.; Meeks, K.; Beune, E.; de-Graft Aikins, A.; Addo, J.; Owusu-Dabo, E.; Mockenhaupt, F.P.; Bahendeka, S.; Danquah, I.; Schulze, M.B.; et al. The prevalence of metabolic syndrome among Ghanaian migrants and their homeland counterparts: The Research on Obesity and type 2 Diabetes among African Migrants (RODAM) study. Eur. J. Public Health 2019, 29, 906–913. [Google Scholar] [CrossRef] [PubMed]
- Saklayen, M.G. The global epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akombi, B.J.; Agho, K.E.; Merom, D.; Renzaho, A.M.; Hall, J.J. Child malnutrition in sub-Saharan Africa: A meta-analysis of demographic and health surveys (2006–2016). PLoS ONE 2017, 12, e0177338. [Google Scholar] [CrossRef] [Green Version]
- Watkins, K.; Quattri, M. Child Poverty, Inequality and Demography Why Sub-Saharan Africa Matters for the Sustainable Development Goals; ODI-Overseas Development Institute: London, UK, 2016; Available online: https://www.refworld.org/docid/57c440364.html (accessed on 17 September 2021).
- Kuzawa, C.W.; Hallal, P.C.; Adair, L.; Bhargava, S.K.; Fall, C.H.; Lee, N.; Noris, S.A.; Osmond, C.; Ramirez-Zea, M.; Sachdev, H.S.; et al. Birth weight, postnatal weight gain, and adult body composition in five low and middle income countries. Am. J. Hum. Biol. 2012, 24, 5–13. [Google Scholar] [CrossRef] [Green Version]
- Norris, S.A.; Osmond, C.; Gigante, D.; Kuzawa, C.W.; Ramakrishnan, L.; Lee, N.R.; Ramirez-Zea, M.; Richter, L.M.; Stein, A.D.; Tandon, N.; et al. Size at birth, weight gain in infancy and childhood, and adult diabetes risk in five low- or middle-income country birth cohorts. Diabetes Care 2012, 35, 72–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poulton, R.; Caspi, A.; Milne, B.J.; Thomson, W.M.; Taylor, A.; Sears, M.R.; Moffitt, T.E. Association between children’s experience of socioeconomic disadvantage and adult health: A life-course study. Lancet 2002, 360, 1640–1645. [Google Scholar] [CrossRef] [Green Version]
- Hanson, M.A.; Gluckman, P.D. Early developmental conditioning of later health and disease: Physiology or pathophysiology? Physiol. Rev. 2014, 94, 1027–1076. [Google Scholar] [CrossRef]
- Jelenkovic, A.; Sund, R.; Hur, Y.M.; Yokoyama, Y.; Hjelmborg, J.V.B.; Möller, S.; Honda, C.; Magnusson, P.K.E.; Pedersen, N.L.; Ooki, S.; et al. Genetic and environmental influences on height from infancy to early adulthood: An individual-based pooled analysis of 45 twin cohorts. Sci. Rep. 2016, 6, 28496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bateson, P.; Gluckman, P.; Hanson, M. The biology of developmental plasticity and the Predictive Adaptive Response hypothesis. J. Physiol. 2014, 592, 2357–2368. [Google Scholar] [CrossRef]
- Munthali, R.J.; Kagura, J.; Lombard, Z.; Norris, S.A. Early life growth predictors of childhood adiposity trajectories and future risk for obesity: Birth to Twenty Cohort. Child. Obes. 2017, 13, 384–391. [Google Scholar] [CrossRef]
- Agyemang, C.; Beune, E.; Meeks, K.; Owusu-Dabo, E.; Agyei-Baffour, P.; de-Graft Aikins, A.; Dodoo, F.; Smeeth, L.; Addo, J.; Mockenhaupt, F.P.; et al. Rationale and cross-sectional study design of the research on obesity and type 2 diabetes among African migrants: The RODAM study. BMJ Open 2014, 4, e004877. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boateng, D.; Danquah, I.; Said-Mohamed, R.; Smeeth, L.; Nicolaou, M.; Meeks, K.; Beune, E.; Addo, J.; Bahendeka, S.; Agyei-Baffour, P.; et al. Early-life exposures and cardiovascular disease risk among Ghanaian migrant and home populations: The RODAM study. J. Dev. Orig. Health Dis. 2020, 11, 250–263. [Google Scholar] [CrossRef] [Green Version]
- Danquah, I.; Addo, J.; Boateng, D.; Klipstein-Grobusch, K.; Meeks, K.; Galbete, C.; Beune, E.; Bahendeka, S.; Spranger, J.; Mockenhaupt, F.P.; et al. Early-life factors are associated with waist circumference and type 2 diabetes among Ghanaian adults: The RODAM Study. Sci. Rep. 2019, 9, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bogin, B.; Varela-Silva, M.I. Leg length, body proportion, and health: A review with a note on beauty. Int. J. Environ. Res. Public Health 2010, 7, 1047–1075. [Google Scholar] [CrossRef] [Green Version]
- Johnston, L.W.; Harris, S.B.; Retnakaran, R.; Gerstein, H.C.; Zinman, B.; Hamilton, J.; Hanley, A. Short leg length, a marker of early childhood deprivation, is associated with metabolic disorders underlying type 2 diabetes: The PROMISE cohort study. Diabetes Care 2013, 36, 3599–3606. [Google Scholar] [CrossRef] [Green Version]
- Wadsworth, M.; Hardy, R.; Paul, A.; Marshall, S.; Cole, T. Leg and trunk length at 43 years in relation to childhood health, diet and family circumstances; evidence from the 1946 national birth cohort. Int. J. Epidemiol. 2002, 31, 383–390. [Google Scholar] [CrossRef]
- Said-Mohamed, R.; Prioreschi, A.; Nyati, L.H.; van Heerden, A.; Munthali, R.J.; Kahn, K.; Tollman, S.M.; Gómez-Olivé, F.X.; Houle, B.; Dunger, D.B.; et al. Rural–urban variations in age at menarche, adult height, leg-length and abdominal adiposity in black South African women in transitioning South Africa. Ann. Hum. Biol. 2018, 45, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Pryzbek, M.; Liu, J. Association between upper leg length and metabolic syndrome among US elderly participants results from the NHANES (2009–2010). J. Geriatr. Cardiol. 2016, 13, 58–63. [Google Scholar] [CrossRef]
- Mueller, N.T.; Pereira, M.A. Leg length and type 2 diabetes: What’s the link? Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 452–456. [Google Scholar] [CrossRef] [Green Version]
- Vilar-Compte, M.; Macinko, J.; Weitzman, B.C.; Avendaño-Villela, C.M. Short relative leg length is associated with overweight and obesity in Mexican immigrant women. Int. J. Equity Health 2019, 18, 103. [Google Scholar] [CrossRef] [Green Version]
- Vafeiadi, M.; Myridakis, A.; Roumeliotaki, T.; Margetaki, K.; Chalkiadaki, G.; Dermitzaki, E.; Venihaki, M.; Sarri, K.; Vassilaki, M.; Leventakou, V.; et al. Association of early life exposure to phthalates with obesity and cardiometabolic traits in childhood: Sex specific associations. Front. Public Health 2018, 6, 327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McIntyre, M.H. Adult stature, body proportions and age at menarche in the United States National Health and Nutrition Survey (NHANES) III. Ann. Hum. Biol. 2011, 38, 716–720. [Google Scholar] [CrossRef]
- Lawlor, D.; Ebrahim, S.; Smith, G.D. The association between components of adult height and type II diabetes and insulin resistance: British Women’s Heart and Health Study. Diabetologia 2002, 45, 1097–1106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Rooij, S.R.; Painter, R.C.; Holleman, F.; Bossuyt, P.M.; Roseboom, T.J. The metabolic syndrome in adults prenatally exposed to the Dutch famine. Am. J. Clin. Nutr. 2007, 86, 1219–1224. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Jaddoe, V.W.; Qi, L.; He, Y.; Wang, D.; Lai, J.; Zhang, J.; Fu, P.; Yang, X.; Hu, F.B. Exposure to the Chinese famine in early life and the risk of metabolic syndrome in adulthood. Diabetes Care 2011, 34, 1014–1018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marciniak, A.; Patro-Małysza, J.; Kimber-Trojnar, Ż.; Marciniak, B.; Oleszczuk, J.; Leszczyńska-Gorzelak, B. Fetal programming of the metabolic syndrome. Taiwan. J. Obstet. Gynecol. 2017, 56, 133–138. [Google Scholar] [CrossRef]
- Gluckman, P.; Hanson, M. Mismatch: Why Our World No Longer Fits Our Bodies; Oxford University Press: New York, NY, USA, 2006. [Google Scholar]
- Tan, C.M.; Rockmore, M. Famine in Ghana and Its Impact. Handb. Famine Starvation Nutr. Deprivation 2019, 1, 31–45. [Google Scholar] [CrossRef]
- Masih, I.; Maskey, S.; Mussá, F.E.F.; Trambauer, P. A review of droughts on the African continent: A geospatial and long-term perspective. Hydrol. Earth Syst. Sci. 2014, 18, 3635–3649. [Google Scholar] [CrossRef] [Green Version]
- van Dijk, A.M.; Dingerink, S.; Chilunga, F.P.; Meeks, K.A.; Bahendeka, S.; Schulze, M.B.; Danquah, I.; Osei, T.B.; Serné, E.; Agyemang, C.; et al. Metabolic-associated fatty liver disease as assessed by the Fatty Liver Index among migrant and non-migrant Ghanaian populations. J. Clin. Transl. Hepatol. 2021, 9, 494–502. [Google Scholar] [CrossRef]
- Katsiki, N.; Perez-Martinez, P.; Anagnostis, P.; Mikhailidis, D.P.; Karagiannis, A. Is nonalcoholic fatty liver disease indeed the hepatic manifestation of metabolic syndrome? Curr. Vasc. Pharmacol. 2018, 16, 219–227. [Google Scholar] [CrossRef]
- Young, F.; Critchley, J.A.; Johnstone, L.K.; Unwin, N.C. A review of co-morbidity between infectious and chronic disease in Sub Saharan Africa: TB and diabetes mellitus, HIV and metabolic syndrome, and the impact of globalization. Glob. Health 2009, 5, 1–9. [Google Scholar] [CrossRef] [Green Version]
- DeBoer, M.D.; Lima, A.A.; Oría, R.B.; Scharf, R.J.; Moore, S.R.; Luna, M.A.; Guerrant, R.L. Early childhood growth failure and the developmental origins of adult disease: Do enteric infections and malnutrition increase risk for the metabolic syndrome? Nutr. Rev. 2012, 70, 642–653. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, K.; Sakuraya, A.; Kawakami, N.; Imamura, K.; Ando, E.; Asai, Y.; Eguchi, H.; Kobayashi, Y.; Nishida, N.; Arima, H.; et al. Work-related psychosocial factors and metabolic syndrome onset among workers: A systematic review and meta-analysis. Obes. Rev. 2018, 19, 1557–1568. [Google Scholar] [CrossRef]
- Cohen, S.; Janicki-Deverts, D.; Chen, E.; Matthews, K.A. Childhood socioeconomic status and adult health. Ann. New York Acad. Sci. 2010, 1186, 37–55. [Google Scholar] [CrossRef]
- Galobardes, B.; Shaw, M.; Lawlor, D.A.; Lynch, J.W.; Smith, G.D. Indicators of socioeconomic position (part 1). J. Epidemiol. Community Health 2006, 60, 7–12. [Google Scholar] [CrossRef] [Green Version]
- Njelekela, M.A.; Liu, E.; Mpembeni, R.; Muhihi, A.; Mligiliche, N.; Spiegelman, D.; Finkelstein, J.L.; Fawzi, W.W.; Willett, W.C.; Mtabaji, J. Socio-economic status, urbanization, and cardiometabolic risk factors among middle-aged adults in Tanzania. East Afr. J. Public Health 2011, 8, 216–223. [Google Scholar]
- Adedoyin, R.A.; Afolabi, A.; Adegoke, O.O.; Akintomide, A.O.; Awotidebe, T.O. Relationship between socioeconomic status and metabolic syndrome among Nigerian adults. Diabetes Metab. Syndr. Clin. Res. Rev. 2013, 7, 91–94. [Google Scholar] [CrossRef]
- Adler, N.E.; Newman, K. Socioeconomic Disparities In Health: Pathways And Policies Inequality in education, income, and occupation exacerbates the gaps between the health ‘haves’ and ‘have-nots’. In Carrots, Sticks and Sermons: Policy Instruments and Their Evaluation; Transaction Publishers: Piscataway, NJ, USA, 2020. [Google Scholar]
- Agyemang, C.; van Valkengoed, I.; Hosper, K.; Nicolaou, M.; van den Born, B.-J.; Stronks, K. Educational inequalities in metabolic syndrome vary by ethnic group: Evidence from the SUNSET study. Int. J. Cardiol. 2009, 141, 266–274. [Google Scholar] [CrossRef]
- Güneş, P.M. The role of maternal education in child health: Evidence from a compulsory schooling law. Econ. Educ. Rev. 2015, 47, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Matias, T.S.; Silva, K.S.; da Silva, J.A.; de Mello, G.T.; Salmon, J. Clustering of diet, physical activity and sedentary behavior among Brazilian adolescents in the national school-based health survey (PeNSE 2015). BMC Public Health 2018, 18, 1283. [Google Scholar] [CrossRef]
- Dzramedo, J.E.; Amoako, B.M.; Amos, P.M. The state of the extended family system in Ghana: Perceptions of some families. Res. Humanit. Soc. Sci. 2018, 8, 24. [Google Scholar]
| Risk Factor | Participant Has Risk Factor Yes/No |
|---|---|
| Elevated triglycerides | ≥150 mg/dL (1.7 mmol/L) or receiving treatment for risk factor |
| Reduced high-density lipid cholesterol | <40 mg/dL (1.0 mmol/L) in males; <50 mg/dL (1.3 mmol/L) in females or receiving treatment for risk factor |
| Elevated blood pressure | Systolic ≥ 130 and/or diastolic ≥ 85 mmHg or receiving treatment for risk factor |
| Elevated fasting glucose plasma | ≥100 mg/dL or receiving treatment for risk factor |
| Increased waist circumference for Sub-Saharan Africans 1 | Males ≥ 94 cm; Females ≥ 80 cm |
| Rural Ghanaians | Urban Ghanaians | Migrant Ghanaians | p-Value 6 | |
|---|---|---|---|---|
| Numbers enrolled, n (%) | 941 (21.74) | 1379 (31.86) | 2008 (46.39) | |
| Women, n (%) | 575 (61.10) | 991 (71.86) | 1162 (57.87) | <0.001 |
| Age in years (mean ± SD) | 46.3 ± 12.6 | 45.3 ± 11.5 | 47.0 ± 9.7 | <0.001 |
| Education, n (%) | <0.001 | |||
| Never/elementary only | 539 (57.28%) | 603 (43.73) | 434 (21.56) | |
| Lower vocational/secondary school | 296 (31.35) | 538 (39.01) | 750 (36.95) | |
| Higher vocational/secondary school | 72 (7.55) | 172 (12.47) | 479 (23.75) | |
| University | 35 (3.72) | 65 (4.71) | 341 (16.88) | |
| Metabolic syndrome, n (%) | 174 (18.49) | 383 (27.77) | 672 (33.47) | <0.001 |
| Systolic Blood Pressure, mmHg (median (IQR)) | 119.5 (110–133.5) | 123.5 (112.5–136) | 132.5 (122.75–144.5) | <0.001 |
| Hypertensive, n (%) | 275 (29.22) | 506 (36.69) | 1.161 (57.82) | <0.001 |
| BP medication, n (%) 1 | 127 (13.50) | 263 (19.07) | 695 (34.61) | <0.001 |
| Total cholesterol, mmol/L (mean ± SD) | 4.50 ± 1.13 | 5.21 ± 1.15 | 5.07 ± 1.07 | <0.001 |
| LDL cholesterol, mmol/L (mean ± SD) 2 | 2.79 ± 0.95 | 3.43 ± 0.99 | 3.23 ± 0.94 | <0.001 |
| HDLcholesterol, mmol/L (mean ± SD) 3 | 1.20 ± 0.38 | 1.26 ± 0.32 | 1.42 ± 0.34 | <0.001 |
| Cholesterol medication, n (%) | 17 (1.81) | 26 (1.89) | 277 (13.79) | <0.001 |
| Median tryglycerides, mmol/L | 0.98 (0.74–11.31) | 1.02 (0.74–1.35) | 0.79 (0.61–1.05) | <0.001 |
| Blood glucose, mmol/L | 4.91 (4.59–5.30) | 5.1 (4.77–5.46) | 5.09 (4.71–5.62) | <0.001 |
| Diabetes medication, n (%) | 23 (2.44) | 73 (5.29) | 164 (8.17) | <0.001 |
| Waist circumference,(mean ± SD) | 81.11 ± 10.76 | 89.26 ± 11.74 | 94.76 ± 11.66 | <0.001 |
| Abdominal obesity n (%) 4 | 184 (19.55) | 582 (42.20) | 1026 (51.10) | <0.001 |
| Height (mean ± SD) | 162.11 ± 8.57 | 161.74 ± 7.94 | 165.62 ± 7.99 | <0.001 |
| Leg length, (mean ± SD) | 82.17 ± 5.47 | 81.65 ± 5.48 | 82.81 ± 5.52 | <0.001 |
| Leg-length to height ratio (LLHR), (mean ± SD) | 0.51 ± 0.02 | 0.50 ± 0.02 | 0.50 ± -0.02 | <0.001 |
| Maternal Education, n (%) | <0.001 | |||
| Lower education | 858 (91.18) | 1164 (84.40) | 1415 (70.47) | |
| Intermediate education | 62 (6.59) | 169 (12.26) | 223 (11.11) | |
| Higher education | 21 (2.23) | 46 (3.34) | 370 (18.42) | |
| Paternal Education, n (%) | <0.001 | |||
| Lower education | 790 (83.95) | 893 (64.76) | 934 (46.51) | |
| Intermediate education | 98 (10.41) | 313 (22.69) | 257 (12.80) | |
| Higher education | 53 (5.63) | 173 (12.55) | 817 (40.69) | |
| Type 2 diabetes mellitus, n (%) | 49 (5.21) | 130 (9.43) | 235 (11.70) | <0.001 |
| Length of stay, (median (IQR)) | 16.38 (9.82–23.79) | N/A | ||
| Age of menarche (Female only), (mean ± SD) | 14.86 ± 1.95 | 14.83 ± 1.55 | 14.64 ± 1.81 | <0.001 |
| Smoking, n(%) | <0.001 | |||
| Current smoker | 20 (2.13) | 14 (1.02) | 72 (3.59) | |
| Former smoker | 62 (6.59) | 82 (5.95) | 150 (7.47) | |
| Alcohol-consumption, n(%) | <0.001 | |||
| No alcohol | 548 (58.24) | 955 (69.25) | 1134 (56.47) | |
| Alcohol | 393 (41.76) | 424 (30.75) | 874 (43.53) | |
| Total energy consumption per day (median (IQR)) | 2588.3 (2055.5–3374.6) | 2229.1 (1842.8–2697.3) | 2600.6 (1946.6–3520.3) | <0.001 |
| Physical Activity levels, n (%) | <0.001 | |||
| Unknown | 4 (0.43) | 12 (0.87) | 137 (6.82) | |
| Low | 173 (18.38) | 485 (35.17) | 530 (26.39) | |
| Moderate | 196 (20.83) | 229 (16.61) | 419 (20.87) | |
| High | 568 (60.36) | 653 (47.35) | 922 (45.92) | |
| BMI, n (%) 5 | <0.001 | |||
| <25 kg/m2 | 715 (75.98) | 555 (40.28) | 414 (20.63) | |
| 25–30 kg/m2 | 176 (18.70) | 467 (33.89) | 856 (42.65) | |
| ≥30 kg/m2 | 50 (5.31) | 356 (25.83) | 737 (36.72) | |
| Variable | Rural Ghanaians, OR (95% CI) | Urban Ghanaians, OR (95% CI) | Migrant Ghanaians, OR (95% CI) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | % MetSyn | Model 0 a | Model 1 b | Model 2 c | n (%) | % MetSyn | Model 0 a | Model 1 b | Model 2 c | n (%) | % MetSyn | Model 0 a | Model 1 b | Model 2 c | Model 3 d | |
| Paternal education | ||||||||||||||||
| Lower educataion | 790 (83.95) | 19.11 | 1.16 (0.55–2.42) | 0.61 (0.26–1.41) | 0.57 (0.25–1.33) | 893 (64.76) | 29.22 | 1.05 (0.73–1.50) | 0.75 (0.50–1.12) | 0.77 (0.51–1.16) | 934 (46.51) | 33.83 | 1.07 (0.87–1.30) | 0.76 (0.60–0.96) | 0.69 (0.53–0.90) | 0.71 (0.54–0.94) |
| Intermediate education | 98 (10.41) | 14.29 | 0.81 (0.33–2.03) | 0.69 (0.26–1.82) | 0.69 (0.26–1.85) | 313 (22.69) | 23.32 | 0.77 (0.50–1.17) | 0.69 (0.44–1.08) | 0.72 (0.46–1.13) | 257 (12.80) | 35.41 | 1.14 (0.85–1.53) | 0.97 (0.71–1.33) | 1.02 (0.70–1.47) | 0.96 (0.66–1.47) |
| Higher eduaction | 53 (5.63) | 16.98 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 173 (12.55) | 28.32 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 817 (40.69) | 32.44 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Maternal education | ||||||||||||||||
| Lower educataion | 858 (91.18) | 18.88 | 0.99 (0.33–2.98) | 0.55 (0.16–1.91) | 0.53 (0.15–1.88) | 1164 (84.40) | 28.43 | 4.17 (1.48–11.72) | 2.67 (0.92–7.78) | 2.70 (0.93–7.86) | 1415 (70.47) | 34.98 | 1.29 (1.00–1.65) | 0.79 (0.59–1.04) | 0.77 (0.55–1.06) | 0.79 (0.56–1.11) |
| Intermediate education | 62 (6.59) | 12.90 | 0.63 (0.17–2.35) | 0.61 (0.15–2.56) | 0.63 (0.15–1.68) | 169 (12.26) | 28.40 | 4.16 (1.42–12.25) | 4.49 (1.49–13.54) | 4.53 (1.50–3.74) | 223 (11.11) | 30.49 | 1.05 (0.73–1.51) | 0.94 (0.64–1.39) | 0.91 (0.58–1.43) | 0.96 (0.60–1.53) |
| Higher eduaction | 21 (2.23) | 19.05 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 46 (3.34) | 8.70 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 370 (18.42) | 29.46 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Leg-Length to Height ratio (standardized values) | ||||||||||||||||
| Leg-Length to Height ratio | 941 (100) | 18.49 | 1.12 (0.95–1.31) | 0.99 (0.84–1.18) | 1.00 (0.84–1.19) | 1379 (100) | 27.77 | 0.96 (0.85–1.08) | 0.92 (0.80–1.05) | 0.92 (0.80–1.06) | 2008 (100) | 33.47 | 0.87 (0.79–0.96) | 0.83 (0.75–0.92) | 0.88 (0.78–0.99) | 0.89 (0.79–1.01) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Heijden, T.G.W.; Chilunga, F.P.; Meeks, K.A.C.; Addo, J.; Danquah, I.; Beune, E.J.; Bahendeka, S.K.; Klipstein-Grobusch, K.; Mockenhaupt, F.P.; Waltz, M.M.; et al. The Magnitude and Directions of the Associations between Early Life Factors and Metabolic Syndrome Differ across Geographical Locations among Migrant and Non-Migrant Ghanaians—The RODAM Study. Int. J. Environ. Res. Public Health 2021, 18, 11996. https://doi.org/10.3390/ijerph182211996
van der Heijden TGW, Chilunga FP, Meeks KAC, Addo J, Danquah I, Beune EJ, Bahendeka SK, Klipstein-Grobusch K, Mockenhaupt FP, Waltz MM, et al. The Magnitude and Directions of the Associations between Early Life Factors and Metabolic Syndrome Differ across Geographical Locations among Migrant and Non-Migrant Ghanaians—The RODAM Study. International Journal of Environmental Research and Public Health. 2021; 18(22):11996. https://doi.org/10.3390/ijerph182211996
Chicago/Turabian Stylevan der Heijden, Thijs G. W., Felix P. Chilunga, Karlijn A. C. Meeks, Juliet Addo, Ina Danquah, Erik J. Beune, Silver K. Bahendeka, Kerstin Klipstein-Grobusch, Frank P. Mockenhaupt, Mitzi M. Waltz, and et al. 2021. "The Magnitude and Directions of the Associations between Early Life Factors and Metabolic Syndrome Differ across Geographical Locations among Migrant and Non-Migrant Ghanaians—The RODAM Study" International Journal of Environmental Research and Public Health 18, no. 22: 11996. https://doi.org/10.3390/ijerph182211996
APA Stylevan der Heijden, T. G. W., Chilunga, F. P., Meeks, K. A. C., Addo, J., Danquah, I., Beune, E. J., Bahendeka, S. K., Klipstein-Grobusch, K., Mockenhaupt, F. P., Waltz, M. M., & Agyemang, C. (2021). The Magnitude and Directions of the Associations between Early Life Factors and Metabolic Syndrome Differ across Geographical Locations among Migrant and Non-Migrant Ghanaians—The RODAM Study. International Journal of Environmental Research and Public Health, 18(22), 11996. https://doi.org/10.3390/ijerph182211996








