Loneliness and Mental Health: The Mediating Effect of Perceived Social Support
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Measures
2.3. Data Analysis
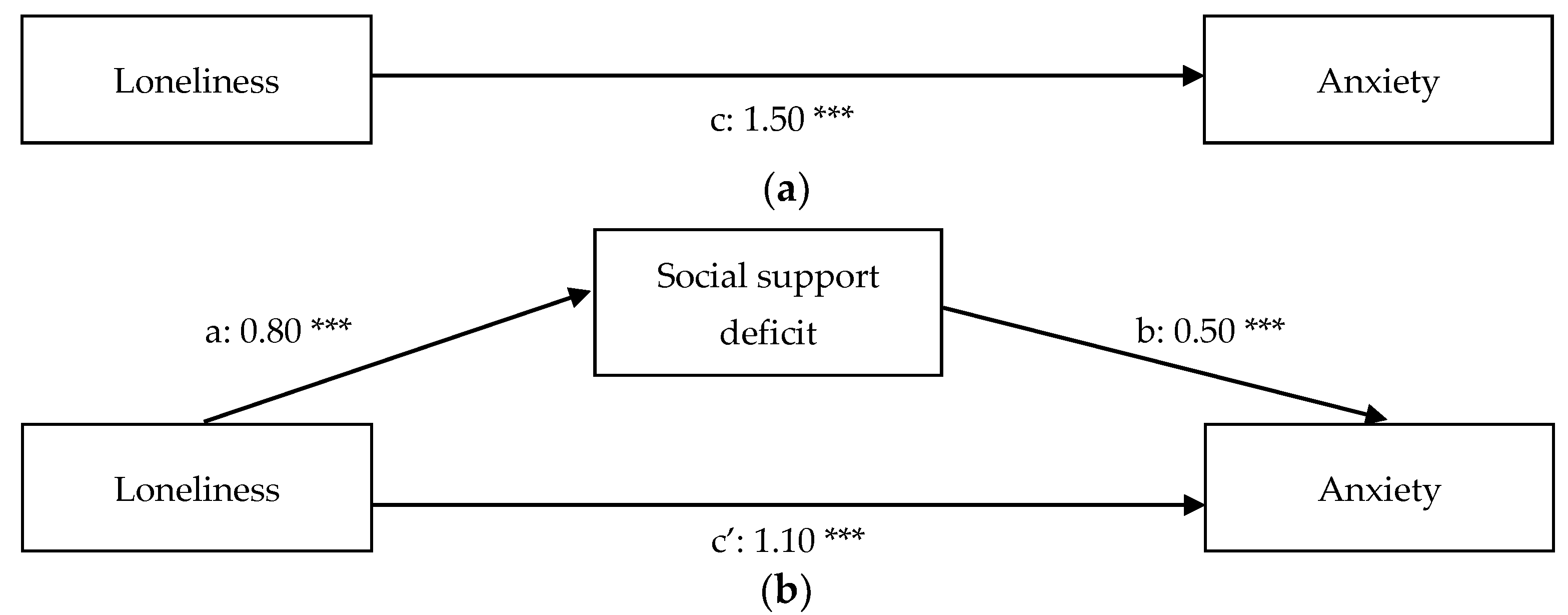
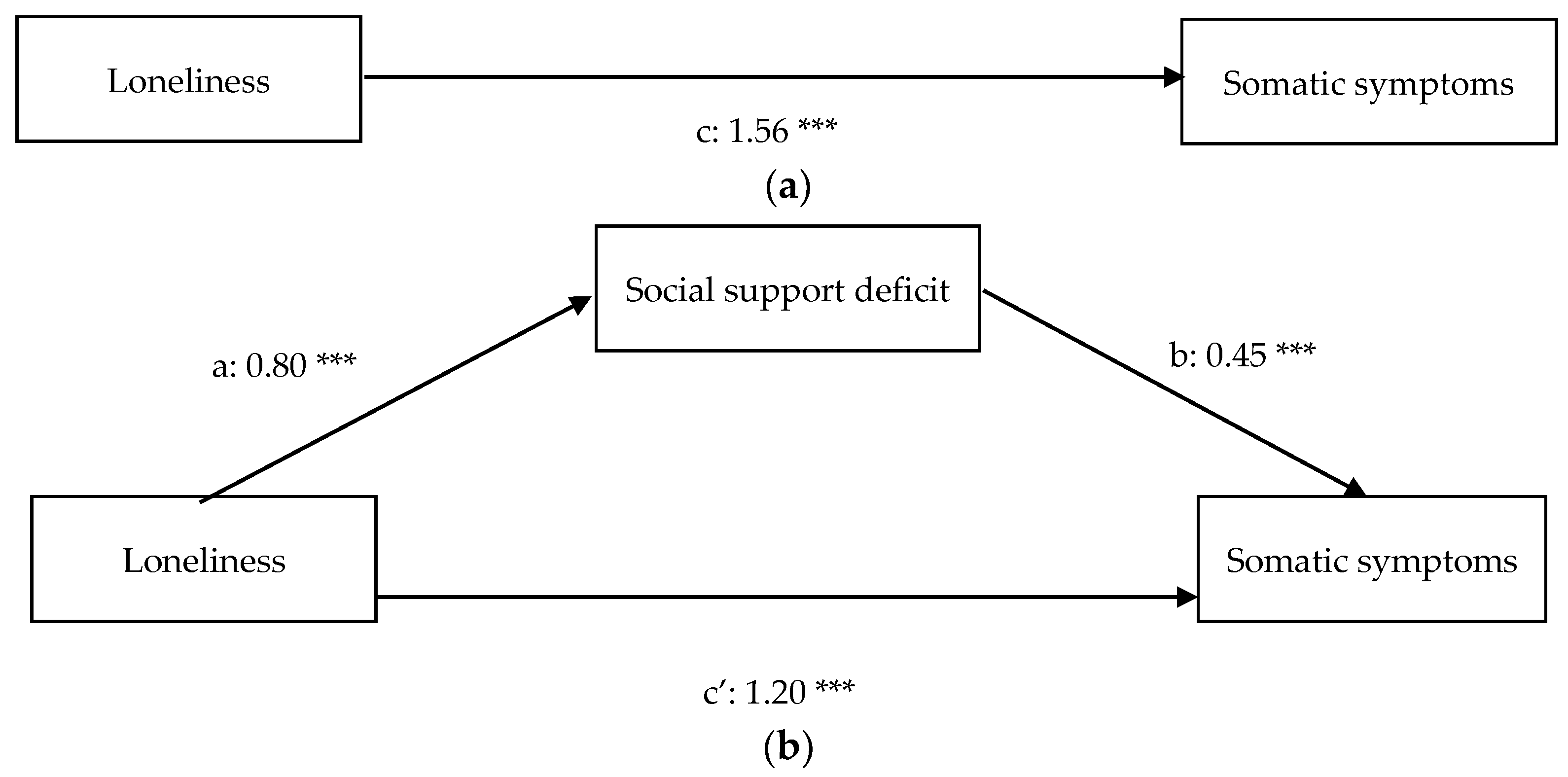
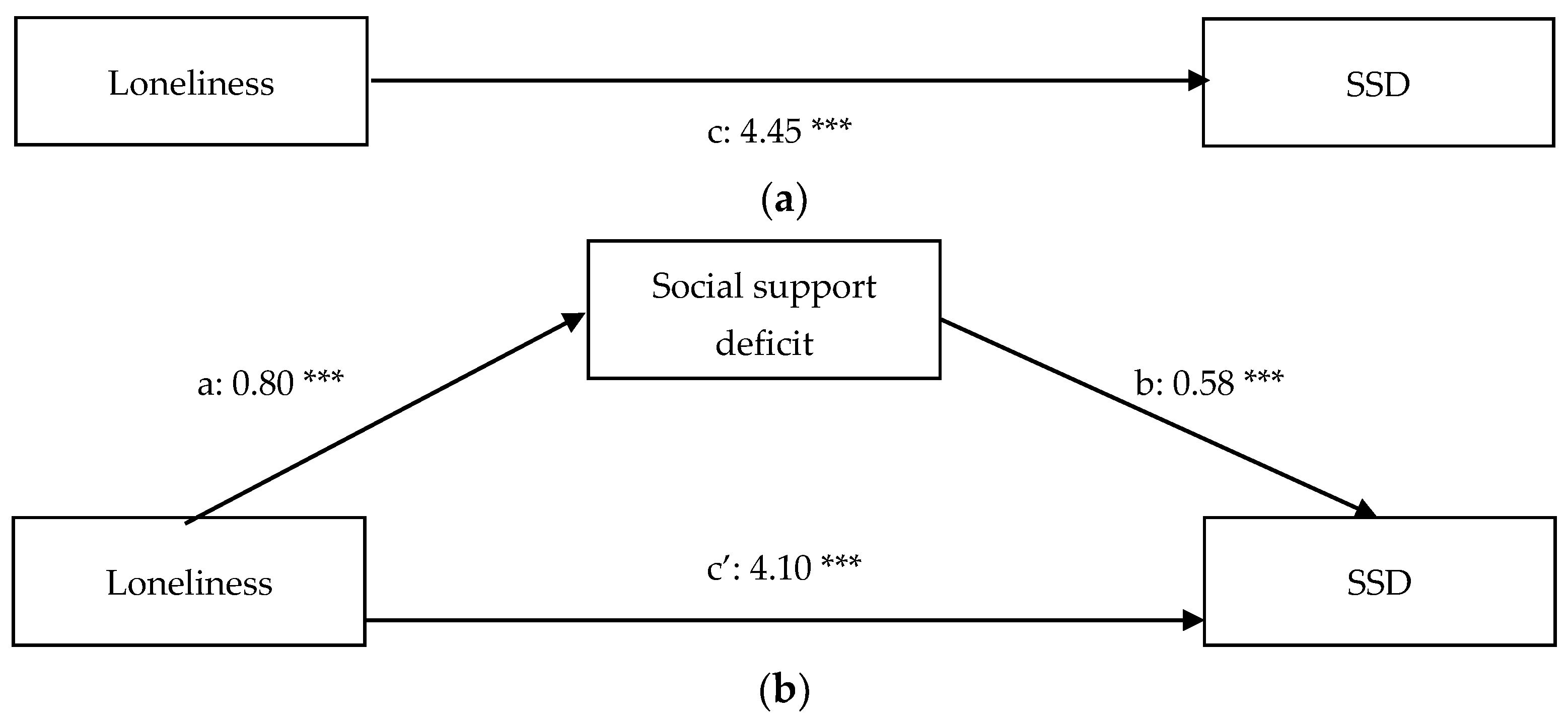
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baumeister, R.F.; Leary, M.R. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychol. Bull. 1995, 117, 497–529. [Google Scholar] [CrossRef]
- Perlman, D.; Peplau, L.A. Toward a social psychology of loneliness. Pers. Relatsh. 1981, 3, 31–56. [Google Scholar]
- Beutel, M.E.; Klein, E.M.; Brähler, E.; Reiner, I.; Jünger, C.; Michal, M.; Tibubos, A.N. Loneliness in the general population: Prevalence, determinants and relations to mental health. BMC Psychiatry 2017, 17, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, M.; Bonnici, J.; Azzopardi, A. Loneliness in Malta: Findings from the first National Prevalence Study. J. Soc. Pers. Relatsh. 2021, 38, 2751–2771. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Cacioppo, S. The growing problem of loneliness. Lancet 2018, 391, 426. [Google Scholar] [CrossRef] [Green Version]
- Groarke, J.M.; Berry, E.; Graham-Wisener, L.; McKenna-Plumley, P.E.; McGlinchey, E.; Armour, C. Loneliness in the UK during the COVID-19 pandemic: Cross-sectional results from the COVID-19 Psychological Wellbeing Study. Plos ONE 2020, 15, e0239698. [Google Scholar] [CrossRef] [PubMed]
- Victor, C.R.; Yang, K. The prevalence of loneliness among adults: A case study of the United Kingdom. J. Psychol. 2012, 146, 85–104. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef] [Green Version]
- Cacioppo, J.T.; Cacioppo, S. Loneliness in the modern age: An evolutionary theory of loneliness (etl). Adv. Exp. Soc. Psychol. 2018, 58, 127–197. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Patrick, W. Loneliness: Human Nature and the Need for Social Connection; WW Norton & Company: New York, NY, USA, 2008. [Google Scholar]
- Cacioppo, J.T.; Cacioppo, S.; Boomsma, D.I. Evolutionary mechanisms for loneliness. Cogn. Emot. 2014, 28, 3–21. [Google Scholar] [CrossRef]
- Silk, J.B. Ties that bond: The role of kinship in primate societies. In New Directions in Anthropological Kinship; Stone, L., Ed.; Rowman and Littlefield: Lanham, MD, USA, 2000; pp. 71–92. [Google Scholar]
- Cacioppo, J.T.; Hawkley, L.C. Perceived social isolation and cognition. Trends Cogn. Sci. 2009, 13, 447–454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, J.; Wang, X.; Wei, D.; Qiu, J. State loneliness is associated with emotional hypervigilance in daily life: A network analysis. Personal. Individ. Differ. 2020, 165, 110154. [Google Scholar] [CrossRef]
- Spithoven, A.W.M.; Cacioppo, S.; Goossens, L.; Cacioppo, J.T. Genetic contributions to loneliness and their relevance to the evolutionary theory of loneliness. Perspect. Psychol. Sci. 2019, 14, 376–396. [Google Scholar] [CrossRef] [PubMed]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef] [Green Version]
- Mushtaq, R.; Shoib, S.; Shah, T.; Mushtaq, S. Relationship between loneliness, psychiatric disorders and physical health? A review on the psychological aspects of loneliness. J. Clin. Diagn. Res. 2014, 8, WE01–WE04. [Google Scholar] [CrossRef]
- Nuyen, J.; Tuithof, M.; de Graaf, R.; Van Dorsselaer, S.; Kleinjan, M.; Have, M.T. The bidirectional relationship between loneliness and common mental disorders in adults: Findings from a longitudinal population-based cohort study. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 1297–1310. [Google Scholar] [CrossRef]
- Wang, J.; Mann, F.; Lloyd-Evans, B.; Ma, R.; Johnson, S. Associations between loneliness and perceived social support and outcomes of mental health problems: A systematic review. BMC Psychiatry 2018, 18, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Heinrich, L.M.; Gullone, E. The clinical significance of loneliness: A literature review. Clin. Psychol. Rev. 2006, 26, 695–718. [Google Scholar] [CrossRef] [PubMed]
- Sylvers, P.; Lilienfeld, S.O.; LaPrairie, J.L. Differences between trait fear and trait anxiety: Implications for psychopathology. Clin. Psychol. Rev. 2011, 31, 122–137. [Google Scholar] [CrossRef]
- Hutten, E.; Jongen, E.M.; Verboon, P.; Bos, A.E.; Smeekens, S.; Cillessen, A.H. Trajectories of loneliness and psychosocial functioning. Front. Psychol. 2021, 12, 2367. [Google Scholar] [CrossRef]
- Vanhalst, J.; Goossens, L.; Luyckx, K.; Scholte, R.H.; Engels, R.C. The development of loneliness from mid-to late adolescence: Trajectory classes, personality traits, and psychosocial functioning. J. Adolesc. 2013, 36, 1305–1312. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Mundó, J.; Haro, J.M.; Rubio-Valera, M. Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA). J. Affect. Disord. 2019, 246, 82–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dobson, K.S. The relationship between anxiety and depression. Clin. Psychol. Rev. 1985, 5, 307–324. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Qualter, P.; Brown, S.L.; Rotenberg, K.J.; Vanhalst, J.; Harris, R.A.; Goossens, L.; Munn, P. Trajectories of loneliness during childhood and adolescence: Predictors and health outcomes. J. Adolesc. 2013, 36, 1283–1293. [Google Scholar] [CrossRef] [PubMed]
- Schinka, K.C.; van Dulmen, M.H.; Mata, A.D.; Bossarte, R.; Swahn, M. Psychosocial predictors and outcomes of loneliness trajectories from childhood to early adolescence. J. Adolesc. 2013, 36, 1251–1260. [Google Scholar] [CrossRef] [PubMed]
- Grover, S.; Avasthi, A.; Sahoo, S.; Lakdawala, B.; Dan, A.; Nebhinani, N.; Suthar, N. Relationship of loneliness and social connectedness with depression in elderly: A multicentric study under the aegis of Indian Association for Geriatric Mental Health. J. Geriatr. Ment. Health 2018, 5, 99. [Google Scholar] [CrossRef]
- Kapfhammer, H.P. Somatic symptoms in depression. Dialogues Clin. Neurosci. 2006, 8, 227. [Google Scholar] [CrossRef] [PubMed]
- Dimsdale, J.E.; Creed, F.; Escobar, J.; Sharpe, M.; Wulsin, L.; Barsky, A.; Levenson, J. Somatic symptom disorder: An important change in DSM. J. Psychosom. Res. 2013, 75, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Dirkzwager, A.J.; Verhaak, P.F. Patients with persistent medically unexplained symptoms in general practice: Characteristics and quality of care. BMC Fam. Pract. 2007, 8, 1–10. [Google Scholar] [CrossRef]
- Donker, G.A.; Foets, M.; Spreeuwenberg, P. Patients with irritable bowel syndrome: Health status and use of health care services. Br. J. Gen. Pract. 1999, 49, 787–792. [Google Scholar]
- Kool, M.B.; Van Middendorp, H.; Lumley, M.A.; Schenk, Y.; Jacobs, J.W.G.; Bijlsma, J.W.J.; Geenen, R. Lack of understanding in fibromyalgia and rheumatoid arthritis: The Illness Invalidation Inventory (3* I). Ann. Rheum. Dis. 2010, 69, 1990–1995. [Google Scholar] [CrossRef] [PubMed]
- Wan Mohd Azam, W.M.Y.; Din, N.C.; Ahmad, M.; Ghazali, S.E.; Ibrahim, N.; Said, Z.; Maniam, T. Loneliness and depression among the elderly in an agricultural settlement: Mediating effects of social support. Asia-Pac. Psychiatry 2013, 5, 134–139. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Cacioppo, J.T. Aging and loneliness: Downhill quickly? Curr. Dir. Psychol. Sci. 2007, 16, 187–191. [Google Scholar] [CrossRef]
- Segrin, C.; Passalacqua, S.A. Functions of loneliness, social support, health behaviors, and stress in association with poor health. Health Commun. 2010, 25, 312–322. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Gou, Z.; Zuo, J. Social support mediates loneliness and depression in elderly people. J. Health Psychol. 2016, 21, 750–758. [Google Scholar] [CrossRef] [PubMed]
- Swami, V.; Chamorro-Premuzic, T.; Sinniah, D.; Maniam, T.; Kannan, K.; Stanistreet, D.; Furnham, A. General health mediates the relationship between loneliness, life satisfaction and depression. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 161–166. [Google Scholar] [CrossRef]
- Zhao, X.; Zhang, D.; Wu, M.; Yang, Y.; Xie, H.; Li, Y.; Su, Y. Loneliness and depression symptoms among the elderly in nursing homes: A moderated mediation model of resilience and social support. Psychiatry Res. 2018, 268, 143–151. [Google Scholar] [CrossRef]
- Cobb, S. Social support as a moderator of life stress. Psychosom. Med. 1976, 38, 300–314. [Google Scholar] [CrossRef] [Green Version]
- Van Sonderen, E. Measurement of social network and social support. Empirical results in relation to the EURIDISS instruments. Int. J. Health Sci. 1990, 1, 203–216. [Google Scholar]
- Langford, C.P.H.; Bowsher, J.; Maloney, J.P.; Lillis, P.P. Social support: A conceptual analysis. J. Adv. Nurs. 1997, 25, 95–100. [Google Scholar] [CrossRef]
- Haber, M.G.; Cohen, J.L.; Lucas, T.; Baltes, B.B. The relationship between self-reported received and perceived social support: A meta-analytic review. Am. J. Community Psychol. 2007, 39, 133–144. [Google Scholar] [CrossRef]
- Sarason, B.R.; Sarason, I.G.; Pierce, G.R. Social Support: An Interactional View; John Wiley & Sons: New York, NY, USA, 1990. [Google Scholar]
- Eagle, D.E.; Hybels, C.F.; Proeschold-Bell, R.J. Perceived social support, received social support, and depression among clergy. J. Soc. Pers. Relatsh. 2019, 36, 2055–2073. [Google Scholar] [CrossRef]
- Prati, G.; Pietrantoni, L. The relation of perceived and received social support to mental health among first responders: A meta-analytic review. J. Community Psychol. 2010, 38, 403–417. [Google Scholar] [CrossRef]
- Uchino, B.N. Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of perceived and received support. Perspect. Psychol. Sci. 2009, 4, 236–255. [Google Scholar] [CrossRef] [Green Version]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310. [Google Scholar] [CrossRef]
- Uchino, B.N. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. J. Behav. Med. 2006, 29, 377–387. [Google Scholar] [CrossRef]
- Fiksenbaum, L.M.; Greenglass, E.R.; Eaton, J. Perceived social support, hassles, and coping among the elderly. J. Appl. Gerontol. 2006, 25, 17–30. [Google Scholar] [CrossRef]
- Das, S.; Mandal, U.S.; Nath, S.; Mondal, A. Relationship between perceived social support and severity of symptoms in persons with somatoform disorder. J. Evol. Med. Dent. Sci. 2020, 9, 320–323. [Google Scholar] [CrossRef]
- Nakkas, C.; Annen, H.; Brand, S. Somatization and coping in ethnic minority recruits. Mil. Med. 2019, 184, e680–e685. [Google Scholar] [CrossRef] [PubMed]
- Arrindell, W.A.; Ettema, J.H.M. Symptom Checklist SCL-90; Swets and Zeitlinger: Lisse, The Netherlands, 2004. [Google Scholar]
- Bridges, K.R.; Sanderman, R.; Van Sonderen, E. An English language version of the social support list: Preliminary reliability. Psychol. Rep. 2002, 90, 1055–1058. [Google Scholar] [CrossRef] [PubMed]
- Van Sonderen, E. Het Meten van Sociale Steun Met de Sociale Steun Lijst Handleiding [Assessing Social Support with the Social Support List Manual]. Groningen: Rijksunversiteit Groningen. 1993. Available online: https://research.rug.nl/en/publications/het-meten-van-sociale-steun (accessed on 26 October 2021).
- de Jong Gierveld, J.; Kamphuis, F.H. The development of a Rasch-type loneliness scale. Appl. Psychol. Meas. 1985, 9, 289–299. [Google Scholar] [CrossRef]
- Process-Based CBT: The Science and Core Clinical Competencies of Cognitive Behavioral Therapy; Hayes, S.C.; Hofmann, S.G. (Eds.) New Harbinger: Oakland, CA, USA, 2018. [Google Scholar]
- MacKinnon, D.P.; Lockwood, C.M.; Williams, J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivar. Behav. Res. 2004, 39, 99–128. [Google Scholar] [CrossRef] [Green Version]
- Afifi, M. Gender differences in mental health. Singap. Med. J. 2007, 48, 385. [Google Scholar]
- Rosenfield, S.; Mouzon, D. Gender and mental health. In Handbook of the Sociology of Mental Health; Springer: Dordrecht, The Netherlands, 2013; pp. 277–296. [Google Scholar]
- Blazer, D.; George, L.K.; Hughes, D. The epidemiology of anxiety disorders: An age comparison. In Anxiety in the Elderly: Treatment and Research; Salzman, C., Lebowitz, B.D., Eds.; Springer: New York, NY, USA, 1991; pp. 17–30. [Google Scholar]
- Gatz, M.; Hurwicz, M.L. Are old people more depressed? Cross-sectional data on Center for Epidemiological Studies Depression Scale factors. Psychol. Aging 1990, 5, 284. [Google Scholar] [CrossRef]
- Kessler, R.C.; Foster, C.; Webster, P.S.; House, J.S. The relationship between age and depressive symptoms in two national surveys. Psychol. Aging 1992, 7, 119. [Google Scholar] [CrossRef]
- Peyrot, W.J.; Lee, S.H.; Milaneschi, Y.; Abdellaoui, A.; Byrne, E.M.; Esko, T.; Penninx, B.W.J.H. The association between lower educational attainment and depression owing to shared genetic effects? Results in~ 25 000 subjects. Mol. Psychiatry 2015, 20, 735–743. [Google Scholar] [CrossRef] [Green Version]
- Yuan, S.; Xiong, Y.; Michaëlsson, M.; Michaëlsson, K.; Larsson, S.C. Genetically predicted education attainment in relation to somatic and mental health. Sci. Rep. 2021, 11, 1–11. [Google Scholar]
- Dooley, D.; Prause, J.; Ham-Rowbottom, K.A. Underemployment and depression: Longitudinal relationships. J. Health Soc. Behav. 2000, 41, 421–436. [Google Scholar] [CrossRef]
- Evans, J.; Repper, J. Employment, social inclusion and mental health. J. Psychiatr. Ment. Health Nurs. 2000, 7, 15–24. [Google Scholar]
- Social Determinants of Health; Marmot, M.; Wilkinson, R. (Eds.) Oxford University Press: Oxford, UK, 2005. [Google Scholar]
- Waddell, G.; Burton, A.K. Is work good for your health and well-being? Occup. Med. 2006, 57, 229. [Google Scholar]
- van der Noordt, M.; IJzelenberg, H.; Droomers, M.; Proper, K.I. Health effects of employment: A systematic review of prospective studies. Occup. Environ. Med. 2014, 71, 730–736. [Google Scholar] [CrossRef]
- Westman, M.; Etzion, D.; Horovitz, S. The toll of unemployment does not stop with the unemployed. Hum. Relat. 2004, 57, 823–844. [Google Scholar] [CrossRef] [Green Version]
- Simon, R.W. Revisiting the relationships among gender, marital status, and mental health. Am. J. Sociol. 2002, 107, 1065–1096. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Fredrickson, B.L. The broaden-and-build theory of positive emotions. Philos. Trans. R. Soc. London. Ser. Bbiological Sci. 2004, 359, 1367–1378. [Google Scholar] [CrossRef] [PubMed]
- Conway, A.M.; Tugade, M.M.; Catalino, L.I.; Fredrickson, B.L. The broaden-andbuild theory of positive emotions: Form, function, and mechanisms. In The Oxford Handbook of Happiness; David, S.A., Boniwell, I., Ayers, A.C., Eds.; Oxford University Press: Oxford, UK, 2013; pp. 17–34. [Google Scholar]
- Turner, R.J.; Lloyd, D.A. The stress process and the social distribution of depression. J. Health Soc. Behav. 1999, 374–404. [Google Scholar]
- Cutler, D.; Lleras-Muney, A. Education and Health: Evaluating the Theories and Evidence; National Bureau of Economic Researcho: Cambridge, MA, USA, 2006. [Google Scholar]
- Dodu, N. Is employment good for well-being? A literature review. J. Occup. Psychol. Employ. Disabil. 2005, 7, 17–33. [Google Scholar]
- McWhirter, B.T. Loneliness: A review of current literature, with implications for counseling and research. J. Couns. Dev. 1990, 68, 417–422. [Google Scholar] [CrossRef]
- Jones, W.H.; Freemon, J.E.; Goswick, R.A. The persistence of loneliness: Self and other determinants 1. J. Personal. 1981, 49, 27–48. [Google Scholar] [CrossRef]
- Wittenberg, M.T.; Reis, H.T. Loneliness, social skills, and social perception. Personal. Soc. Psychol. Bull. 1986, 12, 121–130. [Google Scholar] [CrossRef]
- Bolger, N.; Amarel, D. Effects of social support visibility on adjustment to stress: Experimental evidence. J. Personal. Soc. Psychol. 2007, 92, 458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bessaha, M.L.; Sabbath, E.L.; Morris, Z.; Malik, S.; Scheinfeld, L.; Saragossi, J. A systematic review of loneliness interventions among non-elderly adults. Clin. Soc. Work J. 2020, 48, 110–125. [Google Scholar] [CrossRef]
- Masi, C.M.; Chen, H.Y.; Hawkley, L.C.; Cacioppo, J.T. A meta-analysis of interventions to reduce loneliness. Personal. Soc. Psychol. Rev. 2011, 15, 219–266. [Google Scholar] [CrossRef] [Green Version]
- Barrera, M.; Glasgow, R.E.; McKay, H.G.; Boles, S.M.; Feil, E.G. Do Internet-based support interventions change perceptions of social support?: An experimental trial of approaches for supporting diabetes self-management. Am. J. Community Psychol. 2002, 30, 637–654. [Google Scholar] [CrossRef] [PubMed]
- Hogan, B.E.; Linden, W.; Najarian, B. Social support interventions: Do they work? Clin. Psychol. Rev. 2002, 22, 381–440. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| M(SD) or % | Min | Max | Kurtosis | Skewness | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Loneliness | 0.25 (0.30) | 0.00 | 1.00 | 0.15 | 1.13 | 1 | 0.70 ** | 0.67 ** | 0.74 ** | 0.66 ** | 0.58 ** | 0.03 | 0.14 | −0.32 ** | −0.38 ** | −0.30 ** |
| 2. Social support deficit | 1.34 (0.37) | 1.00 | 2.68 | 1.16 | 1.32 | 1 | 0.59 ** | 0.66 ** | 0.57 ** | 0.44 ** | 0.07 | 0.11 | −0.27 ** | −0.30 ** | 0.28 ** | |
| 3. Anxiety | 1.72 (0.84) | 1.00 | 4.90 | 1.58 | 1.40 | 1 | 0.89 ** | 0.87 ** | 0.73 ** | −0.01 | 0.12 | −0.38 ** | −0.44 ** | 0.22 ** | ||
| 4. Depression | 1.91 (0.99) | 1.00 | 4.63 | 0.10 | 1.11 | 1 | 0.86 ** | 0.74 ** | 0.00 | 0.12 | −0.35 ** | −0.46 ** | 0.21 ** | |||
| 5. Somatic symptoms | 1.91 (0.94) | 1.00 | 4.75 | −0.36 | 0.92 | 1 | 0.83 ** | −0.03 | 0.15 * | −0.44 ** | −0.47 ** | 0.21 ** | ||||
| 6. SSD | 40.1% | 1 | 0.01 | 0.13 | −0.51 ** | −0.54 ** | 0.20 ** | |||||||||
| 7. Sex | 36.9% | 1 | 0.08 | 0.07 | 0.04 | −0.05 | ||||||||||
| 8. Age | 43.99 (13.42) | 1 | −0.08 | −0.01 | −0.20 ** | |||||||||||
| 9. Education | 53.5% | 1 | 0.28 ** | −0.02 | ||||||||||||
| 10. Having a paid job | 66.8% | 1 | −0.27 ** | |||||||||||||
| 11. Being single | 27.8% | 1 |
| Anxiety | Depression | Somatic Symptoms | Somatic Symptom Disorder | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimated Effect | 95% CI | Estimated Effect | 95% CI | Estimated Effect | 95% CI | Estimated Effect | 95% CI | |||||
| Lower Bounds | Upper Bounds | Lower Bounds | Upper Bounds | Lower Bounds | Upper Bounds | Lower Bounds | Upper Bounds | |||||
| Direct effect | ||||||||||||
| Loneliness → social support deficit | 0.87 ** | 0.74 | 0.99 | 0.87 ** | 0.74 | 0.99 | 0.87 ** | 0.74 | 0.99 | 0.87 ** | 0.74 | 0.99 |
| Loneliness → outcome | 1.37 ** | 0.96 | 1.78 | 1.76 ** | 1.34 | 2.19 | 1.60 ** | 1.13 | 2.06 | 4.74 ** | 2.92 | 6.57 |
| Social support deficit → outcome | 0.55 ** | 0.21 | 0.88 | 0.74 ** | 0.39 | 1.08 | 0.52 ** | 0.10 | 0.81 | 0.77 | −0.60 | 2.15 |
| Indirect effect | ||||||||||||
| Loneliness → social support deficit → outcome | 0.47 ** | 0.12 | 0.83 | 0.64 ** | 0.22 | 1.09 | 0.45 ** | 0.05 | 0.86 | 0.67 | −0.69 | 1.97 |
| N | 187 | 187 | 187 | 187 | ||||||||
| R2 | 0.47 | 0.58 | 0.46 | 0.28 | ||||||||
| Anxiety | Depression | Somatic Symptoms | Somatic Symptom Disorder | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimated Effect | 95% CI | Estimated Effect | 95% CI | Estimated Effect | 95% CI | Estimated Effect | 95% CI | |||||
| Lower Bounds | Upper Bounds | Lower Bounds | Upper Bounds | Lower Bounds | Upper Bounds | Lower Bounds | Upper Bounds | |||||
| Direct effect | ||||||||||||
| Loneliness → social support deficit | 0.80 ** | 0.65 | 0.95 | 0.80 ** | 0.65 | 0.95 | 0.80 ** | 0.65 | 0.95 | 0.80 ** | 0.65 | 0.95 |
| Loneliness → outcome | 1.10 ** | 0.68 | 1.53 | 1.52 ** | 1.08 | 1.95 | 1.20 ** | 0.74 | 1.65 | 4.10 ** | 1.94 | 6.25 |
| Social support deficit → outcome | 0.50 ** | 0.18 | 0.83 | 0.71 ** | 0.38 | 1.05 | 0.45 * | 0.10 | 0.81 | 0.58 | −1.11 | 2.27 |
| Indirect effect | ||||||||||||
| Loneliness → social support deficit → outcome | 0.40 ** | 0.08 | 0.74 | 0.57 ** | 0.21 | 0.99 | 0.36 ** | 0.01 | 0.72 | 0.46 | −1.31 | 2.36 |
| N | 187 | 187 | 187 | 187 | ||||||||
| R2 | 0.53 | 0.63 | 0.55 | 0.50 | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hutten, E.; Jongen, E.M.M.; Vos, A.E.C.C.; van den Hout, A.J.H.C.; van Lankveld, J.J.D.M. Loneliness and Mental Health: The Mediating Effect of Perceived Social Support. Int. J. Environ. Res. Public Health 2021, 18, 11963. https://doi.org/10.3390/ijerph182211963
Hutten E, Jongen EMM, Vos AECC, van den Hout AJHC, van Lankveld JJDM. Loneliness and Mental Health: The Mediating Effect of Perceived Social Support. International Journal of Environmental Research and Public Health. 2021; 18(22):11963. https://doi.org/10.3390/ijerph182211963
Chicago/Turabian StyleHutten, Elody, Ellen M. M. Jongen, Anique E. C. C. Vos, Anja J. H. C. van den Hout, and Jacques J. D. M. van Lankveld. 2021. "Loneliness and Mental Health: The Mediating Effect of Perceived Social Support" International Journal of Environmental Research and Public Health 18, no. 22: 11963. https://doi.org/10.3390/ijerph182211963
APA StyleHutten, E., Jongen, E. M. M., Vos, A. E. C. C., van den Hout, A. J. H. C., & van Lankveld, J. J. D. M. (2021). Loneliness and Mental Health: The Mediating Effect of Perceived Social Support. International Journal of Environmental Research and Public Health, 18(22), 11963. https://doi.org/10.3390/ijerph182211963






