The Relationship between Leg Extension Angle at Late Stance and Knee Flexion Angle at Swing Phase during Gait in Community-Dwelling Older Adults
Abstract
:1. Introduction
2. Materials and Methods
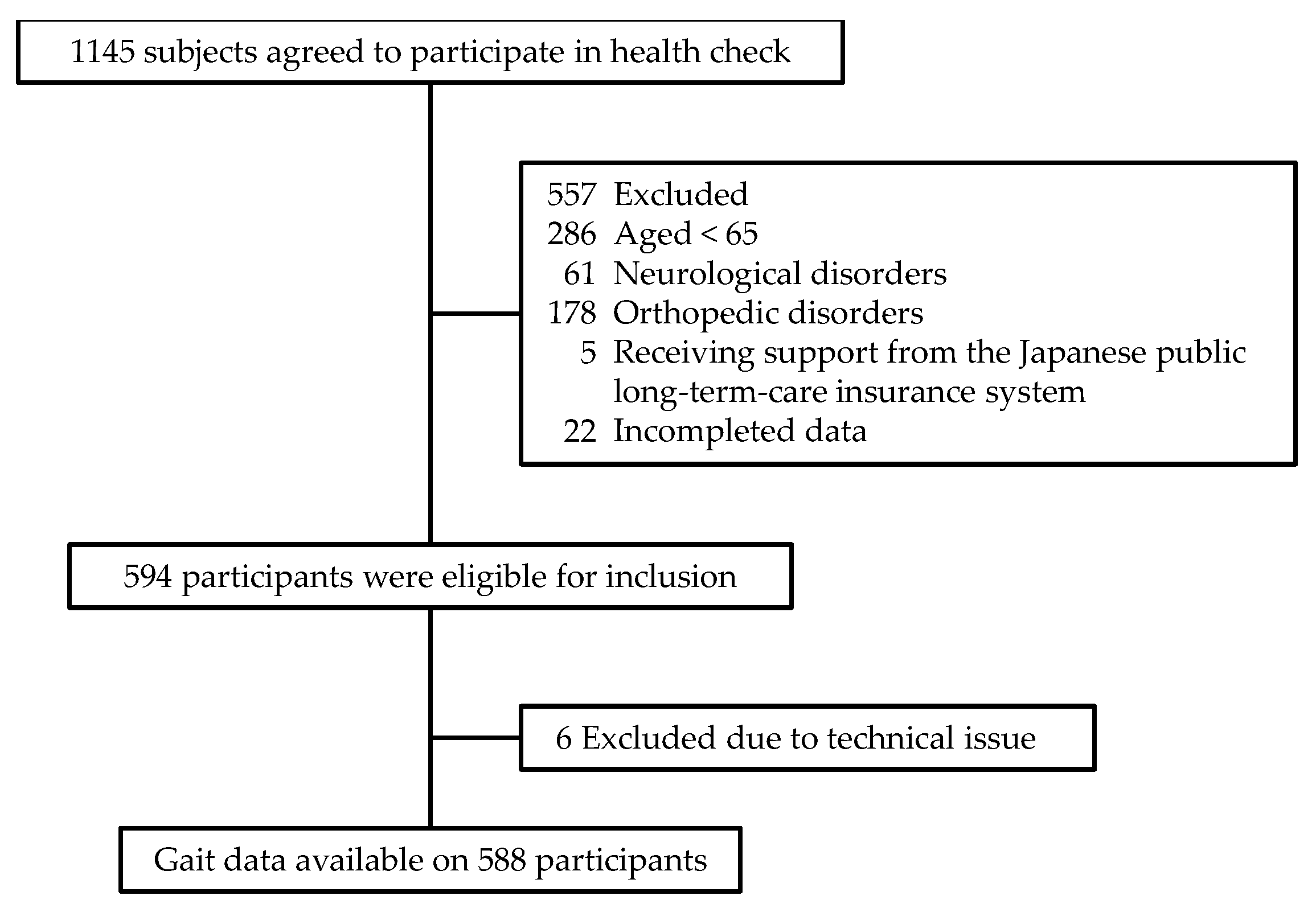
2.1. Participants
2.2. Gait Measurement
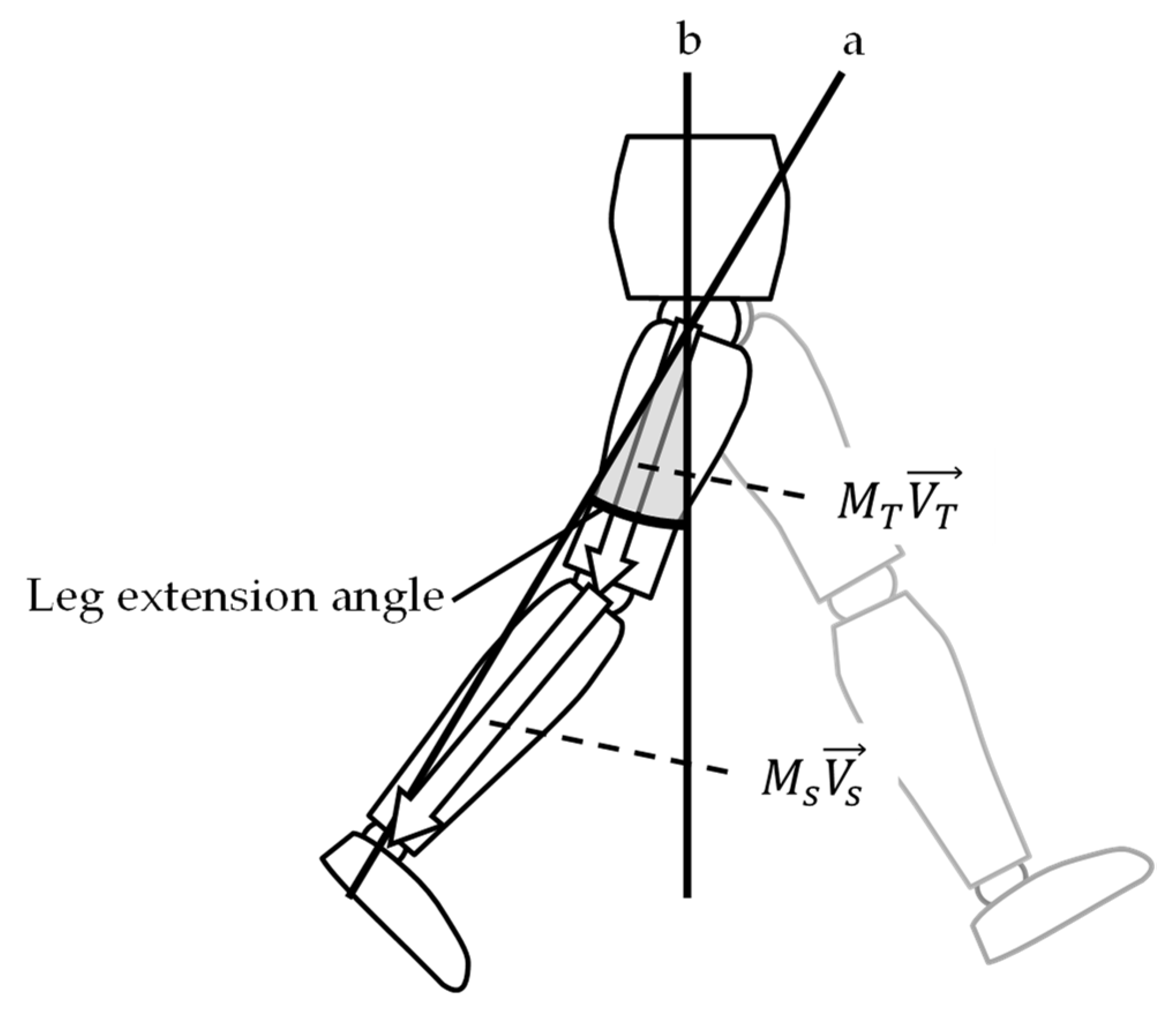
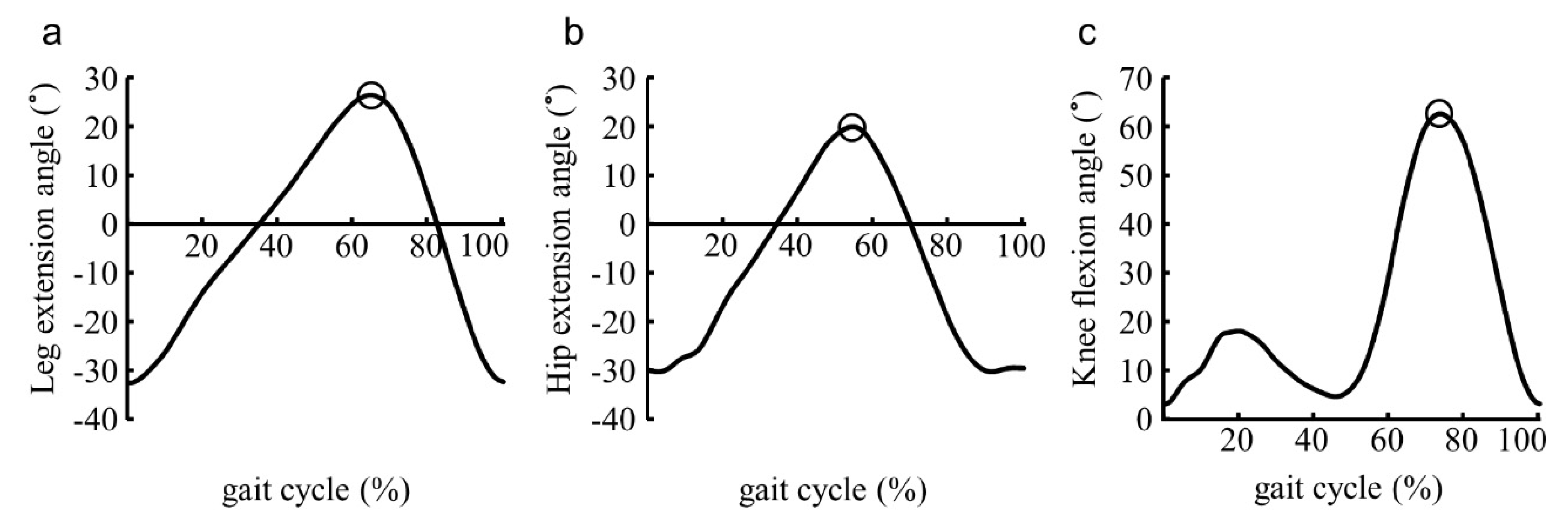
2.3. Data Analysis
2.4. Statistical Analysis
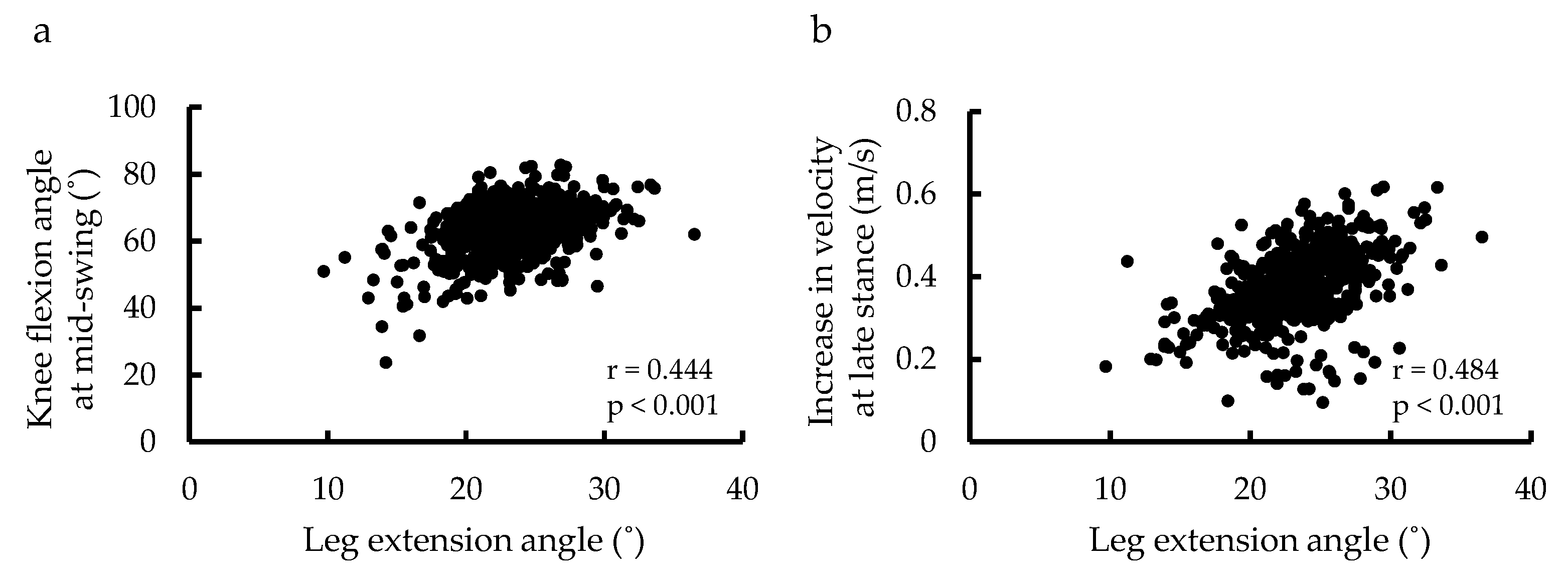
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van Kan, G.A.; Rolland, Y.; Andrieu, S.; Bauer, J.; Beauchet, O.; Bonnefoy, M.; Cesari, M.; Donini, L.; Gillette-Guyonnet, S.; Inzitari, M.; et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J. Nutr. Health Aging 2009, 13, 881–889. [Google Scholar] [CrossRef]
- Barnes, L.L.; Wilson, R.S.; Bienias, J.L.; De Leon, C.F.M.; Kim, H.-J.N.; Buchman, A.S.; Bennett, D.A. Correlates of Life Space in a Volunteer Cohort of Older Adults. Exp. Aging Res. 2007, 33, 77–93. [Google Scholar] [CrossRef]
- Barrett, R.; Mills, P.; Begg, R. A systematic review of the effect of ageing and falls history on minimum foot clearance characteristics during level walking. Gait Posture 2010, 32, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Boyer, K.A.; Johnson, R.; Banks, J.J.; Jewell, C.; Hafer, J.F. Systematic review and meta-analysis of gait mechanics in young and older adults. Exp. Gerontol. 2017, 95, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Astephen, J.L.; Deluzio, K.J.; Caldwell, G.E.; Dunbar, M.J. Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis severity. J. Orthop. Res. 2007, 26, 332–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monda, M.; Goldberg, A.; Smitham, P.; Thornton, M.; McCarthy, I. Use of Inertial Measurement Units to Assess Age-related Changes in Gait Kinematics in an Active Population. J. Aging Phys. Act. 2015, 23, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Thaler-Kall, K.; Peters, A.; Thorand, B.; Grill, E.; Autenrieth, C.S.; Horsch, A.; Meisinger, C. Description of spatio-temporal gait parameters in elderly people and their association with history of falls: Results of the population-based cross-sectional KORA-Age study. BMC Geriatr. 2015, 15, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benson, L.C.; Cobb, S.C.; Hyngstrom, A.S.; Keenan, K.G.; Luo, J.; O’Connor, K.M. Identifying trippers and non-trippers based on knee kinematics during obstacle-free walking. Hum. Mov. Sci. 2018, 62, 58–66. [Google Scholar] [CrossRef] [Green Version]
- Kesar, T.M.; Binder-Macleod, S.A.; Hicks, G.; Reisman, D.S. Minimal detectable change for gait variables collected during treadmill walking in individuals post-stroke. Gait Posture 2011, 33, 314–317. [Google Scholar] [CrossRef] [Green Version]
- Hsiao, H.; Knarr, B.A.; Higginson, J.S.; Binder-Macleod, S.A. The relative contribution of ankle moment and trailing limb angle to propulsive force during gait. Hum. Mov. Sci. 2014, 39, 212–221. [Google Scholar] [CrossRef] [Green Version]
- Awad, L.N.; Binder-Macleod, S.A.; Pohlig, R.T.; Reisman, D.S. Paretic Propulsion and Trailing Limb Angle Are Key Determinants of Long-Distance Walking Function After Stroke. Neurorehabilit. Neural Repair 2014, 29, 499–508. [Google Scholar] [CrossRef] [Green Version]
- McGrath, R.L.; Ziegler, M.L.; Pires-Fernandes, M.; Knarr, B.A.; Higginson, J.S.; Sergi, F. The effect of stride length on lower extremity joint kinetics at various gait speeds. PLoS ONE 2019, 14, e0200862. [Google Scholar] [CrossRef] [Green Version]
- Chen, G.; Patten, C.; Kothari, D.H.; Zajac, F.E. Gait differences between individuals with post-stroke hemiparesis and non-disabled controls at matched speeds. Gait Posture 2005, 22, 51–56. [Google Scholar] [CrossRef]
- Ganley, K.J.; Powers, C.M. Gait kinematics and kinetics of 7-year-old children: A comparison to adults using age-specific anthropometric data. Gait Posture 2005, 21, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Schache, A.G.; Baker, R. On the expression of joint moments during gait. Gait Posture 2007, 25, 440–452. [Google Scholar] [CrossRef]
- Anderson, F.C.; Goldberg, S.R.; Pandy, M.; Delp, S.L. Contributions of muscle forces and toe-off kinematics to peak knee flexion during the swing phase of normal gait: An induced position analysis. J. Biomech. 2004, 37, 731–737. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, S.R.; Anderson, F.C.; Pandy, M.; Delp, S.L. Muscles that influence knee flexion velocity in double support: Implications for stiff-knee gait. J. Biomech. 2004, 37, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- Whittington, B.; Silder, A.; Heiderscheit, B.; Thelen, D.G. The contribution of passive-elastic mechanisms to lower extremity joint kinetics during human walking. Gait Posture 2008, 27, 628–634. [Google Scholar] [CrossRef] [Green Version]
- Ferrari, A.; Cutti, A.G.; Garofalo, P.; Raggi, M.; Heijboer, M.; Cappello, A.; Davalli, A. First in vivo assessment of “Outwalk”: A novel protocol for clinical gait analysis based on inertial and magnetic sensors. Med. Biol. Eng. Comput. 2009, 48, 1–15. [Google Scholar] [CrossRef]
- Miyazaki, T.; Kawada, M.; Nakai, Y.; Kiyama, R.; Yone, K. Validity of Measurement for Trailing Limb Angle and Propulsion Force during Gait Using a Magnetic Inertial Measurement Unit. BioMed Res. Int. 2019, 2019, 8123467. [Google Scholar] [CrossRef]
- Mortaza, N.; Abu Osman, N.A.; Mehdikhani, N. Are the spatio-temporal parameters of gait capable of distinguishing a faller from a non-faller elderly? Eur. J. Phys. Rehabil. Med. 2014, 50, 677–691. [Google Scholar]
- Huijben, B.; van Schooten, K.; van Dieën, J.; Pijnappels, M. The effect of walking speed on quality of gait in older adults. Gait Posture 2018, 65, 112–116. [Google Scholar] [CrossRef] [Green Version]
- Magnani, P.E.; Junior, R.C.F.; Zanellato, N.F.G.; Genovez, M.B.; Alvarenga, I.C.; de Abreu, D.C.C. The influence of aging on the spatial and temporal variables of gait during usual and fast speeds in older adults aged 60 to 102 years. Hum. Mov. Sci. 2019, 68, 102540. [Google Scholar] [CrossRef] [PubMed]
- Seino, S.; Shinkai, S.; Fujiwara, Y.; Obuchi, S.; Yoshida, H.; Hirano, H.; Kim, H.K.; Ishizaki, T.; Takahashi, R.; on behalf of the TMIG-LISA Research Group. Reference Values and Age and Sex Differences in Physical Performance Measures for Community-Dwelling Older Japanese: A Pooled Analysis of Six Cohort Studies. PLoS ONE 2014, 9, e99487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawai, H.; Taniguchi, Y.; Seino, S.; Sakurai, R.; Osuka, Y.; Obuchi, S.; Watanabe, Y.; Kim, H.; Inagaki, H.; Kitamura, A.; et al. Reference values of gait parameters measured with a plantar pressure platform in community-dwelling older Japanese adults. Clin. Interv. Aging 2019, 14, 1265–1276. [Google Scholar] [CrossRef] [Green Version]
- Kerrigan, D.; Lee, L.W.; Collins, J.J.; Riley, P.O.; Lipsitz, L.A. Reduced hip extension during walking: Healthy elderly and fallers versus young adults. Arch. Phys. Med. Rehabil. 2001, 82, 26–30. [Google Scholar] [CrossRef]
- Panizzolo, F.A.; Green, D.J.; Lloyd, D.G.; Maiorana, A.J.; Rubenson, J. Soleus fascicle length changes are conserved between young and old adults at their preferred walking speed. Gait Posture 2013, 38, 764–769. [Google Scholar] [CrossRef]
- Peterson, C.L.; Cheng, J.; Kautz, S.; Neptune, R.R. Leg extension is an important predictor of paretic leg propulsion in hemiparetic walking. Gait Posture 2010, 32, 451–456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, T.; Li, H.; Liu, Q.; Duan, L.; Li, M.; Wang, C.; Liu, Q.; Li, W.; Shang, W.; Wu, Z.; et al. Inertial Sensor-Based Motion Analysis of Lower Limbs for Rehabilitation Treatments. J. Health Eng. 2017, 2017, 1949170. [Google Scholar] [CrossRef]
- Genthe, K.; Schenck, C.; Eicholtz, S.; Zajac-Cox, L.; Wolf, S.; Kesar, T.M. Effects of real-time gait biofeedback on paretic propulsion and gait biomechanics in individuals post-stroke. Top. Stroke Rehabil. 2017, 25, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Kesar, T.M.; Reisman, D.S.; Perumal, R.; Jancosko, A.M.; Higginson, J.S.; Rudolph, K.S.; Binder-Macleod, S.A. Combined effects of fast treadmill walking and functional electrical stimulation on post-stroke gait. Gait Posture 2011, 33, 309–313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reisman, D.S.; Kesar, T.M.; Perumal, R.; Roos, M.A.; Rudolph, K.S.; Higginson, J.; Helm, E.; Binder-Macleod, S. Time Course of Functional and Biomechanical Improvements During a Gait Training Intervention in Persons With Chronic Stroke. J. Neurol. Phys. Ther. 2013, 37, 159–165. [Google Scholar] [CrossRef] [PubMed]
| Gait Parameter | Late Stance | Mid-Swing | ||
|---|---|---|---|---|
| Leg Extension Angle | Hip Extension | Increase in Velocity | Knee Flexion | |
| Late stance | ||||
| Leg extension angle | - | 0.508 ** | 0.484 ** | 0.444 ** |
| Hip extension | - | 0.300 ** | 0.126 ** | |
| Increase in velocity | - | 0.344 ** | ||
| Mid-swing | ||||
| Knee flexion | - | |||
| Variables | Unstandardized Regression Coefficient (B) | Standardized Regression Coefficient (β) | p |
|---|---|---|---|
| Leg extension angle | 0.663 | 0.296 | <0.001 |
| Hip extension angle | −0.264 | −0.150 | <0.001 |
| Gait speed | 7.623 | 0.219 | <0.001 |
| Age | −0.342 | −0.265 | <0.001 |
| Sex | −1.107 | −0.060 | 0.047 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miyazaki, T.; Kiyama, R.; Nakai, Y.; Kawada, M.; Takeshita, Y.; Araki, S.; Hayashi, H.; Higashi, N.; Makizako, H. The Relationship between Leg Extension Angle at Late Stance and Knee Flexion Angle at Swing Phase during Gait in Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2021, 18, 11925. https://doi.org/10.3390/ijerph182211925
Miyazaki T, Kiyama R, Nakai Y, Kawada M, Takeshita Y, Araki S, Hayashi H, Higashi N, Makizako H. The Relationship between Leg Extension Angle at Late Stance and Knee Flexion Angle at Swing Phase during Gait in Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health. 2021; 18(22):11925. https://doi.org/10.3390/ijerph182211925
Chicago/Turabian StyleMiyazaki, Takasuke, Ryoji Kiyama, Yuki Nakai, Masayuki Kawada, Yasufumi Takeshita, Sota Araki, Hiroyuki Hayashi, Naoto Higashi, and Hyuma Makizako. 2021. "The Relationship between Leg Extension Angle at Late Stance and Knee Flexion Angle at Swing Phase during Gait in Community-Dwelling Older Adults" International Journal of Environmental Research and Public Health 18, no. 22: 11925. https://doi.org/10.3390/ijerph182211925
APA StyleMiyazaki, T., Kiyama, R., Nakai, Y., Kawada, M., Takeshita, Y., Araki, S., Hayashi, H., Higashi, N., & Makizako, H. (2021). The Relationship between Leg Extension Angle at Late Stance and Knee Flexion Angle at Swing Phase during Gait in Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health, 18(22), 11925. https://doi.org/10.3390/ijerph182211925







