Exploring the Role of Health Expenditure and Maternal Mortality in South Asian Countries: An Approach towards Shaping Better Health Policy
Abstract
:1. Introduction
2. Literature Review
3. Materials and Methods
3.1. Data Sources
3.2. Model Specification
4. Results and Discussion
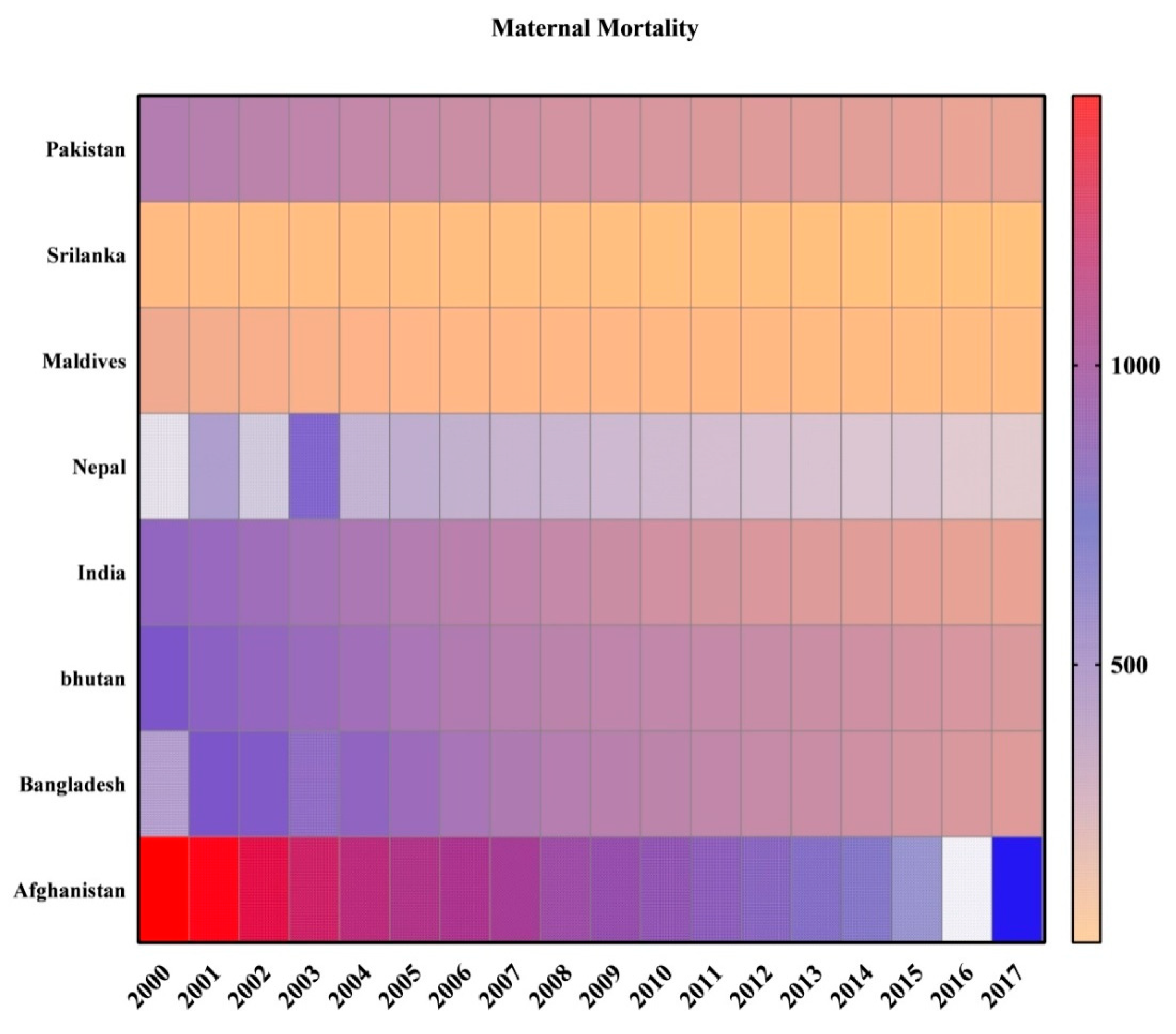
4.1. Descriptive Statistics
4.2. Unit Root Tests
4.3. Panel Cointegration Test
4.4. Panel Estimation Results
4.4.1. Fixed Effect and Random Effect Results
4.4.2. FMOLS and DOLS Results
4.5. Discussion
5. Conclusions and Policy Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kiross, G.T.; Chojenta, C.; Barker, D.; Loxton, D. The effects of health expenditure on infant mortality in sub-Saharan Africa: Evidence from panel data analysis. Health Econ. Rev. 2020, 10, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romer, D. Advanced Macroeconomics, 5th ed.; McGraw-Hill Education: New York, NY, USA, 2018. [Google Scholar]
- Owusu, P.A.; Sarkodie, S.A.; Pedersen, P.A. Relationship between mortality and health care expenditure: Sustainable assessment of health care system. PLoS ONE 2021, 16, e0247413. [Google Scholar] [CrossRef] [PubMed]
- How Maternal Mortality Has Been Reduced in South Asia. Available online: https://www.weforum.org/agenda/2015/01/how-maternal-mortality-has-been-reduced-in-south-asia/ (accessed on 15 January 2015).
- Alkema, L.; Chou, D.; Hogan, D.; Zhang, S.; Moller, A.B.; Gemmill, A.; Fat, D.M.; Boerma, T.; Temmerman, M.; Mathers, C.; et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 2016, 387, 462–474. [Google Scholar] [CrossRef] [Green Version]
- Hill, K.; Johnson, P.; Singh, K.; Amuzu-Pharin, A.; Kharki, Y. Using census data to measure maternal mortality: A review of recent experience. Demographic. Demogr. Res. 2018, 39, 337–364. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Maternal Mortality; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Le Blanc, D. Towards Integration at Last? The Sustainable Development Goals as a Network of Targets. Sustain. Dev. 2015, 23, 176–187. [Google Scholar] [CrossRef]
- Anyanwu, J.C.; Andrew, E.O.E. Health expenditures and health outcomes in Africa. Afr. Dev. Rev. 2009, 21, 400–433. [Google Scholar] [CrossRef]
- WHO. New Perspectives on Global Health Spending for Universal Health Coverage; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Si, R.; Lu, Q.; Aziz, N. Impact of COVID-19 on peoples’ willingness to consume wild animals: Empirical insights from China. One Health 2021, 12, 100240. [Google Scholar] [CrossRef]
- Si, R.; Yao, Y.; Zhang, X.; Lu, Q.; Aziz, N. Investigating the Links Between Vaccination Against COVID-19 and Public Attitudes Toward Protective Countermeasures: Implications for Public Health. Front. Public Health 2021, 9, 1040. [Google Scholar] [CrossRef]
- WHO. World Health Statistics; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Babazono, A.; Hillman, A. A comparison of international health outcomes and health care spending. Int. J. Technol. Assess. Health Care 1994, 10, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.C.; Messer, J. Public financing of health expenditures, insurance, and health outcomes. Appl. Econ. 2002, 34, 2105–2113. [Google Scholar] [CrossRef]
- Crémieux, P.Y.; Meilleur, M.C.; Ouellette, P.; Petit, P.; Zelder, M.; Potvin, K.C. Public and private pharmaceutical spending as determinants of health outcomes in Canada. Health Econ. 2005, 14, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Hitiris, T.; Posnett, J. The determinants and effects of health expenditure in developed countries. J. Health Econ. 1992, 11, 173–181. [Google Scholar] [CrossRef]
- Zeynep, O. Determinants of health outcomes in industrialised countries: A pooled, cross-country, time-series analysis. OECD Econ. Stud. 2000, 30, 53–77. [Google Scholar]
- Nixon, J.; Ulmann, P. The relationship between health care expenditure and health outcomes. Evidence and caveats for a causal link. Eur. J. Health Econ. 2006, 7, 7–18. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Gupta, I.; De’silva, H.; Manandhar, D.; Awasthi, S.; Hossain, M.; Salam, M.A.; Lanka, S. Education and debate Maternal and child health: Is South Asia ready for change? Situational analysis. BMJ Br. Med. J. 2004, 328, 816–819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nair, V.; Jayasinghe, S.; Behranwala, A.; Unger, J.; Ana, J. Health in South Asia. Br. Med. J. 2004, 328, 1497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baldacci, E.; Clements, B.J.; Gupta, S.; Cui, Q. Social Spending, Human Capital, and Growth in Developing Countries. World Dev. 2008, 36, 1317–1341. [Google Scholar] [CrossRef]
- Aid, the Incentive Regime, and Poverty Reduction. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=597236 (accessed on 20 April 2016).
- Filmer, D.; Pritchett, L. The impact of public spending on health: Does money matter? Soc. Sci. Med. 1999, 49, 1309–1323. [Google Scholar] [CrossRef]
- Novignon, J.; Olakojo, S.A.; Nonvignon, J. The effects of public and private health care expenditure on health status in sub-Saharan Africa: New evidence from panel data analysis. Health Econ. Rev. 2012, 2, 22. [Google Scholar] [CrossRef] [Green Version]
- Ssozi, J.; Amlani, S. The Effectiveness of Health Expenditure on the Proximate and Ultimate Goals of Healthcare in Sub-Saharan Africa. World Dev. 2015, 76, 165–179. [Google Scholar] [CrossRef]
- Sen, A. Development as Freedom. In The Globalization and Development Reader: Perspectives on Development and Global Change; Oxford University Press: Oxford, UK, 1999. [Google Scholar]
- Perkins, D.; Radelet, S.; Lindauer, D.; Block, S. Economics of Development; W.W. Norton & Company: New York, NY, USA, 2013. [Google Scholar]
- Booth, D.; Cammack, D. Governance for Development in Africa; Zed Books: New York, NY, USA, 2013. [Google Scholar]
- Betrán, A.P.; Wojdyla, D.; Posner, S.F.; Gülmezoglu, A.M. National estimates for maternal mortality: An analysis based on the WHO systematic review of maternal mortality and morbidity. BMC Public Health 2005, 5, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chirowa, F.; Atwood, S.; Van der Putten, M. Gender inequality, health expenditure and maternal mortality in sub-Saharan Africa: A secondary data analysis. Afr. J. Prim. Health Care Fam. Med. 2013, 5, 471. [Google Scholar] [CrossRef]
- Akca, N.; Sonmez, S.; Yilmaz, A. Determinants of health expenditure in OECD countries: A decision tree model. Pak. J. Med. Sci. 2017, 33, 1490–1494. [Google Scholar] [CrossRef] [PubMed]
- Bhalotra, S. Spending to save? State health expenditure and infant mortality in India. Health Econ. 2007, 16, 911–928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rana, R.H.; Alam, K.; Gow, J. Health Expenditure, Child and Maternal Mortality Nexus: A Comparative Global Analysis. BMC Int. Health Hum. Rights 2018, 18, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aziz, N.; He, J.; Raza, A.; Sui, H.; Yue, W. Elucidating the Macroeconomic Determinants of Undernourishment in South Asian Countries: Building the Framework for Action. Front. Public Health 2021, 9, 696789. [Google Scholar] [CrossRef] [PubMed]
- Aldogan, M.; Austill, A.D.; Kocakülâh, M.C. The excellence of activity-based costing in cost calculation: Case study of a private hospital in Turkey. J. Health Care Financ. 2014, 41, 1–27. [Google Scholar]
- Bokhari, F.; Gai, Y.; Gottret, P. Government health expenditures and health outcomes. Health Econ. 2007, 16, 257–273. [Google Scholar] [CrossRef]
- Nketiah-Amponsah, E. The Impact of Health Expenditures on Health Outcomes in Sub-Saharan Africa. J. Dev. Soc. 2019, 35, 134–152. [Google Scholar] [CrossRef]
- Arthur, E.; Oaikhenan, H.E. The effects of health expenditure on health outcomes in Sub-Saharan Africa (SSA). Afr. Dev. Rev. 2017, 29, 524–525. [Google Scholar] [CrossRef]
- Musgrove, P. Public and private roles in health: Theory and financing patterns. In HNP Discussion Paper Series; The World Bank: Washington, DC, USA, 1996. [Google Scholar]
- Ashiabi, N.; Nketiah-Amponsah, E.; Senadza, B. The Effect of Health Expenditure on Selected Maternal and Child Health Outcomes in Sub Saharan Africa. Int. J. Soc. Econ. 2016, 43, 1386–1399. [Google Scholar]
- Bradley, E.H.; Elkins, B.R.; Herrin, J.; Elbel, B. Health and social services expenditures: Associations with health outcomes. BMJ Qual. Saf. 2011, 20, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Self, S.; Grabowski, R. How effective is public health expenditure in improving overall health? A cross-country analysis. Appl. Econ. 2003, 35, 835–845. [Google Scholar] [CrossRef]
- Gupta, M.; Verhoeven, M.; Tiongson, M. Public spending on health care and poor. Health Econ. 2003, 12, 685–696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, S.; Verhoeven, M.; Tiongson, E.R. The effectiveness of government spending on education and health care in developing and transition economies. Eur. J. Polit. Econ. 2002, 18, 717–737. [Google Scholar] [CrossRef]
- Ullah, I.; Ullah, A.; Ali, S.; Poulova, P.; Akbar, A.; Shah, M.H.; Rehman, A.; Zeeshan, M.; Afridi, F. Public Health Expenditures and Health Outcomes in Pakistan: Evidence from Quantile Autoregressive Distributed Lag Model. Risk Manag. Healthc. Policy 2021, 14, 3893. [Google Scholar] [CrossRef]
- Yaqub, J.; Ojapinwa, T.; Yussuff, R. Public health expenditure and health outcome in Nigeria: The impact of governance. Eur. Sci. J. 2012, 8, 198–201. [Google Scholar]
- Aziz, N.; Sharif, A.; Raza, A.; Rong, K. Revisiting the role of forestry, agriculture, and renewable energy in testing environment Kuznets curve in Pakistan: Evidence from Quantile ARDL approach. Environ. Sci. Pollut. Res. 2020, 27, 10115–10128. [Google Scholar] [CrossRef]
- Granger, C.W.J.; Newbold, P. Spurious regressions in econometrics. J. Econ. 1974, 2, 111–120. [Google Scholar] [CrossRef] [Green Version]
- Im, K.S.; Pesaran, M.H.; Shin, Y. Testing for Unit Roots in Heterogeneous Panels. J. Econ. 2003, 115, 53–74. [Google Scholar] [CrossRef]
- Khan, Z.A.; Koondhar, M.A.; Aziz, N.; Ali, U.; Tianjun, L. Revisiting the effects of relevant factors on Pakistan’s agricultural products export. Agric. Econ. 2020, 66, 527–541. [Google Scholar]
- Ahmed, M.; Aziz, N.; Tan, Z.; Yang, S.; Raza, K.; Kong, R. Green growth of cereal food production under the constraints of agricultural carbon emissions: A new insights from ARDL and VECM models. Sustain. Energy Technol. Assess. 2021, 47, 101452. [Google Scholar]
- Si, R.; Aziz, N.; Raza, A. Short and long-run causal effects of agriculture, forestry, and other land use on greenhouse gas emissions: Evidence from China using VECM approach. Environ. Sci. Pollut. Res. 2021, 1–12. [Google Scholar] [CrossRef]
- Pesaran, M.H. A simple panel unit root test in the presence of cross-section dependence. J. Appl. Econom. 2007, 22, 265–312. [Google Scholar] [CrossRef] [Green Version]
- Aziz, N.; Sharif, A.; Raza, A.; Jermsittiparsert, K. The role of natural resources, globalization, and renewable energy in testing the EKC hypothesis in MINT countries: New evidence from Method of Moments Quantile Regression approach. Environ. Sci. Pollut. Res. 2020, 28, 13454–13468. [Google Scholar] [CrossRef]
- Aziz, N.; Mihardjo, L.W.W.; Sharif, A.; Jermsittiparsert, K. The role of tourism and renewable energy in testing the environmental Kuznets curve in the BRICS countries: Fresh evidence from methods of moments quantile regression. Environ. Sci. Pollut. Res. 2020, 27, 39427–39441. [Google Scholar] [CrossRef]
- Pedroni, P. Panel cointegration: Asymptotic and finite sample properties of pooled time series tests with an application to the PPP hypothesis. Econ. Theory 2004, 20, 597–625. [Google Scholar] [CrossRef] [Green Version]
- Raza, A.; Sui, H.; Jermsittiparsert, K.; Zukiewicz-Sobczak, W.; Sobczak, P. Trade liberalization and environmental performance index: Mediation role of climate change performance and greenfield investment. Sustainability 2021, 13, 9734. [Google Scholar] [CrossRef]
- Kao, C.; Chiang, M.H. On the estimation and inference of a cointegrated regression in panel data. In Advances in Econometrics; Baltagi, B.H., Fomby, T.B., Eds.; Emarald: Bradford, UK, 2000; pp. 179–222. [Google Scholar]
- Hausman, J.A. Specification Tests in Econometrics. Econometrica 1978, 46, 1251–1271. [Google Scholar] [CrossRef] [Green Version]
- Haseeb, A.; Xia, E.; Baloch, M.A.; Abbas, K. Financial development, globalization, and CO2 emission in the presence of EKC: Evidence from BRICS countries. Environ. Sci. Pollut. Res. 2018, 25, 31283–31296. [Google Scholar] [CrossRef]
- Dogan, B.; Madaleno, M.; Tiwari, A.K.; Hammoudeh, S. Impacts of export quality on environmental degradation: Does income matter? Environ. Sci. Pollut. Res. 2020, 27, 13735–13772. [Google Scholar] [CrossRef] [PubMed]
- Fokunang, C.N.; Ndikum, V.; Tabi, O.Y.; Jiofack, R.B.; Ngameni, B.; Guedje, N.M.; Tembe-Fokunang, E.A.; Tomkins, P.; Barkwan, S.; Kechia, F.; et al. Traditional medicine: Past, present and future research and development prospects and integration in the National Health System of Cameroon. Afr. J. Tradit. Complement. Altern. Med. 2011, 8, 284–295. [Google Scholar] [CrossRef] [PubMed]
- Anand, S.; Ravallion, M. Human Development in Poor Countries: On the Role of Private Incomes and Public Services. J. Econ. Perspect. 1993, 7, 133–150. [Google Scholar] [CrossRef] [Green Version]
- Rahman, M.; Khanam, R.; Rahman, M. Health care expenditure and health outcome nexus: New evidence from the SAARC-ASEAN region. Glob. Health 2018, 14, 113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zakir, M.; Wunnava, P. Factors affecting infant mortality rates: Evidence from cross-sectional data. Appl. Econ. Lett. 1999, 6, 271–273. [Google Scholar] [CrossRef]
- Nolte, E.; McKee, M. Does Health Care Save Lives? Avoidable Mortality Revisited; The Nuffield Trust: London, UK, 2004. [Google Scholar]
- Bhandari, A. Women’s status and global food security: An overview. Sociol. Compass 2017, 11, e12479. [Google Scholar] [CrossRef]
- Fatema, K.; Lariscy, J.T. Mass Media Exposure and Maternal Healthcare Utilization in South Asia. SSM Popul. Health 2020, 11, 100614. [Google Scholar] [CrossRef] [PubMed]
- Aziz, N.; Ren, Y.; Rong, K.; Zhou, J. Women’s empowerment in agriculture and household food insecurity: Evidence from Azad Jammu & Kashmir (AJK), Pakistan. Land Use Policy 2021, 102, 105249. [Google Scholar]
- Aziz, N.; Nisar, Q.A.; Koondhar, M.A.; Meo, M.S.; Rong, K. Analyzing the women’s empowerment and food security nexus in rural areas of Azad Jammu & Kashmir, Pakistan: By giving consideration to sense of land entitlement and infrastructural facilities. Land Use Policy 2020, 94, 104529. [Google Scholar]
- Wei, W.; Sarker, T.; Zukiewicz-Sobczak, W.; Roy, R.; Alam, G.M.; Rabbany, M.; Hossain, M.S.; Aziz, N. The Influence of Women’s Empowerment on Poverty Reduction in the Rural Areas of Bangladesh: Focus on Health, Education and Living Standard. Int. J. Environ. Res. Public Health 2021, 18, 6909. [Google Scholar] [CrossRef]
- Si, R.; Lu, Q.; Aziz, N. Does the stability of farmland rental contract & conservation tillage adoption improve family welfare? Empirical insights from Zhangye, China. Land Use Policy 2021, 107, 105486. [Google Scholar]
- Joshi, P.K.; Parappurathu, S.; Kumar, P. Dynamics of food consumption and nutrient insecurity in India. Proc. Indian Natl. Sci. Acad. 2016, 82, 1587–1599. [Google Scholar]
- Kumar, A.K.S. Why are levels of child malnutrition not improving? Econ. Polit. Wkly. 2007, 42, 1337–1345. [Google Scholar]
- Bhutta, Z. Pakistan National Nutrition Survey 2011; UNICEF Pakistan: Islamabad, Pakistan, 2012; pp. 1–84. [Google Scholar]
- Headey, D.; Ecker, O. Rethinking the measurement of food security: From first principles to best practice. Food Secur. 2013, 5, 327–343. [Google Scholar] [CrossRef]
- Pritchett, L.; Summers, L. Wealthier is Healthier. J. Hum. Resour. 1996, 31, 841–868. [Google Scholar] [CrossRef]
- Bloom, D.E.; Canning, D.; Kotschy, R.; Prettner, K.; Schünemann, J.J. Health and Economic Growth: Reconciling the Micro and Macro Evidence (No. w26003); National Bureau of Economic Research: Cambridge, MA, USA, 2019. [Google Scholar]
- Botting, M.J.; Porbeni, E.O.; Joffres, M.R.; Johnston, B.C.; Black, R.E.; Mills, E.J. Water and sanitation infrastructure for health: The impact of foreign aid. Glob. Health 2010, 6, 12. [Google Scholar] [CrossRef] [Green Version]
- Wayland, J. A Drop in the Bucket? The Effectiveness of Foreign Aid in the Water, Sanitation, and Hygiene (WASH) Sector; American University: Washington, DC, USA, 2013. [Google Scholar]
- Esrey, S.A.; Habicht, J.P.; Latham, M.C.; Sisler, D.G.; Casella, G. Drinking water source, diarrheal morbidity, and child growth in villages with both traditional and improved water supplies in rural Lesotho, southern Africa. Am. J. Public Health 1988, 78, 1451–1455. [Google Scholar] [CrossRef] [Green Version]
- Fewtrell, L.; Kaufmann, R.B.; Kay, D.; Enanoria, W.; Haller, L.; Colford, J.M. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: A systematic review and meta-analysis. Lancet Infect. Dis. 2005, 5, 42–52. [Google Scholar] [CrossRef]
- Fink, G.; Günther, I.; Hill, K. The effect of water and sanitation on child health: Evidence from the demographic and health surveys 1986–2007. Int. J. Epidemiol. 2011, 40, 1196–1204. [Google Scholar] [CrossRef] [Green Version]
- Pickbourn, L.; Ndikumana, L. Does Health Aid Reduce Infant and Child Mortality from Diarrhoea in Sub-Saharan Africa? J. Dev Stud. 2019, 55, 2212–2231. [Google Scholar] [CrossRef]
- Irfan, M. Poverty in South Asia. Pak. Dev. Rev. 2000, 39, 1141–1151. [Google Scholar] [CrossRef] [Green Version]
| Maternal Mortality | Health Expenditure | Economic Growth | Population | Clean Fuel Technologies | Basic Sanitation | |
|---|---|---|---|---|---|---|
| Mean | 312.4028 | 105.0910 | 24.18627 | 1.834289 | 32.16650 | 53.63868 |
| Median | 236.5000 | 40.11737 | 24.24980 | 1.562703 | 26.56000 | 48.65390 |
| Maximum | 1450.000 | 946.8112 | 28.60913 | 4.668361 | 94.56000 | 99.37300 |
| Minimum | 36.00000 | 8.362380 | 20.31048 | −0.266960 | 7.240000 | 15.12425 |
| Std. Dev. | 302.9920 | 184.0360 | 2.209372 | 1.067289 | 20.24544 | 23.83500 |
| Skewness | 1.957352 | 2.931312 | 0.159694 | 0.850876 | 1.503814 | 0.484218 |
| Kurtosis | 6.467059 | 10.90132 | 2.181728 | 3.393813 | 4.979517 | 2.010786 |
| Jarque–Bera | 164.0724 | 580.8078 | 4.629465 | 18.30628 | 77.24570 | 11.49848 |
| Probability | 0.000000 | 0.000000 | 0.098793 | 0.000106 | 0.000000 | 0.003185 |
| Variable | Im, Pesaran, and Shin | |||
|---|---|---|---|---|
| I (0) | I (1) | |||
| Intercept | Intercept with Trend | Intercept | Intercept with Trend | |
| Maternal Mortality | −3.44394 *** | 1.28452 | −3.37734 *** | −6.50037 *** |
| Health Expenditure | 6.53287 | −1.45462 * | −5.33655 *** | −5.31860 *** |
| Economic Growth | 1.32175 | −20.9478 *** | −33.4276 *** | −30.2320 *** |
| Population | −3.65753 *** | −7.00708 *** | −9.68864 *** | −12.4179 *** |
| Basic Sanitation | 5.17881 | 1.69497 | −4.75597 *** | −17.7165 *** |
| Clean Technologies | 3.39259 | 1.21140 | −4.34171 *** | −9.37003 *** |
| Variables | CD Test | p-Value | CIPS Test | |
|---|---|---|---|---|
| Level | First Difference | |||
| Maternal Mortality | 22.01677 | 0.000 | −2.606 *** | −4.253 *** |
| Health Expenditure | 21.45441 | 0.000 | −0.909 | −3.654 *** |
| Economic Growth | 16.55560 | 0.000 | −2.653 *** | −4.603 *** |
| Population | 5.181234 | 0.000 | −3.334 *** | −1.659 *** |
| Basic Sanitation | 22.39049 | 0.000 | −0.451 | −2.028 * |
| Clean Technologies | 21.89715 | 0.000 | −0.269 | −3.935 *** |
| MMR = f (HE+ LNGDP + POP + BS+ CT) | ||
|---|---|---|
| Estimates | Stats. | Prob. |
| Panel v-statistics | −0.4468 | 0.673 |
| Panel rho-statistics | 2.04059 | 0.979 |
| Panel PP-statistics | −11.393 | 0.000 |
| Panel ADF-statistics | −6.6653 | 0.000 |
| Alternative hypothesis: individual AR coefficient | ||
| Group rho-statistic | 2.97338 | 0.999 |
| Group PP-statistic | −14.826 | 0.000 |
| Group ADF-statistic | −3.5834 | 0.002 |
| Fixed Effect | Random Effect | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Coefficient | Std. Error | T-Stat | p-Value | Coefficient | Std. Error | T-Stat | p-Value |
| Health Expenditure | 0.4347 | 0.1183 | 3.67 | 0.000 | 0.4284 | 0.1190 | 3.6 | 0.000 |
| Economic Growth | 58.853 | 13.533 | 4.35 | 0.000 | 44.911 | 12.554 | 3.58 | 0.000 |
| Population | 71.887 | 12.736 | 5.64 | 0.000 | 72.051 | 12.923 | 5.58 | 0.000 |
| Basic Sanitation | −4.415 | 1.0606 | −4.16 | 0.000 | −4.258 | 1.0396 | −4.1 | 0.000 |
| Clean Fuel Technologies | −8.577 | 1.4936 | −5.74 | 0.000 | −8.273 | 1.4802 | −5.59 | 0.000 |
| Constant | −775.0 | 320.65 | −2.42 | 0.017 | −456.6 | 308.21 | −1.48 | 0.138 |
| R2 | 0.2783 | R2 | 0.3399 | |||||
| Prob > F | 0.0000 | Prob > chi-sq | 0.0000 | |||||
| Hausman test Prob > chi2 | 0.0000 |
| FMOLS | DOLS | |||||
|---|---|---|---|---|---|---|
| Variables | Coefficient | Std. Error | T-Stat | Coefficient | Std. Error | T-Stat |
| Health Expenditure | 1.9592 *** | 0.1910 | 10.255 | 0.1675 ** | 0.0803 | 2.0813 |
| Economic Growth | −94.264 *** | 26.727 | −3.526 | −18.22 | 13.392 | −1.360 |
| Population | 40.640 *** | 7.3916 | 5.4981 | 10.61 ** | 4.9330 | 2.1513 |
| Basic Sanitation | −7.2306 ** | 3.2193 | −2.245 | −1.960 ** | 0.8554 | −2.291 |
| Clean Fuel Technologies | −11.581 *** | 1.4931 | −7.756 | −5.691 *** | 1.0351 | −5.498 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aziz, N.; He, J.; Sarker, T.; Sui, H. Exploring the Role of Health Expenditure and Maternal Mortality in South Asian Countries: An Approach towards Shaping Better Health Policy. Int. J. Environ. Res. Public Health 2021, 18, 11514. https://doi.org/10.3390/ijerph182111514
Aziz N, He J, Sarker T, Sui H. Exploring the Role of Health Expenditure and Maternal Mortality in South Asian Countries: An Approach towards Shaping Better Health Policy. International Journal of Environmental Research and Public Health. 2021; 18(21):11514. https://doi.org/10.3390/ijerph182111514
Chicago/Turabian StyleAziz, Noshaba, Jun He, Tanwne Sarker, and Hongguang Sui. 2021. "Exploring the Role of Health Expenditure and Maternal Mortality in South Asian Countries: An Approach towards Shaping Better Health Policy" International Journal of Environmental Research and Public Health 18, no. 21: 11514. https://doi.org/10.3390/ijerph182111514
APA StyleAziz, N., He, J., Sarker, T., & Sui, H. (2021). Exploring the Role of Health Expenditure and Maternal Mortality in South Asian Countries: An Approach towards Shaping Better Health Policy. International Journal of Environmental Research and Public Health, 18(21), 11514. https://doi.org/10.3390/ijerph182111514






