A Scoping Review Investigating Relationships between Depression, Anxiety, and the PrEP Care Continuum in the United States
Abstract
:1. Introduction
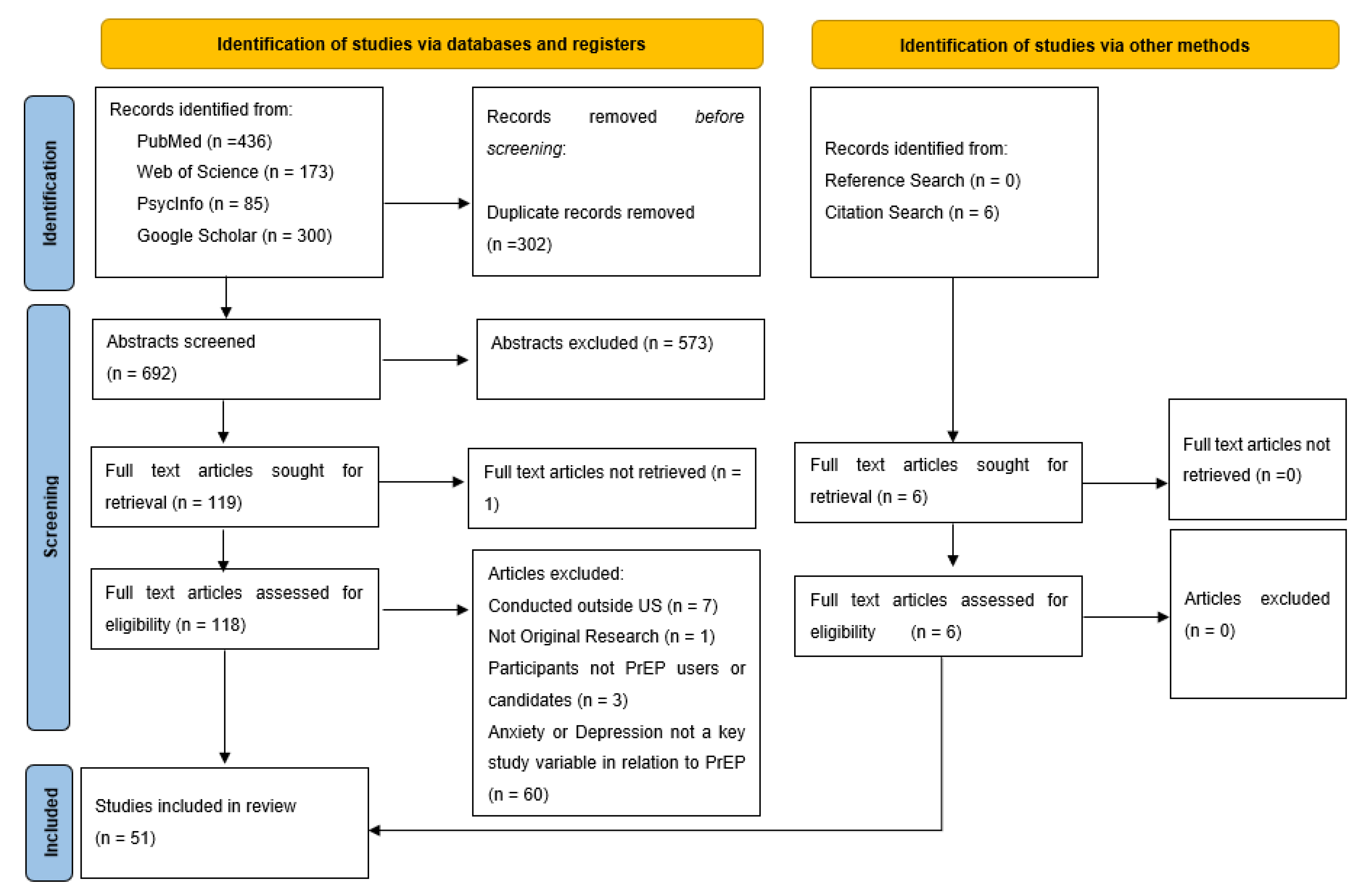
2. Materials and Methods
3. Results
4. Depression
4.1. PrEP Awareness
4.2. PrEP Uptake
4.3. PrEP Adherence and Retention
5. Anxiety
5.1. PrEP Awareness
5.2. PrEP Uptake
5.3. PrEP Adherence and Retention
5.4. Effects of PrEP Use on Anxiety
6. Discussion
6.1. Current Gaps and Future Directions
6.2. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- CDC HIV Basic Statistics. Available online: https://www.cdc.gov/hiv/basics/statistics.html (accessed on 27 July 2021).
- Fauci, A.S.; Redfield, R.R.; Sigounas, G.; Weahkee, M.D.; Giroir, B.P. Ending the HIV epidemic: A plan for the United States. JAMA 2019, 321, 844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC HIV Special Focus Profiles. Available online: https://www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-32/content/special-focus-profiles.html (accessed on 7 September 2021).
- Clark, H.; Babu, A.S.; Wiewel, E.W.; Opoku, J.; Crepaz, N. Diagnosed HIV infection in transgender adults and adolescents: Results from the national HIV surveillance system, 2009–2014. AIDS Behav. 2017, 21, 2774–2783. [Google Scholar] [CrossRef] [Green Version]
- Becasen, J.S.; Denard, C.L.; Mullins, M.M.; Higa, D.H.; Sipe, T.A. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: A systematic review and meta-analysis, 2006–2017. Am. J. Public Health 2019, 109, e1–e8. [Google Scholar] [CrossRef]
- HIV.gov Pre-Exposure Prophylaxis. Available online: https://www.hiv.gov/hiv-basics/hiv-prevention/using-hiv-medication-to-reduce-risk/pre-exposure-prophylaxis (accessed on 9 September 2021).
- Choopanya, K.; Martin, M.; Suntharasamai, P.; Sangkum, U.; Mock, P.A.; Leethochawalit, M.; Chiamwongpaet, S.; Kitisin, P.; Natrujirote, P.; Kittimunkong, S.; et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir study): A randomised, double-blind, placebo-controlled phase 3 trial. Lancet 2013, 381, 2083–2090. [Google Scholar] [CrossRef]
- Martin, M.; Vanichseni, S.; Suntharasamai, P.; Sangkum, U.; Mock, P.A.; Leethochawalit, M.; Chiamwongpaet, S.; Curlin, M.E.; Na-Pompet, S.; Warapronmongkholkul, A.; et al. The impact of adherence to preexposure prophylaxis on the risk of HIV infection among people who inject drugs. AIDS 2015, 29, 819–824. [Google Scholar] [CrossRef] [PubMed]
- FDA Truvada for PrEP Fact Sheet. Available online: https://www.fda.gov/media/83586/download. (accessed on 9 September 2021).
- HIV.gov Long-Acting HIV Prevention Tools. Available online: https://www.hiv.gov/hiv-basics/hiv-prevention/potential-future-options/long-acting-prep (accessed on 13 September 2021).
- Landovitz, R.J.; Donnell, D.; Clement, M.E.; Hanscom, B.; Cottle, L.; Coelho, L.; Cabello, R.; Chariyalertsak, S.; Dunne, E.F.; Frank, I.; et al. Cabotegravir for HIV prevention in cisgender men and transgender women. New Engl. J. Med. 2021, 385, 595–608. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention Preexposure Prophylaxis for the Prevention of HIV Infection in the United States—2017 Update: A Clinical Practice Guideline 2017. Available online: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. (accessed on 9 September 2021).
- Nunn, A.S.; Brinkley-Rubinstein, L.; Oldenburg, C.E.; Mayer, K.H.; Mimiaga, M.; Patel, R.; Chan, P.A. Defining the HIV pre-exposure prophylaxis care continuum. AIDS 2017, 31, 731–734. [Google Scholar] [CrossRef] [Green Version]
- Parsons, J.T.; Rendina, H.J.; Lassiter, J.M.; Whitfield, T.H.F.; Starks, T.J.; Grov, C. Uptake of HIV Pre-Exposure Prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States: The motivational PrEP cascade. J. Acquir. Immune Defic. Syndr. 2017, 74, 285–292. [Google Scholar] [CrossRef] [Green Version]
- Kamitani, E.; Johnson, W.D.; Wichser, M.E.; Adegbite, A.H.; Mullins, M.M.; Sipe, T.A. Growth in proportion and disparities of HIV PrEP use among key populations identified in the United States national goals: Systematic review and meta-analysis of published surveys. J. Acquir. Immune Defic. Syndr. 2020, 84, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Bush, S.; Magnuson, D.; Rawlings, M.K.; Hawkins, T.; McCallister, S.; Mera Giler, R. Racial characteristics of FTC/TDF for Pre-Exposure Prophylaxis (PrEP) users in the US. ASM Microbe/ICAAC 2016, 16, 16. [Google Scholar]
- Golub, S.A.; Gamarel, K.E.; Rendina, H.J.; Surace, A.; Lelutiu-Weinberger, C.L. From efficacy to effectiveness: Facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care STDS 2013, 27, 248–254. [Google Scholar] [CrossRef] [Green Version]
- Rowniak, S.; Ong-Flaherty, C.; Selix, N.; Kowell, N. Attitudes, beliefs, and barriers to PrEP among trans men. AIDS Educ. Prev. 2017, 29, 302–314. [Google Scholar] [CrossRef] [Green Version]
- Bauermeister, J.A.; Meanley, S.; Pingel, E.; Soler, J.H.; Harper, G.W. PrEP awareness and perceived barriers among single young men who have sex with men in the United States. Curr. HIV Res. 2013, 11, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Meyer, I.H. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol. Bull. 2003, 129, 674–697. [Google Scholar] [CrossRef] [PubMed]
- Hasin, D.S.; Sarvet, A.L.; Meyers, J.L.; Saha, T.D.; Ruan, W.J.; Stohl, M.; Grant, B.F. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry 2018, 75, 336–346. [Google Scholar] [CrossRef] [Green Version]
- Meyer, I.H.; Dietrich, J.; Schwartz, S. Lifetime prevalence of mental disorders and suicide attempts in diverse lesbian, gay, and bisexual populations. Am. J. Public Health 2008, 98, 1004–1006. [Google Scholar] [CrossRef]
- Budge, S.L.; Adelson, J.L.; Howard, K.A.S. Anxiety and depression in transgender individuals: The roles of transition status, loss, social support, and coping. J. Consult. Clin. Psychol. 2013, 81, 545–557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kessler, R.C.; Petukhova, M.; Sampson, N.A.; Zaslavsky, A.M.; Wittchen, H.-U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int. J. Methods Psychiatr. Res. 2012, 21, 169–184. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection 2016 Recommendations for a Public Health Approach; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Remien, R.H.; Stirratt, M.J.; Nguyen, N.; Robbins, R.N.; Pala, A.N.; Mellins, C.A. Mental health and HIV/AIDS: The need for an integrated response. AIDS 2019, 33, 1411. [Google Scholar] [CrossRef]
- Remien, R.H.; Patel, V.; Chibanda, D.; Abas, M.A. Integrating mental health into HIV prevention and care: A call to action. J. Int. AIDS Soc. 2021, 24, e25748. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [Green Version]
- Peters, M.D.J.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. JBI Evid. Implement. 2015, 13, 141–146. [Google Scholar] [CrossRef] [Green Version]
- Haddaway, N.R.; Collins, A.M.; Coughlin, D.; Kirk, S. The role of Google Scholar in evidence reviews and its applicability to grey literature searching. PLoS ONE 2015, 10, e0138237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Eaton, L.A.; Matthews, D.D.; Driffin, D.D.; Bukowski, L.; Wilson, P.A.; Stall, R.D. A multi-US city assessment of awareness and uptake of Pre-Exposure Prophylaxis (PrEP) for HIV prevention among black men and transgender women who have sex with men. Prev. Sci. 2017, 18, 505–516. [Google Scholar] [CrossRef] [PubMed]
- Friedman, M.R.; Sang, J.M.; Bukowski, L.A.; Chandler, C.J.; Egan, J.E.; Eaton, L.A.; Matthews, D.D.; Ho, K.; Raymond, H.F.; Stall, R. Prevalence and correlates of PrEP awareness and use among black men who have sex with men and women (MSMW) in the United States. AIDS Behav. 2019, 23, 2694–2705. [Google Scholar] [CrossRef]
- Krakower, D.S.; Mimiaga, M.J.; Rosenberger, J.G.; Novak, D.S.; Mitty, J.A.; White, J.M.; Mayer, K.H. Limited awareness and low immediate uptake of pre-exposure prophylaxis among men who have sex with men using an internet social networking site. PLoS ONE 2012, 7, e33119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Brown, L.; Przybyla, S.; Bleasdale, J.; Mitchell, J.; Zhang, C. Characterizing racial differences of mental health burdens, psychosocial determinants, and impacts on HIV prevention outcomes among young men who have sex with men: A community-based study in two, U.S. Cities. J. Racial Ethn. Health Disparities 2021, 1–11. [Google Scholar] [CrossRef]
- Sullivan, M.C.; Eaton, L.A. Intersecting barriers to PrEP awareness and uptake in black men who have sex with men in Atlanta, GA: A syndemic perspective. Int. J. Behav. Med. 2020, 28, 349–359. [Google Scholar] [CrossRef]
- Ni, Z.; Altice, F.L.; Wickersham, J.A.; Copenhaver, M.M.; DiDomizio, E.E.; Nelson, L.E.; Shrestha, R. Willingness to initiate Pre-Exposure Prophylaxis (PrEP) and its use among opioid-dependent individuals in drug treatment. Drug Alcohol Depend. 2021, 219, 108477. [Google Scholar] [CrossRef] [PubMed]
- Tomko, C.; Park, J.N.; Allen, S.T.; Glick, J.; Galai, N.; Decker, M.R.; Footer, K.H.; Sherman, S.G. Awareness and interest in HIV pre-exposure prophylaxis among street-based female sex workers: Results from a US context. AIDS Patient care STDs 2019, 33, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Blackstock, O.J.; Platt, J.; Golub, S.A.; Anakaraonye, A.R.; Norton, B.L.; Walters, S.M.; Sevelius, J.M.; Cunningham, C.O. A pilot study to evaluate a novel pre-exposure prophylaxis peer outreach and navigation intervention for women at high risk for HIV infection. AIDS Behav. 2021, 25, 1411–1422. [Google Scholar] [CrossRef] [PubMed]
- Bologna, E.S.; Panesar-Aguilar, S.; McCraney, M.; Cale, C. Evaluating HIV risk factors and willingness to use prep among African American collegiate women. Am. Int. J. Contemp. Res. 2020, 10, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Blashill, A.J.; Brady, J.P.; Rooney, B.M.; Rodriguez-Diaz, C.E.; Horvath, K.J.; Blumenthal, J.; Morris, S.; Moore, D.J.; Safren, S.A. Syndemics and the PrEP cascade: Results from a sample of young latino men who have sex with men. Arch. Sex. Behav. 2020, 49, 125–135. [Google Scholar] [CrossRef] [Green Version]
- Kuo, I.; Olsen, H.; Patrick, R.; Phillips, G., 2nd; Magnus, M.; Opoku, J.; Rawls, A.; Peterson, J.; Hamilton, F.; Kharfen, M.; et al. Willingness to Use HIV pre-exposure prophylaxis among community-recruited, older people who inject drugs in Washington, DC. Drug Alcohol Depend. 2016, 164, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Ojikutu, B.O.; Bogart, L.M.; Higgins-Biddle, M.; Dale, S.K.; Allen, W.; Dominique, T.; Mayer, K.H. Facilitators and barriers to Pre-Exposure Prophylaxis (PrEP) use among black individuals in the United States: Results from the National Survey on HIV in the Black Community (NSHBC). AIDS Behav. 2018, 22, 3576–3587. [Google Scholar] [CrossRef]
- Shrestha, R.; DiDomizio, E.E.; Kim, R.S.; Altice, F.L.; Wickersham, J.A.; Copenhaver, M.M. Awareness about and willingness to use Long-Acting Injectable Pre-Exposure Prophylaxis (LAI-PrEP) among people who use drugs. J. Subst. Abuse Treat. 2020, 117, 108058. [Google Scholar] [CrossRef]
- Shrestha, R.; Karki, P.; Altice, F.L.; Huedo-Medina, T.B.; Meyer, J.P.; Madden, L.; Copenhaver, M. Correlates of willingness to initiate pre-exposure prophylaxis and anticipation of practicing safer drug- and sex-related behaviors among high-risk drug users on methadone treatment. Drug Alcohol Depend. 2017, 173, 107–116. [Google Scholar] [CrossRef] [Green Version]
- Willie, T.C.; Kershaw, T.S.; Blackstock, O.; Galvao, R.W.; Safon, C.B.; Tekeste, M.; Ogburn, D.F.; Wilbourn, B.; Modrakovic, D.; Taggart, T.; et al. Racial and ethnic differences in women’s HIV risk and attitudes towards pre-exposure prophylaxis (prep) in the context of the substance use, violence, and depression syndemic. AIDS Care 2021, 33, 219–228. [Google Scholar] [CrossRef]
- Ogunbajo, A.; Storholm, E.D.; Ober, A.J.; Bogart, L.M.; Reback, C.J.; Flynn, R.; Lyman, P.; Morris, S. Multilevel barriers to HIV prep uptake and adherence among black and hispanic/latinx transgender women in Southern California. AIDS Behav. 2021, 25, 2301–2315. [Google Scholar] [CrossRef] [PubMed]
- Watson, C.W.-M.; Pasipanodya, E.; Savin, M.J.; Ellorin, E.E.; Corado, K.C.; Flynn, R.P.; Opalo, C.; Lampley, E.; Henry, B.L.; Blumenthal, J.; et al. Barriers and facilitators to PrEP initiation and adherence among transgender and gender non-binary individuals in Southern California. AIDS Educ. Prev. 2020, 32, 472–485. [Google Scholar] [CrossRef]
- Laborde, N.D.; Kinley, P.M.; Spinelli, M.; Vittinghoff, E.; Whitacre, R.; Scott, H.M.; Buchbinder, S.P. Understanding prep persistence: Provider and patient perspectives. AIDS Behav. 2020, 24, 2509–2519. [Google Scholar] [CrossRef] [PubMed]
- Rutledge, R.; Madden, L.; Ogbuagu, O.; Meyer, J.P. HIV risk perception and eligibility for pre-exposure prophylaxis in women involved in the criminal justice system. AIDS Care 2018, 30, 1282–1289. [Google Scholar] [CrossRef]
- Bruxvoort, K.J.; Schumacher, C.M.; Towner, W.; Jones, J.; Contreras, R.; Grant, D.L.; Hechter, R.C. Referral linkage to preexposure prophylaxis care and persistence on preexposure prophylaxis in an integrated health care system. JAIDS J. Acquir. Immune Defic. Syndr. 2021, 87, 918–927. [Google Scholar] [PubMed]
- Serota, D.P.; Rosenberg, E.S.; Thorne, A.L.; Sullivan, P.S.; Kelley, C.F. Lack of health insurance is associated with delays in PrEP initiation among young black men who have sex with men in Atlanta, US: A longitudinal cohort study. J. Int. AIDS Soc. 2019, 22, e25399. [Google Scholar] [CrossRef]
- Serota, D.P.; Rosenberg, E.S.; Sullivan, P.S.; Thorne, A.L.; Rolle, C.-P.M.; Del Rio, C.; Cutro, S.; Luisi, N.; Siegler, A.J.; Sanchez, T.H.; et al. Pre-exposure prophylaxis uptake and discontinuation among young black men who have sex with men in Atlanta, Georgia: A prospective cohort study. Clin. Infect. Dis 2020, 71, 574–582. [Google Scholar] [CrossRef]
- Wheeler, D.P.; Fields, S.D.; Beauchamp, G.; Chen, Y.Q.; Emel, L.M.; Hightow-Weidman, L.; Hucks-Ortiz, C.; Kuo, I.; Lucas, J.; Magnus, M. Pre-exposure prophylaxis initiation and adherence among black men who have sex with men (MSM) in three US cities: Results from the HPTN 073 study. J. Int. AIDS Soc. 2019, 22, e25223. [Google Scholar] [CrossRef] [Green Version]
- Okafor, C.N.; Hucks-Ortiz, C.; Hightow-Weidman, L.B.; Magnus, M.; Emel, L.; Beauchamp, G.; Kuo, I.; Hendrix, C.; Mayer, K.H.; Shoptaw, S.J. Brief report: Associations between self-reported substance use behaviors and PrEP acceptance and adherence among black MSM in the HPTN 073 study. J. Acquir. Immune Defic. Syndr. 2020, 85, 23–29. [Google Scholar] [CrossRef]
- Sewell, W.C.; Powell, V.E.; Mayer, K.H.; Ochoa, A.; Krakower, D.S.; Marcus, J.L. Nondaily use of HIV preexposure prophylaxis in a large online survey of primarily men who have sex with men in the United States. J. Acquir. Immune Defic. Syndr. 2020, 84, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Wood, S.M.; Morales, K.H.; Metzger, D.; Davis, A.; Fiore, D.; Petsis, D.; Barnett, K.; Koenig, H.C.; Dowshen, N.; Gross, R.; et al. Mental health, social influences, and HIV pre-exposure prophylaxis (prep) utilization among men and transgender individuals screening for HIV prevention trials. AIDS Behav. 2020, 25, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, P.B.; Westmoreland, D.A.; Patel, V.V.; Grov, C. Factors associated with being PrEP-naïve among a US National cohort of former-PrEP and PrEP-naïve participants meeting objective criteria for PrEP care. Arch. Sex. Behav. 2021, 50, 1793–1803. [Google Scholar] [CrossRef]
- Chandler, C.J.; Bukowski, L.A.; Matthews, D.D.; Hawk, M.E.; Markovic, N.; Stall, R.D.; Egan, J.E. Understanding the impact of a syndemic on the use of pre-exposure prophylaxis in a community-based sample of behaviorally PrEP-eligible BMSM in the United States. AIDS Care 2020, 32, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Eaton, L.A.; Matthews, D.D.; Bukowski, L.A.; Friedman, M.R.; Chandler, C.J.; Whitfield, D.L.; Sang, J.M.; Stall, R.D.; POWER Study Team. Elevated HIV prevalence and correlates of PrEP use among a community sample of black men who have sex with men. J. Acquir. immune Defic. Syndr. 2018, 79, 339. [Google Scholar] [CrossRef]
- Moeller, R.W.; Seehuus, M.; Wahl, L.; Gratch, I. Use of prep, sexual behaviors and mental health correlates in a sample of gay, bisexual and other men who have sex with men. J. Gay Lesbian Ment. Health 2020, 24, 94–111. [Google Scholar] [CrossRef]
- Young, L.B.; Lalley-Chareczko, L.; Clark, D.; Ramos, M.T.; Nahan, R.A.; Troutman, G.S.; Cantor, R.; DiFlavis, L.; Koenig, H.C. Correlation of pre-exposure prophylaxis adherence to a mental health diagnosis or experience of childhood trauma in high-risk youth. Int. J. STD AIDS 2020, 31, 440–446. [Google Scholar] [CrossRef]
- Gandhi, M.; Murnane, P.M.; Bacchetti, P.; Elion, R.; Kolber, M.A.; Cohen, S.E.; Horng, H.; Louie, A.; Kuncze, K.; Koss, C.A. Hair levels of preexposure prophylaxis drugs measure adherence and are associated with renal decline among men/transwomen. Aids 2017, 31, 2245–2251. [Google Scholar] [CrossRef] [PubMed]
- Liu, A.Y.; Cohen, S.E.; Vittinghoff, E.; Anderson, P.L.; Doblecki-Lewis, S.; Bacon, O.; Chege, W.; Postle, B.S.; Matheson, T.; Amico, K.R. Preexposure prophylaxis for HIV infection integrated with municipal-and community-based sexual health services. JAMA Intern. Med. 2016, 176, 75–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoenigl, M.; Jain, S.; Moore, D.; Collins, D.; Sun, X.; Anderson, P.L.; Corado, K.; Blumenthal, J.S.; Daar, E.S.; Milam, J.; et al. Substance use and adherence to HIV preexposure prophylaxis for men who have sex with men. Emerg. Infect. Dis. 2018, 24, 2292–2302. [Google Scholar] [CrossRef] [PubMed]
- Mannheimer, S.; Hirsch-Moverman, Y.; Franks, J.; Loquere, A.; Hughes, J.P.; Li, M.; Amico, K.R.; Grant, R.M. Factors associated with sex-related pre-exposure prophylaxis adherence among men who have sex with men in New York City in HPTN 067. J. Acquir. immune Defic. Syndr. 2019, 80, 551. [Google Scholar] [CrossRef]
- Colson, P.W.; Franks, J.; Wu, Y.; Winterhalter, F.S.; Knox, J.; Ortega, H.; El-Sadr, W.M.; Hirsch-Moverman, Y. Adherence to pre-exposure prophylaxis in black men who have sex with men and transgender women in a community setting in Harlem, NY. AIDS Behav. 2020, 24, 3436–3455. [Google Scholar] [CrossRef] [PubMed]
- Pasipanodya, E.C.; Jain, S.; Sun, X.; Blumenthal, J.; Ellorin, E.; Corado, K.; Dube, M.P.; Daar, E.S.; Morris, S.R.; Moore, D.J.; et al. Trajectories and predictors of longitudinal preexposure prophylaxis adherence among men who have sex with men. J. Infect. Dis. 2018, 218, 1551–1559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spinelli, M.A.; Laborde, N.; Kinley, P.; Whitacre, R.; Scott, H.M.; Walker, N.; Liu, A.Y.; Gandhi, M.; Buchbinder, S.P. Missed opportunities to prevent HIV infections among pre-exposure prophylaxis users: A population-based mixed methods study, San Francisco, United States. J. Int. AIDS Soc. 2020, 23, e25472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krakower, D.; Maloney, K.M.; Powell, V.E.; Levine, K.; Grasso, C.; Melbourne, K.; Marcus, J.L.; Mayer, K.H. Patterns and clinical consequences of discontinuing HIV preexposure prophylaxis during primary care. J. Int. AIDS Soc. 2019, 22, e25250. [Google Scholar] [CrossRef]
- Scott, H.M.; Spinelli, M.; Vittinghoff, E.; Morehead-Gee, A.; Hirozawa, A.; James, C.; Hammer, H.; Liu, A.; Gandhi, M.; Buchbinder, S. Racial/ethnic and HIV risk category disparities in preexposure prophylaxis discontinuation among patients in publicly funded primary care clinics. Aids 2019, 33, 2189–2195. [Google Scholar] [CrossRef] [PubMed]
- Zucker, J.; Carnevale, C.; Richards, P.; Slowikowski, J.; Borsa, A.; Gottlieb, F.; Vakkur, I.; Hyden, C.; Olender, S.; Cohall, A.; et al. Predictors of disengagement in care for individuals receiving Pre-Exposure Prophylaxis (PrEP). JAIDS-J. Acquir. Immune Defic. Syndr. 2019, 81, E104–E108. [Google Scholar] [CrossRef] [PubMed]
- Meyers, K.; Rodriguez, K.; Brill, A.L.; Wu, Y.; La Mar, M.; Dunbar, D.; Koblin, B.; Margolis, D.; Sobieszczyk, M.E.; Van Tieu, H.; et al. Lessons for patient education around long-acting injectable PrEP: Findings from a mixed-method study of phase II trial participants. AIDS Behav. 2017, 22, 1209–1216. [Google Scholar] [CrossRef] [PubMed]
- Hojilla, J.C.; Koester, K.A.; Cohen, S.E.; Buchbinder, S.; Ladzekpo, D.; Matheson, T.; Liu, A.Y. Sexual behavior, risk compensation, and HIV prevention strategies among participants in the San Francisco PrEP demonstration project: A qualitative analysis of counseling notes. AIDS Behav. 2016, 20, 1461–1469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zapata, J.P.; Petroll, A.; de St. Aubin, E.; Quinn, K. Perspectives on social support and stigma in prep-related care among gay and bisexual men: A qualitative investigation. J. Homosex. 2020, 1–23. [Google Scholar] [CrossRef]
- Devarajan, S.; Sales, J.M.; Hunt, M.; Comeau, D.L. PrEP and sexual well-being: A qualitative study on PrEP, sexuality of MSM, and patient-provider relationships. AIDS Care 2020, 32, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Mutchler, M.G.; McDavitt, B.; Ghani, M.A.; Nogg, K.; Winder, T.J.A.; Soto, J.K. Getting prepared for HIV prevention navigation: Young black gay men talk about HIV prevention in the biomedical era. AIDS Patient Care STDs 2015, 29, 490–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hammack, P.L.; Toolis, E.E.; Wilson, B.D.M.; Clark, R.C.; Frost, D.M. Making meaning of the impact of Pre-Exposure Prophylaxis (PrEP) on public health and sexual culture: Narratives of three generations of gay and bisexual men. Arch. Sex. Behav. 2019, 48, 1041–1058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quinn, K.G.; Christenson, E.; Sawkin, M.T.; Hacker, E.; Walsh, J.L. The unanticipated benefits of PrEP for young black gay, bisexual, and other men who have sex with men. AIDS Behav. 2020, 24, 1376–1388. [Google Scholar] [CrossRef] [PubMed]
- Storholm, E.D.; Volk, J.E.; Marcus, J.L.; Silverberg, M.J.; Satre, D.D. Risk perception, sexual behaviors, and PrEP adherence among substance-using men who have sex with men: A qualitative study. Prev. Sci. 2017, 18, 737–747. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Krishnan, N.; Kelley, E.; Dawkins, J.; Akolo, O.; Redd, R.; Olawale, A.; Max-Browne, C.; Johnsen, L.; Latkin, C. Beyond HIV prevention: A qualitative study of patient-reported outcomes of PrEP among MSM patients in two public STD clinics in Baltimore. AIDS Care 2020, 32, 238–241. [Google Scholar] [CrossRef]
- Mitchell, J.W.; Lee, J.-Y.; Woodyatt, C.; Bauermeister, J.; Sullivan, P.; Stephenson, R. HIV-negative male couples’ attitudes about Pre-Exposure Prophylaxis (PrEP) and using PrEP with a sexual agreement. AIDS Care 2016, 28, 994–999. [Google Scholar] [CrossRef] [Green Version]
- Brooks, R.A.; Landovitz, R.J.; Kaplan, R.L.; Lieber, E.; Lee, S.-J.; Barkley, T.W. Sexual risk behaviors and acceptability of HIV pre-exposure prophylaxis among HIV-negative gay and bisexual men in serodiscordant relationships: A mixed methods study. AIDS Patient Care STDs 2012, 26, 87–94. [Google Scholar] [CrossRef] [Green Version]
- Whitfield, T.H.F.; Jones, S.S.; Wachman, M.; Grov, C.; Parsons, J.T.; Rendina, H.J. The impact of Pre-Exposure Prophylaxis (PrEP) use on sexual anxiety, satisfaction, and esteem among gay and bisexual men. J. Sex. Res. 2019, 56, 1128–1135. [Google Scholar] [CrossRef]
- Scheer, J.R.; Pachankis, J.E. Psychosocial syndemic risks surrounding physical health conditions among sexual and gender minority individuals. LGBT Health 2019, 6, 377–385. [Google Scholar] [CrossRef]
- Mustanski, B.; Garofalo, R.; Herrick, A.; Donenberg, G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: Preliminary evidence of a syndemic in need of attention. Ann. Behav. Med. 2007, 34, 37–45. [Google Scholar] [CrossRef]
- Singer, M.C.; Erickson, P.I.; Badiane, L.; Diaz, R.; Ortiz, D.; Abraham, T.; Nicolaysen, A.M. Syndemics, sex and the city: Understanding sexually transmitted diseases in social and cultural context. Soc. Sci. Med. 2006, 63, 2010–2021. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, M.L.; Glidden, D.V.; McMahan, V.; Amico, K.R.; Hosek, S.; Defechereux, P.; Mayer, K.H.; Veloso, V.G.; Bekker, L.-G.; Avelino-Silva, V.I.; et al. The Effect of depressive symptoms on adherence to daily oral PrEP in men who have sex with men and transgender women: A marginal structural model analysis of the IPrEx OLE study. AIDS Behav. 2016, 20, 1527–1534. [Google Scholar] [CrossRef] [Green Version]
- Rojas Castro, D.; Delabre, R.M.; Molina, J. Give PrEP a chance: Moving on from the “Risk Compensation” concept. J. Int. AIDS Soc. 2019, 22, e25351. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Center for Disease Control & Prevention HIV in the Southern United States 2019. Available online: https://www.cdc.gov/hiv/pdf/policies/cdc-hiv-in-the-south-issue-brief.pdf (accessed on 16 September 2021).
- Center for Disease Control and Prevention HIV in the United States by Region. 2020. Available online: https://www.cdc.gov/hiv/statistics/overview/geographicdistribution.html (accessed on 27 September 2021).
- Reif, S.; Safley, D.; McAllaster, C.; Wilson, E.; Whetten, K. State of HIV in the US deep south. J. Community Health 2017, 42, 844–853. [Google Scholar] [CrossRef] [PubMed]
- Evon, D.M.; Golin, C.E.; Bonner, J.E.; Grodensky, C.; Velloza, J. Adherence during antiviral treatment regimens for chronic Hepatitis C: A qualitative study of patient-reported facilitators and barriers. J. Clin. Gastroenterol 2015, 49, e41–e50. [Google Scholar] [CrossRef] [Green Version]
- Tan, D.H.S.; Leon-Carlyle, M.; Mills, R.; Moses, E.; Carvalhal, A. Self-administered screening for syndemic mental health problems should be routinely implemented among MSM PrEP users. J. Gay Lesbian Ment. Health 2016, 20, 13–20. [Google Scholar] [CrossRef]
- Taylor, S.W.; Psaros, C.; Pantalone, D.W.; Tinsley, J.; Elsesser, S.A.; Mayer, K.H.; Safren, S.A. “Life-Steps” for PrEP adherence: Demonstration of a CBT-based intervention to increase adherence to Preexposure Prophylaxis (PrEP) medication among sexual-minority men at high risk for HIV acquisition. Cogn. Behav. Pract. 2017, 24, 38–49. [Google Scholar] [CrossRef] [Green Version]
- Haberer, J.E. Current concepts for PrEP adherence. Curr. Opin. HIV AIDS 2016, 11, 10–17. [Google Scholar] [CrossRef] [Green Version]
- Fuchs, J.D.; Stojanovski, K.; Vittinghoff, E.; McMahan, V.M.; Hosek, S.G.; Amico, K.R.; Kouyate, A.; Gilmore, H.J.; Buchbinder, S.P.; Lester, R.T.; et al. A mobile health strategy to support adherence to antiretroviral preexposure prophylaxis. AIDS Patient Care STDs 2018, 32, 104–111. [Google Scholar] [CrossRef]
| PubMed | PsycInfo | Web of Science | Google Scholar | |
|---|---|---|---|---|
| PrEP | (Pre-Exposure Prophylaxis[Mesh] OR “pre-exposure prophylaxis”[Title/Abstract] OR “preexposure prophylaxis”[Title/Abstract] OR “pre exposure prophylaxis” [Title/Abstract] OR PrEP [Title/Abstract] OR “HIV PrEP” [Title/Abstract] OR tenofovir [Title/Abstract] OR truvada [Title/Abstract] OR emtricitabine [Title/Abstract] OR descovy [Title/Abstract]) | (DE(“Pre-Exposure Prophylaxis”) OR AB (“pre-exposure prophylaxis” OR “preexposure prophylaxis” OR “pre exposure prophylaxis” OR PrEP OR “HIV PrEP” OR tenofovir OR truvada OR emtricitabine OR descovy) OR TI (“pre-exposure prophylaxis” OR “preexposure prophylaxis” OR “pre exposure prophylaxis” OR PrEP OR “HIV PrEP” OR tenofovir OR truvada OR emtricitabine OR descovy)) | (AB = (“pre-exposure prophylaxis” OR “preexposure prophylaxis” OR “pre exposure prophylaxis” OR PrEP OR “HIV PrEP” OR tenofovir OR truvada OR emtricitabine OR descovy) OR TI = (“pre-exposure prophylaxis” OR “preexposure prophylaxis” OR “pre exposure prophylaxis” OR PrEP OR “HIV PrEP” OR tenofovir OR truvada OR emtricitabine OR descovy)) | (PrEP OR “pre-exposure prophylaxis” OR “pre exposure prophylaxis” OR “preexposure prophylaxis” OR tenofovir OR truvada OR descovy) |
| AND | AND | AND | AND | |
| Anxiety | “Anxiety”[Mesh] OR “Anxiety Disorders”[Mesh] OR anxiety[Title/Abstract] OR anxious[Title/Abstract] | DE(“Anxiety” OR “Anxiety Disorders” OR “Generalized Anxiety Disorder”) OR AB(anxiety OR anxious) OR TI (anxiety OR anxious) | AB = (“generalized anxiety disorder” OR “anxiety disorder” OR anxiety OR anxious) OR TI = (“generalized anxiety disorder” OR “anxiety disorder” OR anxiety OR anxious) | anxiety OR anxious |
| OR | OR | OR | OR | |
| Depression | (“Depression”[Mesh] OR “Depressive Disorder”[Mesh] OR “Depressive Disorder, Major”[Mesh] OR depress*[Title/Abstract]) | (DE (“Major Depression” OR “Depression(Emotion)”) OR AB(depress *) OR TI(depress *) | (AB = (“major depression” OR “depressive disorder” OR “major depressive disorder” OR depress *) OR TI = (“major depression” OR “depressive disorder” OR “major depressive disorder” OR depress *) | depression OR depressive OR depress * |
| OR | OR | OR | OR | |
| Mental Health | (“Mental Health”[Mesh] OR “Mental Disorders”[Mesh] OR “mental health”[Title/Abstract] OR “mental disorder”[Title/Abstract]) | (DE (“Mental Health” OR “Mental Disorders”) OR AB(“mental health” OR “mental disorder”) OR TI (“mental health” OR “mental disorder”)) | (AB = (“mental health” OR “mental disorder”) OR TI = (“mental health” OR “mental disorder”)) | (“mental health” OR “mental disorder”) |
| Limiters | From: 2012/1/1 English Article Type: Journal Article | Publication Year: 2012–2021 Source Types: Academic Journals | Language: (English) Document Types (Article) Timespan = 2012–2021 | NA |
| Authors & Year | Location(s) | Sample Demographics | Design | Depression Measure (Scoring) | Depression Related Findings |
|---|---|---|---|---|---|
| Blashill, Brady, Rooney et al. 2020 [42] | San Diego, CA | 151 Latino MSM; mean age: 24. | Cross-sectional survey | PHQ-8 (10+ screened positive) | A psychosocial syndemic (depression, binge drinking, marijuana use, illicit polysubstance use, childhood sexual abuse) was not associated with PrEP awareness or willingness to use. |
| Blackstock, Platt, Golub et al. 2021 [40] | East Harlem, NY; Bronx, NY | 52 women, 11.5% TGW; 34.6% non-Latina Black; 51.9% Latina/Hispanic, 42.3% LGB; mean age: 45. | Pilot test | PHQ-2 (dichotomous screening) | Depression was not associated with PrEP interest. |
| Bologna, Panesar-Aguilar, McCraney, and Cale 2020 [41] | United States | 190 female individuals; 90% African American; mean age: 22. | Cross-sectional survey | PHQ-9 (continuous) | Depression was not related to willingness to use PrEP. |
| Eaton, Matthews, Driffin et al. 2017 [33] | Atlanta, GA; Detroit, MI; Houston, TX; Philadelphia, PA; Washington DC | 1274 Black MSM and TGW; 96% Male; 76% gay/same gender loving; mean age: 30. | Cross-sectional survey | CESD-10 (10+ screened positive) | Depression not associated with PrEP awareness. |
| Friedman, Sang, Bukowski et al. 2019 [34] | Atlanta, GA; Detroit, MI; Houston, TX; Memphis, TN; Philadelphia, PA; Washington DC | 2398 Black MSM, 82% MSM only; 3.4% Hispanic/Latino; mean age: 29. | Serial cross-sectional survey | CESD-10 (10+ screened positive) | Depressive symptoms was not associated with PrEP awareness. |
| Krakower, Mimiaga, Rosenberger et al. 2012 [35] | United States | 398 MSM 2 months prior to iPrEX trial results publication; 82% White; 89% Gay; mean age: 40. 558 MSM 2 months following publication; 84% White; 83% gay; mean age: 39. | Repeated cross-sectional survey | CESD-10 (10+ screened positive) | Depression was not associated with PrEP awareness. |
| Kuo, Olsen, Patrick et al. 2016 [43] | Washington, DC | 304 PWID; 69% male; 97.7% Black; 83% 50+ yrs. | Cross-sectional survey | CESD-10 (dichotomous screening) | Those who screened positive for depressive symptoms were more likely to be willing to use PrEP. |
| Liu, Brown, Przybyla et al. 2021 [36] | Nashville, TN; Buffalo, NY | 374 MSM, 60.2% Black; 77% gay/homosexual; median age: 26. | Cross-sectional survey | PHQ-9 Categorical (0–4, 5–9, 10–14, 15–19, 20–27) | Depression was not associated with PrEP awareness or willingness to use. |
| Ni, Altice, Wickersham et al. 2021 [38] | Connecticut | 234 individuals dependent on opioids; 51% male; 63.3% non-Hispanic White; mean age: 42.7. | Cross-sectional survey | CESD-20 (16+ screened positive) | Moderate to severe depression was not correlated with willingness to use PrEP. |
| Ojikutu, Bogart, Higgins-Biddle et al. 2018 [44] | United States | 855 participants; 54% female; 91% Black; 4% Latino. | Cross-sectional survey | Whooley et al. 1997 2-item measure (categorical frequency) | Depressive symptoms was associated with greater PrEP willingness amongst the entire sample, but not amongst those who were PrEP indicated. |
| Shrestha, DiDomizio, Kim et al. 2020 [45] | New Haven, CT | 234 people who use drugs; 51% male; 63% White; 79% heterosexual; mean age: 42.7. | Cross-sectional survey | CESD (16+ screened positive) | Depression was not associated with willingness to use LAI-PrEP. |
| Shrestha, Karki, Altice et al. 2017 [46] | New Haven, CT | 400 people who use drugs; 58% male; 63% White; 15% Hispanic/Latino; 86% straight; mean age: 41. | Cross-sectional survey | CESD-20 (16+ screened positive) | Those who had moderate to severe depression were more likely to be willing to initiate PrEP. |
| Sullivan and Eaton 2020 [37] | Atlanta, GA | 293 Black MSM; 56% gay/homosexual; mean age: 30. | Cross-sectional survey | CESD-10 (10+ screened positive) | Depression was not associated with PrEP awareness. |
| Tomko, Park, Allen et al. 2019 [39] | Baltimore, MD | 232 female sex workers; 66% non-Hispanic White; 50% ages < 35. | Cross-sectional survey | CESD-10 (10+ screened positive) | Depressive symptoms were not associated with PrEP awareness or interest. |
| Willie, Kershaw, Blackstock et al. 2020 [47] | New Haven, CT; Bridgeport, CT; Hartfort, CT | 271 women; 36% non-Hispanic White, 35% non-Hispanic Black; 28% Hispanic; 75% heterosexual; 61% ages 25+. | Cross-sectional survey | PHQ-9 (10+ screened positive) | Adjusting for sociodemographic variables, there was no difference between number of syndemic conditions (IPV, depression, substance use) and PrEP interest or intentions to use. |
| Authors & Year | Location(s) | Sample Demographics | Design | Depression Measure | Depression Related Findings |
|---|---|---|---|---|---|
| Blashill, Brady, Rooney et al. 2020 [42] | San Diego, CA | 151 Latino MSM men; mean age: 24. | Cross-sectional survey | PHQ-8 10+ screened positive | A psychosocial syndemic (depression, binge drinking, marijuana use, illicit polysubstance use, childhood sexual abuse) was not associated with PrEP use. |
| Blackstock, Platt, Golub et al. 2021 [40] | East Harlem, NY; Bronx, NY | 52 women, 11.5% TGW; 34.6% non-Latina Black; 51.9% Latina/Hispanic, 42.3% LGB; mean age: 45. | Pilot test | PHQ-2 (dichotomous screening) | Depression was not associated with PrEP appointment acceptance. |
| Bruxvoort, Schumacher, Towner et al. 2021 [52] | Southern California | 2995 PrEP candidates; 96.6% male; 60% racial/ethnic minorities; age: 50% < 35. | Retrospective Chart Review | Diagnostic codes | Depression was not associated with PrEP referral. |
| Eaton, Matthews, Driffin et al. 2017 [36] | Atlanta, GA; Detroit, MI; Houston, TX; Philadelphia, PA; Washington DC | 1274 Black MSM and TGW; 96% male; 76% gay/same gender loving; mean age: 30. | Cross-sectional survey | CESD-10 (10+ screened positive) | In bivariate analyses, depressive symptoms were associated with PrEP use. The association did not hold in multivariable analyses. |
| Friedman, Sang, Bukowski et al. 2019 [34] | Atlanta, GA; Detroit, MI; Houston, TX; Memphis, TN; Philadelphia, PA; Washington DC | 2398 Black MSM, 82% MSMO; 3.4% Hispanic/Latino; mean age: 29. | Serial cross-sectional survey | CESD-10 (10+ screened positive) | Depressive symptoms were not associated with PrEP use. |
| Krakower, Mimiaga, Rosenberger et al. 2012 [35] | United States | 398 MSM 2 months prior to iPrEX publication; 82% White; 89% gay; mean age: 40. 558 MSM 2 months following publication; 84% White; 83% gay; mean age: 39. | Repeated cross-sectional survey | CESD-10 (10+ screened positive) | Depression was not associated with PrEP use. |
| Laborde, Kinley, Spinelli et al. 2020 [50] | San Francisco, CA | 25 current or former PrEP users; 60% MSM, 20% TGW who have sex with men; 32% Black; 28% Hispanic; ages 18–57. | Qualitative Interviews | Qualitative focus | One participant reported stigma surrounding depression and HIV making it difficult to seek help. |
| Liu, Brown, Przybyla et al. 2021 [36] | Nashville, TN; Buffalo, NY | 374 MSM, 60.2% Black; 77% gay/homosexual; median age: 26. | Cross-sectional survey | PHQ-9 (categorical: 0–4, 5–9, 10–14, 15–19, 20–27) | Depression was not associated with PrEP use. |
| Sullivan and Eaton 2020 [37] | Atlanta, GA | 293 Black MSM; 56% gay/homosexual; mean age: 30 | Cross-sectional survey | CESD-10 (10+ screened positive) | Depression alone was not associated with PrEP use. However, having two or more syndemic conditions (depression symptoms, alcohol consumption, illicit drug use, transactional sex) was associated with less likelihood of PrEP use. |
| Ni, Altice, Wickersham et al. 2021 [38] | Connecticut | 234 individuals dependent on opioids; 51% male; 63.3% non-Hispanic White; mean age: 42.7. | Cross-sectional survey | CESD-20 (16+ screened positive) | Moderate to severe depression was not correlated with PrEP use. |
| Ogunbajo, Storholm, Ober et al. 2021 [48] | Southern California | 30 TGW; 33.3% Black/African American; 53% Hispanic/Latina/Latinx; 46% straight/heterosexual; mean age: 30. | Mixed methods | Qualitative focus | Mental health concerns were a barrier to PrEP uptake. |
| Okafor, Hucks-Ortiz, Hightow-Weidman et al. 2020 [56] | Los Angeles, CA; Washington DC; Chapel Hill, NC. | 226 Black MSM; 60% > 25 yrs old. | Non-randomized open-label PrEP study | CESD (10+ screened positive) | No differences were found in PrEP initiation by depression. |
| Serota, Rosenberg, Thorne, Sullivan, and Kelley 2019 [53] | Atlanta, GA | 154 Black MSM, 45% age 22–25. | Longitudinal | PHQ-8 (10+ screened positive) | Depression was not associated with a delay between PrEP prescription and initiation. |
| Serota, Rosenberg, Sullivan et al. 2020 [54] | Atlanta, GA | 298 non-Hispanic Black cis-gender MSM; 73% gay; 62% ages 18–21. | Prospective Observational Cohort Study | PHQ-8 (10+ screened positive) | Depressive symptoms were not associated with PrEP uptake. |
| Sewell, Powell, Mayer et al. 2020 [57] | United States | 9697 individuals; 92% male; 69% non-Hispanic White; mean age: 43. | Cross-sectional survey | CESD (continuous) | Those who used nondaily PrEP compared with daily PrEP were more likely to have higher depressive symptoms. |
| Rutledge, Madden, Ogbuagu, and Meyer 2018 [51] | Connecticut | 125 women involved in the criminal justice system; 69% White; mean age: 37. | Cross-sectional survey | Unspecified | There was no difference in PrEP eligibility by depressive symptoms. |
| Watson, Pasipanodya, Savin et al. 2020 [49] | San Diego, CA; Los Angeles, CA | 37 individuals; 48% TGW, 27% trans men; 41% White, non-Hispanic; 16% Latinx/Hispanic. | Qualitative focus groups | Qualitative focus | Mental health concerns, including depression and anxiety made it difficult to access PrEP care as well as other services. |
| Wheeler, Fields, Beauchamp et al. 2019 [55] | Los Angeles, CA; Washington DC; Chapel Hill, NC. | 226 MSM; 86% Black; 73% gay; median age: 26 | Non-randomized open-label PrEP study | CESD-10 (10+ screened positive) | Depressive symptoms were not related to PrEP initiation. |
| Wood, Morales, Metzger et al. 2020 [58] | Philadelphia, PA | 247 individuals; 89% cis male; 46% African American; 19% Latinx ethnicity; 47% ages 25–34. | Cross-sectional survey | PHQ-8 (10+ screened positive) | No associations were found between depressive symptoms and mental health treatment on PrEP use. |
| Carneiro, Westmoreland, Patel, and Grov 2020 [59] | United States | 6283 individuals; 98% cis men; 52% White; 33% 30–39 yrs old | Cross-sectional survey | PHQ-4 (dichotomous screening) | Depression was not associated with PrEP use |
| Chandler, Bukowski, Matthews et al. 2020 [60] | Atlanta, GA; Detroit, MI; Houston, TX; Memphis, TN; Philadelphia, PA; Washington DC | 1411 Black MSM; 80% gay/homosexual, 16% bisexual; 64% 18–29 years old | Cross-sectional survey | CESD-10 (10+ screened positive) | There was no difference between PrEP users and non-users in depressive symptoms. In considering syndemic psychosocial conditions (substance use, intimate partner violence, depression), those with greater number of syndemic conditions were more likely to report PrEP use. |
| Eaton, Matthews, Bukowski et al. 2018 [61] | Philadelphia, PA; Detroit, MI; Washington, DC; Atlanta, GA; Houston, TX; and Memphis, TN. | 4184 Black MSM or TGW. 77.7% gay/same gender loving, mean age: 30.47. | Cross-sectional survey | CESD-10 (10+ screened positive) | Depression was associated with current PrEP use. |
| Moeller, Seehuus, Wahl, and Gratch 2020 [62] | United States | 2406 MSM; 55% White; 18.6% Latino; 78.6% gay; mean age: 34. | Cross-sectional survey | PHQ-9 (categorical: 0–4, 5–9, 10–14, 15–19, 20+) | PrEP users reported lowest levels of depression compared with non-PrEP using participants. Use of PrEP was not associated with depression. |
| Authors & Year | Location(s) | Sample Demographics | Design | Depression Measure | Depression Related Findings |
|---|---|---|---|---|---|
| Blashill, Brady, Rooney et al. 2020 [42] | San Diego, CA | 151 Latino MSM; Mean age: 24. | Cross-sectional survey | PHQ-8 10+ screened positive | A psychosocial syndemic (depression, binge drinking, marijuana use, illicit polysubstance use, childhood sexual abuse) was associated with lowered self-reported adherence. |
| Bruxvoort, Schumacher, Towner et al. 2021 [52] | Southern California | 2995 PrEP candidates; 96.6% male; 60% racial/ethnic minorities; 50% < 35 years old. | Retrospective chart review | Diagnostic codes | Depression was not associated with PrEP persistence according to medical and pharmacy records. |
| Colson, Franks, Wu et al. 2020 [68] | Harlem, NY | 204 Black MSM (95.1%) and TGW (4.9%) newly enrolled on PrEP, 20.6% Latino; Median age: 31. | Randomized control trial | CES-D (16+ screened positive) | Those who reported depressive symptoms at baselines were less likely to be adherent according to self-report and dried blood spot (DBS) drug concentration. |
| Gandhi, Murnane, Bacchetti et al. 2017 [64] | Miami, Fl; San Francisco, CA; Washington DC | 280 PrEP users; 99% male, 78% White; Mean age: 34. | Longitudinal | PHQ-2 (dichotomous screening) | Depressive symptoms were not associated with PrEP adherence according to DBS drug concentration. |
| Hoenigl, Jain, Moore 2018 [66] | Southern California | 394 MSM and TGW, 99% male; 76% White; 30% Hispanic; Median age: 33. | Randomized control trial | PHQ-9 (continuous) | Baseline PHQ-9 scores were not associated with adherence according to DBS drug concentration. |
| Krakower, Maloney, Powell et al. 2019 [71] | Boston, MA | 663 PrEP users; 96% male, 3% transgender women; 73% non-Hispanic White; Median age: 32.6. | Retrospective chart review | Medical problems list and diagnostic codes | PrEP discontinuations were more likely to occur in those who had multiple mental health disorders (includes anxiety, depression, substance use, PTSD, bipolar, schizophrenia, and attention deficit disorder). |
| Laborde, Kinley, Spinelli et al. 2020 [50] | San Francisco, CA | 25 current or former PrEP users; 60% MSM, 20% TGW who have sex with men; 32% Black; 28% Hispanic; Ages 18–57. | Qualitative interviews | Qualitative focus | Participants indicated it was difficult to keep track of medications when having mental health problems. |
| Liu, Cohen, Vittinghoff et al. 2016 [65] | Miami, Fl; San Francisco, CA; Washington DC | 557 PrEP users; 48% White, 34% Latino; 98% MSM; Mean age: 35. | Longitudinal | PHQ-2 (2+ screened positive) | Depression was not associated with PrEP adherence. |
| Mannheimer, Hirsch-Moverman, Franks et al. 2019 [67] | New York City, NY | 176 MSM; 59% non-Hispanic Black; 25% Hispanic; Median age: 31. | Randomized control trial | CES-D (16+ screened positive) | Depressive symptoms were not associated with adherence measured through self-report, pill counts, and DBS drug concentration. |
| Ogunbajo, Storholm, Ober et al. 2021 [48] | Southern California | 30 TGW; 33.3% Black/African American; 53% Hispanic/Latina/Latinx; 46% straight/heterosexual; Mean age 29.8. | Mixed methods: cross-sectional survey and qualitative interviews | Qualitative focus | Mental health concerns, including depression and anxiety, decreased motivation to take PrEP, making it less of a priority and making adherence difficult. For some, however, PrEP adherence was a coping mechanism. |
| Pasipanodya, Jain, Sun et al. 2018 [69] | Southern California | 181 MSM; 81% White; Mean age 34.98. | Longitudinal | PHQ (categorical: 0–4, 5–9, 10–14) | Individuals with worse self-reported adherence were more likely to have depressive symptoms. |
| Scott, Spinelli, Vittinghoff et al. 2019 [72] | San Francisco | 348 PrEP patients; 84% male; 39% White; 27% Latino; Median age: 35. | Retrospective chart review | Clinical diagnosis | Depression was not associated with discontinuations in PrEP use. |
| Serota, Rosenberg, Sullivan et al. 2020 [54] | Atlanta, GA | 298 non-Hispanic Black cis-gender MSM; 73% gay; 62% ages 18–21. | Prospective observational cohort study | PHQ-8 (10+ screened positive) | Depressive symptoms were not associated with PrEP discontinuations. |
| Spinelli, Laborde, Kinley et al. 2020 [70] | San Francisco, CA | 8 individuals; 63% MSM, 38% TGW who have sex with men; 38% White, 25% African American; 25% Latinx; 38% ages < 25, 38% ages 40–64. | Qualitative interviews | Qualitative focus | One participant noted depression and its intersection with substance use as a major barrier to adherence. |
| Wheeler, Fields, Beauchamp et al. 2019 [55] | Los Angeles, CA; Washington DC; Chapel Hill, NC. | 226 MSM; 86% Black; 73% Gay; Median age: 26 | Non-randomized open-label PrEP study | CESD-10 (10+ screened positive) | Depressive symptoms were not related to PrEP adherence according to DBS drug concentration. |
| Young, Lalley-Chareczko, Clark et al. 2020 [63] | Philadelphia, PA | 31 PrEP users; 87% male, 13% TGW; 74% African American; 16% Hispanic; Mean age: 21.7. | Cross-sectional survey | PHQ-9 (10+ screened positive) | Depressive symptoms were not associated with adherence according to urine drug concentration. |
| Zucker, Carnevale, Richards et al. 2019 [73] | Manhattan, NY | 696 PrEP users, 93% male at birth; 23% African American; 45.7% Hispanic; 54% age < 30. | Retrospective chart review | PHQ-9 (5+ screened positive) | Depressive symptoms were not associated with retention. |
| Authors & Year | Location(s) | Sample Demographics | Design | PrEP Stage | Anxiety Measure | Anxiety Related Findings |
|---|---|---|---|---|---|---|
| Blackstock, Platt, Golub et al. 2021 [34] | East Harlem, NY; Bronx, NY | 52 women, 11.5% TGW; 34.6% non-Latina Black; 51.9% Latina/Hispanic, 42.3% LGB; mean age: 45. | Pilot test | Awareness, initiation | GAD-2 (dichotomous screening) | Anxiety did not predict PrEP interest or appointment acceptance. |
| Liu, Brown, Przybyla et al. 2021 [40] | Nashville, TN; Buffalo, NY | 374 MSM, 60.2% Black; 77% gay; median age: 26. | Cross-sectional survey | Awareness, initiation | GAD-7 categorical (0–4, 5–9, 10–14, 15–21) | Anxiety was not associated with PrEP awareness, willingness to use, or use. |
| Meyers, Rodriguez, Brill et al. 2017 [74] | New York City, NY; Philadelphia, PA | 28 individuals receiving long-acting injectable cabotegravir; 60% MSM of color; 14% Latino; mean age: 31. | Mixed methods: cross-sectional survey and qualitative interviews | Uptake | Qualitative focus | Participants reported anxiety related to injections, which decreased over time and was not correlated with pain. Two forms of anxiety were present related to needles and expected pain. |
| Watson, Pasipanodya, Savin et al. 2020 [49] | San Diego, CA; Los Angeles, CA | 37 individuals; 48% TGW, 27% trans men; 41% White, non-Hispanic; 16% Latinx/Hispanic. | Qualitative focus groups | Access | Qualitative focus | Mental health concerns, including depression and anxiety, made it difficult to access PrEP care as well as other services. |
| Bruxvoort, Schumacher, Towner et al. 2021 [52] | Southern California | 2995 PrEP candidates; 96.6% male; 60% racial/ethnic minorities; 50% < 35 years old. | Retrospective chart review | Adherence and retention | Diagnostic codes | Anxiety was not associated with PrEP referral or persistence. |
| Carneiro, Westmoreland, Patel, and Grov 2020 [59] | United States | 6283 individuals; 98% cis men; 52% White; 33% 30–39 years old | Cross-sectional survey | Initiation | PHQ-4 (dichotomous screening) | Anxiety was not associated with prior or current PrEP use. |
| Ogunbajo, Storholm, Ober et al. 2021 [48] | Southern California | 30 TGW; 33.3% Black/African American; 53% Hispanic/Latina/Latinx; 46% straight/heterosexual; mean age 29.8. | Mixed methods: cross-sectional survey and qualitative interviews | Adherence and retention | Qualitative focus | Mental health concerns, including depression and anxiety, decreased motivation to take PrEP, making it less of a priority and making adherence difficult. For some, however, PrEP adherence was a coping mechanism. |
| Young, Lalley-Chareczko, Clark et al. 2020 [63] | Philadelphia, PA | 31 PrEP users; 87% male, 13% transgender women; 74% African American; 16% Hispanic; mean age: 21.7. | Cross-sectional survey | Adherence and retention | GAD-7 (10+ screened positive) | Anxiety was associated with lower adherence according to urine drug concentration. |
| Scott, Spinelli, Vittinghoff et al. 2019 [72] | San Francisco | 348 PrEP patients; 84% male; 39% White; 27% Latino; median age: 35. | Retrospective chart review | Adherence and retention | Diagnostic codes | Anxiety was not associated with discontinuations in PrEP use. |
| Krakower, Maloney, Powell et al. 2019 [71] | Boston, MA | 663 PrEP users; 96% male, 3% transgender women; 73% non-Hispanic White; median age: 32.6. | Retrospective chart review | Adherence and retention | Medical problems list and diagnostic codes | PrEP discontinuations were more likely to occur in those who had multiple mental health disorders (includes anxiety, depression, substance use, PTSD, bipolar, schizophrenia, and attention deficit disorder). |
| Authors & Year | Location(s) | Sample Demographics | Design | Anxiety Measure | Anxiety Related Findings |
|---|---|---|---|---|---|
| Brooks, Landovitz, Kaplan et al. 2012 [84] | Los Angeles, CA | 25 gay or bisexual men in HIV serodiscordant relationships; 40% Black/African American; 32% Hispanic/Latino; 76% gay/homosexual, 24% bisexual. | Mixed methods | Qualitative focus | Having less anxiety when having sex with an HIV-positive partner was one of three reasons participants indicated for willingness to take PrEP. |
| Devarajan, Sales, Hunt, Comeau 2020 [77] | Atlanta, GA | 10 MSM currently or formerly on PrEP; 75% Black; 95% non-Hispanic/Latino; mean Age: 30.2. | Qualitative interviews | Qualitative focus | PrEP use reduced feelings of anxiety and stress. |
| Hammack, Toolis, Wilson et al. 2019 [79] | New York City, NY; San Francisco, CA; Tuscon, AZ; Austin, TX | 89 gay or bisexual men; 23.6% White; 24.7% Latino/Hispanic; 78.6% gay; ages 18–59. | Qualitative interviews | Qualitative focus | PrEP improved sexual culture, making sex more comfortable and enjoyable, and reducing anxiety, particularly amongst younger participants. PrEP alleviated anxiety, removing HIV-related worry. |
| Hojilla, Koester, Cohen et al. 2016 [75] | San Francisco, CA; Miami, FL; Washington DC | 26 men on PrEP; 62% White; 27% Hispanic. | Qualitative analysis of counseling notes | Qualitative focus | PrEP alleviated anxiety related to sex and HIV, providing “peace of mind” and alleviating anxiety for both participants and their partners. As a result, some participants explored sexual roles which they otherwise would have not been comfortable with. |
| Mitchell, Lee, Woodyatt et al. 2016 [83] | Atlanta, GA; Detroit, MI | 19 male couples, most were non-Hispanic and/or White; 28% of couples were mixed race. Specific demographics are unavailable; mean age: 33. | Qualitative interviews | Qualitative focus | Some participants reported that PrEP could be a part of couple’s agreements in order to reduce sexual anxiety and risk, to keep the couple safe. |
| Moeller, Seehuus, Wahl, and Gratch 2020 [62] | United States | 2406 MSM; 55% White; 18.6% Latino; 78.6% gay; mean age: 34. | Cross-sectional survey | GAD-7 categorical (0–4, 5–9, 10–14, 15+) | PrEP users reported lowest levels of anxiety compared with non-PrEP-using participants. Among those on PrEP, internalized homophobia, but not number of condomless anal intercourse partners was associated with greater anxiety. In contrast, for those not on PrEP, greater number of CAI partners and internalized homophobia were associated with higher anxiety (r square = 0.06). |
| Mutchler, McDavitt, Ghani et al. 2015 [78] | Los Angeles, CA | 24 friend pairs; 83% male; 87.5% Black; 14.6% Latino; 68.8% gay; mean age: 22.1. | Qualitative interviews | Qualitative focus | Participants described PrEP as a backup option which could provide peace of mind and reduce anxiety if other preventative methods failed. |
| Quinn, Christenson, Sawkin et al. 2020 [80] | Milwaukee, WI; Minneapolis, MN; Detroit, MI; and Kansas City, MO | 36 Black MSM current/past PrEP users; 69% gay; mean age: 26. | Qualitative focus groups | Qualitative focus | PrEP reduced sexual and HIV-related anxiety, including relieving anxieties related to having sex, getting HIV tests, and potential fears of acquiring HIV. This reduced anxiety created sexual freedom, increasing control and autonomy regarding sexual health and providing the opportunity to explore without fears of HIV. |
| Storholm, Volk, Marcus et al. 2017 [81] | San Francisco, CA | 30 MSM PrEP users; 40% White; 23% Latino; mean age: 27.5. | Qualitative interviews | Qualitative focus | Individuals indicated PrEP enhanced their sexual wellbeing, decreasing HIV related anxiety, and increasing openness to HIV positive partners. |
| Whitfield, Jones, Wachman et al. 2021 [85] | United States | 1071 cis MSM PrEP users; 70% White; 11% Latino; 38.7% ages 25–34. | Longitudinal | Sexual anxiety MSSCQ subscale (continuous) | Participants showed less sexual anxiety when on PrEP compared to their sexual anxiety before beginning PrEP. |
| Yang, Krishnan, Kelley et al. 2020 [82] | Baltimore, MD | 18 MSM PrEP users; 83% non-Hispanic Black/African American. | Qualitative interviews | Qualitative focus | Participants reported PrEP as providing “peace of mind”, reducing anxiety related to HIV or partner dishonesty. |
| Zapata, Petroll, de St. Aubin, and Quinn 2020 [76] | Milwaukee, WI | 20 PrEP patients; 93% cis male; 60% White; 20% Hispanic; 85% gay; mean age: 33. | Qualitative interviews | Qualitative focus | PrEP helped alleviate HIV-related anxiety, allowing individuals to feel they were being responsible. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miller, S.J.; Harrison, S.E.; Sanasi-Bhola, K. A Scoping Review Investigating Relationships between Depression, Anxiety, and the PrEP Care Continuum in the United States. Int. J. Environ. Res. Public Health 2021, 18, 11431. https://doi.org/10.3390/ijerph182111431
Miller SJ, Harrison SE, Sanasi-Bhola K. A Scoping Review Investigating Relationships between Depression, Anxiety, and the PrEP Care Continuum in the United States. International Journal of Environmental Research and Public Health. 2021; 18(21):11431. https://doi.org/10.3390/ijerph182111431
Chicago/Turabian StyleMiller, Sarah J., Sayward E. Harrison, and Kamla Sanasi-Bhola. 2021. "A Scoping Review Investigating Relationships between Depression, Anxiety, and the PrEP Care Continuum in the United States" International Journal of Environmental Research and Public Health 18, no. 21: 11431. https://doi.org/10.3390/ijerph182111431
APA StyleMiller, S. J., Harrison, S. E., & Sanasi-Bhola, K. (2021). A Scoping Review Investigating Relationships between Depression, Anxiety, and the PrEP Care Continuum in the United States. International Journal of Environmental Research and Public Health, 18(21), 11431. https://doi.org/10.3390/ijerph182111431






