Tele-Yoga in Long Term Illness–Protocol for a Randomised Controlled Trial Including a Process Evaluation and Results from a Pilot Study
Abstract
:1. Introduction
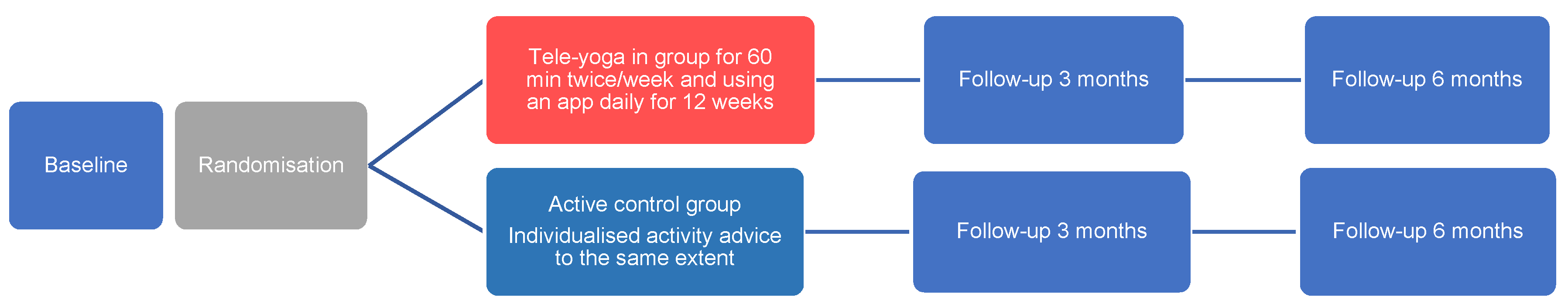
2. Methods
2.1. Development of the Tele-Yoga Intervention
2.2. Study Protocol
2.3. Study Participants
2.4. Inclusion Criteria
2.5. Exclusion Criteria
2.6. Hypothesis
2.7. Research Questions Related to the Process Evaluation
2.7.1. Health Technology Assessment
2.7.2. Patient Experiences and Preferences
2.7.3. Exercise Motivation, Fidelity, Adherence and Social Selectivity
2.8. Intervention Group (Tele-Yoga)
2.8.1. Group Yoga Sessions
2.8.2. Yoga App
2.9. Active Control Group
2.10. Data Collection
2.11. Qualitative Analysis
2.12. Health Technology Assessment
3. Pilot Study
3.1. Feasibility of Interventions (Tele-Yoga and Active Control Group)
3.2. Acceptability of the Tele-Yoga
3.3. Safety of the Interventions (Tele-Yoga and Active Control Group)
3.4. Data Analysis Pilot Study
4. Results
4.1. Pilot Study
4.2. Feasibility
4.2.1. Fidelity of Tele-Yoga and Individual Activity Advice
4.2.2. Exercise Motivation
4.3. Acceptability of the Tele-Yoga
4.4. Safety of the Interventions and Data Collection
4.5. Primary Composite End-Point
4.6. Secondary End Points
4.6.1. Gait Speed
4.6.2. Sit-to-Stand
4.6.3. Cognition
4.6.4. Health-Related Quality of Life
4.6.5. Sleep
4.6.6. Activity Monitoring
4.7. Process Evaluation
5. Discussion
5.1. Summary of Main Findings
5.2. Delivery of the Yoga Intervention
5.3. The Active Control Group
5.4. Hypothesis, Study Outcomes and Sample Size for the RCT Following the Pilot
5.5. Strength and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stephens, I. Medical Yoga Therapy. Children 2017, 4, 12. [Google Scholar] [CrossRef] [PubMed]
- Katuri, K.K.; Dasari, A.B.; Kurapati, S.; Vinnakota, N.R.; Bollepalli, A.C.; Dhulipalla, R. Association of yoga practice and serum cortisol levels in chronic periodontitis patients with stress-related anxiety and depression. J. Int. Soc. Prev. Community Dent. 2016, 6, 7–14. [Google Scholar] [CrossRef] [Green Version]
- Grensman, A.; Acharya, B.D.; Wändell, P.; Nilsson, G.H.; Falkenberg, T.; Sundin, Ö.; Werner, S. Effect of traditional yoga, mindfulness-based cognitive therapy, and cognitive behavioral therapy, on health related quality of life: A randomized controlled trial on patients on sick leave because of burnout. BMC Complement. Altern. Med. 2018, 18, 80. [Google Scholar] [CrossRef] [Green Version]
- Listunova, L.; Roth, C.; Bartolovic, M.; Kienzle, J.; Bach, C.; Weisbrod, M.; Roesch-Ely, D. Cognitive Impairment Along the Course of Depression: Non-Pharmacological Treatment Options. Psychopathology 2018, 51, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Hägglund, E.; Hagerman, I.; Dencker, K.; Strömberg, A. Effects of yoga versus hydrotherapy training on health-related quality of life and exercise capacity in patients with heart failure: A randomized controlled study. Eur. J. Cardiovasc. Nurs. J. Work. Group Cardiovasc. Nurs. Eur. Soc. Cardiol. 2017, 16, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Donesky, D.; Selman, L.; McDermott, K.; Citron, T.; Howie-Esquivel, J. Evaluation of the Feasibility of a Home-Based TeleYoga Intervention in Participants with Both Chronic Obstructive Pulmonary Disease and Heart Failure. J. Altern. Complement. Med. (N. Y.) 2017, 23, 713–721. [Google Scholar] [CrossRef]
- Selman, L.; McDermott, K.; Donesky, D.; Citron, T.; Howie-Esquivel, J. Appropriateness and acceptability of a Tele-Yoga intervention for people with heart failure and chronic obstructive pulmonary disease: Qualitative findings from a controlled pilot study. BMC Complement. Altern. Med. 2015, 15, 21. [Google Scholar] [CrossRef] [Green Version]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ (Clin. Res. Ed.) 2014, 348, g1687. [Google Scholar] [CrossRef] [Green Version]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ (Clin. Res. Ed.) 2015, 350, h1258. [Google Scholar] [CrossRef] [Green Version]
- Wahlström, M.; Rosenqvist, M.; Medin, J.; Walfridsson, U.; Rydell-Karlsson, M. MediYoga as a part of a self-management programme among patients with paroxysmal atrial fibrillation—A randomised study. Eur. J. Cardiovasc. Nurs. J. Work. Group Cardiovasc. Nurs. Eur. Soc. Cardiol. 2020, 19, 74–82. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Sullivan, M.J.; Thompson, P.J.; Fallen, E.L.; Pugsley, S.O.; Taylor, D.W.; Berman, L.B. The 6-minute walk: A new measure of exercise capacity in patients with chronic heart failure. Can. Med. Assoc. J. 1985, 132, 919–923. [Google Scholar] [PubMed]
- Csuka, M.; McCarty, D.J. Simple method for measurement of lower extremity muscle strength. Am. J. Med. 1985, 78, 77–81. [Google Scholar] [CrossRef]
- Rydwik, E.; Bergland, A.; Forsén, L.; Frändin, K. Investigation into the reliability and validity of the measurement of elderly people’s clinical walking speed: A systematic review. Physiother. Theory Pract. 2012, 28, 238–256. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Orwelius, L.; Nilsson, M.; Nilsson, E.; Wenemark, M.; Walfridsson, U.; Lundström, M.; Taft, C.; Palaszewski, B.; Kristenson, M. The Swedish RAND-36 Health Survey—Reliability and responsiveness assessed in patient populations using Svensson’s method for paired ordinal data. J. Patient-Rep. Outcomes 2017, 2, 4. [Google Scholar] [CrossRef] [Green Version]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Westergren, A.; Broman, J.E.; Hellström, A.; Fagerström, C.; Willman, A.; Hagell, P. Measurement properties of the minimal insomnia symptom scale as an insomnia screening tool for adults and the elderly. Sleep Med. 2015, 16, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Stenström, C.H.; Boestad, C.; Carlsson, M.; Edström, M.; Reuterhäll, A. Why exercise?: A preliminary investigation of an exercise motivation index among individuals with rheumatic conditions and healthy individuals. Physiother. Res. Int. J. Res. Clin. Phys. Ther. 1997, 2, 7–16. [Google Scholar] [CrossRef]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ (Clin. Res. Ed.) 2016, 355, i5239. [Google Scholar] [CrossRef] [Green Version]
- Song, J.; Wang, T.; Wang, Y.; Li, R.; Niu, S.; Zhuo, L.; Guo, Q.; Li, X. The Effectiveness of Yoga on Cancer-Related Fatigue: A Systematic Review and Meta-Analysis. Oncol. Nurs. Forum 2021, 48, 207–228. [Google Scholar] [CrossRef] [PubMed]
- Seshadri, A.; Adaji, A.; Orth, S.S.; Singh, B.; Clark, M.M.; Frye, M.A.; Fuller-Tyszkiewicz, M.; McGillivray, J. Exercise, Yoga, and Tai Chi for Treatment of Major Depressive Disorder in Outpatient Settings: A Systematic Review and Meta-Analysis. Prim. Care Companion CNS Disord. 2020, 23. [Google Scholar] [CrossRef]
- Li, J.; Gao, X.; Hao, X.; Kantas, D.; Mohamed, E.A.; Zheng, X.; Xu, H.; Zhang, L. Yoga for secondary prevention of coronary heart disease: A systematic review and meta-analysis. Complement. Ther. Med. 2020, 57, 102643. [Google Scholar] [CrossRef] [PubMed]
- Köhn, M.; Persson Lundholm, U.; Bryngelsson, I.L.; Anderzén-Carlsson, A.; Westerdahl, E. Medical yoga for patients with stress-related symptoms and diagnoses in primary health care: A randomized controlled trial. Evid. Based Complement Alternat Med. 2013, 2013, 215348. [Google Scholar] [CrossRef]
- Wahlstrom, M.; Rydell Karlsson, M.; Medin, J.; Frykman, V. Effects of yoga in patients with paroxysmal atrial fibrillation—A randomized controlled study. Eur. J. Cardiovasc. Nurs. 2017, 16, 57–63. [Google Scholar] [CrossRef] [Green Version]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ (Clin. Res. Ed.) 2008, 337, a1655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Tele-Yoga n = 5 | Active Control n = 5 | |
|---|---|---|
| Age, median years (range) | 50.0 (41–68) | 67.0 (54–76) |
| Female/male gender | 3/2 | 3/2 |
| Married | 3 | 5 |
| Children | 4 | 5 |
| Living alone | 1 | 0 |
| Economic situation rated as good/problematic | 4/1 | 5/0 |
| Education: Secondary school/university | 5/0 | 2/3 |
| Computer use daily | 5 | 5 |
| Having a smartphone | 5 | 3 |
| Having a tablet | 1 | 4 |
| Internet use daily | 5 | 5 |
| Earlier experience yoga | 2 | 2 |
| Exercising > 3 h/week (self-reported before the study) | 1 | 1 |
| Patient | Group Randomisation | 6MWT Distance Change | EQ-5D Number of the 5 Dimensions that Changed | HADS Depression | HADS Anxiety | Composite End-Point |
|---|---|---|---|---|---|---|
| 1 | Tele-yoga | +77 m | 3 improved | No Depression at baseline or follow-up | Going from above to below a score of 8 | +3 |
| 2 | Control | +101 m | 3 improved | No Depression at baseline or follow-up | Going from above to below a score of 8 | +3 |
| 3 | Tele-yoga | +42 m | 1 improved | Going from above to below a score of 8 | Going from above to below a score of 8 | +3 |
| 4 | Tele-yoga | +72 m | No change | No Depression at baseline or follow-up | No anxiety at baseline or follow-up | +1 |
| 5 | Control | Data missing 3 months | 1 improved | No Depression at baseline or follow-up | No anxiety at baseline or follow-up | +1 |
| 6 | Tele-yoga | +37 m | 1 improved | No Depression at baseline or follow-up | No anxiety at baseline or follow-up | +2 |
| 7 | Control | +81 | 1 deteriorated | No Depression at baseline or follow-up | No anxiety at baseline or follow-up | 0 |
| 8 | Control | Drop out at 3 months | ||||
| 9 | Tele-yoga | Data missing 3 months | 2 improved | No Depression at baseline or follow-up | No anxiety at baseline or follow-up | +1 |
| 10 | Control | −1 m | No change | No Depression at baseline or follow-up | No anxiety at baseline or follow-up | −1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strömberg, A.; Thylén, I.; Orwelius, L.; Klompstra, L.; Jaarsma, T. Tele-Yoga in Long Term Illness–Protocol for a Randomised Controlled Trial Including a Process Evaluation and Results from a Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 11343. https://doi.org/10.3390/ijerph182111343
Strömberg A, Thylén I, Orwelius L, Klompstra L, Jaarsma T. Tele-Yoga in Long Term Illness–Protocol for a Randomised Controlled Trial Including a Process Evaluation and Results from a Pilot Study. International Journal of Environmental Research and Public Health. 2021; 18(21):11343. https://doi.org/10.3390/ijerph182111343
Chicago/Turabian StyleStrömberg, Anna, Ingela Thylén, Lotti Orwelius, Leonie Klompstra, and Tiny Jaarsma. 2021. "Tele-Yoga in Long Term Illness–Protocol for a Randomised Controlled Trial Including a Process Evaluation and Results from a Pilot Study" International Journal of Environmental Research and Public Health 18, no. 21: 11343. https://doi.org/10.3390/ijerph182111343
APA StyleStrömberg, A., Thylén, I., Orwelius, L., Klompstra, L., & Jaarsma, T. (2021). Tele-Yoga in Long Term Illness–Protocol for a Randomised Controlled Trial Including a Process Evaluation and Results from a Pilot Study. International Journal of Environmental Research and Public Health, 18(21), 11343. https://doi.org/10.3390/ijerph182111343






