Recognition of Anemia in Elderly People in a Rural Community Hospital
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
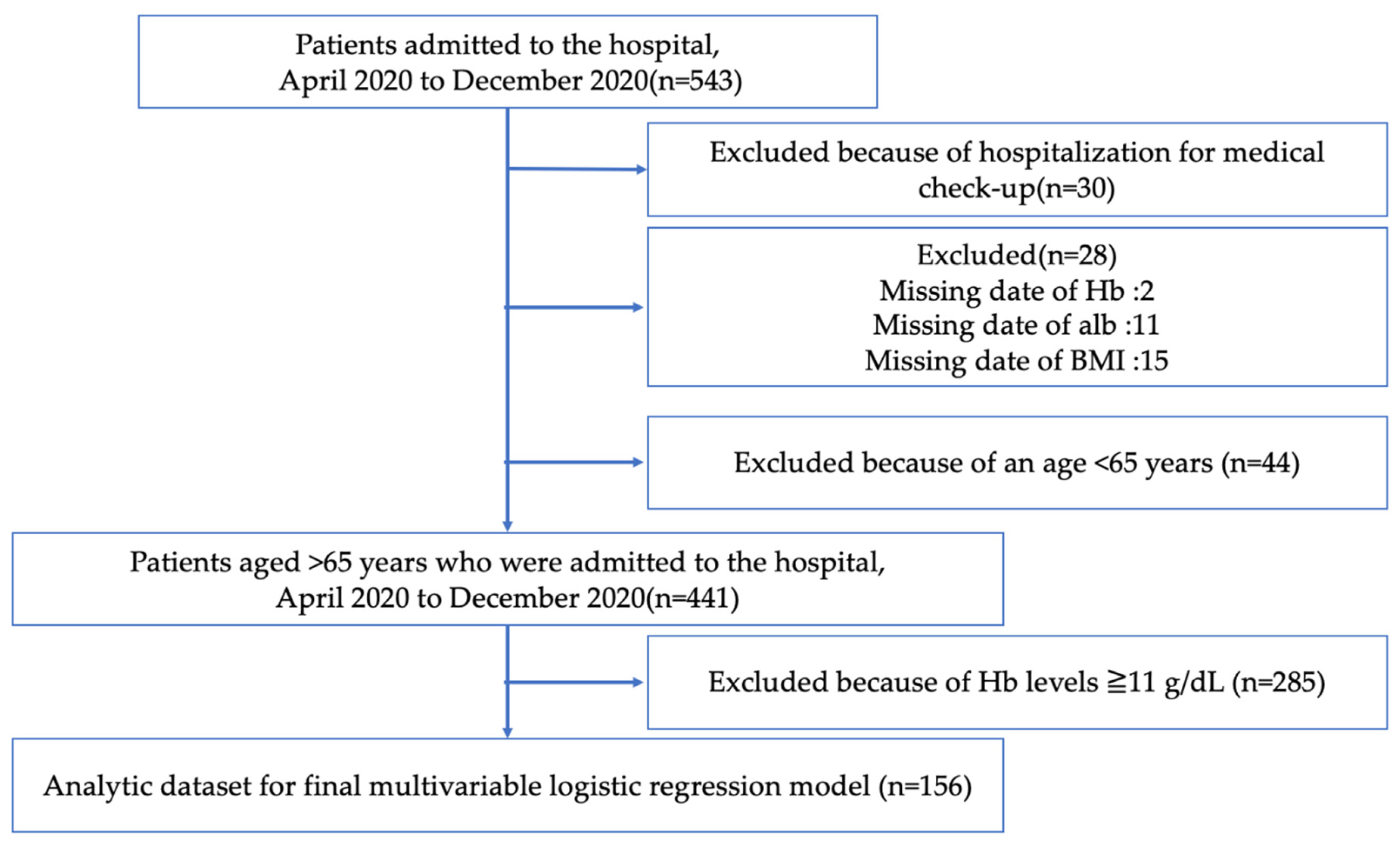
2.2. Participants
2.3. Sample Size
2.4. Data Collection
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
3.1. Demographics of the Participants
3.2. Association between the Recognition of Anemia and Influential Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nutritional Anaemias. Report of a WHO scientific group. World Health Organ. Technol. Rep. Ser. 1968, 405, 5–37. [Google Scholar]
- Lanier, J.B.; Park, J.J.; Callahan, R.C. Anemia in older adults. Am. Fam. Physician 2018, 98, 437–442. [Google Scholar]
- Stauder, R.; Thein, S.L. Anemia in the elderly: Clinical implications and new therapeutic concepts. Haematologica 2014, 99, 1127–1130. [Google Scholar] [CrossRef]
- Beutler, E.; Waalen, J. The definition of anemia: What is the lower limit of normal of the blood hemoglobin concentration. Blood 2006, 107, 1747–1750. [Google Scholar] [CrossRef]
- Culleton, B.F.; Manns, B.J.; Zhang, J.; Tonelli, M.; Klarenbach, S.; Hemmelgarn, B.R. Impact of anemia on hospitalization and mortality in older adults. Blood 2006, 107, 3841–3846. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Eisenstaedt, R.S.; Ferrucci, L.; Klein, H.G.; Woodman, R.C. Prevalence of anemia in persons 65 years and older in the United States: Evidence for a high rate of unexplained anemia. Blood 2004, 104, 2263–2268. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kitayuguchi, J.; Gomi, T.; Katsube, T. Challenges and solutions in the continuity of home care for rural older people: A thematic analysis. Home Health Care Serv. Q. 2020, 39, 126–139. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Leung, G.; Woo, J. Randomized controlled trial on the effects of a combined intervention of computerized cognitive training preceded by physical exercise for improving frailty status and cognitive function in older adults. Int. J. Environ. Res. Public Health 2021, 18, 1396. [Google Scholar] [CrossRef] [PubMed]
- Kamada, M.; Kitayuguchi, J.; Abe, T.; Taguri, M.; Inoue, S.; Ishikawa, Y.; Bauman, A.; Lee, I.M.; Miyachi, M.; Kawachi, I. Community-wide intervention and population-level physical activity: A 5-year cluster randomized trial. Int. J. Epidemiol. 2018, 47, 642–653. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Otani, J. Rural physicians’ perceptions about the challenges of participating in interprofessional collaboration: Insights from a focus group study. J. Interprofessional Educ. Pract. 2010, 20, 100345. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Katsube, T.; Sano, C. Rural homecare nurses' challenges in providing seamless patient care in rural Japan. Int. J. Environ. Res. Public Health 2020, 17, 9330. [Google Scholar] [CrossRef] [PubMed]
- Ohta, R.; Maeki, N.; Maniwa, S.; Miyakoshi, K. Predicting factors of elderly patients' discharge to home after rehabilitation in rural Japan: A retrospective cohort study. Rural Remote Health 2021, 21, 6406. [Google Scholar] [PubMed]
- Unnan City. Available online: https://www.city.unnan.shimane.jp/unnan/ (accessed on 25 May 2021).
- Nilsson-Ehle, H.; Jagenburg, R.; Landahl, S.; Svanborg, A. Blood haemoglobin declines in the elderly: Implications for reference intervals from age 70 to 88. Eur. J. Haematol. 2000, 65, 297–305. [Google Scholar] [CrossRef]
- Tsutsumi, H.; Ota, M. Diagnosis and treatment of anemia. 4. Anemia of the aged. Nihon Naika Gakkai Zasshi J. Jpn. Soc. Intern. Med. 2006, 95, 2021–2025. [Google Scholar]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Linacre, J.M.; Heinemann, A.W.; Wright, B.D.; Granger, C.V.; Hamilton, B.B. The structure and stability of the Functional Independence Measure. Arch. Phys. Med. Rehabil. 1994, 75, 127–132. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Sloane, P.D.; Gruber-Baldini, A.L.; Zimmerman, S.; Roth, M.; Watson, L.; Boustani, M.; Magaziner, J.; Hebel, J.R. Medication undertreatment in assisted living settings. Arch. Intern. Med. 2004, 164, 2031–2037. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lang, P.O.; Hasso, Y.; Dramé, M.; Vogt-Ferrier, N.; Prudent, M.; Gold, G.; Michel, J.P. Potentially inappropriate prescribing including under-use amongst older patients with cognitive or psychiatric co-morbidities. Age Ageing 2010, 39, 373–381. [Google Scholar] [CrossRef]
- Chang, E.S.; Kannoth, S.; Levy, S.; Wang, S.Y.; Lee, J.E.; Levy, B.R. Global reach of ageism on older persons' health: A systematic review. PLoS ONE 2020, 15, e0220857. [Google Scholar]
- Iwao-Kawamura, Y.; Shigeishi, H.; Uchida, S.; Kawano, S.; Maehara, T.; Sugiyama, M.; Ohta, K. Changes in physical and oral function after a long-term care prevention program in community-dwelling Japanese older adults: A 12-month follow-up study. Healthcare 2021, 9, 719. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.J.; Kim, B.H.; Lee, H.; Wang, J. The beneficial effects of cognitive walking program on improving cognitive function and physical fitness in older adults. Healthcare 2021, 9, 419. [Google Scholar] [CrossRef]
- Light, J.M.; Grigsby, J.S.; Bligh, M.C. Aging and heterogeneity: Genetics, social structure, and personality. Gerontologist 1996, 36, 165–173. [Google Scholar] [CrossRef]
- Lee, E.; Cha, S.; Kim, G.M. Factors affecting health-related quality of life in multimorbidity. Healthcare 2021, 9, 334. [Google Scholar] [CrossRef]
- Sargent-Cox, K. Ageism: We are our own worst enemy. Int. Psychogeriatr. 2017, 29, 1–8. [Google Scholar] [CrossRef]
- Ohta, R.; Sano, C. Risk of hospital readmission among older patients discharged from the rehabilitation unit in a rural community hospital: A retrospective cohort study. J. Clin. Med. 2021, 10, 659. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kitayuguchi, J.; Sano, C.; Könings, K.D. Educational intervention to improve citizen's healthcare participation perception in rural Japanese communities: A pilot study. Int. J. Environ. Res. Public Health 2021, 18, 1782. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Matarese, M.; Arcangeli, V.; Alciati, V.; Candela, V.; Facchinetti, G.; Marchetti, A.; De Marinis, M.G.; Denaro, V. Family caregiver strain and challenges when caring for orthopedic patients: A systematic review. J. Clin. Med. 2020, 9, 1497. [Google Scholar] [CrossRef]
- Heo, J.; Youk, T.M.; Seo, K.D. Anemia is a risk factor for the development of ischemic stroke and post-stroke mortality. J. Clin. Med. 2021, 10, 2556. [Google Scholar] [CrossRef] [PubMed]
- Lopez, C.; Holgado, J.L.; Fernandez, A.; Sauri, I.; Uso, R.; Trillo, J.L.; Vela, S.; Bea, C.; Nuñez, J.; Ferrer, A.; et al. Impact of acute hemoglobin falls in heart failure patients: A population study. J. Clin. Med. 2020, 9, 1869. [Google Scholar] [CrossRef]
| Anemia Recognition | |||
|---|---|---|---|
| Characteristics | Negative (n = 93) | Positive (n = 63) | p-Value |
| Age (years), mean (SD) 65–69, n (%) 70–74, n (%) 75–79, n (%) 80–84, n (%) 85–89, n (%) 90–94, n (%) 95–99, n (%) | 89.49 (6.30) 0 (0.00) 2 (2.15) 5 (5.38) 14 (15.05) 22 (23.66) 25 (26.88) 25 (26.88) | 84.81 (7.71) 3 (4.76) 7 (11.11) 5 (7.94) 7 (11.11) 24 (38.10) 14 (22.22) 3 (4.76) | <0.001 |
| Sex, male, n (%) | 34 (36.6) | 22 (34.9) | 0.866 |
| Albumin (g/dL), mean (SD) | 3.15 (0.60) | 3.13 (0.62) | 0.867 |
| BMI (kg/m2), mean (SD) | 19.15 (3.00) | 20.89 (5.17) | 0.009 |
| Hb (g/dL), mean (SD) | 9.76 (1.16) | 8.73 (1.53) | <0.001 |
| Dependent condition, n (%) (dependence ≥ 1) | 61 (65.6) | 32 (50.8) | 0.070 |
| CCI score (≥5), n (%) | 71 (76.3) | 45 (71.4) | 0.576 |
| Myocardial infarction, n (%) | 7 (7.5) | 1 (1.6) | 0.144 |
| Congestive heart failure, n (%) | 22 (23.7) | 18 (28.6) | 0.576 |
| Brain hemorrhage, n (%) | 11 (11.8) | 4 (6.3) | 0.285 |
| Brain stroke, n (%) | 18 (19.4) | 11 (17.5) | 0.836 |
| Dementia, n (%) | 24 (25.8) | 9 (14.3) | 0.110 |
| Chronic obstructive pulmonary disease, n (%) | 6 (6.5) | 5 (7.9) | 0.757 |
| Connective tissue disease, n (%) | 6 (6.5) | 2 (3.2) | 0.475 |
| Peptic ulcer disease, n (%) | 5 (5.4) | 16 (25.4) | <0.001 |
| Hepatic cirrhosis, n (%) | 2 (2.2) | 1 (1.6) | 1 |
| Diabetes, n (%) | 17 (18.3) | 5 (12.7) | 0.383 |
| Hemiplegia, n (%) | 1 (1.1) | 3 (4.8) | 0.304 |
| Chronic kidney disease, n (%) | 61 (65.6) | 50 (79.4) | 0.073 |
| Malignancy, n (%) | 21 (22.6) | 14 (22.2) | 1 |
| Discharge to facility, n (%) | 21 (23.9) | 13 (22) | 0.844 |
| Admission from facility, n (%) | 16 (17.2) | 10 (15.9) | 1 |
| Dysphagia, n (%) | 23 (25) | 5 (7.9) | <0.001 |
| FIM at admission, mean (SD) | 61.88 (39.69) | 79.81 (43.47) | 0.017 |
| Number | Disease | Number of Cases | % | Number | Disease | Number of Cases | % |
|---|---|---|---|---|---|---|---|
| 1 | Heart failure | 21 | 13.5 | 12 | Brain hemorrhage | 2 | 1.3 |
| 2 | UTI | 18 | 11.5 | 13 | Compression fracture | 2 | 1.3 |
| 3 | Aspiration pneumonia | 13 | 8.3 | 14 | Dehydration | 2 | 1.3 |
| 4 | Gastrointestinal bleeding | 9 | 5.8 | 15 | Hypoglycemia | 2 | 1.3 |
| 5 | Brain stroke | 8 | 5.1 | 16 | RS3PE | 2 | 1.3 |
| 6 | Pneumonia | 8 | 5.1 | 17 | TIA | 2 | 1.3 |
| 7 | Cancer | 7 | 4.5 | 18 | Sepsis | 2 | 1.3 |
| 8 | Pseudogout | 6 | 3.8 | 19 | CD colitis | 2 | 1.3 |
| 9 | Syncope | 6 | 3.8 | 20 | Myocardial infarction | 2 | 1.3 |
| 10 | Cellulitis | 4 | 2.6 | 21 | Other | 34 | 21.8 |
| 11 | Anemia | 4 | 2.6 |
| Factor | Odds Ratio | 95% CI | p-Value |
|---|---|---|---|
| Age (every 5 years) | 0.70 | 0.53–0.92 | 0.011 |
| Albumin | 0.80 | 0.45–1.44 | 0.461 |
| BMI | 1.07 | 0.97–1.19 | 0.178 |
| CCI ≥ 5 | 0.69 | 0.31–1.54 | 0.361 |
| Dysphagia | 0.40 | 0.13–1.20 | 0.103 |
| FIM | 1.00 | 0.99–1.01 | 0.509 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amano, S.; Ohta, R.; Sano, C. Recognition of Anemia in Elderly People in a Rural Community Hospital. Int. J. Environ. Res. Public Health 2021, 18, 11179. https://doi.org/10.3390/ijerph182111179
Amano S, Ohta R, Sano C. Recognition of Anemia in Elderly People in a Rural Community Hospital. International Journal of Environmental Research and Public Health. 2021; 18(21):11179. https://doi.org/10.3390/ijerph182111179
Chicago/Turabian StyleAmano, Shiho, Ryuichi Ohta, and Chiaki Sano. 2021. "Recognition of Anemia in Elderly People in a Rural Community Hospital" International Journal of Environmental Research and Public Health 18, no. 21: 11179. https://doi.org/10.3390/ijerph182111179
APA StyleAmano, S., Ohta, R., & Sano, C. (2021). Recognition of Anemia in Elderly People in a Rural Community Hospital. International Journal of Environmental Research and Public Health, 18(21), 11179. https://doi.org/10.3390/ijerph182111179







