Determinants of Intention to Participate in Breast Cancer Screening among Urban Chinese Women: An Application of the Protection Motivation Theory
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Data Collection
2.4. Measures
2.4.1. Demographic Variables
2.4.2. Knowledge of Breast Cancer
2.4.3. Breast Cancer PMT Scale
2.4.4. Intention to Participate in Breast Cancer Screening
2.5. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Knowledge of Breast Cancer
3.3. Association of the PMT Subconstructs with Screening Intention
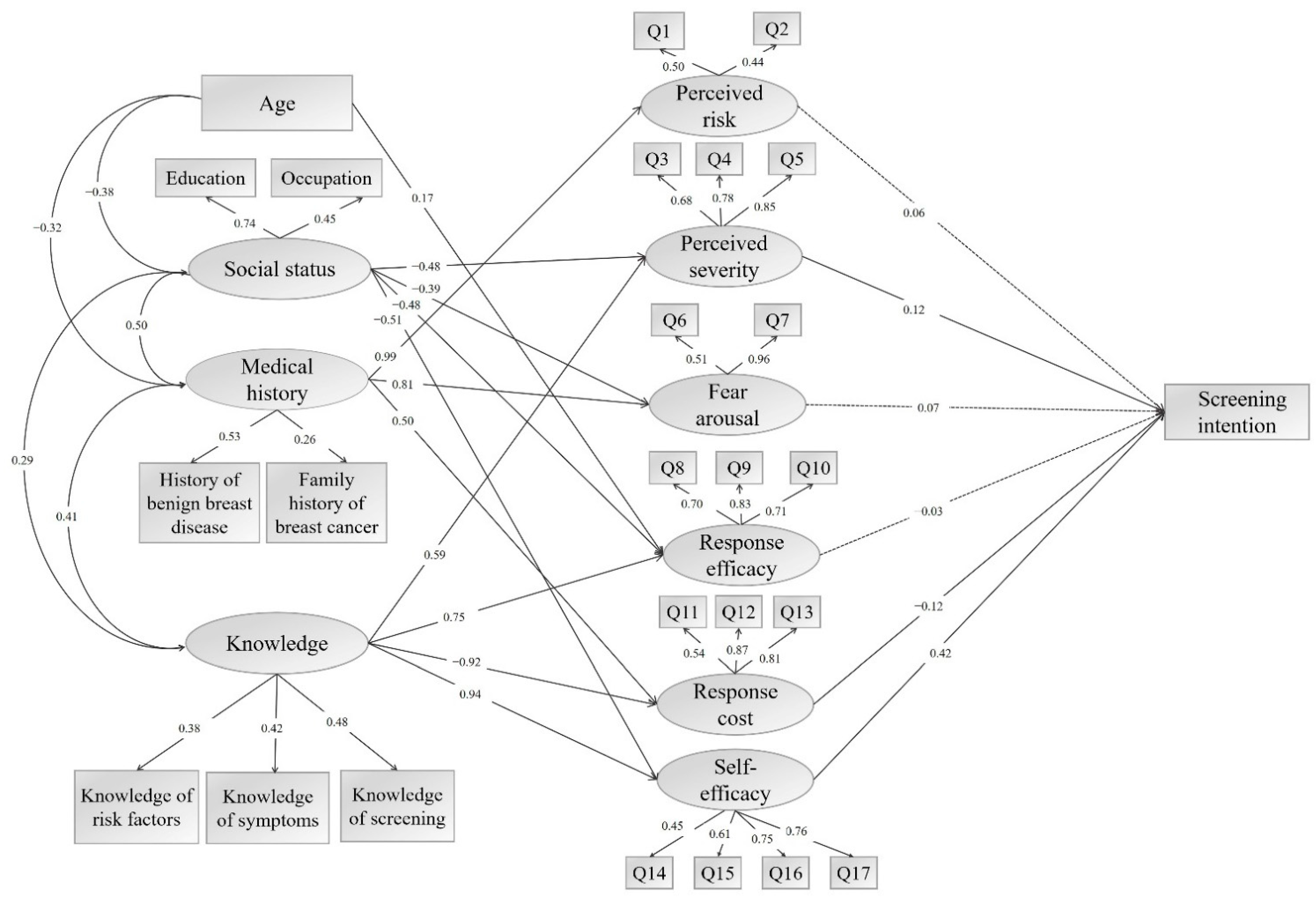
3.4. Structural Equation Modeling
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Item by Subconstructs | Mean (SD) |
|---|---|
| Perceived risk | 5.19 (1.71) |
| Q1. I am more likely to get breast cancer compared with others. | 2.44 (0.94) |
| Q2. Someone once reminded me to be careful of getting breast cancer. | 2.75 (1.23) |
| Perceived severity | 13.26 (1.90) |
| Q3. Getting breast cancer will seriously affect my health. | 4.48 (0.71) |
| Q4. Once I have breast cancer, my life will change significantly. | 4.33 (0.81) |
| Q5. The impact of breast cancer on my whole family is huge. | 4.45 (0.70) |
| Fear arousal | 6.81 (2.18) |
| Q6. When I think of breast cancer, I get nervous. | 3.73 (1.21) |
| Q7. I will worry about getting breast cancer. | 3.08 (1.32) |
| Response efficacy | 11.44 (2.28) |
| Q8. Only by doing mammography, can breast cancer be detected early. | 3.77 (0.97) |
| Q9. Through mammography examination, I can figure out whether I have breast cancer. | 3.94 (0.81) |
| Q10. If someone wants to cure breast cancer, she can’t do it without mammography. | 3.73 (0.94) |
| Response cost | 6.00 (2.43) |
| Q11. I feel embarrassed to receive mammography. | 4.04 (0.98) |
| Q12. Doing mammography examination is too time-consuming. | 4.00 (1.00) |
| Q13. Doing mammography examination is too wasteful of money. | 3.93 (0.99) |
| Self-efficacy | 15.08 (2.98) |
| Q14. I have enough time to do mammography examination. | 3.68 (1.08) |
| Q15. Mammography is very easy for me to accept. | 3.95 (0.87) |
| Q16. Even if others say that mammography is not necessary, I will do it myself. | 3.69 (1.01) |
| Q17. Even if I have to pay for it, I will go for mammography. | 3.76 (1.02) |
References
- International Agency for Research on Cancer. Latest Global Cancer Data: Cancer Burden Rises to 19.3 Million New Cases and 10.0 Million Cancer Deaths in 2020. Available online: https://www.iarc.who.int/faq/latest-global-cancer-data-2020-qa (accessed on 15 January 2021).
- Fan, L.; Zheng, Y.; Yu, K.D.; Liu, G.Y.; Wu, J.; Lu, J.S.; Shen, K.W.; Shen, Z.Z.; Shao, Z.M. Breast cancer in a transitional society over 18 years: Trends and present status in Shanghai, China. Breast Cancer Res. Treat. 2009, 117, 409–416. [Google Scholar] [CrossRef] [PubMed]
- van den Ende, C.; Oordt-Speets, A.M.; Vroling, H.; van Agt, H.M.E. Benefits and harms of breast cancer screening with mammography in women aged 40–49 years: A systematic review. Int. J. Cancer 2017, 141, 1295–1306. [Google Scholar] [CrossRef]
- Pace, L.E.; Keating, N.L. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA 2014, 311, 1327–1335. [Google Scholar] [CrossRef]
- Puliti, D.; Miccinesi, G.; Zappa, M.; Manneschi, G.; Crocetti, E.; Paci, E. Balancing harms and benefits of service mammography screening programs: A cohort study. Breast Cancer Res. 2012, 14, R9. [Google Scholar] [CrossRef]
- Dibden, A.; Offman, J.; Duffy, S.W.; Gabe, R. Worldwide review and meta-analysis of cohort studies measuring the effect of mammography screening programmes on incidence-based breast cancer mortality. Cancers 2020, 12, 976. [Google Scholar] [CrossRef] [PubMed]
- Fan, L.; Strasser-Weippl, K.; Li, J.J.; St, L.J.; Finkelstein, D.M.; Yu, K.D.; Chen, W.Q.; Shao, Z.M.; Goss, P.E. Breast cancer in China. Lancet. Oncol. 2014, 15, e279–e289. [Google Scholar] [CrossRef]
- Wang, B.; He, M.; Wang, L.; Engelgau, M.M.; Zhao, W.; Wang, L. Breast cancer screening among adult women in China, 2010. Prev. Chronic. Dis. 2013, 10, e183. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chen, H.; Li, N.; Ren, J.; Zhang, K.; Dai, M.; He, J. Ultrasound for breast cancer screening in high-risk women: Results from a population-based cancer screening program in China. Front. Oncol. 2019, 9, 286. [Google Scholar] [CrossRef]
- Kang, M.; Zhao, Y.; Huang, Y.; Li, J.; Liu, L.; Li, H. Accuracy and direct medical cost of different screening modalities for breast cancer among Chinese women. Zhonghua Zhong Liu Za Zhi 2014, 36, 236–240. [Google Scholar]
- Bao, H.L.; Wang, L.H.; Wang, L.M.; Fang, L.W.; Zhang, M.; Zhao, Z.P.; Cong, S. Study on the coverage of cervical and breast cancer screening among women aged 35–69 years and related impact of socioeconomic factors in China, 2013. Zhonghua Liu Xing Bing Xue Za Zhi 2018, 39, 208–212. [Google Scholar] [PubMed]
- Achat, H.; Close, G.; Taylor, R. Who has regular mammograms? Effects of knowledge, beliefs, socioeconomic status, and health-related factors. Prev. Med. 2005, 41, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Schueler, K.M.; Chu, P.W.; Smith-Bindman, R. Factors associated with mammography utilization: A systematic quantitative review of the literature. J. Womens Health 2008, 17, 1477–1498. [Google Scholar] [CrossRef]
- Liu, L.Y.; Wang, F.; Yu, L.X.; Ma, Z.B.; Zhang, Q.; Gao, D.Z.; Li, Y.Y.; Li, L.; Zhao, Z.T.; Yu, Z.G. Breast cancer awareness among women in Eastern China: A cross-sectional study. BMC Public Health 2014, 14, 1004. [Google Scholar] [CrossRef]
- Momenimovahed, Z.; Tiznobaik, A.; Taheri, S.; Hassanipour, S.; Salehiniya, H. A review of barriers and facilitators to mammography in Asian women. Ecancermedicalscience 2020, 14, 1146. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Liu, Y.; Li, X.; Song, B.; Ni, C.; Lin, F. Factors associated with breast cancer screening participation among women in mainland China: A systematic review. BMJ Open 2019, 9, e028705. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.Y.; Liu, Y.L.; Chung, S. Improving breast cancer outcomes among women in China: Practices, knowledge, and attitudes related to breast cancer screening. Int. J. Breast Cancer 2012, 2012, 921607. [Google Scholar] [CrossRef][Green Version]
- Wu, T.Y.; West, B.; Chen, Y.W.; Hergert, C. Health beliefs and practices related to breast cancer screening in Filipino, Chinese and Asian-Indian women. Cancer Detect. Prev. 2006, 30, 58–66. [Google Scholar] [CrossRef]
- Meissner, H.I.; Smith, R.A.; Rimer, B.K.; Wilson, K.M.; Rakowski, W.; Vernon, S.W.; Briss, P.A. Promoting cancer screening: Learning from experience. Cancer 2004, 101, 1107–1117. [Google Scholar] [CrossRef]
- Walsh, B.; Silles, M.; O'Neill, C. The importance of socio-economic variables in cancer screening participation: A comparison between population-based and opportunistic screening in the EU-15. Health Policy 2011, 101, 269–276. [Google Scholar] [CrossRef]
- Pasick, R.J.; Burke, N.J. A critical review of theory in breast cancer screening promotion across cultures. Annu. Rev. Public Health 2008, 29, 351–368. [Google Scholar] [CrossRef]
- Saei, G.N.M.; Simbar, M.; Rashidi, F.F.; Ghasemi, V. Effects of model-based interventions on breast cancer screening behavior of women: A systematic review. Asian Pac. J. Cancer Prev. 2018, 19, 2031–2041. [Google Scholar]
- Janz, N.K.; Becker, M.H. The Health belief model: A decade later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef] [PubMed]
- Noman, S.; Shahar, H.K.; Abdul, R.H.; Ismail, S.; Abdulwahid, A.-J.M.; Azzani, M. The effectiveness of educational interventions on breast cancer screening uptake, knowledge, and beliefs among women: A systematic review. Int. J. Environ. Res. Public Health 2020, 18, 263. [Google Scholar] [CrossRef]
- Russell, K.M.; Champion, V.L.; Skinner, C.S. Psychosocial factors related to repeat mammography screening over 5 years in African American women. Cancer Nurs. 2006, 29, 236–243. [Google Scholar] [CrossRef]
- Bastani, R.; Marcus, A.C.; Hollatz-Brown, A. Screening mammography rates and barriers to use: A Los Angeles county survey. Prev. Med. 1991, 20, 350–363. [Google Scholar] [CrossRef]
- Rogers, R.W. A protection motivation theory of fear appeals and attitude change1. J. Psychol. 1975, 91, 93–114. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Li, S.; Chen, X.; Yu, B.; Gao, M.; Yan, H.; Okafor, C.N. Protection motivation theory in predicting intention to engage in protective behaviors against schistosomiasis among middle school students in rural China. PLoS Negl. Trop. Dis. 2014, 8, e3246. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Li, Y.; Wangen, K.R.; Maitland, E.; Nicholas, S.; Wang, J. Analysis of hepatitis B vaccination behavior and vaccination willingness among migrant workers from rural China based on protection motivation theory. Hum. Vaccin. Immunother. 2016, 12, 1155–1163. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Liu, Q.; Chen, X.; Gao, Y.; Gong, H.; Tan, X.; Zhang, M.; Tuo, J.; Zhang, Y.; Xiang, Q.; et al. Protection motivation theory in predicting intention to receive cervical cancer screening in rural Chinese women. Psychooncology 2018, 27, 442–449. [Google Scholar] [CrossRef]
- Orbell, S. Cognition and affect after cervical screening: The role of previous test outcome and personal obligation in future uptake expectations. Soc. Sci. Med. 1996, 43, 1237–1243. [Google Scholar] [CrossRef]
- Li, Q.; Liu, Q.; Chen, X.; Tan, X.; Zhang, M.; Tuo, J.; Xiang, Q.; Yu, Q.; Zhu, Z. Protection motivation theory in predicting cervical cancer screening participation: A longitudinal study in rural Chinese women. Psychooncology 2020, 29, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Bao, Y.; Kwok, C.; Lee, C.F. Breast cancer screening behaviors among Chinese women in Mainland China. Nurs. Health Sci. 2018, 20, 445–451. [Google Scholar] [CrossRef]
- Huang, Y.; Zhou, K.; Li, H.; Wang, A.; Li, J.; Pang, Y.; Wang, Q.; Huang, R.; Fu, L.; Kang, M.; et al. Knowledge, attitudes, and behaviour regarding breast cancer screening among women from different socio-economic regions in southwest China: A cross-sectional study. Asian Pac. J. Cancer Prev. 2011, 12, 203–209. [Google Scholar]
- Bashirian, S.; Barati, M.; Mohammadi, Y.; Moaddabshoar, L.; Dogonchi, M. An application of the protection motivation theory to predict breast self-examination behavior among female healthcare workers. Eur. J. Breast Health 2019, 15, 90–97. [Google Scholar] [CrossRef]
- Ghofranipour, F.; Pourhaji, F.; Delshad, M.H.; Pourhaji, F. Determinants of breast cancer screening: Application of protection motivation theory. Int. J. Cancer Manag. 2020, 13, 1–7. [Google Scholar] [CrossRef]
- Bashirian, S.; Barati, M.; Shoar, L.M.; Mohammadi, Y.; Dogonchi, M. Factors affecting breast self-examination behavior among female healthcare workers in Iran: The role of social support theory. J. Prev. Med. Public Health 2019, 52, 224–233. [Google Scholar] [CrossRef]
- Sun, L.; Legood, R.; Sadique, Z.; Dos-Santos-Silva, I.; Yang, L. Cost-effectiveness of risk-based breast cancer screening programme, China. Bull. World Health Organ. 2018, 96, 568–577. [Google Scholar] [CrossRef] [PubMed]
- China Anti-Cancer Association, National Clinical Research Center for Cancer. Breast cancer screening guideline for Chinese women. Cancer Biol. Med. 2019, 16, 822–824. [Google Scholar]
- Zhang, M.; Liu, Q.; Li, Q.M.; Du, X.Y.; Zuo, D. Development of breast cancer screening protection motivation scale for Chinese women and its reliability and validity test. Chin. J. Health Educ. 2021, 37, 303–307. [Google Scholar]
- Milne, S.; Sheeran, P.; Orbell, S. Prediction and intervention in health-related behavior: A meta-analytic review of protection motivation theory. J. Appl. Soc. Psychol. 2000, 30, 106–143. [Google Scholar] [CrossRef]
- Floyd, D.L.; Prentice-Dunn, S.; Rogers, R.W. A meta-analysis of research on protection motivation theory. J. Appl. Soc. Psychol. 2000, 2, 407–429. [Google Scholar] [CrossRef]
- Luszczynska, A.; Schwarzer, R. Planning and self-efficacy in the adoption and maintenance of breast self-examination: A longitudinal study on self-regulatory cognitions. Psychol. Health 2003, 18, 93–108. [Google Scholar] [CrossRef]
- Garcia, K.; Mann, T. From ‘I Wish’ to ‘I Will’: Social-cognitive predictors of behavioral intentions. J. Health Psychol. 2003, 8, 347–360. [Google Scholar] [CrossRef] [PubMed]
- Eaker, S.; Adami, H.O.; Sparen, P. Attitudes to screening for cervical cancer: A population-based study in Sweden. Cancer Causes Control 2001, 12, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Malmir, S.; Barati, M.; Khani, J.A.; Bashirian, S.; Hazavehei, S.M.M. Effect of an educational intervention based on protection motivation theory on preventing cervical cancer among marginalized women in West Iran. Asian Pac. J. Cancer Prev. 2018, 19, 755–761. [Google Scholar]
- Khodayarian, M.; Mazloomi-Mahmoodabad, S.S.; Lamyian, M.; Morowatisharifabad, M.A.; Tavangar, H. Response costs of mammography adherence: Iranian women's perceptions. Health Promot. Perspect. 2016, 6, 85–91. [Google Scholar] [CrossRef]
- Liu, L.Y.; Wang, Y.J.; Wang, F.; Yu, L.X.; Xiang, Y.J.; Zhou, F.; Li, L.; Zhang, Q.; Fu, Q.Y.; Ma, Z.B.; et al. Factors associated with insufficient awareness of breast cancer among women in Northern and Eastern China: A case-control study. BMJ Open 2018, 8, e018523. [Google Scholar] [CrossRef]
- Guvenc, I.; Guvenc, G.; Tastan, S.; Akyuz, A. Identifying women's knowledge about risk factors of breast cancer and reasons for having mammography. Asian Pac. J. Cancer Prev. 2012, 13, 4191–4197. [Google Scholar] [CrossRef]
- Toan, D.T.T.; Son, D.T.; Hung, L.X.; Minh, L.N.; Mai, D.L.; Hoat, L.N. Knowledge, attitude, and practice regarding breast cancer early detection among women in a mountainous area in Northern Vietnam. Cancer Control 2019, 26, 1073274819863777. [Google Scholar] [CrossRef]
- Shang, C.; Beaver, K.; Campbell, M. Social cultural influences on breast cancer views and breast health practices among Chinese women in the United Kingdom. Cancer Nurs. 2015, 38, 343–350. [Google Scholar] [CrossRef]
- Molaei-Zardanjani, M.; Savabi-Esfahani, M.; Taleghani, F. Fatalism in breast cancer and performing mammography on women with or without a family history of breast cancer. BMC Womens Health 2019, 19, 116. [Google Scholar] [CrossRef] [PubMed]
- Niederdeppe, J.; Levy, A.G. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiol. Biomark. Prev. 2007, 16, 998–1003. [Google Scholar] [CrossRef] [PubMed]
- Befort, C.A.; Nazir, N.; Engelman, K.; Choi, W. Fatalistic cancer beliefs and information sources among rural and urban adults in the USA. J. Cancer Educ. 2013, 28, 521–526. [Google Scholar] [CrossRef] [PubMed]
| Variables | Screening Intention | Total (%) | |
|---|---|---|---|
| Yes | No | ||
| Sample size, N (%) | 357 (86.65) | 55 (13.35) | 412 (100.00) |
| Age in years, n (%) | |||
| 40–49 | 57 (93.44) | 4 (6.56) | 61 (100.00) |
| 50–59 | 118 (86.76) | 18 (13.24) | 136 (100.00) |
| 60–74 | 182 (84.65) | 33 (15.35) | 215 (100.00) |
| Marital status, n (%) | |||
| Single | 3 (100.00) | 0 (0.00) | 3 (100.00) |
| Married | 336 (86.60) | 52 (13.40) | 388 (100.00) |
| Widowed/divorced | 18 (85.71) | 3 (14.29) | 21 (100.00) |
| Education, n (%) | |||
| Primary or less | 81 (84.38) | 15 (15.63) | 96 (100.00) |
| Junior high school | 93 (83.04) | 19 (16.96) | 112 (100.00) |
| Senior high/technical school | 106 (90.60) | 11 (9.40) | 117 (100.00) |
| Junior college/college and above | 77 (88.51) | 10 (2.43) | 87(100.00) |
| Occupation, n (%) | |||
| Employees of enterprises and institutions | 102 (89.47) | 12 (10.53) | 114 (100.00) |
| Industrial/commercial/services workers | 170 (86.73) | 26 (13.27) | 196 (100.00) |
| Farmer | 54 (85.71) | 9 (14.29) | 63 (100.00) |
| Housewife | 18 (81.82) | 4 (18.18) | 22 (100.00) |
| Unemployed/retired | 13 (76.47) | 4 (23.53) | 17 (100.00) |
| History of benign breast disease, n (%) | |||
| Yes | 125 (88.03) | 17 (11.97) | 142 (100.00) |
| No | 232 (85.93) | 38 (14.07) | 270 (100.00) |
| Family history of breast cancer, n (%) | |||
| Yes | 18 (90.00) | 2 (10.00) | 20 (100.00) |
| No | 339 (86.48) | 53 (13.52) | 392 (100.00) |
| Total Scale/Single Item | Screening Intention | p-Value | |
|---|---|---|---|
| Yes | No | ||
| Total scale score, mean (SD) | 6.80 (3.61) | 5.07 (3.66) | 0.001 ** |
| Knowledge of risk factors for breast cancer | |||
| subscale score, mean (SD) | 2.80 (1.95) | 2.18 (2.13) | 0.030 * |
| Older age, n (%) | 171 (47.90) | 17 (30.91) | 0.019 * |
| Obesity, n (%) | 142 (39.78) | 16 (29.09) | 0.129 |
| Oral contraceptive use, n (%) | 131 (36.69) | 14 (25.45) | 0.104 |
| Non-breastfeeding, n (%) | 213 (59.66) | 27 (49.09) | 0.139 |
| Family history of breast cancer, n (%) | 190 (53.22) | 24 (43.64) | 0.185 |
| Menarche at age before 13, n (%) | 71 (19.89) | 10 (18.18) | 0.767 |
| Menopause at age over 55, n (%) | 83 (23.25) | 12 (21.82) | 0.815 |
| Knowledge of symptoms for breast cancer | |||
| subscale score, mean (SD) | 3.39 (1.69) | 2.65 (1.82) | 0.003 ** |
| Lump in breast, n (%) | 293 (82.07) | 39 (70.91) | 0.051 |
| Change in breast texture, n (%) | 189 (52.94) | 24 (43.64) | 0.199 |
| Axillary mass, n (%) | 259 (72.55) | 34 (61.82) | 0.102 |
| Nipple turned inward into the breast, n (%) | 221 (91.32) | 21 (38.18) | 0.001 ** |
| Discharge from nipple, n (%) | 247 (69.19) | 28 (50.91) | 0.007 ** |
| Knowledge of breast cancer screening | |||
| subscale score, mean (SD) | 0.61 (1.10) | 0.24 (0.64) | 0.000 ** |
| Mammography is one of the methods of breast cancer screening, n (%) | 83 (23.25) | 8 (14.55) | 0.147 |
| Mammography is recommended every year among women over 40 years old, n (%) | 51 (14.29) | 1 (1.82) | 0.010 * |
| Breast cancer can be detected early by mammography screening, n (%) | 85 (23.81) | 4 (7.27) | 0.006 ** |
| Variables | X2 | X3 | X4 | X5 | X6 | X7 |
|---|---|---|---|---|---|---|
| X1 Screening intention | 0.09 | 0.27 ** | 0.21 ** | 0.22 ** | –0.31 ** | 0.47 ** |
| X2 Perceived risk | –0.01 | 0.36 ** | 0.03 | 0.05 | 0.15 ** | |
| X3 Perceived severity | 0.22 ** | 0.29 ** | –0.25 ** | 0.26 ** | ||
| X4 Fear arousal | 0.11 * | 0.03 | 0.16 ** | |||
| X5 Response efficacy | –0.30 ** | 0.38 ** | ||||
| X6 Response cost | –0.48 ** | |||||
| X7 Self-efficacy | 1.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, M.; Wei, W.; Li, Q.; Chen, X.; Zhang, M.; Zuo, D.; Liu, Q. Determinants of Intention to Participate in Breast Cancer Screening among Urban Chinese Women: An Application of the Protection Motivation Theory. Int. J. Environ. Res. Public Health 2021, 18, 11093. https://doi.org/10.3390/ijerph182111093
Zhang M, Wei W, Li Q, Chen X, Zhang M, Zuo D, Liu Q. Determinants of Intention to Participate in Breast Cancer Screening among Urban Chinese Women: An Application of the Protection Motivation Theory. International Journal of Environmental Research and Public Health. 2021; 18(21):11093. https://doi.org/10.3390/ijerph182111093
Chicago/Turabian StyleZhang, Miao, Wenshuang Wei, Qinmei Li, Xinguang Chen, Min Zhang, Dan Zuo, and Qing Liu. 2021. "Determinants of Intention to Participate in Breast Cancer Screening among Urban Chinese Women: An Application of the Protection Motivation Theory" International Journal of Environmental Research and Public Health 18, no. 21: 11093. https://doi.org/10.3390/ijerph182111093
APA StyleZhang, M., Wei, W., Li, Q., Chen, X., Zhang, M., Zuo, D., & Liu, Q. (2021). Determinants of Intention to Participate in Breast Cancer Screening among Urban Chinese Women: An Application of the Protection Motivation Theory. International Journal of Environmental Research and Public Health, 18(21), 11093. https://doi.org/10.3390/ijerph182111093






