Association between Adjusted Handgrip Strength and Metabolic Syndrome in Arab Men
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participant Characteristics
2.2. Study Procedure
2.3. Measures of Body Composition and HGS
Data Management of Body Composition
2.4. Measures of MetS
Data Management of MetS
2.5. Statistical Analysis
3. Results
3.1. Description of HGS Categories
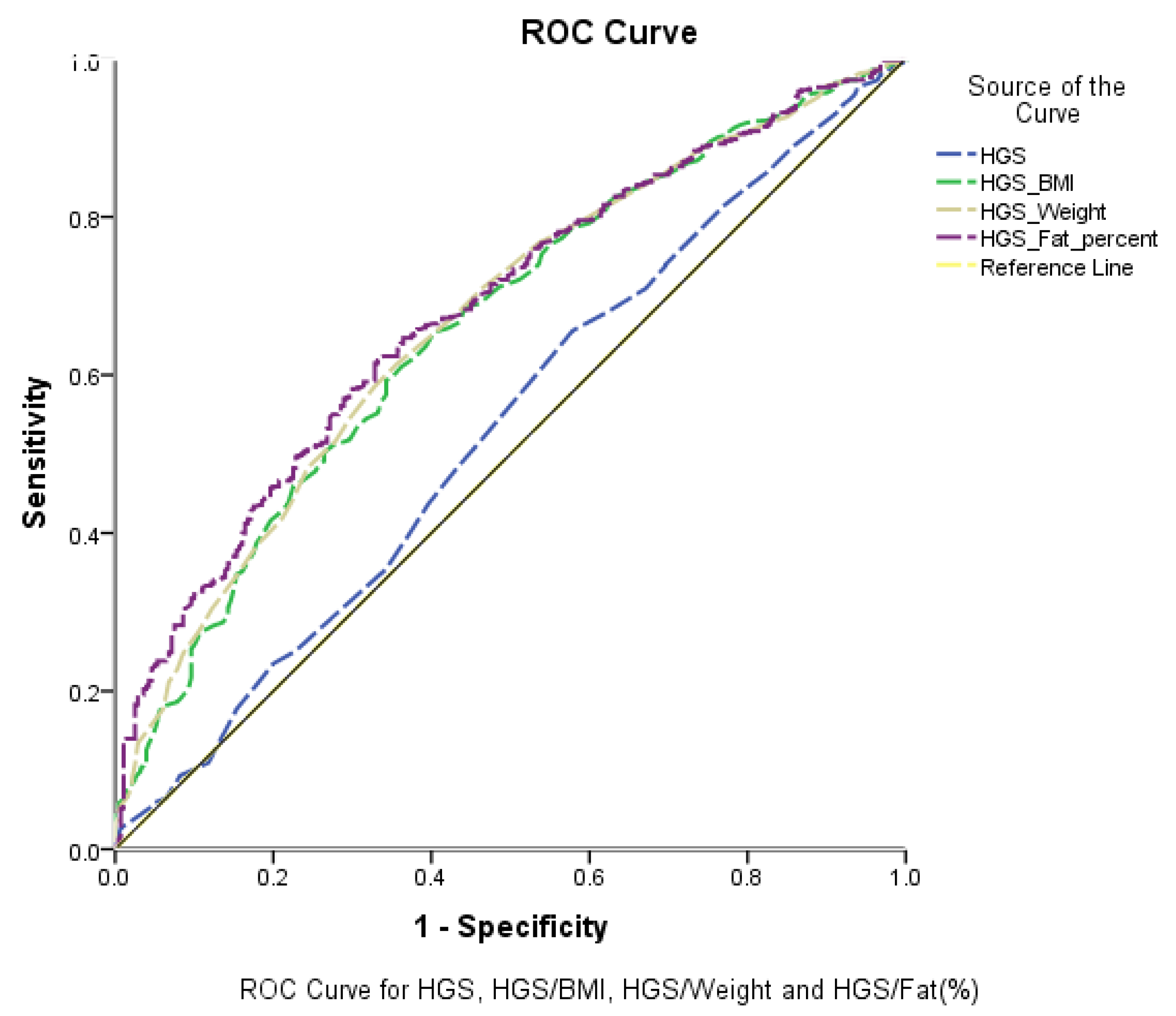
3.2. True-Positive and False-Negative Rates of Adjusted HGS Test Performance
3.3. Predictive Models of MetS Components
3.4. Association between Adjusted HGS and Risk of MetS and Its Components
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosenberg, I.H. Sarcopenia: Origins and Clinical Relevance. J. Nutr. 1997, 127, 990S–991S. [Google Scholar] [CrossRef] [Green Version]
- Cao, L.; Morley, J.E. Sarcopenia is recognized as an independent condition by an international classification of disease, tenth revision, clinical modification (ICD-10-CM) code. J. Am. Med. Dir. Assoc. 2016, 17, 675–677. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Landi, F.; Schneider, S.M.; Zúñiga, C.; Arai, H.; Boirie, Y.; Chen, L.-K.; Fielding, R.A.; Martin, F.C.; Michel, J.-P. Prevalence of and interventions for sarcopenia in ageing adults: A systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 2014, 43, 748–759. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.W.; Youm, Y.; Lee, W.J.; Choi, W.; Chu, S.H.; Park, Y.-R.; Kim, H.C. Appendicular Skeletal Muscle Mass and Insulin Resistance in an Elderly Korean Population: The Korean Social Life, Health and Aging Project-Health Examination Cohort. Diabetes Metab. J. 2015, 39, 37–45. [Google Scholar] [CrossRef]
- Srikanthan, P.; Hevener, A.L.; Karlamangla, A.S. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: Findings from the National Health and Nutrition Examination Survey III. PLoS ONE 2010, 5, e10805. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Lin, S.; Gao, T.; Zhong, F.; Cai, J.; Sun, Y.; Ma, A. Association between sarcopenia and metabolic syndrome in middle-aged and older non-obese adults: A systematic review and meta-analysis. Nutrients 2018, 10, 364. [Google Scholar] [CrossRef] [Green Version]
- Alhussain, M.H.; Alkahtani, S.; Aljuhani, O.; Habib, S.S. Effects of Nutrient Intake on Diagnostic Measures of Sarcopenia among Arab Men: A Cross-Sectional Study. Nutrients 2021, 13, 114. [Google Scholar] [CrossRef] [PubMed]
- Era, P.; Rantanen, T.; Avlund, K.; Gause-Nilsson, I.; Heikkinen, E.; Schroll, M.; Steen, B.; Suominen, H. Maximal isometric muscle strength and anthropometry in 75-year-old men and women in three Nordic localities. Scand. J. Med. Sci. Sports 1994, 4, 26–31. [Google Scholar] [CrossRef]
- Gill, A.; Plasqui, G.; Schols, A.M.; Kok, G. A benefit of being heavier is being strong: A cross-sectional study in young adults. Sports Med.-Open 2018, 4, 12. [Google Scholar]
- Rantanen, T.; Harris, T.; Leveille, S.G.; Visser, M.; Foley, D.; Masaki, K.; Guralnik, J.M. Muscle Strength and Body Mass Index as Long-Term Predictors of Mortality in Initially Healthy Men. J. Gerontol. Ser. A 2000, 55, M168–M173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flegal, K.M.; Kit, B.K.; Orpana, H.; Graubard, B.I. Association of All-Cause Mortality With Overweight and Obesity Using Standard Body Mass Index Categories: A Systematic Review and Meta-analysis. JAMA 2013, 309, 71–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alkahtani, S.; Aljuhani, O.; Alhussain, M.; Habib, S.S. Association between physical activity patterns and sarcopenia in Arab men. J. Int. Med. Res. 2020, 48, 0300060520918694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alberti, K.G.M.M.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabetes Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic syndrome—a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabetes Med. 2006, 23, 469–480. [Google Scholar] [CrossRef] [PubMed]
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.; Loria, C.M.; Smith, S.C. Harmonizing the Metabolic Syndrome. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chun, S.-W.; Kim, W.; Choi, K.H. Comparison between grip strength and grip strength divided by body weight in their relationship with metabolic syndrome and quality of life in the elderly. PLoS ONE 2019, 14, e0222040. [Google Scholar] [CrossRef] [PubMed]
- Ji, C.; Xia, Y.; Tong, S.; Wu, Q.; Zhao, Y. Association of handgrip strength with the prevalence of metabolic syndrome in US adults: The National health and nutrition examination survey. Aging 2020, 12, 7818. [Google Scholar] [CrossRef]
- Merchant, R.A.; Chan, Y.H.; Lim, J.Y.; Morley, J.E. Prevalence of Metabolic Syndrome and Association with Grip Strength in Older Adults: Findings from the HOPE Study. Diabetes Metab. Syndr. Obes. Targets Ther. 2020, 13, 2677–2686. [Google Scholar] [CrossRef] [PubMed]
- Chon, D.; Shin, J.; Kim, J.-H. Consideration of body mass index (BMI) in the association between hand grip strength and hypertension: Korean Longitudinal Study of Ageing (KLoSA). PLoS ONE 2020, 15, e0241360. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.-J.; Peng, L.-N.; Chiou, S.-T.; Chen, L.-K. Relative Handgrip Strength Is a Simple Indicator of Cardiometabolic Risk among Middle-Aged and Older People: A Nationwide Population-Based Study in Taiwan. PLoS ONE 2016, 11, e0160876. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sousa-Santos, A.; Amaral, T. Differences in handgrip strength protocols to identify sarcopenia and frailty—A systematic review. BMC Geriatr. 2017, 17, 238. [Google Scholar] [CrossRef] [Green Version]
- Alkahtani, S.A. A cross-sectional study on sarcopenia using different methods: Reference values for healthy Saudi young men. BMC Musculoskelet. Disord. 2017, 18, 119. [Google Scholar] [CrossRef] [Green Version]
- Davies, H.T.O.; Crombie, I.K.; Tavakoli, M. When can odds ratios mislead? BMJ 1998, 316, 989–991. [Google Scholar] [CrossRef] [Green Version]
- Pearce, N. What Does the Odds Ratio Estimate in a Case-Control Study? Int. J. Epidemiol. 1993, 22, 1189–1192. [Google Scholar] [CrossRef]
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Liao, K.H. Hand Grip Strength in Low, Medium, and High Body Mass Index Males and Females. Middle East J. Rehabil. Health 2016, 3, e53229. [Google Scholar] [CrossRef] [Green Version]
- Jiang, K.; Slee, A.; Davenport, A. Body composition and weakness of hand grip strength and pinch strength in patients with chronic kidney disease from different ethnic backgrounds. J. Hum. Nutr. Diet. 2021, 34, 450–455. [Google Scholar] [CrossRef]
- Abdulrazzaq, V.M.; Al-Rammahi, T.M.M.; Ashor, A.W. Association of hand grip strength with cardiometabolic markers in type 2 diabetes mellitus. AIP Conf. Proc. 2020, 2290, 030041. [Google Scholar] [CrossRef]
- Otten, J.; Stomby, A.; Waling, M.; Isaksson, A.; Tellström, A.; Lundin-Olsson, L.; Brage, S.; Ryberg, M.; Svensson, M.; Olsson, T. Benefits of a Paleolithic diet with and without supervised exercise on fat mass, insulin sensitivity, and glycemic control: A randomized controlled trial in individuals with type 2 diabetes. Diabetes/Metab. Res. Rev. 2017, 33, e2828. [Google Scholar] [CrossRef]
- Mainous, A.G.; Tanner, R.J.; Anton, S.D.; Jo, A. Grip Strength as a Marker of Hypertension and Diabetes in Healthy Weight Adults. Am. J. Prev. Med. 2015, 49, 850–858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Senechal, M.; McGavock, J.M.; Church, T.S.; Lee, D.-C.; Earnest, C.P.; Sui, X.; Blair, S.N. Cut points of muscle strength associated with metabolic syndrome in men. Med. Sci. Sports Exerc. 2014, 46, 1475–1481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jurca, R.; Lamonte, M.J.; Barlow, C.E.; Kampert, J.B.; Church, T.S.; Blair, S.N. Association of muscular strength with incidence of metabolic syndrome in men. Med. Sci. Sports Exerc. 2005, 37, 1849–1855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia-Hermoso, A.; Tordecilla-Sanders, A.; Correa-Bautista, J.E.; Peterson, M.D.; Izquierdo, M.; Prieto-Benavides, D.; Sandoval-Cuellar, C.; González-Ruíz, K.; Ramírez-Vélez, R. Handgrip strength attenuates the adverse effects of overweight on cardiometabolic risk factors among collegiate students but not in individuals with higher fat levels. Sci. Rep. 2019, 9, 6986. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perez-Sousa, M.Á.; del Pozo-Cruz, J.; Cano-Gutiérrez, C.A.; Ferrebuz, A.J.; Sandoval-Cuellar, C.; Izquierdo, M.; Hernandez-Quiñonez, P.A.; Ramirez-Vélez, R. Glucose Levels as a Mediator of the Detrimental Effect of Abdominal Obesity on Relative Handgrip Strength in Older Adults. J. Clin. Med. 2020, 9, 2323. [Google Scholar] [CrossRef] [PubMed]
- Chong, H.; Choi, Y.E.; Kong, J.Y.; Park, J.H.; Yoo, H.J.; Byeon, J.H.; Lee, H.J.; Lee, S.H. Association of Hand Grip Strength and Cardiometabolic Markers in Korean Adult Population: The Korea National Health and Nutrition Examination Survey 2015-2016. Korean J. Fam. Med. 2020, 41, 291–298. [Google Scholar] [CrossRef] [PubMed]
| Parameters | <27kg HGS | 27–42 kg HGS | >42kg HGS | p-Value |
|---|---|---|---|---|
| N | 60 | 434 | 360 | |
| HGS (kg) | 23.0 ± 3.3 | 36.5 ± 3.8 A | 48.5 ± 4.4 AB | <0.001 |
| HGS/BMI | 0.90 ± 0.2 | 1.35 ± 0.3 A | 1.70 ± 0.3 AB | <0.001 |
| HGS/weight | 0.33 ± 0.08 | 0.48 ± 0.09 A | 0.57 ± 0.11 AB | <0.001 |
| HGS/%Fat | 0.93 ± 0.6 | 1.50 ± 0.5 A | 2.0 ± 0.6 AB | <0.001 |
| Age (years) | 57.8 ± 17.4 | 40.8 ± 15.6A | 35.5 ± 11.8AB | <0.001 |
| Height (cm) | 165.8 ± 6.4 | 168.4 ± 6.4 A | 173.1 ± 6.1 AB | <0.001 |
| Weight (kg) | 76.2 ± 17.8 | 79.3 ± 15.6 | 87.0 ± 16.1 AB | <0.001 |
| BMI (kg/m2) | 27.3 ± 5.4 | 27.9 ± 5.1 | 29.1 ± 5.1 AB | 0.002 |
| Fat component (%) | 28.8 ± 8.3 | 26.5 ± 7.1 | 26.3 ± 6.8 A | 0.037 |
| Fat free mass (kg) | 52.7 ± 8.8 | 57.4 ± 7.6 A | 63.4 ± 7.4 AB | <0.001 |
| Muscle mass (kg) | 50.5 ± 9.1 | 54.6 ± 7.3 A | 60.2 ± 7.0 AB | <0.001 |
| Waist circumference (cm) | 90.8 ± 23.1 | 90.8 ± 19.4 | 92.9 ± 18.2 | 0.271 |
| Systolic BP (SBP) (mmHg) | 127.1 ± 19.5 | 119.6 ± 15.6 A | 119.7 ± 13.9 A | 0.002 |
| Diastolic BP (DBP) (mmHg) | 72.7 ± 10.8 | 75.3 ± 10.9 | 76.5 ± 10.2 A | 0.026 |
| Glucose (mg/dL) | 94.6 (82.4–157.6) | 94.8 (82.7–136.0) | 94.2 (83.6–111.9) | 0.498 |
| Total cholesterol (mg/dL) | 181.5 ± 58.2 | 177.9 ± 56.9 | 184.9 ± 54.3 | 0.218 |
| HDL cholesterol (mg/dL) | 39.6 ± 10.8 | 43.9 ± 10.8 A | 42.9 ± 11.4 | 0.021 |
| LDL cholesterol (mg/dL) | 115.6 ± 54.7 | 109.9 ± 55.4 | 116.3 ± 50.9 | 0.254 |
| TG (mg/dL) | 106.3 (84.0–177.3) | 103.9 (76.9–152) | 102.8 (77.9–147.1) | 0.477 |
| Parameters | MetS | WC > 94 cm | Hypertension > 130/85 (mmHg) | Glucose > 100 (mg/dL) | HDL < 40 (mg/dL) | TG > 150 (mg/dL) |
|---|---|---|---|---|---|---|
| ROC (95%CI) | ||||||
| HGS (kg) | 0.54 (0.49–0.57) | 0.49 (0.46–0.54) | 0.53 (0.49–0.58) | 0.54 (0.50–0.58) | 0.48 (0.44–0.52) | 0.54 (0.49–0.59) |
| HGS/BMI | 0.66 (0.63–0.70) ** | 0.75 (0.72–0.79) ** | 0.61 (0.57–0.65) ** | 0.56 (0.52–0.60) ** | 0.54 (0.49–0.58) | 0.62 (0.57–0.66) ** |
| HGS/Weight | 0.67 (0.63–0.71) ** | 0.79 (0.76–0.82) ** | 0.60 (0.56–0.64) ** | 0.55 (0.51–0.59) ** | 0.54 (0.49–0.58) | 0.61 (0.57–0.65) ** |
| HGS/%Fat | 0.70 (0.65–0.72) ** | 0.80 (0.77–0.83) ** | 0.62 (0.58–0.66) ** | 0.56 (0.52–0.60) ** | 0.56 (0.52–0.60) ** | 0.63 (0.59–0.67) ** |
| Parameters | WC | SBP | DBP | Glucose | HDL | TG |
|---|---|---|---|---|---|---|
| Beta (95%CI) | ||||||
| Model 1 | ||||||
| Adjusted R2 | 0.427 | 0.183 | 0.095 | 0.135 | 0.021 | 0.066 |
| Age | 0.22 (0.15–0.28) ** | 0.41 (0.35–0.48) ** | 0.15 (0.10–0.20) ** | 1.25 (1.01–1.47) ** | −0.03 (−0.09–0.02) | 1.23 (0.88–1.58) ** |
| Weight | 0.75 (0.69–0.82) ** | 0.15 (0.09–0.21) ** | 0.14 (0.09–0.19) ** | −0.01 (−0.22–0.21) | −0.11 (−0.16 to −0.06) ** | 0.46 (0.14–0.78) ** |
| HGS | −0.20 (−0.34 to −0.07) ** | 0.06 (−0.07–0.19) | 0.12 (0.03–0.22) * | 0.16 (−0.28–0.59) | 0.04 (−0.06–0.14) | 0.49 (−0.18–1.17) |
| Model 2 | ||||||
| Adjusted R2 | 0.408 | 0.191 | 0.101 | 0.135 | 0.021 | 0.073 |
| Age | 0.14 (0.07–0.21) ** | 0.39 (0.33–0.46) ** | 0.13 (0.08–0.18) ** | 1.23 (1.0–1.46) ** | −0.03 (−0.08–0.03) | 1.23 (0.88–1.58) ** |
| BMI | 2.28 (2.08–2.48) ** | 0.55 (0.36–0.74) ** | 0.47 (0.34–0.61) ** | 0.14 (−0.49–0.78) | −0.32 (−0.47 to −0.17) ** | 1.63 (0.64–2.61) ** |
| HGS | 0.02 (−0.12–0.15) | 0.09 (−0.03–0.21) | 0.16 (0.07–0.25)** | 0.14 (−0.28–0.56) | 0.02 (−0.08–0.12) | 0.54 (−0.11–1.19) |
| Model 3 | ||||||
| Adjusted R2 | 0.398 | 0.189 | 0.087 | 0.136 | 0.041 | 0.088 |
| Age | 0.07 (0.01–0.15) * | 0.38 (0.31–0.45) ** | 0.13 (0.07–0.18) ** | 1.27 (1.04–1.51) ** | −0.01 (−0.06–0.05) | 1.09 (0.73–1.45) ** |
| %Fat | 1.65 (1.5–1.79) ** | 0.38 (0.24–0.52) ** | 0.30 (0.20–0.39) ** | −0.27 (−0.73–0.20) | −0.33 (−0.44 to −0.22) ** | 1.84 (1.12–2.54) ** |
| HGS | 0.27 (0.14–0.40) ** | 0.15 (0.03–0.27) * | 0.21 (0.12–0.30) ** | 0.17 (−0.24–0.58) | −0.02 (−0.12–0.08) | 0.70 (0.06–1.34) * |
| Variables | HGS | HGS/BMI | HGS/Weight | HGS/%Fat | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Q1 | 1 | 1 | 1 | 1 | ||||
| Q2 | 0.81 (0.54–1.21) | 0.307 | 0.64 (0.44–0.94) | 0.024 | 0.59 (0.41–0.86) | 0.006 | 0.68 (0.5–0.99) | 0.044 |
| Q3 | 0.69 (0.45–1.06) | 0.089 | 0.39 (0.27–0.58) | <0.001 | 0.37 (0.25–0.56) | <0.001 | 0.40 (0.3–0.60) | <0.001 |
| Q4 | 0.72 (0.47–1.10) | 0.132 | 0.23 (0.15–0.36) | <0.001 | 0.19 (0.13–0.31) | <0.001 | 0.15(0.10–0.25) | <0.001 |
| Variables | High Waist | Hypertension | High Glucose | Low HDL | High Triglycerides | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| HGS | ||||||||||
| Q1 Q2 Q3 Q4 | 1 0.7 (0.5–1.1) 0.8 (0.5–1.2) 1.1 (0.7–1.6) | 0.09 0.19 0.92 | 1 0.6 (0.4–0.9) 0.4 (0.3–0.7) 0.8 (0.5–1.2) | 0.03 <0.001 0.21 | 1 0.9 (0.6–1.4) 1.0 (0.6–1.4) 0.7 (0.4–0.9) | 0.73 0.82 0.04 | 1 1.3 (0.9–1.9) 1.6 (1.1–2.4) 1.3 (0.8–1.9) | 0.19 0.03 0.26 | 1 0.7 (0.5–1.2) 0.9 (0.6–1.4) 0.6 (0.4–1.1) | 0.17 0.66 0.06 |
| HGS/BMI | ||||||||||
| Q1 Q2 Q3 Q4 | 1 0.9 (0.6–1.5) 0.23 (0.1–0.4) 0.13 (0.08–0.2) | 0.71 <0.001 <0.001 | 1 0.7 (0.5–1.0) 0.5 (0.3–0.8) 0.4 (0.3–0.6) | 0.06 0.001 <0.001 | 1 0.8 (0.6–1.2) 0.7 (0.5–1.1) 0.6 (0.4–0.9) | 0.26 0.09 0.02 | 1 0.9 (0.6–1.4) 0.9 (0.6–1.3) 0.6 (0.4–0.9) | 0.81 0.02 | 1 0.9 (0.6–1.3) 0.7 (0.4–1.0) 0.3 (0.2–0.5) | 0.56 0.06 <0.001 |
| HGS/Weight | ||||||||||
| Q1 Q2 Q3 Q4 | 1 0.5 (0.3–0.8) 0.2 (0.1–0.3) 0.1 (0.04–0.1) | 0.003 <0.001 <0.001 | 1 0.6 (0.4–0.9) 0.5 (0.3–0.7) 0.4 (0.3–0.6) | 0.03 <0.001 <0.001 | 1 0.9 (0.7–1.4) 0.8 (0.5–1.2) 0.6 (0.4–0.9) | 0.81 0.22 0.014 | 1 0.8 (0.6–1.2) 0.8 (0.6–1.2) 0.7 (0.5–1.1) | 0.34 0.30 0.08 | 1 0.7 (0.5–1.1) 0.7 (0.4–1.0) 0.3 (0.2–0.5) | 0.13 0.06 <0.001 |
| HGS/%Fat | ||||||||||
| Q1 Q2 Q3 Q4 | 1 0.8 (0.5–1.2) 0.2 (0.1–0.4) 0.06 (0.03–0.09) | 0.26 <0.001 <0.001 | 1 0.7 (0.4–0.9) 0.6 (0.4–0.8) 0.3 (0.1–0.5) | 0.042 <0.001 <0.001 | 1 1.0 (0.7–1.5) 0.7 (0.5–1.1) 0.6 (0.4–0.8) | 0.93 0.12 0.004 | 1 0.8 (0.5–1.2) 1.0 (0.7–1.5) 0.5 (0.3–0.7) | 0.32 0.97 0.001 | 1 0.7 (0.5–1.1) 0.8 (0.5–1.2) 0.2 (0.1–0.4) | 0.12 0.23 <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkahtani, S. Association between Adjusted Handgrip Strength and Metabolic Syndrome in Arab Men. Int. J. Environ. Res. Public Health 2021, 18, 10898. https://doi.org/10.3390/ijerph182010898
Alkahtani S. Association between Adjusted Handgrip Strength and Metabolic Syndrome in Arab Men. International Journal of Environmental Research and Public Health. 2021; 18(20):10898. https://doi.org/10.3390/ijerph182010898
Chicago/Turabian StyleAlkahtani, Shaea. 2021. "Association between Adjusted Handgrip Strength and Metabolic Syndrome in Arab Men" International Journal of Environmental Research and Public Health 18, no. 20: 10898. https://doi.org/10.3390/ijerph182010898
APA StyleAlkahtani, S. (2021). Association between Adjusted Handgrip Strength and Metabolic Syndrome in Arab Men. International Journal of Environmental Research and Public Health, 18(20), 10898. https://doi.org/10.3390/ijerph182010898






