Community Pharmacists’ Perceptions, Barriers, and Willingness for Offering Sexual and Reproductive Health Services
Abstract
:1. Introduction
Objectives
2. Methods
2.1. Study Design and Sampling
2.2. Inclusion Criteria
2.3. Survey Development
2.4. Data Collection
2.5. Data Analysis
2.6. Ethical Considerations
3. Results
3.1. Demographics
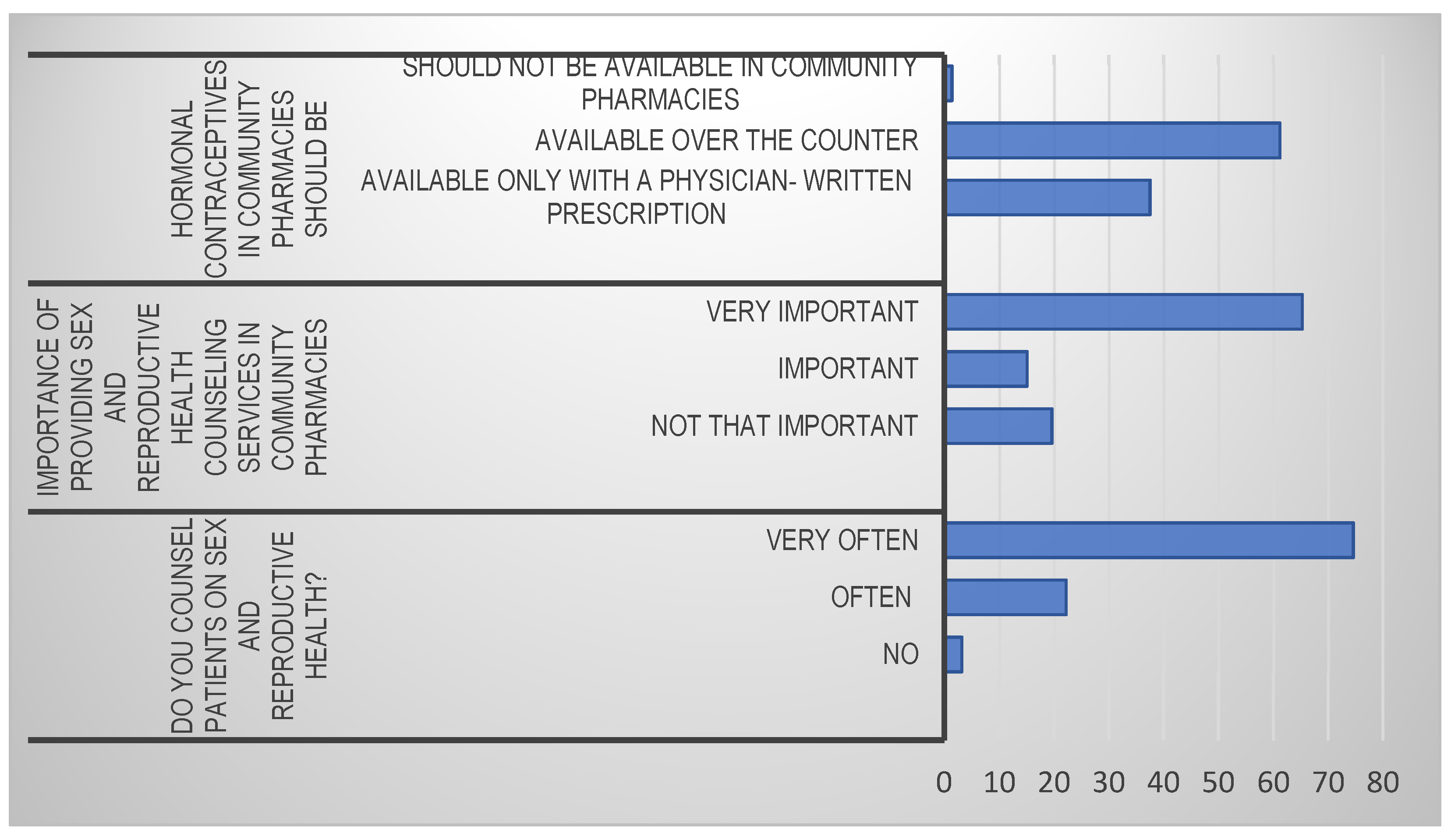
3.2. Perceptions on Offering Sex Education and Reproductive Health Services
3.3. Barriers to the Provision of Sex Education and Reproductive Health Services
3.4. Proficiency
4. Discussion
4.1. Perceptions and Barriers
4.2. Proficiency
4.3. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alkhateeb, F.M.; Thompson, I.; Krska, J. Pharmacy in Public Health; Pharmaceutical Press: London, UK, 2011; p. 284. [Google Scholar]
- Al-Hassan, M.I. A Look at Community Pharmacy Practice in Saudi Arabia. Res. J. Med. Sci. 2009, 1, 3111–3114. [Google Scholar]
- Eades, C.E.; Ferguson, J.E.; O’Carroll, R.E. Public health in community pharmacy: A systematic review of pharmacist and consumer views. BMC Public Health 2011, 11, 582. [Google Scholar] [CrossRef] [Green Version]
- Levin, B.L.; Hurd, P.D.; Hanson, A. Introduction to Public Health in Pharmacy; Jones & Bartlett Publishers: Burlington, MA, USA, 2007. [Google Scholar]
- Lee, C.K. Are pharmacists prepared to be sexual/reproductive health educators? Am. J. Pharm. Educ. 2010, 74, 10. [Google Scholar]
- Gonsalves, L.; Hindin, M.J. Pharmacy provision of sexual and reproductive health commodities to young people: A systematic literature review and synthesis of the evidence. Contraception 2017, 95, 339–363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dehlendorf, C.; Krajewski, C.; Borrero, S. Contraceptive Counseling: Best Practices to Ensure Quality Communication and Enable Effective Contraceptive Use. Clin. Obstet. Gynecol. 2014, 659–673. [Google Scholar] [CrossRef] [PubMed]
- WHO. Joint FIP/WHO Guidelines on Good Pharmacy Practise: Standards for Quality of Pharmacy Services; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Godia, P.; Olenja, J.; Lavussa, J.; Quinney, D.; Hofman, J.; van den Broek, N. Sexual reproductive health service provision to young people in Kenya; health service providers’ experiences. BMC Health Serv. Res. 2013, 13, 476. [Google Scholar] [CrossRef] [Green Version]
- Karim, S.I.; Irfan, F.; Al Rowais, N.; Al Zahrani, B.; Qureshi, R.; Al Qadrah, B.H. Emergency contraception: Awareness, attitudes and barriers of Saudi Arabian Women. Pak. J. Med. Sci. 2015, 31, 1500. [Google Scholar] [CrossRef] [Green Version]
- Vella, M.; Grima, M.; Wirth, F.; Attard Pizzuto, M.; Sammut Bartolo, B.; Vella, J.; Azzopardi, L.M. Consumer perception of community pharmacist extended professional services. J. Pharm. Health Serv. Res. 2015, 6, 91–96. [Google Scholar] [CrossRef]
- Dhaher, E.A. Access to Reproductive Health Care Services for Women in the Southern Region of Saudi Arabia. Women’s Reprod. Health 2017, 4, 126–140. [Google Scholar] [CrossRef]
- Shawky, S.; Milaat, W. Early teenage marriage and subsequent pregnancy outcome. East. Mediterr. Health J. 2000, 6, 46–54. [Google Scholar] [CrossRef]
- Farih, M.; Khan, K.; Freeth, D.; Meads, C. Protocol study: Sexual and reproductive health knowledge, information-seeking behaviour and attitudes among Saudi women: A questionnaire survey of university students. Reprod. Health 2014, 11, 34. [Google Scholar] [CrossRef] [Green Version]
- Rashad, H.; Osman, M.; Roudi-Fahimi, F. Marriage in the Arab World; Population Reference Bureau: Washington, DC, USA, 2005. [Google Scholar]
- WHO. Saudi Arabia: Reproductive Health Profile 2008; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Snyder, M.E.; Zillich, A.J.; Primack, B.A.; Rice, K.R.; Somma McGivney, M.A.; Pringle, J.L.; Smith, R.B. Exploring successful community pharmacist-physician collaborative working relationships using mixed methods. Res. Soc. Adm. Pharm. 2010, 6, 307–323. [Google Scholar] [CrossRef] [Green Version]
- Matowe, L.; Mori, A.T.; Mawa, S. Enhancing the role of pharmacists in public health in developing countries. Pharm. J. 2012, 288, 623. [Google Scholar]
- Benjamin, G.C. Ensuring population health: An important role for pharmacy. Am. J. Pharm. Educ. 2016, 80, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO; OECD; The World Bank. Delivering Quality Health Services: A Global Imperative for Universal Health Coverage; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Rashidian, M.; Minichiello, V.; Knutsen, S.F.; Ghamsary, M. Barriers to sexual health care: A survey of Iranian-American physicians in California, USA. BMC Health Serv. Res. 2016, 16, 263. [Google Scholar] [CrossRef] [Green Version]
- The American Public Health Association. The Role of the Pharmacist in Public Health. Am. Public Health Assoc. 2006, 200614. Available online: https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/07/13/05/the-role-of-the-pharmacist-in-public-health (accessed on 24 October 2020).
- Thongmixay, S.; Essink, D.R.; de Greeuw, T.; Vongxay, V.; Sychareun, V.; Broerse, J.E.W. Perceived barriers in accessing sexual and reproductive health services for youth in Lao People’s Democratic Republic. PLoS ONE 2019, 14, e0218296. [Google Scholar] [CrossRef] [Green Version]
- AlRuthia, Y.; Alsenaidy, M.A.; Alrabiah, H.K.; AlMuhaisen, A.; Alshehri, M. The status of licensed pharmacy workforce in Saudi Arabia: A 2030 economic vision perspective. Hum. Resour. Health 2018, 16, 28. [Google Scholar] [CrossRef]
- Langenbrunner, J.C.; O’Duagherty, S.; Cashin, C.S. Designing and Implementing Health Care Provider Payment Systems: “How-to” Manuals; The World Bank: Washington, DC, USA, 2009. [Google Scholar]
- Sachdev, S.B.; Verma, H.V. Relative importance of service quality dimensions: A multisectoral study. J. Serv. Res. 2004, 4, 93–116. [Google Scholar]
- El-Mowafi, I.M.; Foster, A.M. Emergency contraception in Jordan: Assessing retail pharmacists’ awareness, opinions, and perceptions of need. Contraception 2020, 101, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Setia, M. Methodology series module 3: Cross-sectional studies. Indian J. Dermatol. 2016, 61, 261. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Windows, Version 26.0.; IBM Corp: Armonk, NY, USA, 2019. [Google Scholar]
- Jager, J.; Putnick, D.L.; Bornstein, M.H. More than just convenient: The scientific merits of homogeneous convenience samples. Monogr. Soc. Res. Child Dev. 2017, 82, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Surveysystem. Sample Size Calculator—Confidence Level, Confidence Interval, Sample Size, Population Size, Relevant Population—Creative Research Systems. 2021. Available online: https://www.surveysystem.com/sscalc.htm (accessed on 4 July 2021).
- Tian, L.; Li, J.; Zhang, K. Women’s status, institutional barriers and reproductive health care: A case study in Yunnan, China. Health Policy 2008, 84, 284–297. [Google Scholar] [CrossRef] [PubMed]
- D’Ambruoso, L.; Abbey, M.; Hussein, J. Please understand when I cry out in pain: Women’s accounts of maternity services during labour and delivery in Ghana. BMC Public Health 2005, 5, 140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Zahrani, A. Women’s Sexual Health Care in Saudi Arabia: A Focused Ethnographic Study. Ph.D. Thesis, University of Sheffield, Sheffield, UK, 2011. [Google Scholar]
| Descriptive Characteristics of the Respondents | ||
|---|---|---|
| Particulars | Frequency | Percent |
| Age | ||
| 22–34 years | 856 | 78.0 |
| 35–44 years | 218 | 19.9 |
| 45–54 years | 23 | 2.1 |
| Gender | ||
| Female | 36 | 3.3 |
| Male | 1061 | 96.7 |
| Work location | ||
| In a city | 1006 | 91.7 |
| In a village | 91 | 8.3 |
| Qualification | ||
| Bachelor | 978 | 89.2 |
| Diploma | 6 | 0.5 |
| Fellowship or residency program | 1 | 0.1 |
| Masters | 9 | 0.8 |
| Pharm.D. | 103 | 9.4 |
| Working region | ||
| Central region | 261 | 23.8 |
| Eastern region | 105 | 9.6 |
| Northern region | 104 | 9.5 |
| Southern region | 210 | 19.1 |
| Western region | 417 | 38.0 |
| Board certification | ||
| No | 823 | 75.0 |
| Yes | 274 | 25.0 |
| Present professional level | ||
| Consultant pharmacist | 26 | 2.4 |
| Pharmacist | 781 | 71.2 |
| Senior pharmacist | 289 | 26.3 |
| Technician | 1 | 0.1 |
| Marital status | ||
| Married | 831 | 75.8 |
| Single | 261 | 23.8 |
| Nationality | ||
| Non-Saudi | 1018 | 92.8 |
| Saudi | 79 | 7.2 |
| Work place | ||
| Chain pharmacy | 1092 | 99.5 |
| Independent pharmacy | 5 | 0.5 |
| Employment contract status | ||
| Full-time | 1052 | 95.9 |
| Part-time | 45 | 4.1 |
| Years of experience | ||
| <2 years | 63 | 5.7 |
| 2–5 years | 292 | 26.6 |
| 6–10 years | 474 | 43.2 |
| >10 years | 268 | 24.4 |
| N | Total Number of Responses (1097) | ||||||
|---|---|---|---|---|---|---|---|
| Item | Percentages | Mean | |||||
| Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree | |||
| 1 | Workload | 7 | 70 | 3 | 15 | 5 | 2.3 |
| 2 | Lack of supportive policy | 2 | 6 | 54 | 36 | 2 | 3.5 |
| 3 | Lack of privacy during service provision | 8 | 12 | 1 | 25 | 54 | 3.8 |
| 4 | Lack of information about patient health | 1 | 1 | 2 | 8 | 88 | 4.7 |
| 5 | Fear for responsibility and liability issues | 0 | 1 | 2 | 5 | 92 | 4.8 |
| 6 | Impatient behavior of the patient | 56 | 28 | 0 | 14 | 2 | 1.7 |
| 7 | Lack of incentives and financial rewards | 2 | 4 | 34 | 45 | 15 | 3.2 |
| 8 | Pharmacists not knowledgeable enough | 5 | 12 | 18 | 36 | 27 | 3.1 |
| 9 | Lack of social acceptability | 2 | 5 | 8 | 10 | 75 | 4.6 |
| 10 | Gender difference | 1 | 3 | 3 | 10 | 83 | 4.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshahrani, A.M.; Alsheikh, M.Y. Community Pharmacists’ Perceptions, Barriers, and Willingness for Offering Sexual and Reproductive Health Services. Int. J. Environ. Res. Public Health 2021, 18, 10735. https://doi.org/10.3390/ijerph182010735
Alshahrani AM, Alsheikh MY. Community Pharmacists’ Perceptions, Barriers, and Willingness for Offering Sexual and Reproductive Health Services. International Journal of Environmental Research and Public Health. 2021; 18(20):10735. https://doi.org/10.3390/ijerph182010735
Chicago/Turabian StyleAlshahrani, Ali Mofleh, and Mona Y. Alsheikh. 2021. "Community Pharmacists’ Perceptions, Barriers, and Willingness for Offering Sexual and Reproductive Health Services" International Journal of Environmental Research and Public Health 18, no. 20: 10735. https://doi.org/10.3390/ijerph182010735
APA StyleAlshahrani, A. M., & Alsheikh, M. Y. (2021). Community Pharmacists’ Perceptions, Barriers, and Willingness for Offering Sexual and Reproductive Health Services. International Journal of Environmental Research and Public Health, 18(20), 10735. https://doi.org/10.3390/ijerph182010735






