Risk and Resilience: How Is the Health of Older Adults and Immigrant People Living in Canada Impacted by Climate- and Air Pollution-Related Exposures?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Identifying the Research Question
- What are the reported health impacts of climate- and air pollution-related exposures in older adults and immigrants in Canada?
- Are there socioeconomic and contextual characteristics that impact the relationship between these exposures and adverse health outcomes in these populations?
2.2. Identifying Relevent Studies
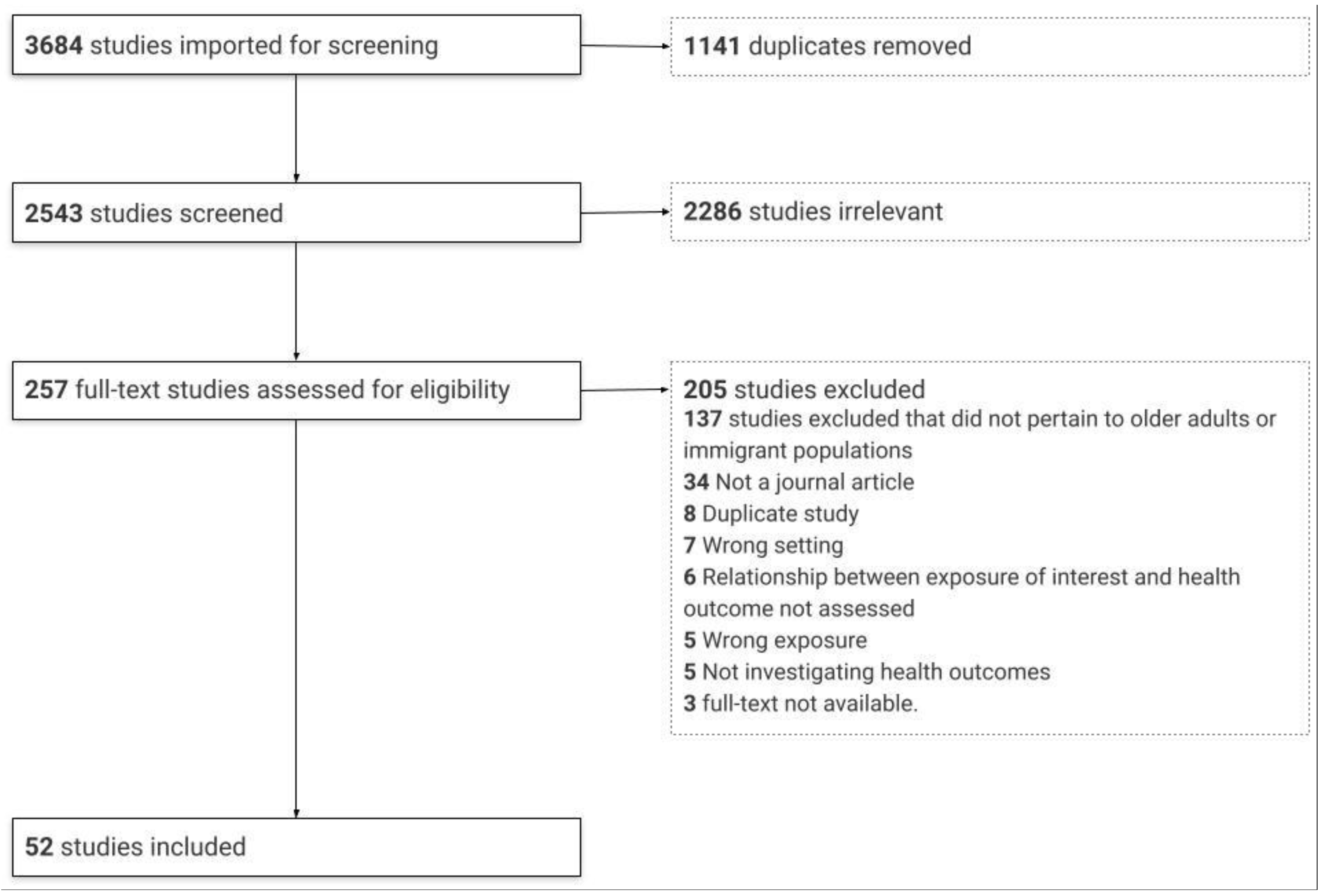
2.3. Study Selection
2.4. Charting the Data
2.5. Collating, Summarizing, and Reporting the Results
3. Results
3.1. Profile of Studies
3.2. Meteorological Parameters
3.2.1. Health Impacts of Meteorological Parameters on Older Adults
Mortality
Overall Morbidity
Cardiovascular Health Outcomes
Respiratory Health Outcomes
Fall-Related Injuries
Mental Health Outcomes
Renal Health Outcomes
Ocular Health Outcomes
Diabetes
3.2.2. Health Impacts in Immigrant Populations
3.3. Air Pollution
3.3.1. Health Impacts of Air Pollution in Older Adults
Cardiovascular Health Outcomes
Respiratory Health Outcomes
Cancer
Neurological Health Outcomes
Diabetes
Mortality
Musculoskeletal Outcomes
3.3.2. Health Impacts in Immigrant Populations
3.4. Factors Influencing the Climate– and Air Pollution–Health Relationships
3.4.1. Sociodemographic Characteristics
3.4.2. Socioeconomic Characteristics
3.4.3. Environmental Characteristics
4. Discussion
4.1. Evidence for Older Adult Health Risk due to Climate- and Air Pollution-Related Exposures in Canada
4.2. One Size Does Not Fit All: Contextual Factors Influencing Older Adult Health Risk
4.3. Missing Knowledge of the Health Risk Facing Immigrant Communities in Canada
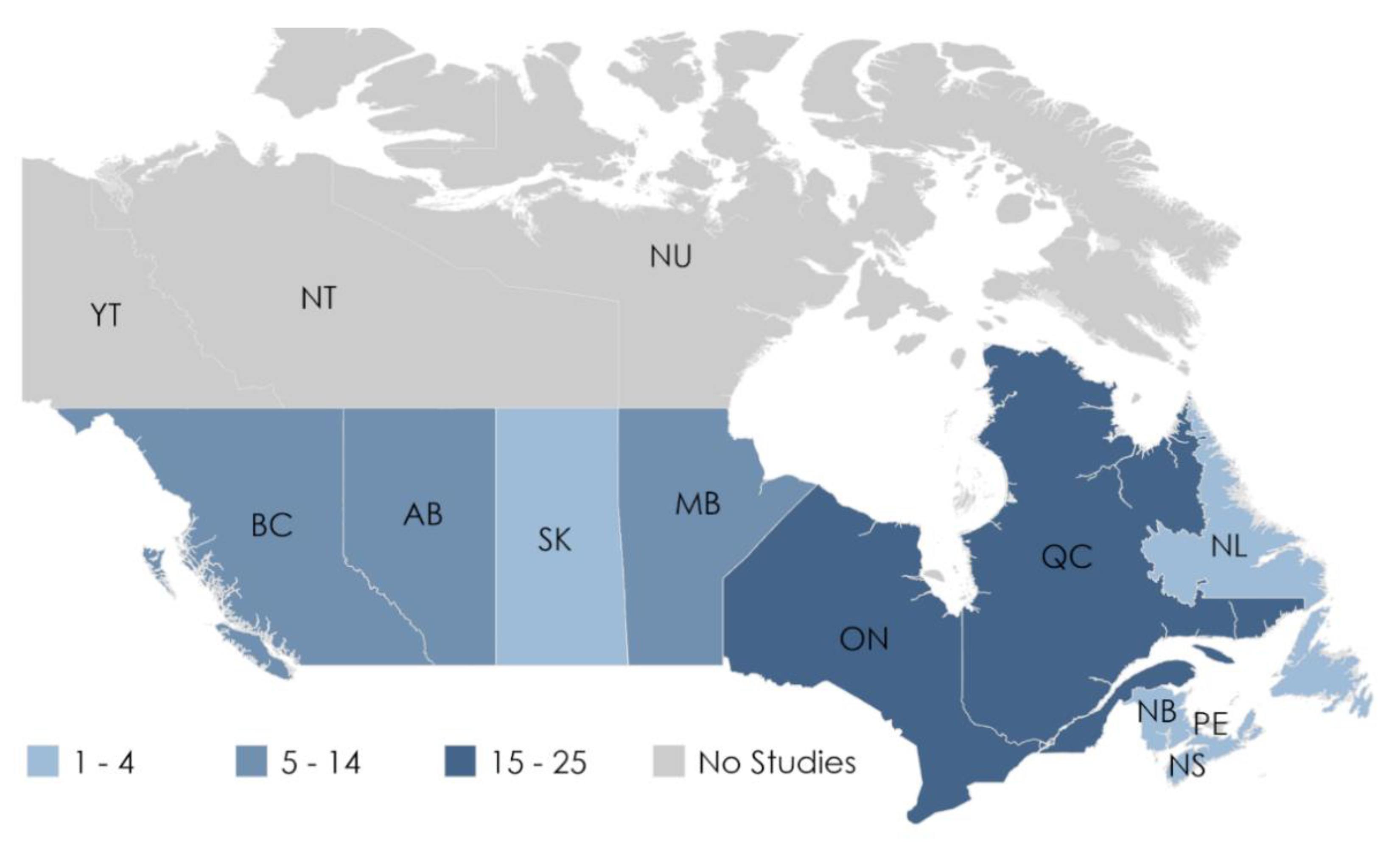
4.4. Geographical Gaps in the Literature
4.5. Limitations
5. Conclusions and Next Steps
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Did You Know? By Taking Action on Climate Change You Can Strengthen Public Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- World Health Organization. Health and the Environment: Addressing the Health Impact of Air Pollution; Sixty-Eighth World Health Assembly Agenda 68/18 Item 146 2015:6; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Bush, E.; Lemmen, D.S. (Eds.) Canada’s Changing Climate Report; Government of Canada: Ottawa, ON, Canada, 2019. [Google Scholar]
- Smith, K.R.; Woodward, A.; Campbell-Lendrum, D.; Chadee, D.D.; Honda, Y.; Qiyong, L.; Olwoch, J.M.; Revich, B.; Sauerborn, R. Human health: Impacts, adaptation, and co-benefits. In Climate Change 2014 Impacts, Adaptation and Vulnerability: Part A: Global and Sectoral Aspects; Cambridge University Press: Cambridge, UK, 2015. [Google Scholar] [CrossRef]
- Warren, F.J.; Lemmen, D.S. (Eds.) Canada in a Changing Climate: Sector Perspectives on Impacts and Adaptation; Government of Canada: Ottawa, ON, Canada, 2014. [Google Scholar]
- Health Canada. Health Impacts of Air Pollution in Canada Estimates of Premature Deaths and Nonfatal Outcomes; Government of Canada: Ottawa, ON, Canada, 2021. [Google Scholar]
- Alberini, A.; Gans, W.; Alhassan, M. Individual and Public-Program Adaptation: Coping with Heat Waves in Five Cities in Canada. Int. J. Environ. Res. Public Health 2011, 8, 4679–4701. [Google Scholar] [CrossRef] [PubMed]
- Manangan, A.P.; Uejio, C.K.; Saha, S.; Schramm, P.J.; Marinucci, G.D.; Brown, C.L.; Hess, J.J.; Luber, G. Assessing health vulnerability to climate change: A guide for health departments. In Climate Change and Public Health: Federal Preparedness Efforts; Nova Science Publishers: Hauppauge, NY, USA, 2016; pp. 71–93. [Google Scholar]
- Benevolenza, M.A.; DeRigne, L. The impact of climate change and natural disasters on vulnerable populations: A systematic review of literature. J. Hum. Behav. Soc. Environ. 2019, 29, 266–281. [Google Scholar] [CrossRef]
- Seguin, J. (Ed.) Human Health in a Changing Climate: A Canadian Assessment of Vulnerabilities and Adaptive Capacity. In Human Health in a Changing Climate; Health Canada: Ottawa, ON, Canada, 2008. [Google Scholar]
- Statistics Canada. Population Projections for Canada; Statistics Canada: Ottawa, ON, Canada, 2010. [Google Scholar]
- Morency, J.-D.; Caron-Malenfant, E.; MacIsaac, S.; Statistics Canada. Immigration and diversity: Population projections for Can-ada and its regions, 2011 to 2036; Statistics Canada: Ottawa, ON, Canada, 2017. [Google Scholar]
- Statistics Canada. Immigration and Ethnocultural Diversity: Key Results from the 2016 Census; The Daily: New York, NY, USA, 2017; pp. 1–8. [Google Scholar]
- Åström, C.; Orru, H.; Rocklöv, J.; Strandberg, G.; Ebi, K.L.; Forsberg, B. Heat-related respiratory hospital admissions in Europe in a changing climate: A health impact assessment. BMJ Open 2013, 3, e001842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abrahamson, V.; Wolf, J.; Lorenzoni, I.; Fenn, B.; Kovats, S.; Wilkinson, P.; Adger, W.N.; Raine, R. Perceptions of heatwave risks to health: Interview-based study of older people in London and Norwich, UK. J. Public Health 2008, 31, 119–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kenny, G.P.; Yardley, J.; Brown, C.; Sigal, R.J.; Jay, O. Heat stress in older individuals and patients with common chronic diseases. Can. Med. Assoc. J. 2010, 182, 1053–1060. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bunker, A.; Wildenhain, J.; Vandenbergh, A.; Henschke, N.; Rocklöv, J.; Hajat, S.; Sauerborn, R. Effects of Air Temperature on Climate-Sensitive Mortality and Morbidity Outcomes in the Elderly; a Systematic Review and Meta-analysis of Epidemiological Evidence. EBioMedicine 2016, 6, 258–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leyva, E.W.A.; Beaman, A.; Davidson, P.M. Health Impact of Climate Change in Older People: An Integrative Review and Implications for Nursing. J. Nurs. Sch. 2017, 49, 670–678. [Google Scholar] [CrossRef]
- Vang, Z.M.; Sigouin, J.; Flenon, A.; Gagnon, A. Are immigrants healthier than native-born Canadians? A systematic review of the healthy immigrant effect in Canada. Ethn. Health 2017, 22, 209–241. [Google Scholar] [CrossRef]
- Beiser, M. The Health of Immigrants and Refugees in Canada. Can. J. Public Health 2005, 96, S30–S44. [Google Scholar] [CrossRef]
- Hansen, A.; Bi, L.; Saniotis, A.; Nitschke, M. Vulnerability to extreme heat and climate change: Is ethnicity a factor? Glob. Health Action 2013, 6, 21364. [Google Scholar] [CrossRef] [Green Version]
- McMichael, C.; Barnett, J.; McMichael, A.J. An Ill Wind? Climate Change, Migration, and Health. Environ. Health Perspect. 2012, 120, 646–654. [Google Scholar] [CrossRef]
- Otto, I.M.; Reckien, D.; Reyer, C.; Marcus, R.; Le Masson, V.; Jones, L.; Norton, A.; Serdeczny, O. Social vulnerability to climate change: A review of concepts and evidence. Reg. Environ. Chang. 2017, 17, 1651–1662. [Google Scholar] [CrossRef]
- Tilstra, M.H.; Tiwari, I.; Niwa, L.; Campbell, S.; Jones, C.A.; Quemerais, B.; Yamamoto, S.S. Characterising Sensitivity to Climate Change in Older Adults and Immigrants in Canada—A Scoping Review Protocol. Open Science Framework Web. OSF 2020. Available online: osf.io/axt67 (accessed on 20 June 2021).
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- International Health Conference. Constitution of the World Health Organization. Public Health Rep. 1946, 61, 1268–1279. [Google Scholar]
- Statistics Canada. Immigrant n.d. Available online: https://www23.statcan.gc.ca/imdb/p3Var.pl?Function=Unit&Id=85107 (accessed on 20 June 2021).
- Vanasse, A.; Talbot, D.; Chebana, F.; Bélanger, D.; Blais, C.; Gamache, P.; Giroux, J.-X.; Dault, R.; Gosselin, P. Effects of climate and fine particulate matter on hospitalizations and deaths for heart failure in elderly: A population-based cohort study. Environ. Int. 2017, 106, 257–266. [Google Scholar] [CrossRef] [Green Version]
- Bai, L.; Li, Q.; Wang, J.; Lavigne, E.; Gasparrini, A.; Copes, R.; Yagouti, A.; Burnett, R.T.; Goldberg, M.S.; Cakmak, S.; et al. Increased coronary heart disease and stroke hospitalisations from ambient temperatures in Ontario. Hearth 2018, 104, 673–679. [Google Scholar] [CrossRef] [Green Version]
- Vida, S.; Durocher, M.; Ouarda, T.B.M.J.; Gosselin, P. Relationship Between Ambient Temperature and Humidity and Visits to Mental Health Emergency Departments in Québec. Psychiatr. Serv. 2012, 63, 1150–1153. [Google Scholar] [CrossRef]
- Wang, X.; Lavigne, E.; Ouellette-Kuntz, H.; Chen, B.E. Acute impacts of extreme temperature exposure on emergency room admissions related to mental and behavior disorders in Toronto, Canada. J. Affect. Disord. 2014, 155, 154–161. [Google Scholar] [CrossRef]
- Benmarhnia, T.; Kaufman, J.S. When evidence of heat-related vulnerability depends on the contrast measure. Int. J. Biometeorol. 2017, 61, 391–393. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.B.; Wan, V.; Kosatsky, T. Differences in heat-related mortality across four ecological regions with diverse urban, rural, and remote populations in British Columbia, Canada. Health Place 2013, 23, 48–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vutcovici, M.; Goldberg, M.S.; Valois, M.-F. Effects of diurnal variations in temperature on non-accidental mortality among the elderly population of Montreal, Québec, 1984–2007. Int. J. Biometeorol. 2014, 58, 843–852. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kosatsky, T.; Henderson, S.B.; Pollock, S.L. Shifts in Mortality During a Hot Weather Event in Vancouver, British Columbia: Rapid Assessment With Case-Only Analysis. Am. J. Public Health 2012, 102, 2367–2371. [Google Scholar] [CrossRef]
- Chen, H.; Wang, J.; Li, Q.; Yagouti, A.; Lavigne, E.; Foty, R.; Burnett, R.T.; Villeneuve, P.J.; Cakmak, S.; Copes, R. Assessment of the effect of cold and hot temperatures on mortality in Ontario, Canada: A population-based study. CMAJ Open 2016, 4, E48–E58. [Google Scholar] [CrossRef] [Green Version]
- Bustinza, R.; Lebel, G.; Gosselin, P.; Bélanger, D.; Chebana, F. Health impacts of the July 2010 heat wave in Québec, Canada. BMC Public Health 2013, 13, 56. [Google Scholar] [CrossRef] [Green Version]
- Burton, H.; Rabito, F.; Danielson, L.; Takaro, T.K. Health effects of flooding in Canada: A 2015 review and description of gaps in research. Can. Water Resour. J. 2016, 41, 238–249. [Google Scholar] [CrossRef]
- Mondor, L.; Charland, K.; Verma, A.; Buckeridge, D.L. Weather warnings predict fall-related injuries among older adults. Age Ageing 2015, 44, 403–408. [Google Scholar] [CrossRef] [Green Version]
- Modarres, R.; Ouarda, T.B.; Vanasse, A.; Orzanco, M.G.; Gosselin, P. Modeling seasonal variation of hip fracture in Montreal, Canada. Bone 2012, 50, 909–916. [Google Scholar] [CrossRef]
- Modarres, R.; Ouarda, T.B.M.J.; Vanasse, A.; Orzanco, M.G.; Gosselin, P. Modeling climate effects on hip fracture rate by the multivariate GARCH model in Montreal region, Canada. Int. J. Biometeorol. 2014, 58, 921–930. [Google Scholar] [CrossRef]
- Auger, N.; Rhéaume, M.-A.; Bilodeau-Bertrand, M.; Tang, T.; Kosatsky, T. Climate and the eye: Case-crossover analysis of retinal detachment after exposure to ambient heat. Environ. Res. 2017, 157, 103–109. [Google Scholar] [CrossRef]
- Laverdière, É.; Payette, H.; Gaudreau, P.; Morais, J.A.; Shatenstein, B.; Généreux, M. Risk and protective factors for heat-related events among older adults of Southern Quebec (Canada): The NuAge study. Can. J. Public Health 2016, 107, e258–e265. [Google Scholar] [CrossRef]
- Bélanger, D.; Gosselin, P.; Valois, P.; Abdous, B. Perceived Adverse Health Effects of Heat and Their Determinants in Deprived Neighbourhoods: A Cross-Sectional Survey of Nine Cities in Canada. Int. J. Environ. Res. Public Health 2014, 11, 11028–11053. [Google Scholar] [CrossRef] [Green Version]
- Stapleton, J.M.; LaRose, J.; Simpson, C.; Flouris, A.; Sigal, R.J.; Kenny, G.P. Do older adults experience greater thermal strain during heat waves? Appl. Physiol. Nutr. Metab. 2014, 39, 292–298. [Google Scholar] [CrossRef]
- Tajmir, P.; Grierson, L.E.M.; Carnahan, H. Interactions between Cold Ambient Temperature and Older Age on Haptic Acuity and Manual Performance. Can. J. Aging 2013, 32, 195–202. [Google Scholar] [CrossRef]
- McTavish, R.K.; Richard, L.; McArthur, E.; Shariff, S.Z.; Acedillo, R.; Parikh, C.R.; Wald, R.; Wilk, P.; Garg, A.X. Association Between High Environmental Heat and Risk of Acute Kidney Injury Among Older Adults in a Northern Climate: A Matched Case-Control Study. Am. J. Kidney Dis. 2018, 71, 200–208. [Google Scholar] [CrossRef]
- Ordon, M.; Welk, B.; Li, Q.; Wang, J.; Lavigne, E.; Yagouti, A.; Copes, R.; Cakmak, S.; Chen, H. Ambient Temperature and the Risk of Renal Colic: A Population-Based Study of the Impact of Demographics and Comorbidity. J. Endourol. 2016, 30, 1138–1143. [Google Scholar] [CrossRef]
- Krstić, G. Apparent Temperature and Air Pollution vs. Elderly Population Mortality in Metro Vancouver. PLoS ONE 2011, 6, e25101. [Google Scholar] [CrossRef] [Green Version]
- Parent, M.-É.; Goldberg, M.S.; Crouse, D.; Ross, N.A.; Chen, H.; Valois, M.-F.; Liautaud, A. Traffic-related air pollution and prostate cancer risk: A case–control study in Montreal, Canada. Occup. Environ. Med. 2013, 70, 511–518. [Google Scholar] [CrossRef]
- Goldberg, M.S.; Labrèche, F.; Weichenthal, S.; Lavigne, E.; Valois, M.-F.; Hatzopoulou, M.; Shekarrizfard, M. Number concentrations of ultrafine particles and the incidence of postmenopausal breast cancer. Environ. Epidemiol. 2018, 2, e006. [Google Scholar] [CrossRef]
- Goldberg, M.S.; Labrèche, F.; Weichenthal, S.; Lavigne, E.; Valois, M.-F.; Hatzopoulou, M.; Van Ryswyk, K.; Shekarrizfard, M.; Villeneuve, P.; Crouse, D.; et al. The association between the incidence of postmenopausal breast cancer and concentrations at street-level of nitrogen dioxide and ultrafine particles. Environ. Res. 2017, 158, 7–15. [Google Scholar] [CrossRef]
- Chen, L.; Villeneuve, P.J.; Rowe, B.H.; Liu, L.; Stieb, D.M. The Air Quality Health Index as a predictor of emergency department visits for ischemic stroke in Edmonton, Canada. J. Expo. Sci. Environ. Epidemiol. 2014, 24, 358–364. [Google Scholar] [CrossRef]
- Wang, X.; Kindzierski, W.B.; Kaul, P. Air Pollution and Acute Myocardial Infarction Hospital Admission in Alberta, Canada: A Three-Step Procedure Case-Crossover Study. PLoS ONE 2015, 10, e0132769. [Google Scholar] [CrossRef]
- Weichenthal, S.; Kulka, R.; Lavigne, E.; van Rijswijk, D.; Brauer, M.; Villeneuve, P.J.; Stieb, D.; Joseph, L.; Burnett, R.T. Biomass Burning as a Source of Ambient Fine Particulate Air Pollution and Acute Myocardial Infarction. Epidemiology 2017, 28, 329–337. [Google Scholar] [CrossRef] [Green Version]
- Gan, W.Q.; Koehoorn, M.; Davies, H.W.; Demers, P.A.; Tamburic, L.; Brauer, M. Long-Term Exposure to Traffic-Related Air Pollution and the Risk of Coronary Heart Disease Hospitalization and Mortality. Environ. Health Perspect. 2011, 119, 501–507. [Google Scholar] [CrossRef]
- Shin, S.; Burnett, R.T.; Kwong, J.C.; Hystad, P.; Van Donkelaar, A.; Brook, J.R.; Goldberg, M.S.; Tu, K.; Copes, R.; Martin, R.V.; et al. Ambient Air Pollution and the Risk of Atrial Fibrillation and Stroke: A Population-Based Cohort Study. Environ. Health Perspect. 2019, 127, 087009. [Google Scholar] [CrossRef]
- Bai, L.; Shin, S.; Burnett, R.T.; Kwong, J.C.; Hystad, P.; Van Donkelaar, A.; Goldberg, M.S.; Lavigne, E.; Copes, R.; Martin, R.V.; et al. Exposure to ambient air pollution and the incidence of congestive heart failure and acute myocardial infarction: A population-based study of 5.1 million Canadian adults living in Ontario. Environ. Int. 2019, 132, 105004. [Google Scholar] [CrossRef]
- Shin, H.H.; Burr, W.S.; Stieb, D.; Haque, L.; Kalayci, H.; Jovic, B.; Smith-Doiron, M. Air health trend indicator: Association between short-term exposure to ground ozone and circulatory hospitalizations in Canada for 17 years, 1996–2012. Int. J. Environ. Res. Public Health. 2018, 15, 9–11. [Google Scholar] [CrossRef] [Green Version]
- Shin, H.H.; Parajuli, R.P.; Maquiling, A.; Smith-Doiron, M. Temporal trends in associations between ozone and circulatory mortality in age and sex in Canada during 1984–2012. Sci. Total Environ. 2020, 724, 137944. [Google Scholar] [CrossRef]
- Stieb, D.M.; Shutt, R.; Kauri, L.; Mason, S.; Chen, L.; Szyszkowicz, M.; Dobbin, N.A.; Rigden, M.; Jovic, B.; Mulholland, M.; et al. Cardio-Respiratory Effects of Air Pollution in a Panel Study of Outdoor Physical Activity and Health in Rural Older Adults. J. Occup. Environ. Med. 2017, 59, 356–364. [Google Scholar] [CrossRef] [Green Version]
- Stieb, D.M.; Shutt, R.; Kauri, L.; Roth, G.; Szyszkowicz, M.; Dobbin, N.A.; Chen, L.; Rigden, M.; Van Ryswyk, K.; Kulka, R.; et al. Cardiorespiratory Effects of Air Pollution in a Panel Study of Winter Outdoor Physical Activity in Older Adults. J. Occup. Environ. Med. 2018, 60, 673–682. [Google Scholar] [CrossRef] [PubMed]
- Stieb, D.M.; Shutt, R.H.; Kauri, L.M.; Mason-Renton, S.; Chen, L.; Szyszkowicz, M.; Dobbin, N.A.; Rigden, M.; Jovic, B.; Mulholland, M.; et al. Associations between air pollution and cardio-respiratory physiological measures in older adults exercising outdoors. Int. J. Environ. Health Res. 2019, 2019, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bai, L.; Chen, H.; Hatzopoulou, M.; Jerrett, M.; Kwong, J.C.; Burnett, R.T.; Van Donkelaar, A.; Copes, R.; Martin, R.V.; Van Ryswyk, K.; et al. Exposure to Ambient Ultrafine Particles and Nitrogen Dioxide and Incident Hypertension and Diabetes. Epidemiology 2018, 29, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.B.; Brauer, M.; Macnab, Y.C.; Kennedy, S.M. Three Measures of Forest Fire Smoke Exposure and Their Associations with Respiratory and Cardiovascular Health Outcomes in a Population-Based Cohort. Environ. Health Perspect. 2011, 119, 1266–1271. [Google Scholar] [CrossRef]
- Crouse, D.L.; Peters, P.A.; Villeneuve, P.; Proux, M.-O.; Shin, H.H.; Goldberg, M.S.; Johnson, M.; Wheeler, A.; Allen, R.W.; Atari, D.O.; et al. Within- and between-city contrasts in nitrogen dioxide and mortality in 10 Canadian cities; a subset of the Canadian Census Health and Environment Cohort (CanCHEC). J. Expo. Sci. Environ. Epidemiol. 2015, 25, 482–489. [Google Scholar] [CrossRef] [Green Version]
- Farhat, N.; Ramsay, T.; Jerrett, M.; Krewski, D. Short-Term Effects of Ozone and PM2.5 on Mortality in 12 Canadian Cities. J. Environ. Prot. 2013, 04, 18–32. [Google Scholar] [CrossRef]
- Goldberg, M.S.; Burnett, R.T.; Stieb, D.M.; Brophy, J.; Daskalopoulou, S.S.; Valois, M.-F.; Brook, J.R. Associations between ambient air pollution and daily mortality among elderly persons in Montreal, Quebec. Sci. Total Environ. 2013, 463-464, 931–942. [Google Scholar] [CrossRef]
- Vanos, J.K.; Cakmak, S.; Bristow, C.; Brion, V.; Tremblay, N.; Martin, S.L.; Sheridan, S.S. Synoptic weather typing applied to air pollution mortality among the elderly in 10 Canadian cities. Environ. Res. 2013, 126, 66–75. [Google Scholar] [CrossRef] [Green Version]
- De Roos, A.J.; Koehoorn, M.; Tamburic, L.; Davies, H.W.; Brauer, M. Proximity to Traffic, Ambient Air Pollution, and Community Noise in Relation to Incident Rheumatoid Arthritis. Environ. Health Perspect. 2014, 122, 1075–1080. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.; Kwong, J.C.; Copes, R.; Hystad, P.; van Donkelaar, A.; Tu, K.; Brook, J.R.; Goldberg, M.S.; Martin, R.V.; Murray, B.; et al. Exposure to ambient air pollution and the incidence of dementia: A population-based cohort study. Environ. Int. 2017, 108, 271–277. [Google Scholar] [CrossRef]
- Chen, H.; Kwong, J.C.; Copes, R.; Tu, K.; Villeneuve, P.; van Donkelaar, A.; Hystad, P.; Martin, R.V.; Murray, B.; Jessiman, B.; et al. Living near major roads and the incidence of dementia, Parkinson’s disease, and multiple sclerosis: A population-based cohort study. Lancet 2017, 389, 718–726. [Google Scholar] [CrossRef]
- Shin, S.; Burnett, R.T.; Kwong, J.C.; Hystad, P.; Van Donkelaar, A.; Brook, J.R.; Copes, R.; Tu, K.; Goldberg, M.S.; Villeneuve, P.; et al. Effects of ambient air pollution on incident Parkinson’s disease in Ontario, 2001 to 2013: A population-based cohort study. Int. J. Epidemiology 2018, 47, 2038–2048. [Google Scholar] [CrossRef]
- Neupane, B.; Jerrett, M.; Burnett, R.T.; Marrie, T.; Arain, M.A.; Loeb, M. Long-Term Exposure to Ambient Air Pollution and Risk of Hospitalization with Community-acquired Pneumonia in Older Adults. Am. J. Respir. Crit. Care Med. 2010, 181, 47–53. [Google Scholar] [CrossRef]
- Szyszkowicz, M.; Kousha, T. Emergency department visits for asthma in relation to the Air Quality Health Index: A case-crossover study in Windsor, Canada. Can. J. Public Health 2014, 105, e336–e341. [Google Scholar] [CrossRef] [Green Version]
- Lavigne, E.; Villeneuve, P.; Cakmak, S. Air Pollution and Emergency Department Visits for Asthma in Windsor, Canada. Can. J. Public Health 2012, 103, 4–8. [Google Scholar] [CrossRef]
- Gan, W.Q.; Fitzgerald, J.M.; Carlsten, C.; Sadatsafavi, M.; Brauer, M. Associations of Ambient Air Pollution with Chronic Obstructive Pulmonary Disease Hospitalization and Mortality. Am. J. Respir. Crit. Care Med. 2013, 187, 721–727. [Google Scholar] [CrossRef]
- To, T.; Shen, S.; Atenafu, E.; Guan, J.; McLimont, S.; Stocks, B.; Licskai, C. The Air Quality Health Index and Asthma Morbidity: A Population-Based Study. Environ. Health Perspect. 2013, 121, 46–52. [Google Scholar] [CrossRef]
- Ward, C.J. It’s an ill wind: The effect of fine particulate air pollution on respiratory hospitalizations. Can. J. Econ. 2015, 48, 1694–1732. [Google Scholar] [CrossRef]
- Cohen, G.; Gerber, Y. Air Pollution and Successful Aging: Recent Evidence and New Perspectives. Curr. Environ. Health Rep. 2017, 4, 1–11. [Google Scholar] [CrossRef]
- Arbuthnott, K.G.; Hajat, S. The health effects of hotter summers and heat waves in the population of the United Kingdom: A review of the evidence. Environ. Health 2017, 16, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Hajat, S. Health effects of milder winters: A review of evidence from the United Kingdom. Environ. Health 2017, 16, 109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gamble, J.L.; Hurley, B.J.; Schultz, P.A.; Jaglom, W.S.; Krishnan, N.; Harris, M. Climate Change and Older Americans: State of the Science. Environ. Health Perspect. 2013, 121, 15–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guruge, S.; Birpreet, B.; Samuels-Dennis, J.A. Health Status and Health Determinants of Older Immigrant Women in Canada: A Scoping Review. J. Aging Res. 2015, 2015, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Block, S.; Galabuzi, G.-E.; Tranjan, R. Canada’s Colour Coded Income Inequality; Canadian Centre for Policy Alternatives: Ottawa, ON, Canada, 2019; pp. 1–26. [Google Scholar]
- Dusyk, N.; Turcotte, I.; Gunton, T.; Macnab, J.; Mcbain, S.; Penney, N.; Pickrell-Barr, J.; Pope, M. All Hands on Deck: An Assessment of Provincial, Terri-Torial and Federal Readiness to Deliver a Safe Climate; Pembina Institute: Calgary, AB, Canada, 2021; p. 63. [Google Scholar]
- Heaviside, C.; Macintyre, H.; Vardoulakis, S. The Urban Heat Island: Implications for Health in a Changing Environment. Curr. Environ. Health Rep. 2017, 4, 296–305. [Google Scholar] [CrossRef]
| Authors | Population (n, age) | Primary Exposure Variables | Health Impact Category | Main Findings |
|---|---|---|---|---|
| Meteorological | ||||
| Vanasse 2017 [29] | 112,793 participants; ≥65 years | Mean temperature | Cardiovascular | Decreasing temperature associated with increased risk in ≥65 years. |
| Bai 2018a [30] | ~13 million participants; <65 years vs. ≥65 years | Mean, maximum, and extreme temperatures | Cardiovascular | Hot days associated with increased risk in ≥65 years. |
| Vida 2012 [31] | 347,552 events; <65 years, ≥65 years | Mean temperature, diurnal temperature change | Mental health | Higher temperatures associated with increased risk in ≥65 years in an urban region. |
| Wang 2014 [32] | 271,746 events; 0–14 years, 15–39 years, 50–59 years, ≥60 years | Minimum, maximum, mean temperature | Mental health | High temperatures associated with increased risk in ≥60 years. |
| Benmarhnia 2017 [33] | n NR <65 years vs. ≥65 years | Mean temperature | Mortality | Higher temperature associated with increased in ≥65 years. |
| Henderson 2013 [34] | ~4.6 million participants; <75 years vs. ≥75 years | Apparent maximum temperature (°C) | Mortality | Higher temperature associated with increased mortality in ≥75 years living in the coastal region. |
| Vutcovici 2014 [35] | Mean 30.1 (6.9 SD) deaths/day for 8766 days; ≥65 years | Diurnal temperature change | Mortality | Increased diurnal temperature change associated with mortality. |
| Kosatsky 2012 [36] | 398 participants; <65 years, 65–75 years, 75–85 years, ≥85 | Heatwave | Mortality; cardiovascular; respiratory | Heatwaves associated with increased risk in 65–74 years. |
| Chen 2016 [37] | 352,818 participants; <65 years vs. ≥65 years | Mean temperature | Mortality; cardiovascular; respiratory; diabetes | Cold temperatures associated with increased cardiovascular mortality in ≥65 years. |
| Bustinza 2013 [38] | ~6 million people; <65 years, 65–74 years, ≥75 years | Heatwave | Mortality; overall morbidity | Signficant increase in crude death rates for ≥75 years. |
| Burton 2015 [39] | NR | Flooding | Mortality; respiratory; mental health | Older adults at risk of adverse health events due to flooding. |
| Mondor 2015 [40] | 136,323 participants; ≥65 years | Freezing rain, snowstorms | Fall-related injuries | Freezing rain associated with increased risk in ≥65 years. |
| Modarres 2012 [41] | 1,077,813 participants; 40–74 years, ≥75 years | Minimum, maximum, mean temperature, precipitation, snow depth, daylight hours, air pressure | Fall-related injuries | Decreasing temperature, rainfall, daylight hours, and increased snow associated with increased risk in ≥75 years. |
| Modarres 2014 [42] | ~900,000 participants; 40–74 years, ≥75 years | Minimum, maximum, mean temperature, precipitation, snow depth, daylight hours, air pressure | Fall-related injuries | Maximum pressure and daylight hours associated with increased risk older adults. Rainfall depth was a predictor for older males. |
| Auger 2017 [43] | 14,302 participants; <55 years, 55–64 years, 65–74 years, ≥75 years | Mean temperature | Ocular | Increased temperature associated with increased risk in 65–74 years. |
| Laverdière 2016 [44] | 1233 participants; 68–72 years, 73–77 years, 78–82 years | Daily maximum temperature ≥ 30 °C | Overall morbidity | Hot days associated with increased risk. |
| Bélanger 2014 * [45] | 3485 participants; 18–35 years, 35–44 years, 45–54 years, 55–64 years, ≥65 years | Hot and humid days | Overall morbidity | Increased prevalence in low income ≥ 65 years, decreased prevalence in foreign born residents. |
| Stapleton 2014 [46] | 24 participants; 12 younger participants, mean 21 years (3 SD); 12 older participants, mean 65 years (5 SD) | Hot-dry and hot-humid conditions | Overall morbidity | Hot conditions associated with a significant increase in body heat content in older adults compared to younger. |
| Tajmir 2013 [47] | 18 participants 10 younger; mean 26 (2.4 SD) years; 8 older; mean 68 (4.4 SD) years | Temperature categories; 23 °C vs. 1 °C | Overall morbidity | Cold conditions associated with greater impairment of manual movements in and reduced sensitivity. |
| McTavish 2018 [48] | 227,135 participants Median 80 (74–85 IQR) years | Maximum temperature | Renal | High heat marginally associated with greater risk of acute kidney injury. |
| Ordon 2015 [49] | 423,396 participants; 18–39 years, 40–49 years, 50–59 years, 60–69 years, >70 years | Minimum, maximum, mean temperature, extreme temperatures | Renal | Extreme heat associated with increased risk in 60–69 years. |
| Meteorological and Air pollution | ||||
| Krstic 2011 [50] | ≥65 years | Steadman’s apparent temperature, PM2.5 | Mortality; cardiovascular; respiratory | High and low temperatures associated with increased risk. |
| Air pollution | ||||
| Parent 2013 * [51] | 1772 participants; <60 years, 60–66 years, 67–71 years, >71 years | NO2 | Cancer | Increased risk in third quartile distribution of recent immigrants. |
| Goldberg 2018 [52] | 788 participants; 50–70 years | UFP | Cancer | Positive but insignificant associations. |
| Goldberg 2017 [53] | 1277 participants; Cases mean 62.23 years (SD NR), controls 61.03 years (SD NR) | NO2, UFP | Cancer | Positive but insignificant associations. |
| Chen 2014 [54] | 5229 participants; 25–44 years, 45–64 years, 65–74 years, 75–84 years, ≥85 years | AQHI, CO, NO2, O3, PM2.5, PM10, SO2 | Cardiovascular | AQHI, CO, and NO2 associated with increased risk in ≥75 years. |
| Wang 2015 [55] | 25,894 participants; <65 years vs. ≥65 years | CO, NO2, NO, O3, PM2.5 | Cardiovascular | Observed positive associations with NO2 and NO and negative associations with CO in ≥65 years. |
| Weichenthal 2017 [56] | 2881 events; <65 years vs. ≥65 years | PM2.5, NO2, O3 | Cardiovascular | PM2.5 associated with increased risk in ≥65 years. |
| Gan 2011 [57] | 452,735 participants; <60 years, 60–69 years, ≥70 years | BC, NO, NO2, PM2.5 | Cardiovascular | BC associated with increased risk of mortality in ≥60 years and hospitalizations in 60–69 years. |
| Shin 2019 [58] | 5,071,956 participants; 35–44 years, 45–54 years, 55–64 years, 65–74 years, 75–85 years | NO2, O3, Ox, PM2.5 | Cardiovascular | All pollutants were associated with increased risk of cardiovascular outcomes. |
| Bai 2019 [59] | 50,062,146 and 5,141,172 participants; 35–44 years, 45–54 years, 55–64 years, 65–74 years, 75–85 years; | PM2.5, NO2, O3, Ox | Cardiovascular | All pollutants associated with increased risk in ≥65 years. |
| Shin 2018a [60] | 2,194,519 participants; <50 years, ≥50 years, ≥65 years | O3 | Cardiovascular | No significant associations ≥ 50 years. |
| Shin 2020 [61] | ~19 million participants; 1–65 years vs. >65 years | O3 | Cardiovascular | O3 associated with increased risk in ≥65 years. |
| Stieb 2017 [62] | 2013: 36 participants, 2014: 41 participants; 55–59 years, 60–64 years, 65–69 years, ≥70 years | AQHI, CO, NO2, O3, PM2.5, SO2 | Cardiovascular | AQHI, PM2.5, and O3 associated with subclinical adverse cardio-respiratory effects. |
| Stieb 2018 [63] | 2014: 36 participants, 2015: 34 participants; 55–59 years, 60–64 years, 65–69 years, ≥70 years | AQHI, CO, NO2, O3, Ox, PM2.5, SO2 | Cardiovascular | AQHI, PM2.5, O3 and Ox associated with subclinical cardio-respiratory effects. |
| Stieb 2019 [64] | 72 participants; 55–81 years | AQHI, CO, NO2, O3, PM2.5 | Cardiovascular | AQHI and PM2.5 associated with subclinical cardio-respiratory effects and markers of oxidative stress. |
| Bai 2018b [65] | Hypertension: 893,499 participants; Mean 48.6 (SD 14.3) years; Diabetes: 1,056,012 participants; Mean 51.1 (15.3 SD) years | UFP, NO2 | Cardiovascular; diabetes | UFP and NO2 associated with diabetes and hypertension; NO2 negatively associated with hypertension in 60–74 years. |
| Henderson 2011 [66] | 281,711 participants; 0–5 years, 5–10 years, 10–20 years, 20–30 years, 30–40 years, 40–50 years, 50–60 years, 60–70 years, 70–80 years, ≥80 years | PM10 | Cardiovascular; respiratory | PM10 was associated with increased risk in 60–70 years and ≥80 years. |
| Crouse 2015 [67] | 735,590 participants; 25–34 years, 35–44 years, 45–54 years, 55–64 years, 65–74 years, ≥75 years | NO2 | Cardiovascular; respiratory; diabetes; mortality | NO2 associated with increased risk in 60–79 years. |
| Farhat 2013 [68] | ~9.1 million participants; <75 years vs. ≥75 years | O3, PM2.5 | Cardiovascular; respiratory; mortality | O3 and PM2.5 were associated with increased risk in those ≥75 years. |
| Goldberg 2013 [69] | 158,350 participants; ≥65 years | CO, NO2, O3, PM2.5, SO2 | Mortality; cancer; cardiovascular; respiratory; diabetes | All pollutants associated with increased risk. |
| Vanos 2013 [70] | n NR <65 years, 65–74 years, 75–84 years, ≥85 years | CO, NO2, O3, SO2 | Mortality | All pollutants associated with increased risk in ≥85 years. |
| de Roos 2014 [71] | 678,361 participants; <65 years vs. ≥65 years | Proximity to roads, BC, CO, NO, NO2, O3, PM2.5, PM10 | Musculo-skeletal | O3 associated with increased risk in ≥65 years. |
| Chen 2017a [72] | 2,066,639 participants; 55–64 years, 65–74 years, 75–85 years | NO2, O3, PM2.5 | Neurological | PM2.5 and NO2 associated with increased risk of dementia in those 55–85 years. |
| Chen 2017b [73] | 2,165,269 participants; Mean 66.8 (8.2 SD) years | NO2, Proximity to roads, PM2.5 | Neurological | Closer proximity to roads, PM2.5 and NO2 associated with increased risk of dementia, PM2.5 associated with increased risk of Parkinson’s. |
| Shin 2018b [74] | 2,194,519 participants; 55–85 years | NO2, O3, PM2.5 | Neurological | PM2.5 and O3 associated with increased risk. |
| Neupane 2010 [75] | 859 participants; ≥65 years | NO2, PM2.5, SO2 | Respiratory | NO2 and PM2.5 were associated with increased risk. |
| Szyszkowicz 2014 [76] | 6697 participants; 2–14 years, 15–39 years, 40–59 years, ≥60 years | AQHI, NO2, O3, PM2.5 | Respiratory | No significant associations in ≥60 years observed. |
| Lavigne 2012 [77] | 3728 participants; 2–14 years, 15–39 years, 40–59 years, ≥60 years | NO2, CO, PM2.5, SO2 | Respiratory | O3 associated with increased risk during cold season in ≥60 years. |
| Gan 2013 [78] | 467,994 participants; Mean 60 (11 SD) years | BC, NO, NO2, PM2.5 | Respiratory | BC associated with increased risk in ≥65 years. |
| To 2013 [79] | ~1.5 million participants; 0–4 years, 5–9 years, 10–19 years, 20–59 years, ≥60 years | AQHI, NO2, O3, PM2.5 | Respiratory | AQHI was associated with asthma in ≥60 years. |
| Ward 2015 [80] | 107,108 participants; 0–19 years, 20–64 years, ≥65 years | AQI, CO, O3, PM2.5 | Respiratory | No significant associations observed in ≥65 years. |
| Outcome Category | Climate-Related Exposures |
|---|---|
| Mortality | ↑ Temperature Diurnal temperature variation Heatwave Flooding |
| Overall morbidity | ↑ Temperature Heat waves |
| Cardiovascular | ↑ Temperature Extreme heat Extreme cold Heatwave |
| Respiratory | ↑ Temperature Heatwave Flooding |
| Fall-related injuries | ↓ Temperature Precipitation Snow depth Daylight hours Air pressure |
| Mental health | ↑ Temperature ↑Humidity Heatwave Flooding |
| Renal | ↑ Temperature Heatwave |
| Ocular health | ↑ Temperature Heatwave |
| Diabetes | Extreme heat (null) Extreme cold (null) |
| Outcome Category | Air Pollution Exposures |
|---|---|
| Cardiovascular | AQHI, AQI, BC, CO, NO, NO2, O3, Ox, PM2.5, PM10, SO2, UFP |
| Respiratory | AQHI, BC, CO, NO, NO2, O3, PM2.5, PM10, SO2, UFP |
| Cancer | CO, NO2, O3, PM2.5, SO2, UFP |
| Neurological | NO2, O3, PM2.5 |
| Diabetes | CO, NO2, O3, PM2.5, SO2 |
| Mortality | CO, NO2, O3, PM10, SO2 |
| Musculoskeletal outcomes | Proximity to roads, BC, CO, NO, NO2, O3, PM2.5, PM10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tilstra, M.H.; Tiwari, I.; Niwa, L.; Campbell, S.; Nielsen, C.C.; Jones, C.A.; Osornio Vargas, A.; Bulut, O.; Quemerais, B.; Salma, J.; et al. Risk and Resilience: How Is the Health of Older Adults and Immigrant People Living in Canada Impacted by Climate- and Air Pollution-Related Exposures? Int. J. Environ. Res. Public Health 2021, 18, 10575. https://doi.org/10.3390/ijerph182010575
Tilstra MH, Tiwari I, Niwa L, Campbell S, Nielsen CC, Jones CA, Osornio Vargas A, Bulut O, Quemerais B, Salma J, et al. Risk and Resilience: How Is the Health of Older Adults and Immigrant People Living in Canada Impacted by Climate- and Air Pollution-Related Exposures? International Journal of Environmental Research and Public Health. 2021; 18(20):10575. https://doi.org/10.3390/ijerph182010575
Chicago/Turabian StyleTilstra, McKenzie H., Ishwar Tiwari, Leigh Niwa, Sandra Campbell, Charlene C. Nielsen, C. Allyson Jones, Alvaro Osornio Vargas, Okan Bulut, Bernadette Quemerais, Jordana Salma, and et al. 2021. "Risk and Resilience: How Is the Health of Older Adults and Immigrant People Living in Canada Impacted by Climate- and Air Pollution-Related Exposures?" International Journal of Environmental Research and Public Health 18, no. 20: 10575. https://doi.org/10.3390/ijerph182010575
APA StyleTilstra, M. H., Tiwari, I., Niwa, L., Campbell, S., Nielsen, C. C., Jones, C. A., Osornio Vargas, A., Bulut, O., Quemerais, B., Salma, J., Whitfield, K., & Yamamoto, S. S. (2021). Risk and Resilience: How Is the Health of Older Adults and Immigrant People Living in Canada Impacted by Climate- and Air Pollution-Related Exposures? International Journal of Environmental Research and Public Health, 18(20), 10575. https://doi.org/10.3390/ijerph182010575








