Teaching and Practicing Cognitive-Behavioral and Mindfulness Skills in a Web-Based Platform among Older Adults through the COVID-19 Pandemic: A Pilot Randomized Controlled Trial
Abstract
:1. Introduction
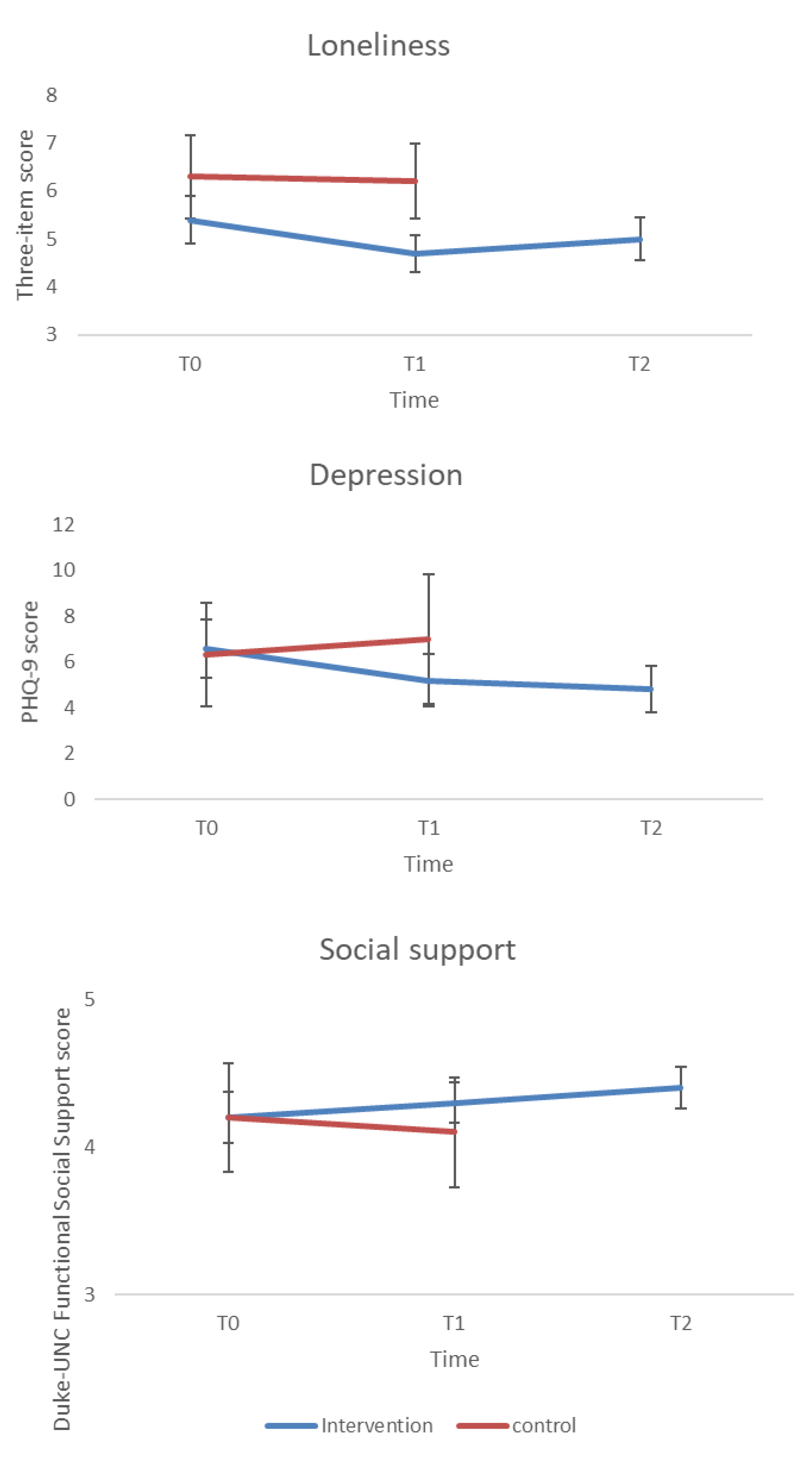
- Compared with the control group, participants in the intervention group report decreased depressive symptoms immediately and one month following the intervention.
- Participants in the intervention group report decreased loneliness immediately and one month following the intervention.
- Participants in the intervention group report increased social support immediately and one month following the intervention.
2. Materials and Methods
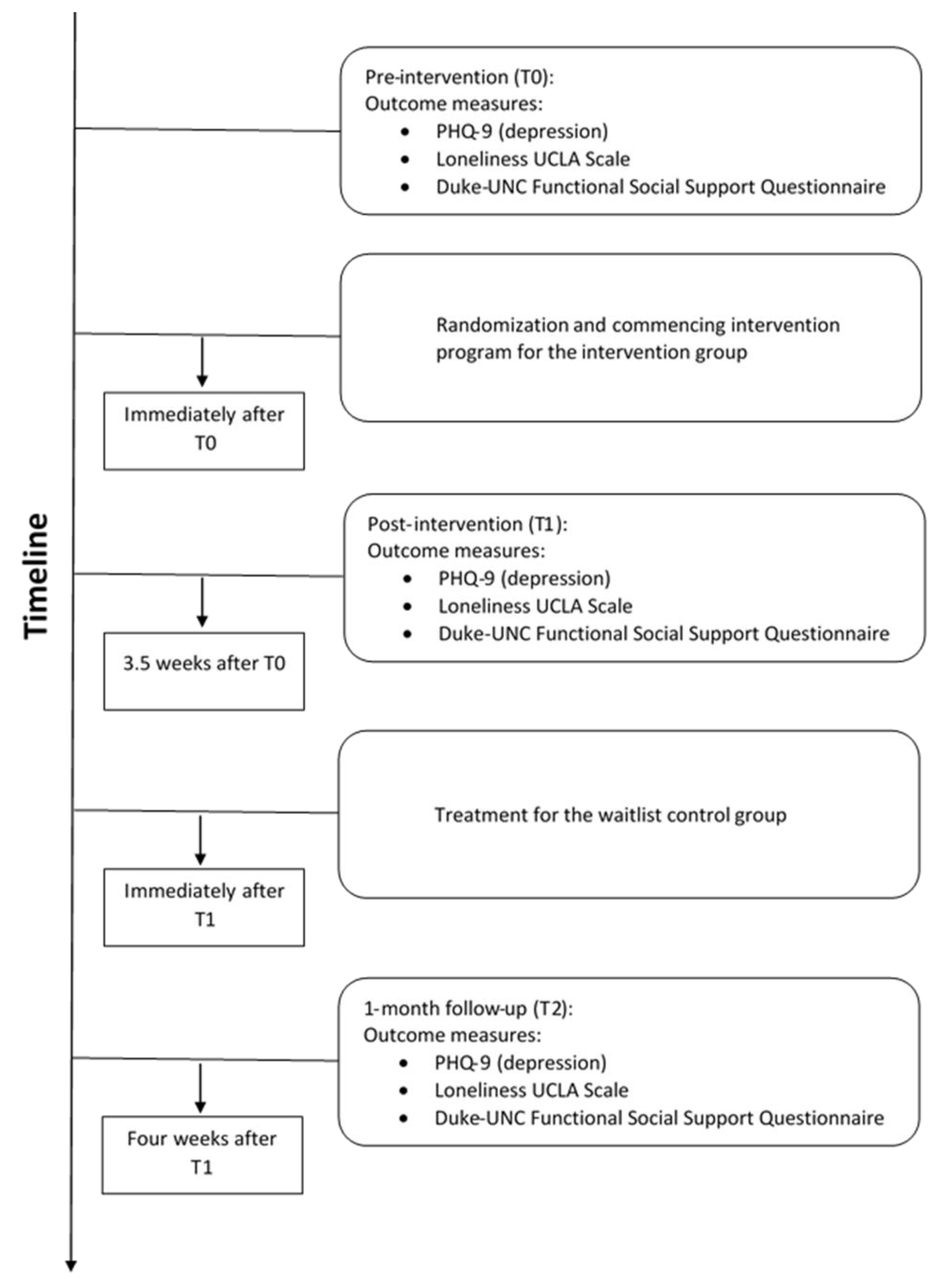
2.1. Procedure
2.2. Group Allocation
2.3. Intervention
Wait-List Control Group
2.4. Outcome Measures
2.4.1. Depression
2.4.2. Loneliness
2.4.3. Social Support
2.5. Sample Size Calculation
2.6. Statistical Analyses
2.7. Clinically Meaningful Improvement
3. Results
3.1. Recruitment and Attrition
3.2. Baseline Characteristics
3.3. Changes in Depressive Symptoms
3.4. Clinically Significant Changes in Depressive Symptoms
3.5. Changes in Loneliness
3.6. Changes in Social Support
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mækelæ†, M.J.; Reggev†, N.; Dutra, N.; Tamayo, R.M.; Silva-Sobrinho, R.A.; Klevjer, K.; Pfuhl, G. Perceived efficacy of COVID-19 restrictions, reactions and their impact on mental health during the early phase of the outbreak in six countries. R. Soc. Open Sci. 2020, 7, 200644. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.E.; Duff, H.; Kelly, S.; Power, J.E.M.; Brennan, S.; Lawlor, B.A.; Loughrey, D.G. The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: A systematic review. Syst. Rev. 2017, 6, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Holt-Lunstad, J. Why Social Relationships Are Important for Physical Health: A Systems Approach to Understanding and Modifying Risk and Protection. Annu. Rev. Psychol. 2018, 69, 437–458. [Google Scholar] [CrossRef]
- Parra-Rizo, M.; Sanchís-Soler, G. Physical Activity and the Improvement of Autonomy, Functional Ability, Subjective Health, and Social Relationships in Women over the Age of 60. Int. J. Environ. Res. Public Health 2021, 18, 6926. [Google Scholar] [CrossRef]
- Cohn-Schwartz, E.; Vitman-Schorr, A.; Khalaila., R. Physical distancing is related to fewer electronic and in-person contacts and to increased loneliness during the COVID-19 pandemic among older Europeans. Qual. Life Res. 2021, 1–10. [Google Scholar] [CrossRef]
- Armitage, R.; Nellums, L.B. COVID-19 and the consequences of isolating the elderly. Lancet Public Health 2020, 5, e256. [Google Scholar] [CrossRef] [Green Version]
- Seifert, A.; Hassler, B. Impact of the COVID-19 pandemic on loneliness among older adults in Austria. Front. Sociol. 2020, 5, 1–15. [Google Scholar] [CrossRef]
- McGinty, E.E.; Presskreischer, R.; Han, H.; Barry, C.L. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA 2020, 324, 93. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-2019) Situation Report—51; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Mansfield, J.; Muff, A.; Meschiany, G.; Lev-Ari, S.; Aviv Israel, T. Adequacy of Web-Based Activities as a Substitute for In-Person Activities for Older Persons during the COVID-19 Pandemic: Survey Study. Available online: https://www.jmir.org/2021/2/e27687/ (accessed on 12 September 2021).
- Zubatsky, M.; Berg-Weger, M.; Morley, J. Using Telehealth Groups to Combat Loneliness in Older Adults through COVID-19. J. Am. Geriatr. Soc. 2020, 68, 1678–1679. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Chau, A.K.C.; Wong, A.; Fung, H.H.; Woo, J. Information and communicative technology use enhances psycho-logical well-being of older adults: The roles of age, social connectedness, and frailty status. Aging Ment. Health 2018, 22, 1516–1524. [Google Scholar] [CrossRef] [PubMed]
- Shapira, N.; Barak, A.; Gal, I. Promoting older adults’ well-being through Internet training and use. Aging Ment. Health 2007, 11, 477–484. [Google Scholar] [CrossRef]
- Yeshua-Katz, D.; Shapira, S.; Aharonson-Daniel, L.; Clarfield, A.M.; Sarid, O. Matching Digital Intervention Affordances with Tasks: The Case of a Zoom and WhatsApp Mental Health Intervention for Seniors during the COVID-19 Pandemic. Health Commun. 2021, 1–13. [Google Scholar] [CrossRef]
- Fokkema, T.; Knipscheer, K. Escape loneliness by going digital: A quantitative and qualitative evaluation of a Dutch experiment in using ECT to overcome loneliness among older adults. Aging Ment. Health 2007, 11, 496–504. [Google Scholar] [CrossRef] [Green Version]
- Silva, P.; Matos, A.D.; Martinez-Pecino, R. Can the internet reduce the loneliness of 50+ living alone? Inf. Commun. Soc. 2020, 1–17. [Google Scholar] [CrossRef]
- Mahlo, L.; Windsor, T. Feasibility, Acceptability, and Preliminary Efficacy of an App-Based Mindfulness-Meditation Program Among Older Adults|The Gerontologist|Oxford Academic. Gerontologist 2020, 61, 775–786. [Google Scholar] [CrossRef]
- Segal-Engelchin, D.; Huss, E.; Sarid, O. The Use of Online CB-ART Interventions in the Context of COVID-19: Enhanc-ing Salutogenic Coping. Int. J. Environ. Res. Public Health 2021, 18, 2057. [Google Scholar] [CrossRef]
- Mewton, L.; Sachdev, P.S.; Andrews, G. A Naturalistic Study of the Acceptability and Effectiveness of Internet-Delivered Cognitive Behavioural Therapy for Psychiatric Disorders in Older Australians. PLoS ONE 2013, 8, e71825. [Google Scholar] [CrossRef] [Green Version]
- Titov, N.; Fogliati, V.J.; Staples, L.G.; Gandy, M.; Johnston, L.; Wootton, B.; Nielssen, O.; Dear, B.F. Treating anxiety and depression in older adults: Randomised controlled trial comparing guided V. self-guided internet-delivered cognitive–behavioural therapy. BJPsych Open 2016, 2, 50–58. [Google Scholar] [CrossRef] [Green Version]
- Tomasino, K.N.; Lattie, E.G.; Ho, J.; Palac, H.L.; Kaiser, S.M.; Mohr, D.C. Harnessing Peer Support in an Online Intervention for Older Adults with Depression. Am. J. Geriatr. Psychiatry 2017, 25, 1109–1119. [Google Scholar] [CrossRef]
- Shiovitz-Ezra, S.; Ayalon, L. Situational versus chronic loneliness as risk factors for all-cause mortality. Int. Psychogeriatr. 2009, 22, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Masi, C.M.; Chen, H.-Y.; Hawkley, L.C.; Cacioppo, J.T. A Meta-Analysis of Interventions to Reduce Loneliness. Pers. Soc. Psychol. Rev. 2010, 15, 219–266. [Google Scholar] [CrossRef] [Green Version]
- Dickens, A.P.; Richards, S.H.; Greaves, C.J.; Campbell, J.L. Interventions targeting social isolation in older people: A systematic review. BMC Public Health 2011, 11, 647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antonucci, T.C.; Ajrouch, K.J.; A Manalel, J. Social Relations and Technology: Continuity, Context, and Change. Innov. Aging 2017, 1, igx029. [Google Scholar] [CrossRef] [PubMed]
- Poscia, A.; Stojanovic, J.; La Milia, D.I.; Duplaga, M.; Grysztar, M.; Moscato, U.; Onder, G.; Collamati, A.; Ricciardi, W.; Magnavita, N. Interventions targeting loneliness and social isolation among the older people: An update systematic review. Exp. Gerontol. 2018, 102, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Khosravi, P.; Rezvani, A.; Wiewiora, A. The impact of technology on older adults’ social isolation. Comput. Hum. Behav. 2016, 63, 594–603. [Google Scholar] [CrossRef]
- Baker, S.; Warburton, J.; Waycott, J.; Batchelor, F.; Hoang, T.; Dow, B.; Ozanne, E.; Vetere, F. Combatting social isolation and increasing social participation of older adults through the use of technology: A systematic review of existing evidence. Australas. J. Ageing 2018, 37, 184–193. [Google Scholar] [CrossRef] [Green Version]
- Cheung, G.; Peri, K. Challenges to dementia care during COVID-19: Innovations in remote delivery of group Cognitive Stimulation Therapy. Aging Ment. Health 2021, 25, 977–979. [Google Scholar] [CrossRef]
- Dikaios, E.; Sekhon, H.; Allard, A.; Vacaflor, B.; Goodman, A.; Dwyer, E.; Lavin-Gonzalez, P.; Mahdanian, A.; Park, H.; Walsh, C.; et al. Connecting During COVID-19: A Protocol of a Volunteer-Based Telehealth Program for Supporting Older Adults’ Health. Front. Psychiatry 2020, 11, 598356. [Google Scholar] [CrossRef] [PubMed]
- Office, E.E.; Rodenstein, M.S.; Merchant, T.S.; Pendergrast, T.R.; Lindquist, L.A. Reducing Social Isolation of Seniors during COVID-19 through Medical Student Telephone Contact. J. Am. Med. Dir. Assoc. 2020, 21, 948–950. [Google Scholar] [CrossRef] [PubMed]
- Shapira, S.; Yeshua-Katz, D.; Cohn-Schwartz, E.; Aharonson-Daniel, L.; Sarid, O.; Clarfield, A.M. A pilot randomized con-trolled trial of a group intervention via Zoom to relieve loneliness and depressive symptoms among older persons during the COVID-19 outbreak. Internet Interv. 2021, 24, 100368. [Google Scholar] [CrossRef] [PubMed]
- Shapira, S.; Yeshua-Katz, D.; Goren, G.; Aharonson-Daniel, L.; Clarfield, A.M.; Sarid, O. Evaluation of a Short-Term Digital Group Intervention to Relieve Mental Distress and Promote Well-Being Among Community-Dwelling Older Individuals During the COVID-19 Outbreak: A Study Protocol. Front. Public Health 2021, 9, 577079. [Google Scholar] [CrossRef]
- Daitch, C. Cognitive Behavioral Therapy, Mindfulness, and Hypnosis as Treatment Methods for Generalized Anxiety Disorder. Am. J. Clin. Hypn. 2018, 61, 57–69. [Google Scholar] [CrossRef]
- Vanhuffel, H.; Rey, M.; Lambert, I.; Da Fonseca, D.; Bat-Pitault, F. Contribution of mindfulness meditation in cognitive behavioral therapy for insomnia. Encephale 2017, 44, 134–140. [Google Scholar] [CrossRef]
- Goren, G.; Schwartz, D.; Friger, M.; Banai, H.; Sergienko, R.; Regev, S.; Abu-Kaf, H.; Greenberg, D.; Nemirovsky, A.; Ilan, K.; et al. Randomized Controlled Trial of Cognitive-Behavioral and Mindfulness-Based Stress Reduction on the Quality of Life of Patients with Crohn Disease. Inflamm. Bowel. Dis. 2021, 1–16. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Neria, Y.; Besser, A.; Kiper, D.; Westphal, M. A longitudinal study of posttraumatic stress disorder, depression, and generalized anxiety disorder in Israeli civilians exposed to war trauma. J. Trauma. Stress 2010, 23, 322–330. [Google Scholar] [CrossRef]
- Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Cacioppo, J.T. A Short Scale for Measuring Loneliness in Large Surveys Results From Two Population-Based Studies. Res. Aging 2004, 26, 655–672. [Google Scholar] [CrossRef]
- Palgi, Y.; Shrira, A.; Ring, L.; Bodner, E.; Avidor, S.; Bergman, Y.; Cohen-Fridel, S.; Keisari, S.; Hoffman, Y. The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020, 275, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Broadhead, W.; Gehlbach, S.; de Gruy, F.; Kaplan, B. The Duke-UNC Functional Social Support Questionnaire: Measure-ment of Social Support in Family Medicine Patients on JSTOR. Med. Care 1988, 26, 709–723. [Google Scholar] [CrossRef]
- Machón, M.; Larrañaga, I.; Dorronsoro, M.; Vrotsou, K.; Vergara, I. Health-related quality of life and associated factors in functionally independent older people. BMC Geriatr. 2017, 17, 19. [Google Scholar] [CrossRef] [Green Version]
- Applebaum, A.J.; Stein, E.M.; Lord-Bessen, J.; Pessin, H.; Rosenfeld, B.; Breitbart, W. Optimism, social support, and mental health outcomes in patients with advanced cancer. Psycho-Oncol. 2014, 23, 299–306. [Google Scholar] [CrossRef] [Green Version]
- Käll, A.; Jägholm, S.; Hesser, H.; Andersson, F.; Mathaldi, A.; Norkvist, B.T.; Shafran, R.; Andersson, G. Internet-Based Cognitive Behavior Therapy for Loneliness: A Pilot Randomized Controlled Trial. Behav Ther. 2020, 51, 54–68. [Google Scholar] [CrossRef] [PubMed]
- Torous, J.; Lipschitz, J.; Ng, M.; Firth, J. Dropout rates in clinical trials of smartphone apps for depressive symptoms: A systematic review and meta-analysis. J. Affect. Disord. 2020, 263, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Unützer, J.; Callahan, C.M.; Perkins, A.J.; Kroenke, K. Monitoring Depression Treatment Outcomes With the Patient Health Questionnaire-9. Med Care 2004, 42, 1194–1201. [Google Scholar] [CrossRef]
- Müller, A.; Arikian, A.; De Zwaan, M.; Mitchell, J. Cognitive-behavioural group therapy versus guided self-help for compulsive buying disorder: A preliminary study. Clin. Psychol. Psychother. 2011, 20, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.R.R.; Schulz, P.J. The Effect of Information Communication Technology Interventions on Reducing Social Isolation in the Elderly: A Systematic Review. J. Med Internet Res. 2016, 18, e4596. [Google Scholar] [CrossRef]
- Pynnönen, K.; Törmäkangas, T.; Rantanen, T.; Tiikkainen, P.; Kallinen, M. Effect of a social intervention of choice vs. control on depressive symptoms, melancholy, feeling of loneliness, and perceived togetherness in older Finnish people: A randomized controlled trial. Aging Ment Health 2018, 22, 77–84. [Google Scholar] [CrossRef]
- Huxhold, O.; Hees, E.; Webster, N.J. Towards bridging the grey digital divide: Changes in internet access and its predictors from 2002 to 2014 in Germany. Eur. J. Ageing 2020, 17, 271–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pywell, J.; Vijaykumar, S.; Dodd, A.; Coventry, L. Barriers to older adults’ uptake of mobile-based mental health interventions. Digit Health 2020, 6, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Cohn-Schwartz, E.; Ayalon, L. COVID-19 Protective Behaviors: The Role of Living Arrangements and Localities. J. Appl. Gerontol. 2021, 40, 799–803. [Google Scholar] [CrossRef] [PubMed]
| Intervention Group (n = 64) | Wait-List Control Group (n = 18) | p Value | Range | |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Gender (female), n(%) | 52 (81%) | 14 (78%) | 0.74 | --- |
| Age (years), M(SD) | 72.1 (5.3) | 71.7 (6.8) | 0.79 | 65–90 |
| Living alone, n(%) | 24 (37.5%) | 6 (35%) | 0.86 | --- |
| Tertiary education, n(%) | 48 (76%) | 10 (59%) | 0.15 | --- |
| Study measures, M(SD) | ||||
| Loneliness | 5.4 (2) | 6.3 (1.9) | 0.21 | 3–9 |
| Depression (PHQ-9) | 6.6 (5.2) | 6.3 (4.9) | 0.85 | 007–27 |
| Social support | 4.2 (0.7) | 4.2 (0.8) | 0.95 | 1–5 |
| To | T1 | T2 | |
|---|---|---|---|
| Measure | M (SD) | M (SD) | M (SD) |
| Loneliness | |||
| Intervention | 5.4 (2.0) | 4.7 (1.6) | 5.0 (1.8) |
| Wait-list | 6.3 (1.9) | 6.2 (1.7) | NA |
| Depressive symptoms | |||
| Intervention | 6.6 (5.2) | 5.2 (4.7) | 4.8 (4.1) |
| Wait-list | 6.3 (4.9) | 7.0 (6.1) | NA |
| Social support | |||
| Intervention | 4.2 (0.7) | 4.3 (0.6) | 4.4 (0.6) |
| Wait-list | 4.2 (0.8) | 4.1 (0.8) | NA |
| Clinical | |||
| Depressed, n(%) | |||
| PHQ ≥ 12 * | |||
| Intervention | 15 (23) | 7 (11) | 6 (9) |
| Wait-list | 2 (11) | 5 (27) | NA |
| Measure | T0 and T1 | Difference, M(SE) | T1 and T2 | Difference, M(SE) | T0 and T2 | Difference, M(SE) |
|---|---|---|---|---|---|---|
| Loneliness | ||||||
| Intervention | t(63) = 2.15 * | −0.7 (0.28) | t(63) = −0.88 | 0.3 (0.26) | t(63) = 1.5 | −0.4 (0.24) |
| Wait-list | t(17) = 0.34 | −0.1 (0.32) | NA | NA | NA | NA |
| Depressive symptoms | ||||||
| Intervention | t(63) = 2.57 * | −1.4 (0.48) | t(63) = 1.15 | −0.4 (0.38) | t(63) = 3.3 * | −1.8 (0.53) |
| Wait-list | t(17) = −0.72 | 0.7 (1) | NA | NA | NA | NA |
| Social support | ||||||
| Intervention | t(63) = −1.03 | 0.1 (0.06) | t(63) = −0.39 | 0.1 (0.06) | t(63) = −1.31 | 0.2 (0.07) |
| Wait-list | t(17) = 1.08 | −0.1 (0.16) | NA | NA | NA | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shapira, S.; Cohn-Schwartz, E.; Yeshua-Katz, D.; Aharonson-Daniel, L.; Clarfield, A.M.; Sarid, O. Teaching and Practicing Cognitive-Behavioral and Mindfulness Skills in a Web-Based Platform among Older Adults through the COVID-19 Pandemic: A Pilot Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 10563. https://doi.org/10.3390/ijerph182010563
Shapira S, Cohn-Schwartz E, Yeshua-Katz D, Aharonson-Daniel L, Clarfield AM, Sarid O. Teaching and Practicing Cognitive-Behavioral and Mindfulness Skills in a Web-Based Platform among Older Adults through the COVID-19 Pandemic: A Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(20):10563. https://doi.org/10.3390/ijerph182010563
Chicago/Turabian StyleShapira, Stav, Ella Cohn-Schwartz, Daphna Yeshua-Katz, Limor Aharonson-Daniel, Avram Mark Clarfield, and Orly Sarid. 2021. "Teaching and Practicing Cognitive-Behavioral and Mindfulness Skills in a Web-Based Platform among Older Adults through the COVID-19 Pandemic: A Pilot Randomized Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 20: 10563. https://doi.org/10.3390/ijerph182010563
APA StyleShapira, S., Cohn-Schwartz, E., Yeshua-Katz, D., Aharonson-Daniel, L., Clarfield, A. M., & Sarid, O. (2021). Teaching and Practicing Cognitive-Behavioral and Mindfulness Skills in a Web-Based Platform among Older Adults through the COVID-19 Pandemic: A Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(20), 10563. https://doi.org/10.3390/ijerph182010563









