Testing of a Dual Process Model to Resolve the Socioeconomic Health Disparities: A Tale of Two Asian Countries
Abstract
1. Introduction
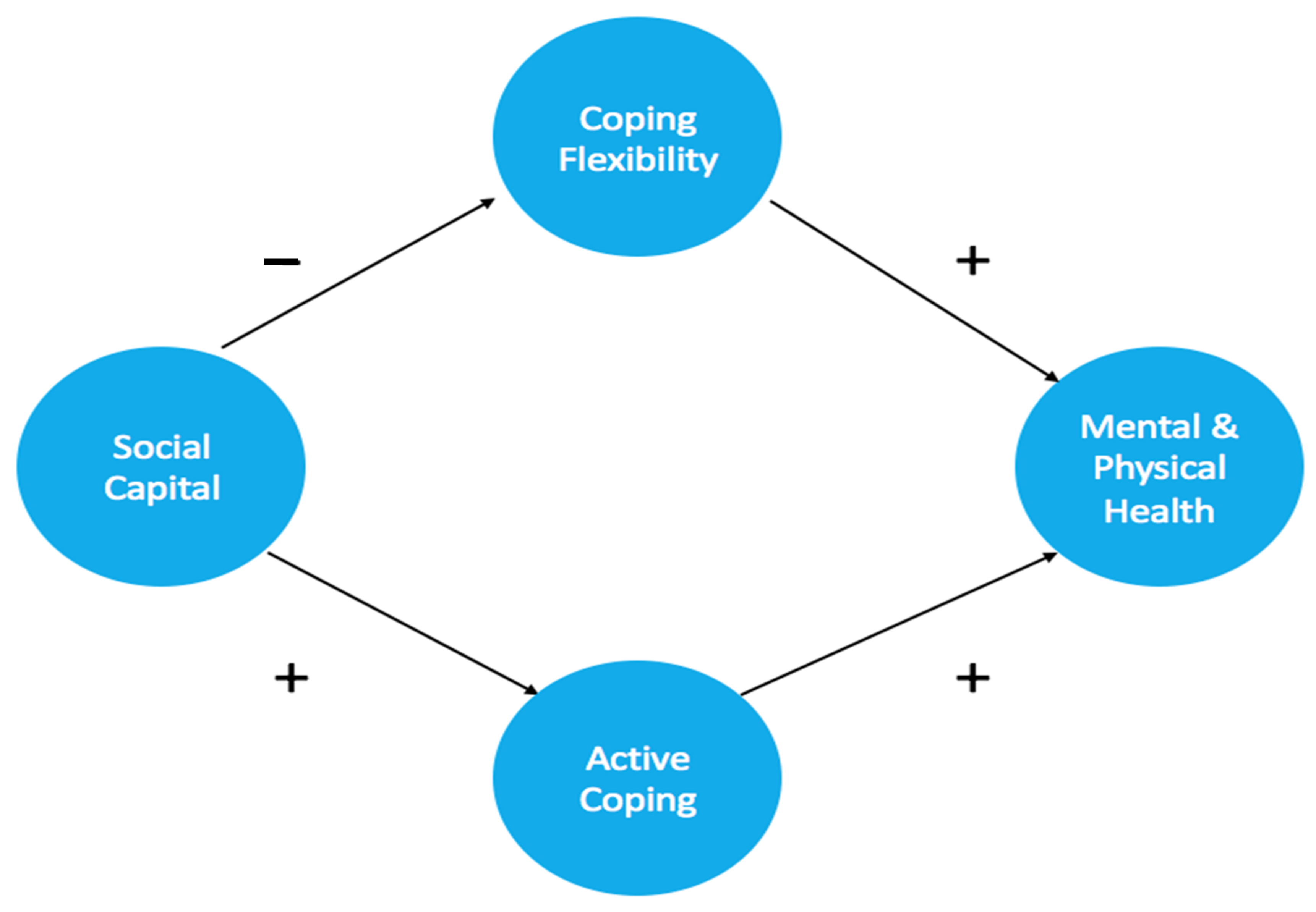
1.1. Active and Flexible Coping as Underlying Psychological Mechanisms
1.2. Individual Differences in Social Capital and Coping
1.3. Aims and Context of the Present Study
2. Methods
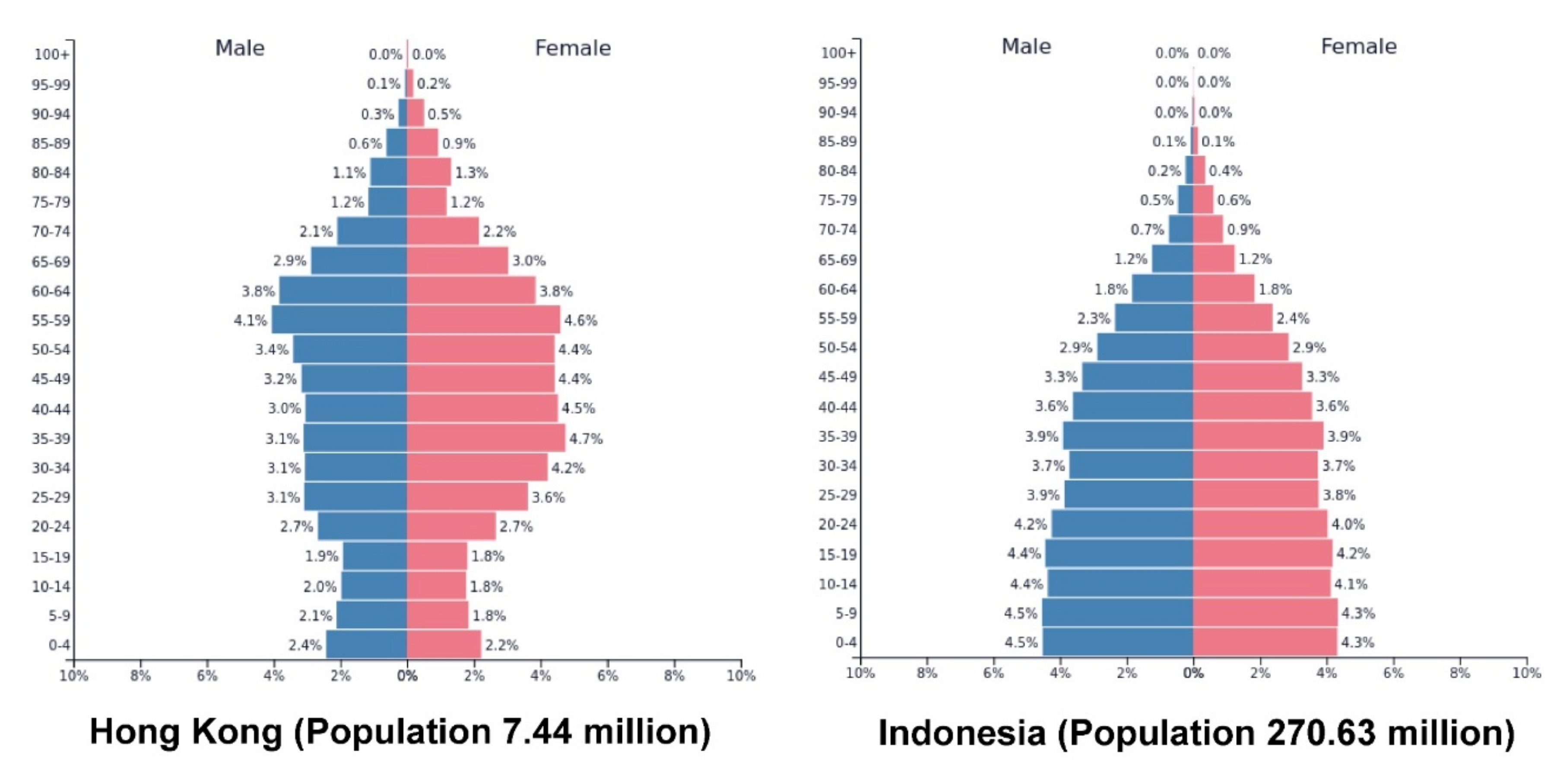
2.1. Study Design
2.2. Participants and Procedures
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Preliminary Analyses
3.2. Descriptive Statistics
3.3. Country and SES Differences
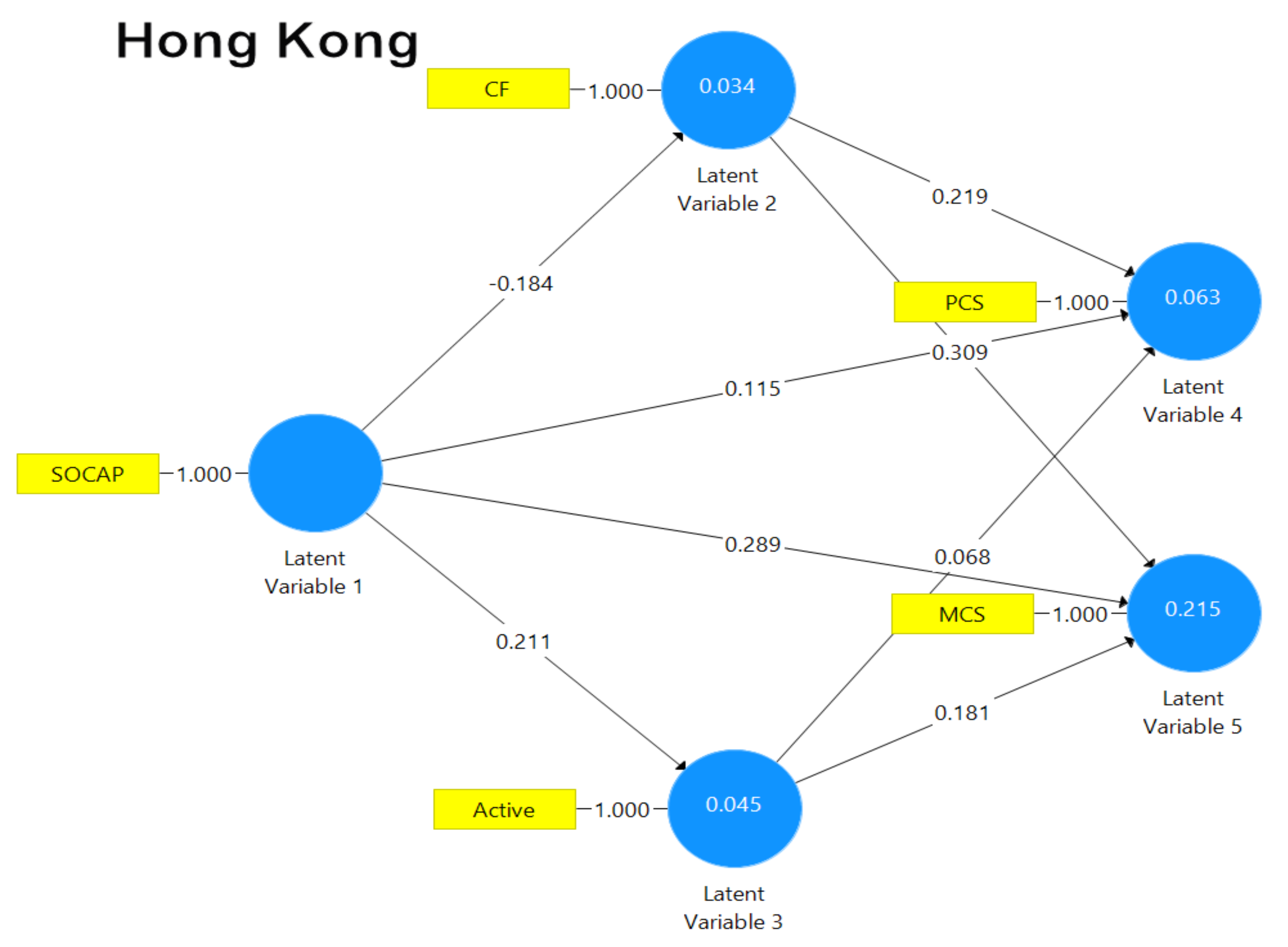
3.4. Path Analysis
4. Discussion
4.1. Dual Process Model
4.2. Mixed Findings on the Social Capital-Health Associations
4.3. Non-Significant Active Coping-Physical Health Associations
4.4. Research and Practical Implications
4.5. Limitations and Research Directions
4.6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Warren, B.S.; Sydenstricker, E. Health of garment workers: The relation of economic status to health. Public Health Rep. 1916, 31, 1298–1305. [Google Scholar]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- Braveman, P.A.; Cubbin, C.; Egerter, S.; Williams, D.R.; Pamuk, E. Socioeconomic disparities in health in the United States: What the patterns tell us. Am. J. Public Health 2010, 100 (Suppl. 1), S186–S196. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics. National Health Interview Survey; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2008.
- Kaplan, G.A.; Keil, J.E. Socioeconomic factors and cardiovascular disease: A review of the literature. Circulation 1993, 88, 1973–1998. [Google Scholar] [CrossRef]
- Taylor, S.E.; Repetti, R.L.; Seeman, T. Health psychology: What is an unhealthy environment and how does it get under the skin? Annu. Rev. Psychol. 1997, 48, 411–447. [Google Scholar] [CrossRef]
- Atal, S.; Cheng, C. Socioeconomic health disparities revisited: Coping flexibility enhances health-related quality of life for individuals low in socioeconomic status. Health Qual. Life Outcomes 2016, 14, 1–7. [Google Scholar] [CrossRef][Green Version]
- Lazarus, R.S.; Folkman, S. Transactional theory and research on emotions and coping. Eur. J. Personal. 1987, 1, 141–169. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Gan, Y.; Liu, Y.; Zhang, Y. Flexible coping responses to severe acute respiratory syndrome-related and daily life stressful events. Asian J. Soc. Psychol. 2004, 7, 55–66. [Google Scholar] [CrossRef]
- Stanton, A.L.; Danoff-Burg, S.; Huggins, M.E. The first year after breast cancer diagnosis: Hope and coping strategies as predictors of adjustment. Psychooncology 2002, 11, 93–102. [Google Scholar] [CrossRef]
- Niihata, K.; Fukuma, S.; Akizawa, T.; Fukuhara, S. Association of coping strategies with mortality and health-related quality of life in hemodialysis patients: The Japan Dialysis Outcomes and Practice Patterns Study. PLoS ONE 2017, 12, e0180498. [Google Scholar] [CrossRef]
- Cramer, R.J.; Johnson, J.C.; Crosby, J.W.; Henderson, C.E.; La Guardia, A.C.; Stroud, C.H. Personality, coping and mental health among lesbian, gay, and bisexual community members. Personal. Individ. Differ. 2016, 96, 272–278. [Google Scholar] [CrossRef]
- Kato, T. Development of the Coping Flexibility Scale: Evidence for the coping flexibility hypothesis. J. Couns. Psychol. 2012, 59, 262–273. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Hui, W.; Lam, S. Psychosocial factors and perceived severity of functional dyspeptic symptoms: A psychosocial interactionist model. Psychosom. Med. 2004, 66, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Leonidou, C.; Panayiotou, G.; Bati, A.; Karekla, M. Coping with psychosomatic symptoms: The buffering role of psychological flexibility and impact on quality of life. J. Health Psychol. 2019, 24, 175–187. [Google Scholar] [CrossRef] [PubMed]
- Weber, M. Class, status, party. In Inequality: Classic Readings in Race, Class, and Gender; Grusky, D.B., Szelenyi, S., Eds.; Westview: Boulder, CO, USA, 2006; pp. 37–53. [Google Scholar]
- Caplan, L.J.; Schooler, C. Socioeconomic status and financial coping strategies: The mediating role of perceived control. Soc. Psychol. Q. 2007, 70, 43–58. [Google Scholar] [CrossRef]
- Ross, C.E.; Mirowsky, J. Explaining the social patterns of depression: Control and problem solving—Or support and talking? J. Health Soc. Behav. 1989, 30, 206–219. [Google Scholar] [CrossRef]
- Cheng, C.; Lau, H.B.; Chan, M.S. Coping flexibility and psychological adjustment to stressful life changes: A meta-analytic review. Psychol. Bull. 2014, 140, 1582–1607. [Google Scholar] [CrossRef]
- World Bank. World Development Indicators Database; The World Bank Group: Washington, DC, USA, 2020; Available online: https://databank.worldbank.org/source/world-development-indicators (accessed on 14 October 2020).
- Li, K. Capitalist Development and Economism in East. Asia: The Rise of Hong Kong, Singapore, Taiwan and South. Korea; Routledge: New York, NY, USA, 2003. [Google Scholar]
- Central Intelligence Agency. The World Factbook: Distribution of Family Income—Gini Index; Central Intelligence Agency: Washington, DC, USA, 2020. Available online: https://www.cia.gov/library/publications/the-world-factbook/rankorder/2172rank.html (accessed on 14 October 2020).
- Park, C. The divergent paths of the East Asian welfare regimes: The effects of production regimes and democratization. Korean Soc. Sci. J. 2007, 34, 39–70. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Mishra, D.; Singh, H.P. Kuppuswamy’s Socioeconomic Status Scale—A revision. Indian J. Pediatrics 2003, 70, 273–274. [Google Scholar] [CrossRef]
- Chen, X.; Stanton, B.; Gong, J.; Fang, X.; Li, X. Personal Social Capital Scale: An instrument for health and behavioral research. Health Educ. Res. 2009, 24, 306–317. [Google Scholar] [CrossRef]
- Wang, P.; Chen, X.; Gong, J.; Jacques-Tiura, A.J. Reliability and validity of the Personal Social Capital Scale 16 and Personal Social Capital Scale 8: Two short instruments for survey studies. Soc. Indic. Res. 2014, 119, 1133–1148. [Google Scholar] [CrossRef]
- Lefante, J.J.; Harmon, G.N.; Ashby, K.M.; Barnard, D.; Webber, L.S. Use of the SF-8 to assess health-related quality of life for a chronically ill, low-income population participating in the Central Louisiana Medication Access Program (CMAP). Qual. Life Res. 2005, 14, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Hakim, M.; Kurniani, N.; Pinzon, R.; Tugasworo, D.; Basuki, M. Improvement of quality of life in patients with peripheral neuropathy treated with a fixed dose combination of high-dose vitamin B1, B6 and B12: Results from a 12-week prospective non-interventional study in Indonesia. J. Clin. Trials 2018, 8, 343. [Google Scholar] [CrossRef]
- Wang, S.; Luan, R.S.; Lei, Y.; Kuang, C.; He, C.; Chan, Y. Development and evaluation of Chinese version of Short Form 8. Mod. Prev. Med. 2007, 6, 1022–1036. [Google Scholar]
- The Jamovi Project jamovi. (Version 1.2.2.0) [Computer Software]. Available online: https://www.jamovi.org (accessed on 8 July 2020).
- Ringle, C.M.; Wende, S.; Becker, J.-M. SmartPLS 3 [Computer Software]. Available online: https://www.smartpls.com (accessed on 8 July 2020).
- Prus, S.G. Age, SES, and health: A population level analysis of health inequalities over the lifecourse. Sociol. Health Illn. 2007, 29, 275–296. [Google Scholar] [CrossRef]
- Stringhini, S.; Sabia, S.; Shipley, M.; Brunner, E.; Nabi, H.; Kivimaki, M.; Singh-Manoux, A. Association of socioeconomic position with health behaviors and mortality. JAMA 2010, 303, 1159–1166. [Google Scholar] [CrossRef]
- Spencer-Rodgers, J.; Boucher, H.C.; Mori, S.C.; Wang, L.; Peng, K. The dialectical self-concept: Contradiction, change, and holism in East Asian cultures. Personal. Soc. Psychol. Bull. 2009, 35, 29–44. [Google Scholar] [CrossRef]
- Gan, Y.; Zhang, Y.; Wang, X.; Wang, S.; Shen, X. The coping flexibility of neurasthenia and depressive patients. Personal. Individ. Differ. 2006, 40, 859–871. [Google Scholar] [CrossRef]
- Kato, T. Relationship between coping flexibility and the risk of depression in Indian adults. Asian J. Psychiatry 2016, 24, 130–134. [Google Scholar] [CrossRef]
- Folkman, S.; Moskowitz, J.T. Positive affect and the other side of coping. Am. Psychol. 2000, 55, 647. [Google Scholar] [CrossRef]
- Tokem, Y.; Ozcelik, H.; Cicik, A. Examination of the relationship between hopelessness levels and coping strategies among the family caregivers of patients with cancer. Cancer Nurs. 2015, 38, E28–E34. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, P.; Kilvert, A.; Hasson, L. A 21-year longitudinal analysis of impact, coping, and appraisals following spinal cord injury. Rehabil. Psychol. 2016, 61, 92. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Meng, T. Bonding, bridging, and linking social capital and self-rated health among Chinese adults: Use of the anchoring vignettes technique. PLoS ONE 2015, 10, e0142300. [Google Scholar] [CrossRef]
- Kawachi, I.; Berkman, L.F. Social ties and mental health. J. Urban Health 2001, 78, 458–467. [Google Scholar] [CrossRef] [PubMed]
- DeLongis, A.; Holtzman, S. Coping in context: The role of stress, social support, and personality in coping. J. Personal. 2005, 73, 1633–1656. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.E.; Sherman, D.K.; Kim, H.S.; Jarcho, J.; Takagi, K.; Dunagan, M.S. Culture and social support: Who seeks it and why? J. Personal. Soc. Psychol. 2004, 87, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.E.; Welch, W.T.; Kim, H.S.; Sherman, D.K. Cultural differences in the impact of social support on psychological and biological stress responses. Psychol. Sci. 2007, 18, 831–837. [Google Scholar] [CrossRef]
- Bozo, Ö.; Demirtepe-Saygılı, D.; Güneş, S.; Çenesiz, G.Z.; Baysan, A. Does problem focused coping buffer the effects of trait anxiety on depressive symptoms of chronic urticaria patients? J. Gen. Psychol. 2018, 145, 64–78. [Google Scholar] [CrossRef]
- Pereira, M.G.; Ramos, C.; Lobarinhas, A.; Machado, J.C.; Pedras, S. Satisfaction with life in individuals with a lower limb amputation: The importance of active coping and acceptance. Scand. J. Psychol. 2018, 59, 414–421. [Google Scholar] [CrossRef]
- Yama, H.; Zakaria, N. Explanations for cultural differences in thinking: Easterners’ dialectical thinking and Westerners’ linear thinking. J. Cogn. Psychol. 2019, 31, 487–506. [Google Scholar] [CrossRef]
- Chen, S.X.; Chan, W.; Bond, M.H.; Stewart, S.M. The effects of self-efficacy and relationship harmony on depression across cultures: Applying Level-Oriented and Structure-Oriented Analyses. J. Cross Cult. Psychol. 2006, 37, 643–658. [Google Scholar] [CrossRef]
- Kim, H.S.; Sherman, D.K.; Ko, D.; Taylor, S.E. Pursuit of comfort and pursuit of harmony: Culture, relationships, and social support seeking. Personal. Soc. Psychol. Bull. 2006, 32, 1595–1607. [Google Scholar] [CrossRef] [PubMed]
- Hofstede, G.H. Culture’s Consequences: Comparing Values, Behaviors, Institutions, and Organizations across Nations, 2nd ed.; Sage: Thousand Oaks, CA, USA, 2001. [Google Scholar]
- Triandis, H.C. Individualism and collectivism: Past, present, and future. In The Handbook of Culture and Psychology; Matsumoto, D., Ed.; Oxford University: New York, NY, USA, 2001; pp. 35–50. [Google Scholar]
- Oyserman, D.; Coon, H.M.; Kemmelmeier, M. Rethinking individualism and collectivism: Evaluation of theoretical assumptions and meta-analyses. Psychol. Bull. 2002, 128, 3–72. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.; Hong, Y.; Mischel, W.; Shoda, Y. Discriminative facility in social competence: Conditional versus dispositional encoding and monitoring-blunting of information. Soc. Cogn. 1995, 13, 49–70. [Google Scholar] [CrossRef]
- Idrus, S.; Rosida, L. Poverty in Indonesia: Critical review. Arch. Bus. Rev. 2020, 8, 127–132. [Google Scholar] [CrossRef]
- Lam, G. Problems encountered by elders in residential care services in Hong Kong. Asian Educ Dev. Studies 2020. [Google Scholar] [CrossRef]
- GovHK. Hong Kong: The Facts—Religion and Custom. Available online: https://www.gov.hk/en/about/abouthk/factsheets/docs/religion.pdf (accessed on 18 November 2020).
- Central Intelligence Agency. The World Factbook: Religions; Central Intelligence Agency: Washington, DC, USA, 2020. Available online: https://www.cia.gov/library/publications/the-world-factbook/fields/401.html (accessed on 14 October 2020).
- Ahmadi, F.; Hussin, N.A.M.; Mohammad, M.T. Religion, culture and meaning-making coping: A study among cancer patients in Malaysia. J. Relig. Health 2019, 58, 1909–1924. [Google Scholar] [CrossRef]
- Serfaty, D.R.; Cherniak, A.D.; Strous, R.D. How are psychotic symptoms and treatment factors affected by religion? A cross-sectional study about religious coping among ultra-Orthodox Jews. Psychiatry Res. 2020, 293, 113349. [Google Scholar] [CrossRef]
- De Silva, M.J.; Huttly, S.R.; Harpham, T.; Kenward, M.G. Social capital and mental health: A comparative analysis of four low income countries. Soc. Sci. Med. 2007, 64, 5–20. [Google Scholar] [CrossRef]
- Paasche-Orlow, M.K.; Parker, R.M.; Gazmararian, J.A.; Nielsen-Bohlman, L.T.; Rudd, R.R. The prevalence of limited health literacy. J. Gen. Intern. Med. 2005, 20, 175–184. [Google Scholar] [CrossRef]
- Kirsch, I.S.; Jungeblut, A.; Jenkins, L.; Kolstad, A. Adult Literacy in America: A First Look at the Findings of the National Adult Literacy Survey; Office of Educational Research and Improvement: Washington, DC, USA, 1993. [Google Scholar]
- Dowd, J.B.; Zajacova, A. Does the predictive power of self-rated health for subsequent mortality risk vary by socioeconomic status in the US? Int. J. Epidemiol. 2007, 36, 1214–1221. [Google Scholar] [CrossRef] [PubMed]

| Country | SES Subgroup | Mean | SD | n | |
|---|---|---|---|---|---|
| Social | Hong Kong | Low SES | 13.10 | 3.234 | 50 |
| Capital | Med SES | 22.68 | 5.133 | 50 | |
| High SES | 26.08 | 4.458 | 50 | ||
| Indonesia | Low SES | 12.32 | 3.254 | 50 | |
| Med SES | 21.08 | 4.873 | 50 | ||
| High SES | 24.20 | 4.891 | 50 | ||
| Coping | Hong Kong | Low SES | 0.5620 | 0.20894 | 50 |
| Flexibility | Med SES | 0.5245 | 0.24549 | 50 | |
| High SES | 0.4635 | 0.21790 | 50 | ||
| Indonesia | Low SES | 0.4755 | 0.24972 | 50 | |
| Med SES | 0.5555 | 0.20586 | 50 | ||
| High SES | 0.4760 | 0.18280 | 50 | ||
| Active | Hong Kong | Low SES | 0.4430 | 0.29735 | 50 |
| Coping | Med SES | 0.4819 | 0.23639 | 50 | |
| High SES | 0.5720 | 0.32288 | 50 | ||
| Indonesia | Low SES | 0.4870 | 0.26732 | 50 | |
| Med SES | 0.4865 | 0.28018 | 50 | ||
| High SES | 0.5545 | 0.24675 | 50 | ||
| Physical | Hong Kong | Low SES | 50.76 | 12.640 | 50 |
| Health | Med SES | 49.78 | 11.134 | 50 | |
| High SES | 50.96 | 11.012 | 50 | ||
| Indonesia | Low SES | 45.10 | 12.541 | 50 | |
| Med SES | 50.86 | 12.103 | 50 | ||
| High SES | 52.44 | 11.262 | 50 | ||
| Mental | Hong Kong | Low SES | 49.68 | 11.991 | 50 |
| Health | Med SES | 52.26 | 11.108 | 50 | |
| High SES | 51.94 | 12.060 | 50 | ||
| Indonesia | Low SES | 52.68 | 13.175 | 50 | |
| Med SES | 54.02 | 12.804 | 50 | ||
| High SES | 54.40 | 11.681 | 50 |
| Variable | SES Subgroup Pairs | p |
|---|---|---|
| Social Capital | Low SES (M = 12.71) vs. Medium SES (M = 21.88) | p < 0.001 |
| Medium SES (M = 21.88) vs. High SES (M = 25.14) | p < 0.001 | |
| Low SES (M = 12.71) vs. High SES (M = 25.14) | p < 0.001 | |
| Coping Flexibility | Medium SES (M = 0.54) vs. High SES (M = 0.47) | p = 0.074 |
| Active Coping | Low SES (M = 0.47) vs. High SES (M = 0.56) | p = 0.037 |
| Physical Health | Low SES (M = 0.47.93) vs. High SES (M = 51.70) | p = 0.076 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, C.; Cheng, F.; Atal, S.; Sarwono, S. Testing of a Dual Process Model to Resolve the Socioeconomic Health Disparities: A Tale of Two Asian Countries. Int. J. Environ. Res. Public Health 2021, 18, 717. https://doi.org/10.3390/ijerph18020717
Cheng C, Cheng F, Atal S, Sarwono S. Testing of a Dual Process Model to Resolve the Socioeconomic Health Disparities: A Tale of Two Asian Countries. International Journal of Environmental Research and Public Health. 2021; 18(2):717. https://doi.org/10.3390/ijerph18020717
Chicago/Turabian StyleCheng, Cecilia, Fanny Cheng, Saloni Atal, and Sarlito Sarwono. 2021. "Testing of a Dual Process Model to Resolve the Socioeconomic Health Disparities: A Tale of Two Asian Countries" International Journal of Environmental Research and Public Health 18, no. 2: 717. https://doi.org/10.3390/ijerph18020717
APA StyleCheng, C., Cheng, F., Atal, S., & Sarwono, S. (2021). Testing of a Dual Process Model to Resolve the Socioeconomic Health Disparities: A Tale of Two Asian Countries. International Journal of Environmental Research and Public Health, 18(2), 717. https://doi.org/10.3390/ijerph18020717






