A Conceptual Model of Long-Term Weight Loss Maintenance: The Importance of Cognitive, Empirical and Computational Approaches
Abstract
1. The Obesity Pandemic
2. Executive Functioning and Overweight and Obesity
3. Can Training Executive Functions Improve Weight Loss Maintenance?
4. The Impacts of Weight Loss on Executive Functioning
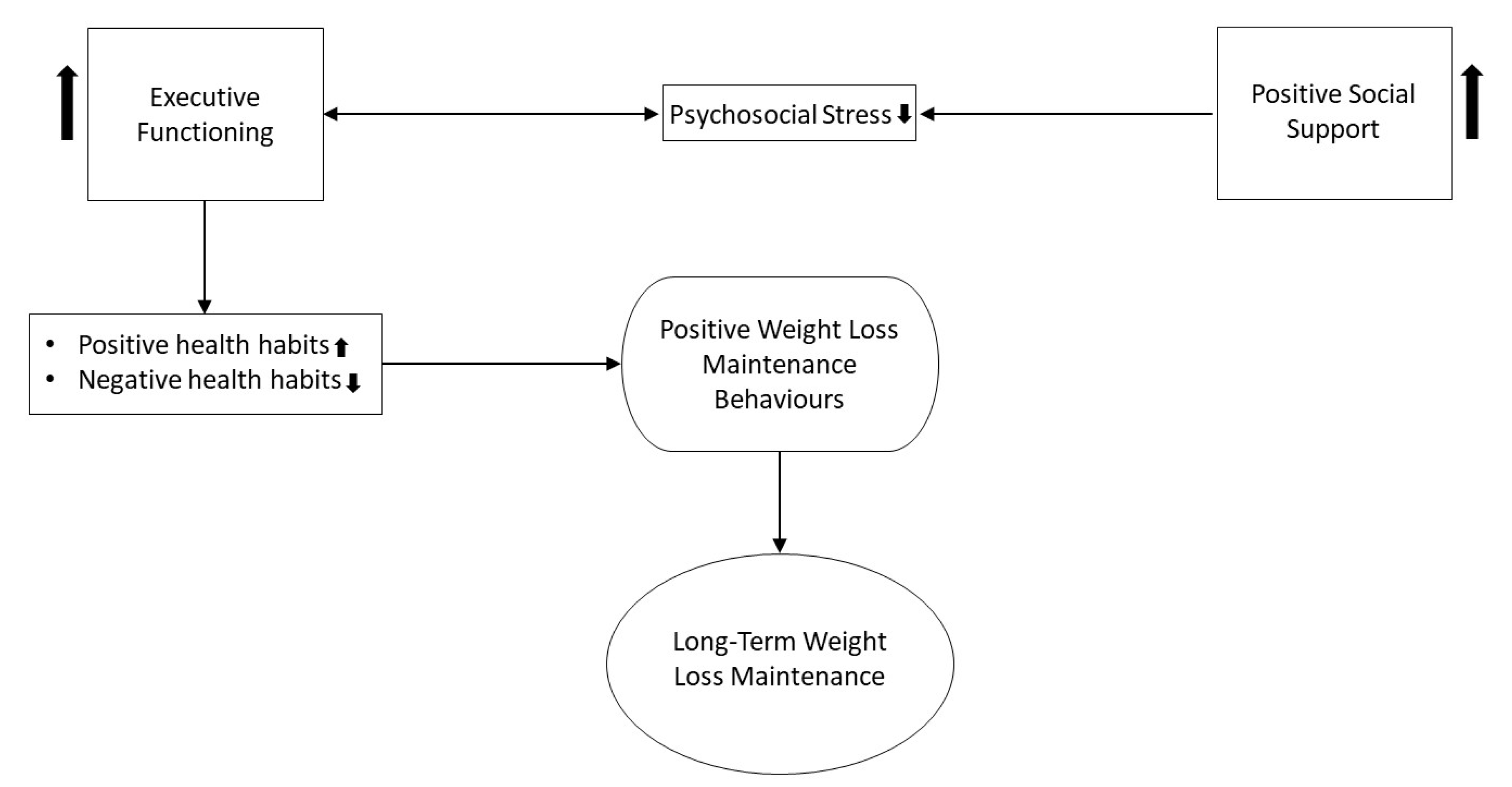
5. Social Support and Weight Loss Maintenance
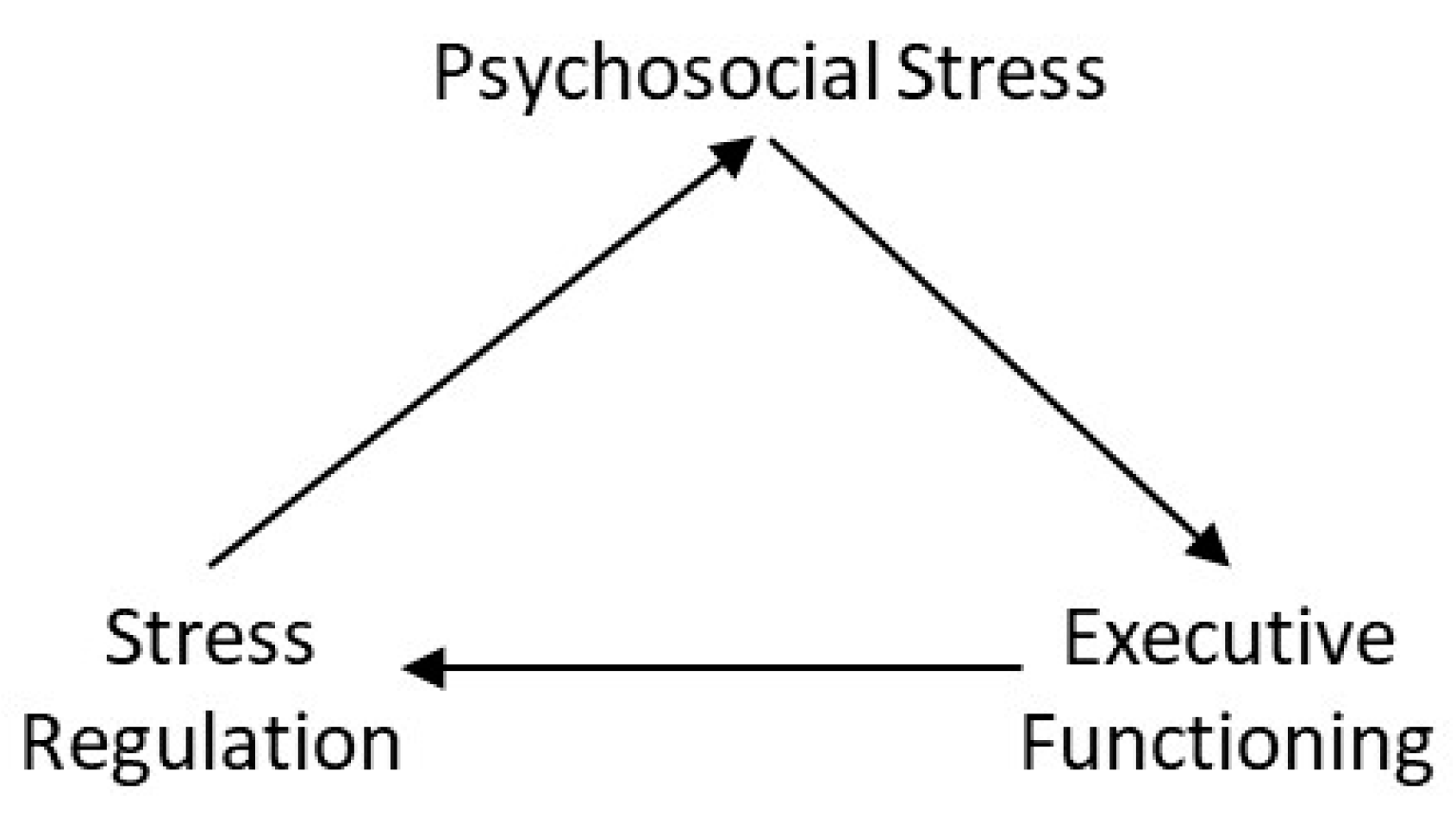
5.1. Psychosocial Stress, Executive Function and Social Support
5.2. Executive Functioning and Habit
6. A Conceptual Framework of Long-Term Weight Loss Maintenance: Executive Functioning, Social Support, Psychosocial Stress and Habit
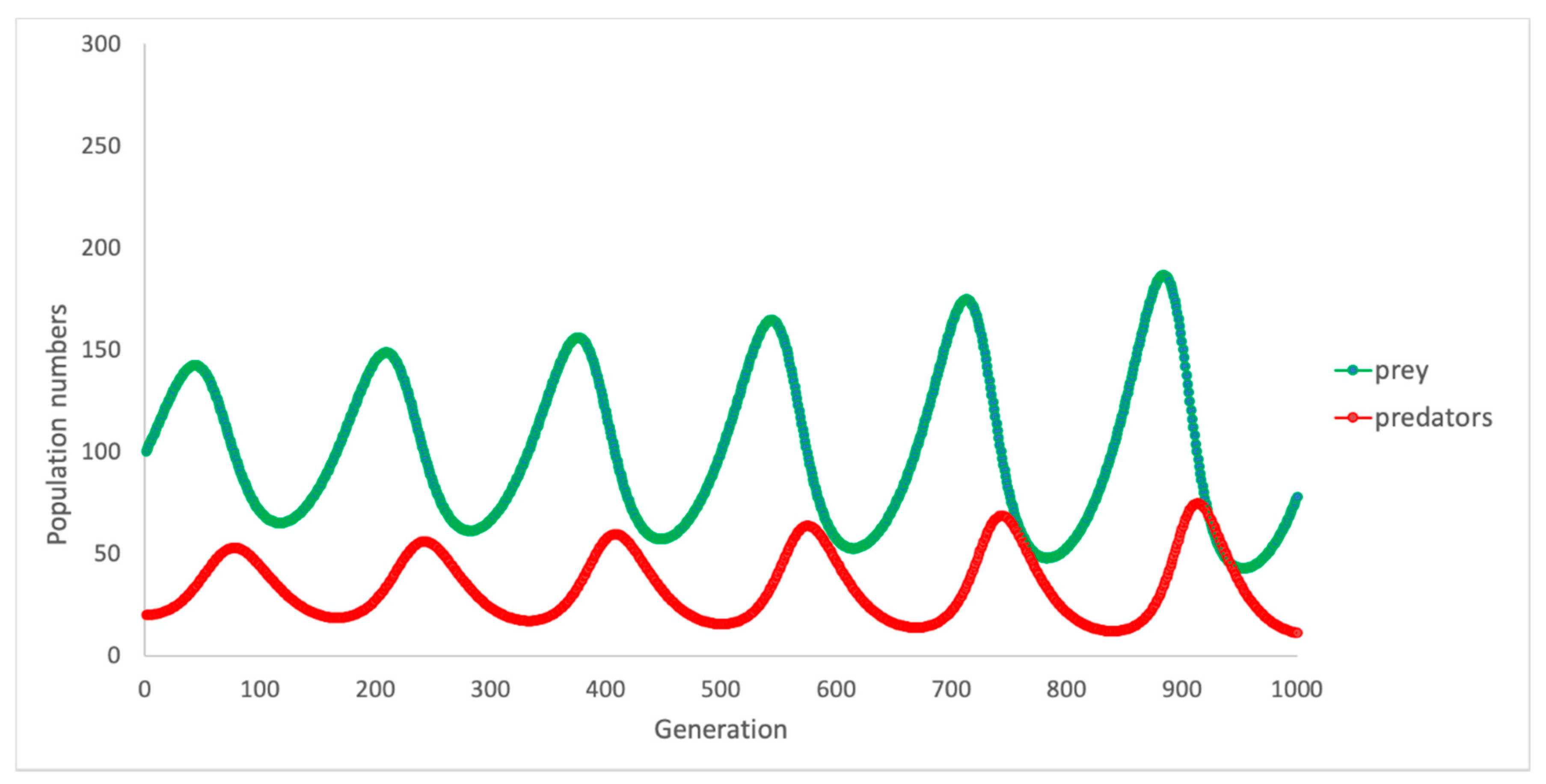
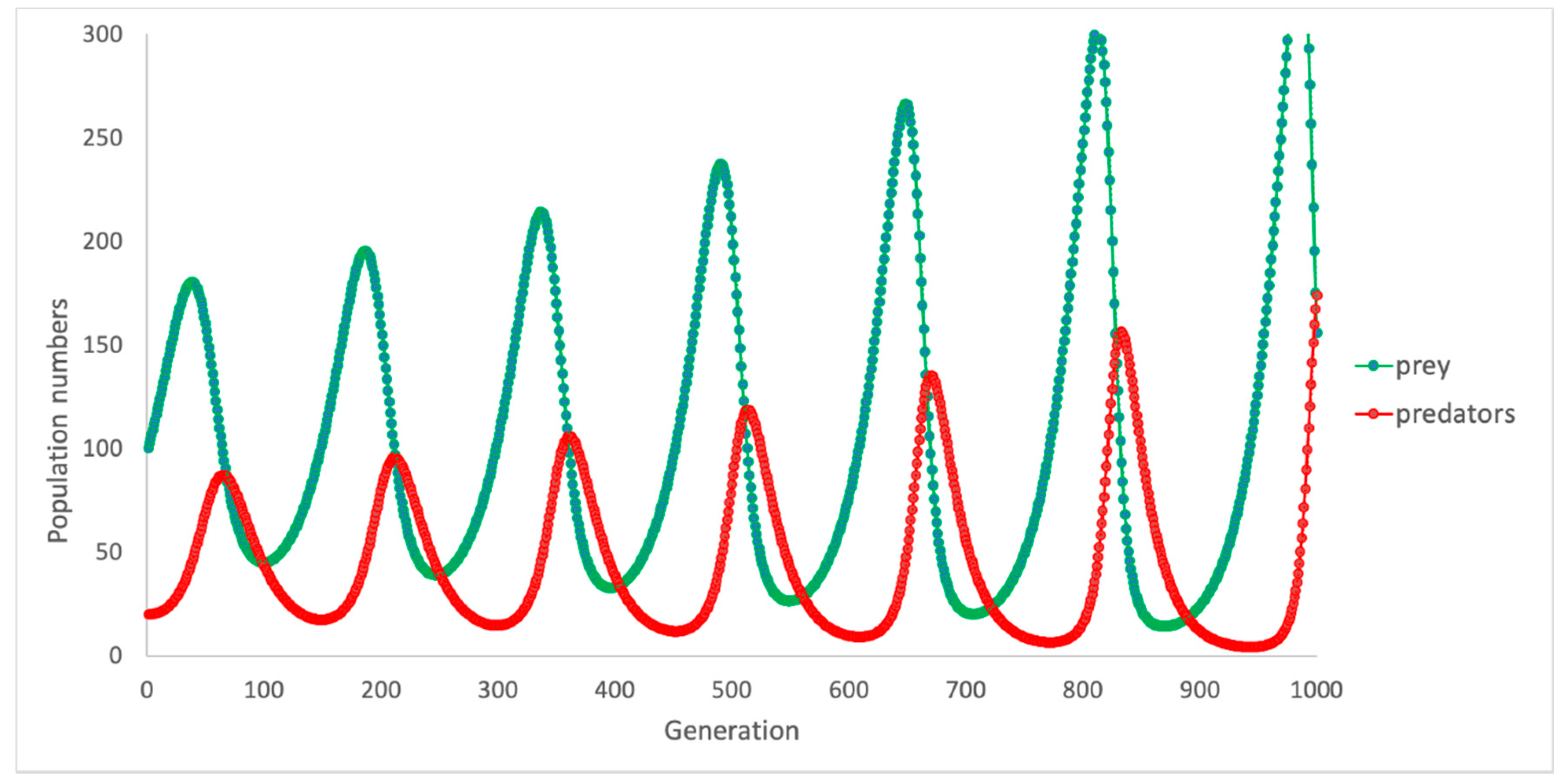
7. Framework Validation and Extension
7.1. Verbal Models—What Are They Good For?
7.2. The Role of Computational Models in Understanding Behaviour
- (1)
- What are the essential or “key variables” of the model (and, thus what is extraneous)?
- (2)
- How should the key variables be instantiated and what is the range of properties or values that should be given to each variable?
- (3)
- How should the relation between key variables be expressed?
- (4)
- What criteria should be used to evaluate the model’s success in simulating the phenomenon?
7.3. The Role of Computational Models in Understanding Behaviour
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Obesity and Overweight; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Ward, Z.J.; Bleich, S.N.; Cradock, A.L.; Barrett, J.L.; Giles, C.M.; Flax, C.; Long, M.W.; Gortmaker, S.L. Projected US state-level prevalence of adult obesity and severe obesity. N. Engl. J. Med. 2019, 381, 2440–2450. [Google Scholar] [CrossRef]
- Khan, S.S.; Ning, H.; Wilkins, J.T.; Allen, N.; Carnethon, M.; Berry, J.D.; Sweis, R.N.; Lloyd-Jones, D.M. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018, 3, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Hinnouho, G.-M.; Czernichow, S.; Dugravot, A.; Nabi, H.; Brunner, E.J.; Kivimaki, M.; Singh-Manoux, A. Metabolically healthy obesity and the risk of cardiovascular disease and type 2 diabetes: The Whitehall II cohort study. Eur. Heart J. 2015, 36, 551–559. [Google Scholar] [CrossRef]
- Avgerinos, K.I.; Spyrou, N.; Mantzoros, C.S.; Dalamaga, M. Obesity and cancer risk: Emerging biological mechanisms and perspectives. Metabolism 2019, 92, 121–135. [Google Scholar] [CrossRef]
- Mannan, M.; Mamun, A.; Doi, S.; Clavarino, A. Prospective associations between depression and obesity for adolescent males and females-a systematic review and meta-analysis of longitudinal studies. PLoS ONE 2016, 11, e0157240. [Google Scholar] [CrossRef]
- Rajan, T.M.; Menon, V. Psychiatric disorders and obesity: A review of association studies. J. Postgrad. Med. 2017, 63, 182. [Google Scholar]
- Jung, F.U.; Luck-Sikorski, C. Overweight and lonely? A representative study on loneliness in obese people and its determinants. Obes. Facts 2019, 12, 440–447. [Google Scholar] [CrossRef]
- Pedditizi, E.; Peters, R.; Beckett, N. The risk of overweight/obesity in mid-life and late life for the development of dementia: A systematic review and meta-analysis of longitudinal studies. Age Ageing 2016, 45, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Berry, E.M. The Obesity Pandemic—Whose Responsibility? No Blame, No Shame, Not More of the Same. Front. Nutr. 2020, 7, 2. [Google Scholar] [CrossRef]
- Livingston, E.H. Reimagining obesity in 2018: A JAMA theme issue on obesity. JAMA 2018, 319, 238–240. [Google Scholar] [CrossRef]
- Ge, L.; Sadeghirad, B.; Ball, G.D.C.; da Costa, B.R.; Hitchcock, C.L.; Svendrovski, A.; Kiflen, R.; Quadri, K.; Kwon, H.Y.; Karamouzian, M. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: Systematic review and network meta-analysis of randomised trials. BMJ 2020, 369. [Google Scholar] [CrossRef] [PubMed]
- Dombrowski, S.U.; Knittle, K.; Avenell, A.; Araujo-Soares, V.; Sniehotta, F.F. Long term maintenance of weight loss with non-surgical interventions in obese adults: Systematic review and meta-analyses of randomised controlled trials. BMJ 2014, 348, g2646. [Google Scholar] [CrossRef]
- Hemmingsson, E. A new model of the role of psychological and emotional distress in promoting obesity: Conceptual review with implications for treatment and prevention. Obes. Rev. 2014, 15, 769–779. [Google Scholar] [CrossRef] [PubMed]
- Olivo, G.; Gour, S.; Schiöth, H.B. Low neuroticism and cognitive performance are differently associated to overweight and obesity: A cross-sectional and longitudinal UK Biobank study. Psychoneuroendocrinology 2019, 101, 167–174. [Google Scholar] [CrossRef]
- Yang, Y.; Shields, G.S.; Guo, C.; Liu, Y. Executive function performance in obesity and overweight individuals: A meta-analysis and review. Neurosci. Biobehav. Rev. 2018, 84, 225–244. [Google Scholar] [CrossRef]
- Lezak, M.D.; Howieson, D.B.; Loring, D.W.; Fischer, J.S. Neuropsychological Assessment; Oxford University Press: New York, NY, USA, 2004. [Google Scholar]
- Norman, D.A.; Shallice, T. Attention to action. In Consciousness and Self-Regulation; Springer: Berlin/Heidelberg, Germany, 1986; pp. 1–18. [Google Scholar]
- Shallice, T.; Burgess, P. The domain of supervisory processes and temporal organization of behaviour. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 1996, 351, 1405–1412. [Google Scholar]
- Banich, M.T. Executive function: The search for an integrated account. Curr. Dir. Psychol. Sci. 2009, 18, 89–94. [Google Scholar] [CrossRef]
- Miyake, A.; Friedman, N.P.; Emerson, M.J.; Witzki, A.H.; Howerter, A.; Wager, T.D. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: A latent variable analysis. Cogn. Psychol. 2000, 41, 49–100. [Google Scholar] [CrossRef]
- Dinn, W.M.; Aycicegi, A.; Harris, C.L. Cigarette smoking in a student sample: Neurocognitive and clinical correlates. Addict. Behav. 2004, 29, 107–126. [Google Scholar] [CrossRef]
- Mullan, B.; Wong, C.; Allom, V.; Pack, S.L. The role of executive function in bridging the intention-behaviour gap for binge-drinking in university students. Addict. Behav. 2011, 36, 1023–1026. [Google Scholar] [CrossRef]
- Golub, S.A.; Starks, T.J.; Kowalczyk, W.J.; Thompson, L.I.; Parsons, J.T. Profiles of executive functioning: Associations with substance dependence and risky sexual behavior. Psychol. Addict. Behav. 2012, 26, 895. [Google Scholar] [CrossRef]
- Kor, K.; Mullan, B.A. Sleep hygiene behaviours: An application of the theory of planned behaviour and the investigation of perceived autonomy support, past behaviour and response inhibition. Psychol. Health 2011, 26, 1208–1224. [Google Scholar] [CrossRef]
- Gettens, K.M.; Gorin, A.A. Executive function in weight loss and weight loss maintenance: A conceptual review and novel neuropsychological model of weight control. J. Behav. Med. 2017, 40, 687–701. [Google Scholar] [CrossRef]
- Allom, V.; Mullan, B.; Smith, E.; Hay, P.; Raman, J. Breaking bad habits by improving executive function in individuals with obesity. BMC Public Health 2018, 18, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Dohle, S.; Diel, K.; Hofmann, W. Executive functions and the self-regulation of eating behavior: A review. Appetite 2018, 124, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.L.; Mullan, B.A. Predicting breakfast consumption: An application of the theory of planned behaviour and the investigation of past behaviour and executive function. Br. J. Health Psychol. 2009, 14, 489–504. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, M.; Raman, J.; Sui, Z. Cognitive remediation-enabled cognitive behaviour therapy for obesity: A case series. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2019, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Raman, J.; Hay, P.; Tchanturia, K.; Smith, E. A randomised controlled trial of manualized cognitive remediation therapy in adult obesity. Appetite 2018, 123, 269–279. [Google Scholar] [CrossRef]
- Smith, E.; Whittingham, C. Cognitive remediation therapy plus behavioural weight loss compared to behavioural weight loss alone for obesity: Study protocol for a randomised controlled trial. Trials 2017, 18, 42. [Google Scholar] [CrossRef]
- O’Neill, J.; Kamper-DeMarco, K.; Chen, X.; Orom, H. Too stressed to self-regulate? Associations between stress, self-reported executive function, disinhibited eating, and BMI in women. Eat. Behav. 2020, 39, 101417. [Google Scholar] [CrossRef]
- Padilla, M.M.; Fernández-Serrano, M.J.; García, A.V.; del Paso, G.A.R. Negative Social Evaluation Impairs Executive Functions in Adolescents with Excess Weight: Associations with Autonomic Responses. Ann. Behav. Med. 2019, 53, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Fossati, P.; Ergis, A.M.; Allilaire, J.F. Executive functioning in unipolar depression: A review. L’encéphale 2002, 28, 97. [Google Scholar] [PubMed]
- Nilsson, J.P.; Söderström, M.; Karlsson, A.U.; Lekander, M.; Åkerstedt, T.; Lindroth, N.E.; Axelsson, J. Less effective executive functioning after one night’s sleep deprivation. J. Sleep Res. 2005, 14, 1–6. [Google Scholar] [CrossRef]
- Cheatham, R.A.; Roberts, S.B.; Das, S.K.; Gilhooly, C.H.; Golden, J.K.; Hyatt, R.; Lerner, D.; Saltzman, E.; Lieberman, H.R. Long-term effects of provided low and high glycemic load low energy diets on mood and cognition. Physiol. Behav. 2009, 98, 374–379. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brubacher, D.; Monsch, A.; Stähelin, H. Weight change and cognitive performance. Int. J. Obes. 2004, 28, 1163–1167. [Google Scholar] [CrossRef][Green Version]
- Peven, J.C.; Jakicic, J.M.; Rogers, R.J.; Lesnovskaya, A.; Erickson, K.I.; Kang, C.; Zhou, X.; Porter, A.; Donofry, S.D.; Watt, J.C. The effects of a 12-Month weight loss intervention on cognitive outcomes in adults with overweight and obesity. Nutrients 2020, 12, 2988. [Google Scholar] [CrossRef] [PubMed]
- Bryan, J.; Tiggemann, M. The effect of weight-loss dieting on cognitive performance and psychological well-being in overweight women. Appetite 2001, 36, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Siervo, M.; Nasti, G.; Stephan, B.C.; Papa, A.; Muscariello, E.; Wells, J.C.; Prado, C.M.; Colantuoni, A. Effects of intentional weight loss on physical and cognitive function in middle-aged and older obese participants: A pilot study. J. Am. Coll. Nutr. 2012, 31, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Espeland, M.A.; Rapp, S.R.; Bray, G.A.; Houston, D.K.; Johnson, K.C.; Kitabchi, A.E.; Hergenroeder, A.L.; Williamson, J.; Jakicic, J.M.; van Dorsten, B. Long-term impact of behavioral weight loss intervention on cognitive function. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2014, 69, 1101–1108. [Google Scholar] [CrossRef]
- Halyburton, A.K.; Brinkworth, G.D.; Wilson, C.J.; Noakes, M.; Buckley, J.D.; Keogh, J.B.; Clifton, P.M. Low- and high-carbohydrate weight-loss diets have similar effects on mood but not cognitive performance. Am. J. Clin. Nutr. 2007, 86, 580–587. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.K.; Anton, S.D.; Han, H.; York-Crowe, E.; Redman, L.M.; Ravussin, E.; Williamson, D.A. Examination of Cognitive Function During Six Months of Calorie Restriction: Results of a Randomized Controlled Trial. Rejuvenation Res. 2007, 10, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Siervo, M.; Arnold, R.; Wells, J.C.K.; Tagliabue, A.; Colantuoni, A.; Albanese, E.; Brayne, C.; Stephan, B.C.M. Intentional weight loss in overweight and obese individuals and cognitive function: A systematic review and meta-analysis. Obes. Rev. 2011, 12, 968–983. [Google Scholar] [CrossRef]
- Green, M.W.; Elliman, N.A.; Kretsch, M.J. Weight loss strategies, stress, and cognitive function: Supervised versus unsupervised dieting. Psychoneuroendocrinology 2005, 30, 908–918. [Google Scholar] [CrossRef] [PubMed]
- Brinkworth, G.D.; Buckley, J.D.; Noakes, M.; Clifton, P.M.; Wilson, C.J. Long-term effects of a very low-carbohydrate diet and a lowfat diet on mood and cognitive function. Arch. Intern. Med. 2009, 169, 1873–1880. [Google Scholar] [CrossRef] [PubMed]
- Tarrant, M.; Khan, S.S.; Farrow, C.V.; Shah, P.; Daly, M.; Kos, K. Patient experiences of a bariatric group programme for managing obesity: A qualitative interview study. Br. J. Health Psychol. 2017, 22, 77–93. [Google Scholar] [CrossRef] [PubMed]
- Verheijden, M.W.; Bakx, J.C.; van Weel, C.; Koelen, M.A.; van Staveren, W.A. Role of social support in lifestyle-focused weight management interventions. Eur. J. Clin. Nutr. 2005, 59, S179–S186. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.N.; Hammen, C.; Henry, R.M.; Daley, S.E. Effects of stress and social support on recurrence in bipolar disorder. J. Affect. Disord. 2004, 82, 143–147. [Google Scholar] [CrossRef]
- Adams, C.E.; Greenway, F.L.; Brantley, P.J. Lifestyle factors and ghrelin: Critical review and implications for weight loss maintenance. Obes. Rev. 2011, 12, e211–e218. [Google Scholar] [CrossRef]
- Elfhag, K.; Rössner, S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes. Rev. 2005, 6, 67–85. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.G.; Suchy, Y.; Rau, H.K. Individual Differences in Executive Functioning: Implications for Stress Regulation. Ann. Behav. Med. 2009, 37, 126–140. [Google Scholar] [CrossRef] [PubMed]
- DePue, J.D.; Clark, M.M.; Ruggiero, L.; Medeiros, M.L.; Pera, V., Jr. Maintenance of Weight Loss: A Needs Assessment. Obes. Res. 1995, 3, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.O.; Ottenbacher, A.J.; Lucke, J.F.; Etchegaray, J.M.; Graham, A.L.; Thomas, E.J.; Bernstam, E.V. Measuring Social Support for Weight Loss in an Internet Weight Loss Community. J. Health Commun. 2011, 16, 198–211. [Google Scholar] [CrossRef] [PubMed]
- Asbjørnsen, R.A.; Wentzel, J.; Smedsrød, M.L.; Hjelmesæth, J.; Clark, M.M.; Nes, L.S.; Van Gemert-Pijnen, J.E. Identifying Persuasive Design Principles and Behavior Change Techniques Supporting End User Values and Needs in eHealth Interventions for Long-Term Weight Loss Maintenance: Qualitative Study. J. Med. Internet Res. 2020, 22, e22598. [Google Scholar] [CrossRef]
- Wolfe, W.A. A review: Maximizing social support—A neglected strategy for improving weight management with African-American women. Ethn. Dis. 2004, 14, 212–218. [Google Scholar] [PubMed]
- Harvey-Berino, J.; Pintauro, S.; Buzzell, P.; Gold, E.C. Effect of Internet Support on the Long-Term Maintenance of Weight Loss. Obes. Res. 2004, 12, 320–329. [Google Scholar] [CrossRef] [PubMed]
- Dailey, R.; Romo, L.; Myer, S.; Thomas, C.; Aggarwal, S.; Nordby, K.; Johnson, M.; Dunn, C. The buddy benefit: Increasing the effectiveness of an employee-targeted weight-loss program. J. Health Commun. 2018, 23, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Brantley, P.J.; Stewart, D.W.; Myers, V.H.; Matthews-Ewald, M.R.; Ard, J.D.; Coughlin, J.W.; Jerome, G.J.; Samuel-Hodge, C.; Lien, L.F.; Gullion, C.M.; et al. Psychosocial predictors of weight regain in the weight loss maintenance trial. J. Behav. Med. 2014, 37, 1155–1168. [Google Scholar] [CrossRef] [PubMed]
- Karfopoulou, E.; Anastasiou, C.A.; Avgeraki, E.; Kosmidis, M.H.; Yannakoulia, M. The role of social support in weight loss maintenance: Results from the MedWeight study. J. Behav. Med. 2016, 39, 511–518. [Google Scholar] [CrossRef]
- Gettens, K.M. The Role of Executive Function on Weight Loss and Maintenance in a Couples-Based Intervention, Doctoral Dissertation; University of Connecticut: Connecticut, CT, USA, 2019; Available online: https://opencommons.uconn.edu/dissertations/2203 (accessed on 21 December 2020).
- Gardner, B. A review and analysis of the use of ‘habit’ in understanding, predicting and influencing health-related behaviour. Health Psychol. Rev. 2015, 9, 277–295. [Google Scholar] [CrossRef]
- Allom, V.; Mullan, B. Self-regulation versus habit: The influence of self-schema on fruit and vegetable consumption. Psychol. Health 2012, 27, 7–24. [Google Scholar] [CrossRef]
- Allom, V.; Mullan, B.; Hagger, M. Does inhibitory control training improve health behaviour? A meta-analysis. Health Psychol. Rev. 2016, 10, 168–186. [Google Scholar] [CrossRef] [PubMed]
- Strack, F.; Deutsch, R. Reflective and Impulsive Determinants of Social Behavior. Personal. Soc. Psychol. Rev. 2004, 8, 220–247. [Google Scholar] [CrossRef]
- Hofmann, W.; Schmeichel, B.J.; Baddeley, A.D. Executive functions and self-regulation. Trends Cogn. Sci. 2012, 16, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.P.; Ruh, N.; Mareschal, D. The Goal Circuit Model: A Hierarchical Multi-Route Model of the Acquisition and Control of Routine Sequential Action in Humans. Cogn. Sci. 2014, 38, 244–274. [Google Scholar] [CrossRef] [PubMed]
- Gardner, B.; Sheals, K.; Wardle, J.; McGowan, L. Putting habit into practice, and practice into habit: A process evaluation and exploration of the acceptability of a habit-based dietary behaviour change intervention. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 135. [Google Scholar] [CrossRef]
- Cooper, R.P. Action Production and Event Perception as Routine Sequential Behaviors. Top. Cogn. Sci. 2019. [Google Scholar] [CrossRef]
- Moghaddam, M.; Chen, Q.; Deshmukh, A.V. A neuro-inspired computational model for adaptive fault diagnosis. Expert Syst. Appl. 2020, 140, 112879. [Google Scholar] [CrossRef]
- Lopes, T.V.; Rocha, A.C.; Murad, M.A.; Garcia, E.L.; Pereira, P.A.; Cazarin, C.L. A new computational model for flow in karst-carbonates containing solution-collapse breccias. Comput. Geosci. 2020, 24, 61–87. [Google Scholar] [CrossRef]
- Baughman, F.D.; Cooper, R.P. Inhibition and young children’s performance on the Tower of London task. Cogn. Syst. Res. 2007, 8, 216–226. [Google Scholar] [CrossRef]
- Thomas, M.; McClelland, J.; Richardson, F.; Schapiro, A.; Baughman, F. Dynamic and Connectionist Approaches to Development: Toward a Future of Mutually Beneficial Coevolution. In Toward a Unified Theory of Development Connectionism and Dynamic System Theory Re-Consider; Oxford University Press: Oxford, UK, 2009; pp. 337–353. [Google Scholar]
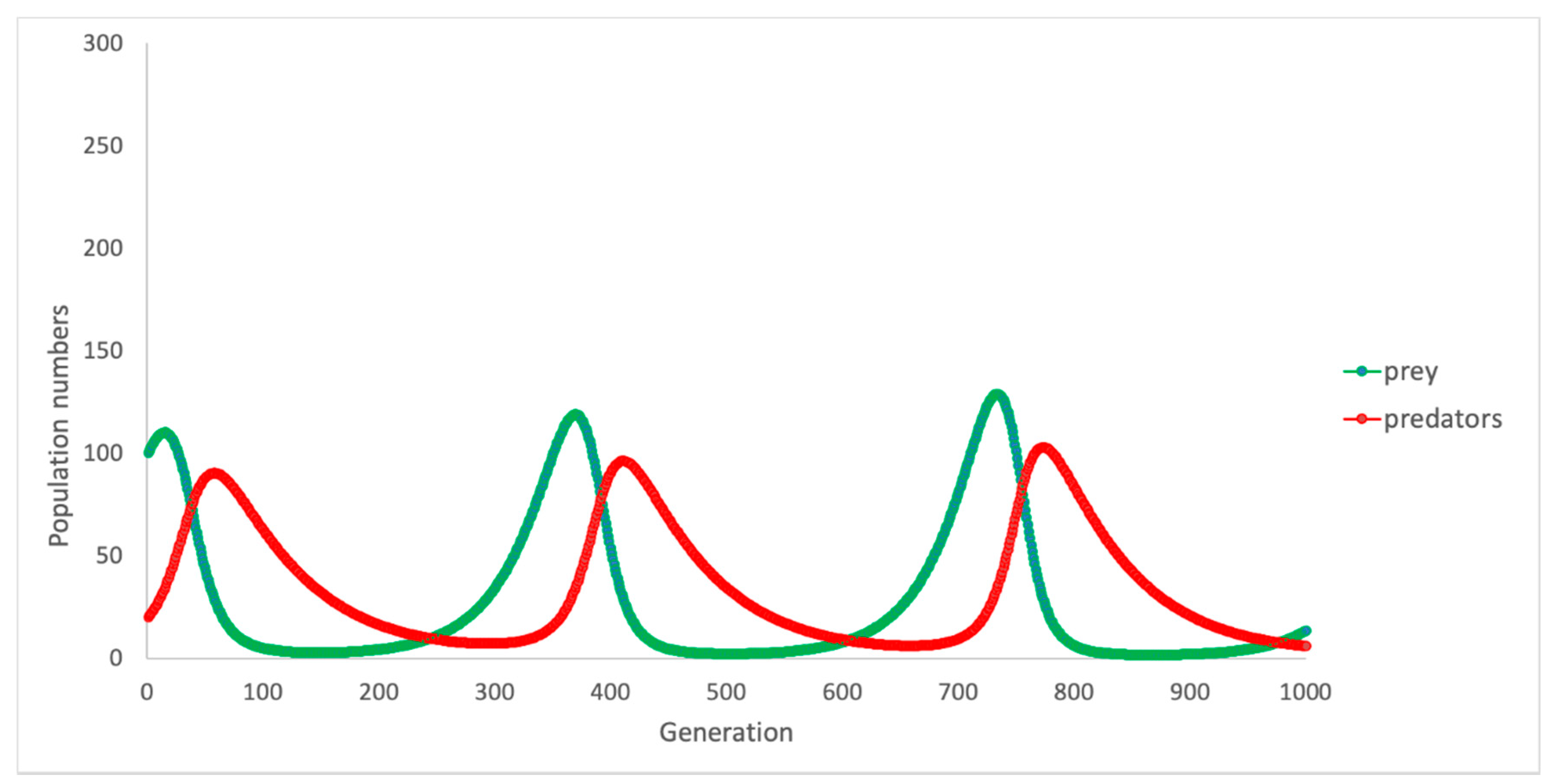
- Murray, J. Mathematical Biology; Springer: New York, NY, USA, 2002. [Google Scholar]
- Wangersky, P.J. Lotka-Volterra Population Models. Annu. Rev. Ecol. Syst. 1978, 9, 189–218. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haywood, D.; Lawrence, B.J.; Baughman, F.D.; Mullan, B.A. A Conceptual Model of Long-Term Weight Loss Maintenance: The Importance of Cognitive, Empirical and Computational Approaches. Int. J. Environ. Res. Public Health 2021, 18, 635. https://doi.org/10.3390/ijerph18020635
Haywood D, Lawrence BJ, Baughman FD, Mullan BA. A Conceptual Model of Long-Term Weight Loss Maintenance: The Importance of Cognitive, Empirical and Computational Approaches. International Journal of Environmental Research and Public Health. 2021; 18(2):635. https://doi.org/10.3390/ijerph18020635
Chicago/Turabian StyleHaywood, Darren, Blake J. Lawrence, Frank D. Baughman, and Barbara A. Mullan. 2021. "A Conceptual Model of Long-Term Weight Loss Maintenance: The Importance of Cognitive, Empirical and Computational Approaches" International Journal of Environmental Research and Public Health 18, no. 2: 635. https://doi.org/10.3390/ijerph18020635
APA StyleHaywood, D., Lawrence, B. J., Baughman, F. D., & Mullan, B. A. (2021). A Conceptual Model of Long-Term Weight Loss Maintenance: The Importance of Cognitive, Empirical and Computational Approaches. International Journal of Environmental Research and Public Health, 18(2), 635. https://doi.org/10.3390/ijerph18020635




