The Effects of Air Pollution, Sea Exposure and Altitude on COVID-19 Hospitalization Rates in Italy
Abstract
1. Introduction
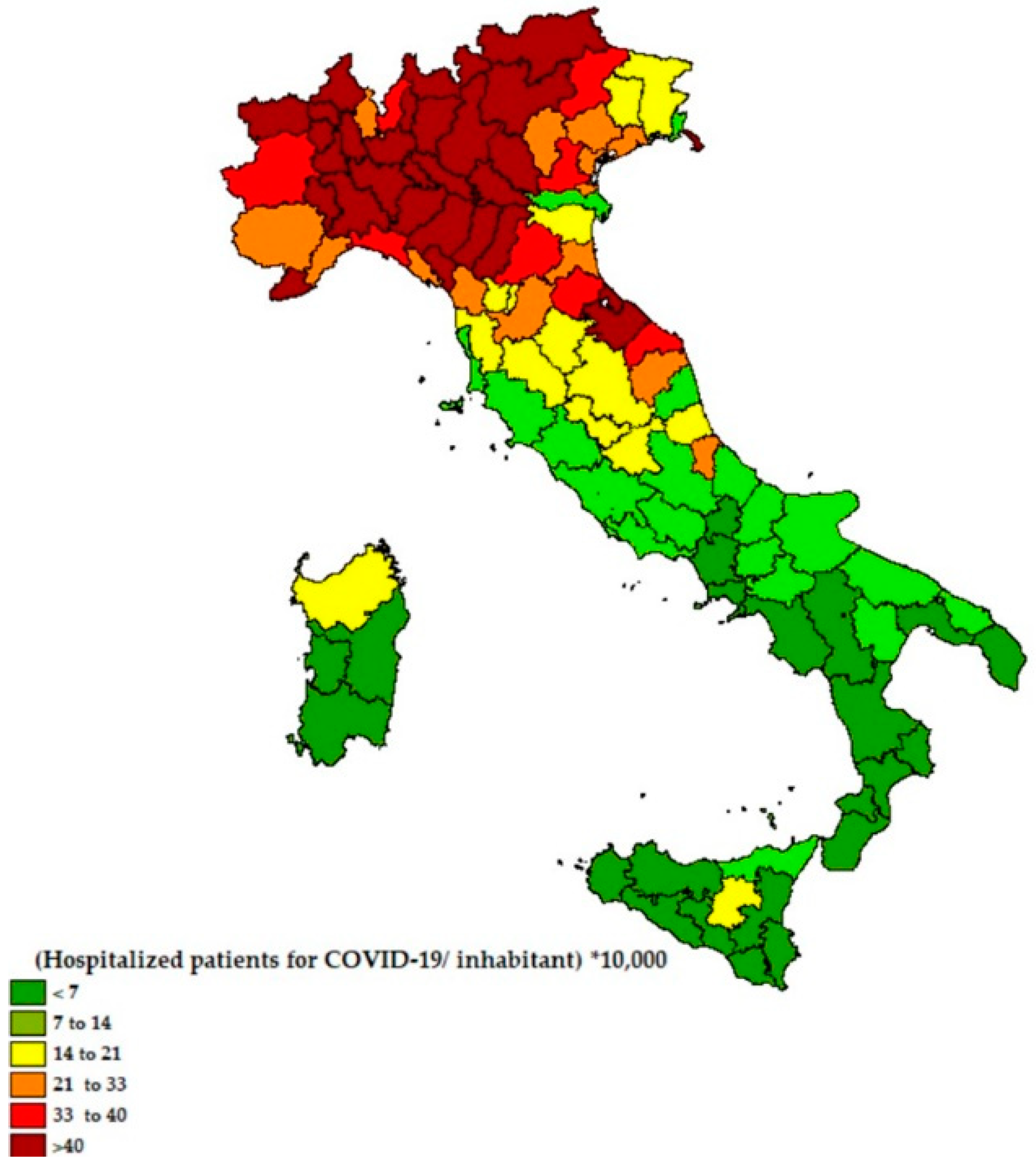
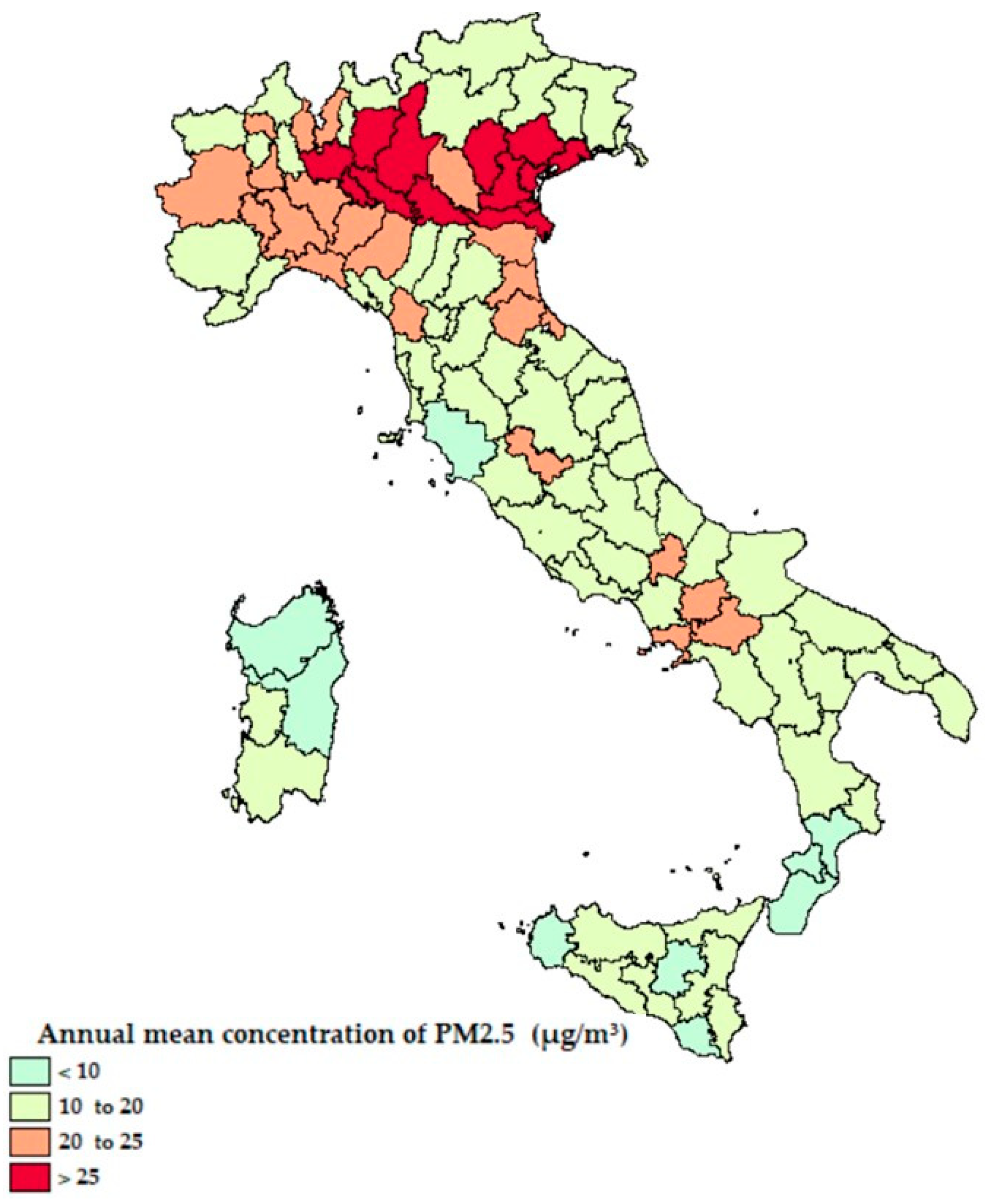
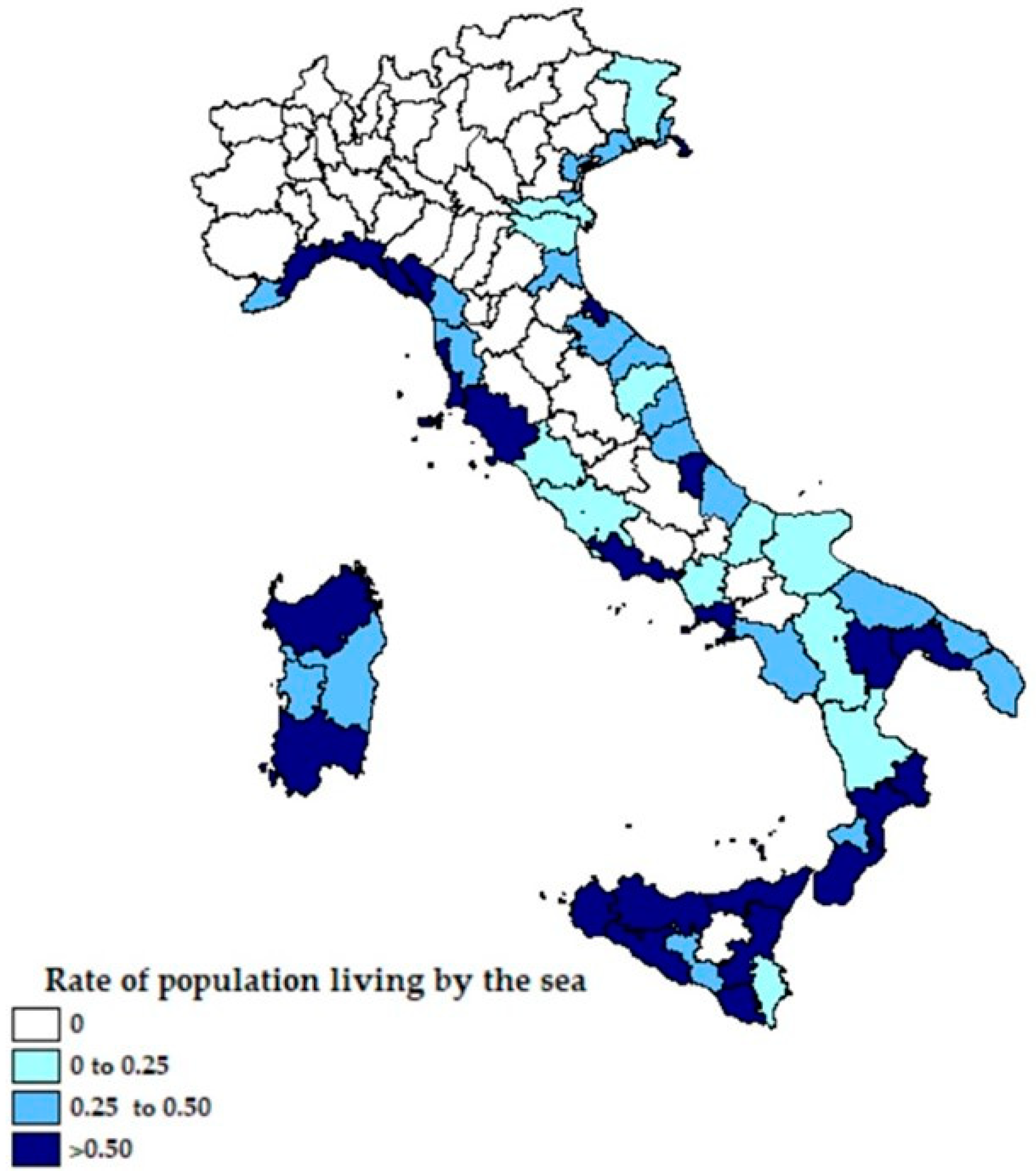
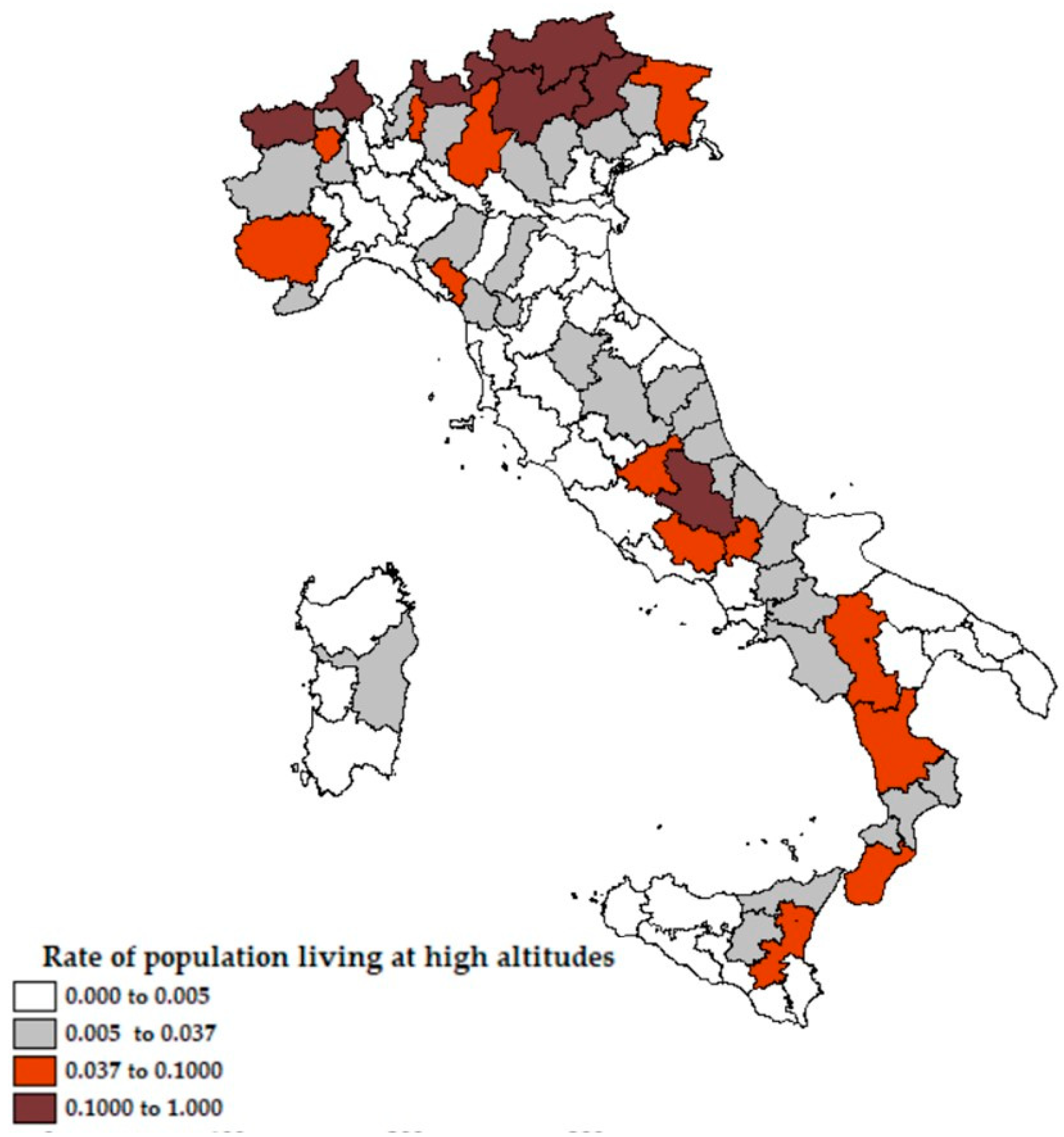
2. The Case Study and the Methodology Proposed
+ β4 ∗ SEA EXPRE RATEi + β5 ∗ GREEN RATEi
PM2.5i + β4 ∗ SEA EXPRE RATEi + β5 ∗ GREEN RATEi
+ β6 ∗ ALTITUDE RATEi
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020, 395, 565–574. [Google Scholar] [CrossRef]
- Contini, D.; Costabile, F.; Wang, A. Does Air Pollution Influence COVID-19 Outbreaks? Atmosphere 2020, 11, 377. [Google Scholar] [CrossRef]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, X.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Ciencewicki, J.; Jaspers, I. Air Pollution and Respiratory Viral Infection. Inhal. Toxicol. 2007, 19, 1135–1146. [Google Scholar] [CrossRef] [PubMed]
- Stieb, D.M.; Szyszkowicz, M.; Rowe, B.H.; Leech, J.A. Air pollution and emergency department visits for cardiac and respiratory conditions: A multi-city time-series analysis. Environ. Health 2009, 8, 25. [Google Scholar] [CrossRef]
- Faustini, A.; Stafoggia, M.; Colais, P.; Berti, G.; Bisanti, L.; Cadum, E.; Cernigliaro, A.; Mallone, S.; Scarnato, C.; Forastiere, F. Air pollution and multiple acute respiratory outcomes. Eur. Respir. J. 2013, 42, 304–313. [Google Scholar] [CrossRef]
- Ortiz, C.; Linares, C.; Carmona, R.; Díaz, J. Evaluation of short-term mortality attributable to particulate matter pollution in Spain. Environ. Pollut. 2017, 224, 541–551. [Google Scholar] [CrossRef]
- Anderson, J.O.; Thundiyil, J.G.; Stolbach, A. Clearing the Air: A Review of the Effects of Particulate Matter Air Pollution on Human Health. J. Med. Toxicol. 2011, 8, 166–175. [Google Scholar] [CrossRef]
- Dominici, F.; Peng, R.D.; Bell, M.L.; Pham, L.; McDermott, A.; Zeger, S.L.; Samet, J.M. Fine Particulate Air Pollution and Hospital Admission for Cardiovascular and Respiratory Diseases. JAMA 2006, 295, 1127–1134. [Google Scholar] [CrossRef]
- Schlesinger, R.B.; Cassee, F. Atmospheric Secondary Inorganic Particulate Matter: The Toxicological Perspective as a Basis for Health Effects Risk Assessment. Inhal. Toxicol. 2003, 15, 197–235. [Google Scholar] [CrossRef]
- Sedlmaier, N.; Hoppenheidt, K.; Krist, H.; Lehmann, S.; Lang, H.; Büttner, M. Generation of avian influenza virus (AIV) contaminated fecal fine particulate matter (PM2.5): Genome and infectivity detection and calculation of immission. Vet. Microbiol. 2009, 139, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Setti, L.; Passarini, F.; de Gennaro, G.; Di Gilio, A.; Palmisani, J.; Buono, P.; Fornari, G.; Perrone, M.G.; Piazzalunga, A.; Barbieri, P.; et al. Relazione Sull’individuazione Dell’inquinamento da Particolato Atmosferico e Diffusione Divirus Nella Popolazione; Position Paper; APE: Milano, Italy, 2020. [Google Scholar]
- Bontempi, E. First data analysis about possible COVID-19 virus airborne diffusion due to air particulate matter (PM): The case of Lombardy (Italy). Environ. Res. 2020, 186, 109639. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Nethery, R.C.; Sabath, M.B.; Braun, D.; Dominici, F. Exposure to air pollution and COVID-19 mortality in the United States. medRxiv 2020. Preprint. [Google Scholar]
- Fattorini, D.; Regoli, F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ. Pollut. 2020, 264, 114732. [Google Scholar] [CrossRef]
- Conticini, E.; Frediani, B.; Caro, D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020, 261, 114465. [Google Scholar] [CrossRef]
- Manigrasso, M.; Abballe, F.; Jack, R.F.; Avino, P. Time-Resolved Measurement of the Ionic Fraction of Atmospheric Fine Particulate Matter. J. Chromatogr. Sci. 2010, 48, 549–552. [Google Scholar] [CrossRef]
- Li, M.; Hu, M.; Du, B.; Guo, Q.; Tan, T.; Zheng, J.; Huang, X.; He, L.; Wu, Z.; Guo, S. Temporal and spatial distribution of PM2.5 chemical composition in a coastal city of Southeast China. Sci. Total Environ. 2017, 605, 337–346. [Google Scholar] [CrossRef]
- White, M.P.; Alcock, I.; Wheeler, B.W.; Depledge, M.H. Coastal proximity, health and well-being: Results from a longitudinal panel survey. Health Place 2013, 23, 97–103. [Google Scholar] [CrossRef]
- Brereton, F.; Clinch, J.P.; Ferreira, S. Happiness, geography and the environment. Ecol. Econ. 2008, 65, 386–396. [Google Scholar] [CrossRef]
- Van Acker, E.; De Rijcke, M.; Asselman, J.; Beck, I.M.; Huysman, S.; Vanhaecke, L.; De Schamphelaere, K.A.C.; Janssen, C.R. Aerosolizable Marine Phycotoxins and Human Health Effects: In Vitro Support for the Biogenics Hypothesis. Mar. Drugs 2020, 18, 46. [Google Scholar] [CrossRef]
- Grant, W.B.; Cross, H.S.; Garland, C.F.; Gorham, E.D.; Moan, J.; Peterlik, M.; Porojnicu, A.C.; Reichrath, J.; Zittermann, A. Estimated benefit of increased vitamin D status in reducing the economic burden of disease in western Europe. Prog. Biophys. Mol. Biol. 2009, 99, 104–113. [Google Scholar] [CrossRef]
- Melillo, J.; Osvaldo, S. Sustaining Life: How Human Health Depends on Biodiversity; Oxford University Press: New York, NY, USA, 2008. [Google Scholar]
- Newman, D.J.; Kilama, J.; Bernstein, A.; Chivian, E. Medicines from nature. In Sustaining Life: How Human Health Depends on Biodiversity; Chivian, E., Bernstein, A., Eds.; Oxford University Press: New York, NY, USA, 2008. [Google Scholar]
- Pandey, P.K. Endangered medicinal species of the Indian Ocean: Radical need for conservation. Chem. Biodivers. 2009, 6, 990–1001. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Liu, X.; Yang, X.; Zou, B.; Wang, J. Spatial variations of PM2. 5 in Chinese cities for the joint impacts of human activities and natural conditions: A global and local regression perspective. J. Clean. Prod. 2018, 203, 143–152. [Google Scholar] [CrossRef]
- Zhang, H.; Wang, Z.; Zhang, W. Exploring spatiotemporal patterns of PM2. 5 in China based on ground-level observations for 190 cities. Environ. Pollut. 2016, 216, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Zhang, H.; Yang, Y.; Wan, H.; Wang, Y. Impacts of geographic factors and population density on the COVID-19 spreading under the lockdown policies of China. Sci. Total Environ. 2020, 746, 141347. [Google Scholar] [CrossRef] [PubMed]
- Arias-Reyes, C.; Zubieta-DeUrioste, N.; Poma-Machicao, L.; Aliaga-Raudan, F.; Carvajal-Rodriguez, F.; Dutschmann, M.; Soliz, J. Does the pathogenesis of SAR-CoV-2 virus decrease at high-altitude? Respir. Physiol. Neurobiol. 2020, 277, 103443. [Google Scholar] [CrossRef]
- Huamaní, C.; Velásquez, L.; Montes, S.; Miranda-Solis, F. Propagation by COVID-19 at high altitude: Cusco case. Respir. Physiol. Neurobiol. 2020, 279, 103448. [Google Scholar] [CrossRef]
- Xi, A.; Zhuo, M.; Dai, J.; Ding, Y.; Ma, X.; Ma, X.; Nuermberger, E. Epidemiological and clinical characteristics of discharged patients infected with SARS-CoV-2 on the Qinghai plateau. J. Med. Virol. 2020, 92, 2528–2535. [Google Scholar] [CrossRef]
- Zeng, J.; Peng, S.; Lei, Y.; Huang, J.; Guo, Y.; Zhang, X.; Pan, L. Clinical and Imaging features of COVID-19 Patients: Analysis of Data from High-Altitude Areas. J. Infect. 2020, 80, e34–e36. [Google Scholar] [CrossRef]
- Quevedo-Ramírez, A.; Al-Kassab-Córdova, A.; Mendez-Guerra, C.; Cornejo-Venegas, G.; Alva-Chavez, K.P. Altitude and excess mortality during COVID-19 pandemic in Peru. Respir. Physiol. Neurobiol. 2020, 281, 103512. [Google Scholar] [CrossRef]
- Segovia-Juarez, J.; Castagnetto, J.M.; Gonzales, G.F. High altitude reduces infection rate of COVID-19 but not case-fatality rate. Respir. Physiol. Neurobiol. 2020, 281, 103494. [Google Scholar] [CrossRef] [PubMed]
- Pun, M.; Turner, R.; Strapazzon, G.; Brugger, H.; Swenson, E.R. Lower Incidence of COVID-19 at High Altitude: Facts and Confounders. High Alt. Med. Biol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Woolcott, O.O.; Bergman, R.N. Mortality attributed to COVID-19 in high-altitude populations. High Alt. Med. Biol. 2020. [Google Scholar] [CrossRef]
- Cartenì, A.; Di Francesco, L.; Martino, M. How mobility habits influenced the spread of the COVID-19 pandemic: Results from the Italian case study. Sci. Total Environ. 2020, 741, 140489. [Google Scholar] [CrossRef] [PubMed]
- Cartenì, A.; Di Francesco, L.; Martino, M. The role of transport accessibility within the spread of the Coronavirus pandemic in Italy. Saf. Sci. 2020, 133, 104999. [Google Scholar] [CrossRef] [PubMed]
- Coker, E.S.; Cavalli, L.; Fabrizi, E.; Guastella, G.; Lippo, E.; Parisi, M.L.; Pontarollo, N.; Rizzati, M.; Varacca, A.; Vergalli, S. The effects of air pollution on COVID-19 related mortality in northern Italy. Environ. Resour. Econ. 2020, 76, 611–634. [Google Scholar] [CrossRef] [PubMed]
- Bowe, B.; Xie, Y.; Yan, Y.; Al-Aly, Z. Burden of Cause-Specific Mortality Associated With PM 2.5 Air Pollution in the United States. JAMA Netw. Open 2019, 2, e1915834. [Google Scholar] [CrossRef]
- Garg, S.; Kim, L.; Whitaker, M.; O’Halloran, A.; Cummings, C.; Holstein, R.; Prill, M.; Chai, S.J.; Kirley, P.D.; Alden, N.B.; et al. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019—COVID-NET, 14 States, March 1–30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 458–464. [Google Scholar] [CrossRef]
- Ezzati, M.; Horwitz, M.E.M.; Thomas, D.S.K.; Friedman, A.B.; Roach, R.; Clark, T.; Murray, C.J.L.; Honigman, B. Altitude, life expectancy and mortality from ischaemic heart disease, stroke, COPD and cancers: National population-based analysis of US counties. J. Epidemiol. Community Health 2011. [Google Scholar] [CrossRef]
| Variables | Min | Avg | Max |
|---|---|---|---|
| COVID Diffusion (0, 1) | +0.049 | +0.144 | +0.530 |
| Pop. over 50 rate (0, 1) | +0.346 | +0.394 | +0.435 |
| PM2.5 (µg/m3) | +6 | +17.538 | +30 |
| Sea Expre Rate (0, 1) | +0 | +0.241 | +0.961 |
| Green Rate (mq/citizen) | +1.19 | +68.28 | +667.05 |
| Altitude Rate (0, 1) | +0.0 | +0.037 | +0.570 |
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| Estimation | Non Robust Standard Error | t- Value | Estimation | Non Robust Standard Error | t- Value | |
| β0 | −0.775 | 0.308 | −2.515 | −0.859 | 0.333 | −2.580 |
| β1 | 6.987 | 0.785 | 8.900 | 6.754 | 0.784 | 8.619 |
| β2 | 2.777 | 1.013 | 2.742 | 2.492 | 0.931 | 2.676 |
| β3 | 0.0471 | 0.009 | 5.284 | 0.055 | 0.010 | 5.734 |
| β4 | −0.168 | 0.063 | −2.669 | −0.026 | 0.012 | −2.200 |
| β5 | −0.0005 | 0.000 | −2.746 | −0.0004 | 0.000 | −2.704 |
| β6 | 1.2556 | 0.694 | 1.81 | |||
| Residual Sum of Squares | 22.626 | 21.628 | ||||
| Adj. R-Squared | 0.646 | 0.657 | ||||
| F-statistic | 29.088 on 5 and 72 | 25.552 on 6 and 71 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cascetta, E.; Henke, I.; Di Francesco, L. The Effects of Air Pollution, Sea Exposure and Altitude on COVID-19 Hospitalization Rates in Italy. Int. J. Environ. Res. Public Health 2021, 18, 452. https://doi.org/10.3390/ijerph18020452
Cascetta E, Henke I, Di Francesco L. The Effects of Air Pollution, Sea Exposure and Altitude on COVID-19 Hospitalization Rates in Italy. International Journal of Environmental Research and Public Health. 2021; 18(2):452. https://doi.org/10.3390/ijerph18020452
Chicago/Turabian StyleCascetta, Ennio, Ilaria Henke, and Luigi Di Francesco. 2021. "The Effects of Air Pollution, Sea Exposure and Altitude on COVID-19 Hospitalization Rates in Italy" International Journal of Environmental Research and Public Health 18, no. 2: 452. https://doi.org/10.3390/ijerph18020452
APA StyleCascetta, E., Henke, I., & Di Francesco, L. (2021). The Effects of Air Pollution, Sea Exposure and Altitude on COVID-19 Hospitalization Rates in Italy. International Journal of Environmental Research and Public Health, 18(2), 452. https://doi.org/10.3390/ijerph18020452






