Hyperbaric Oxygen Therapy and A-PRF Pre-Treated Implants in Severe Periodontitis: A Case Report
Abstract
1. Introduction
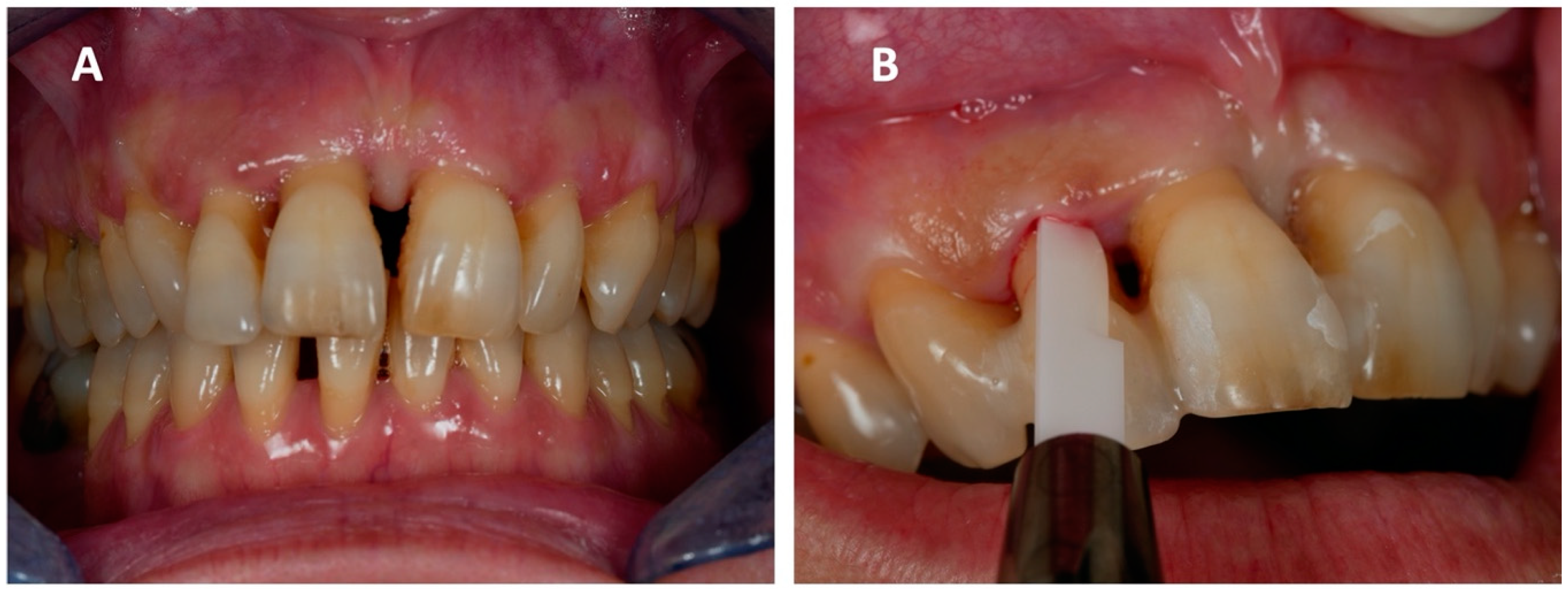
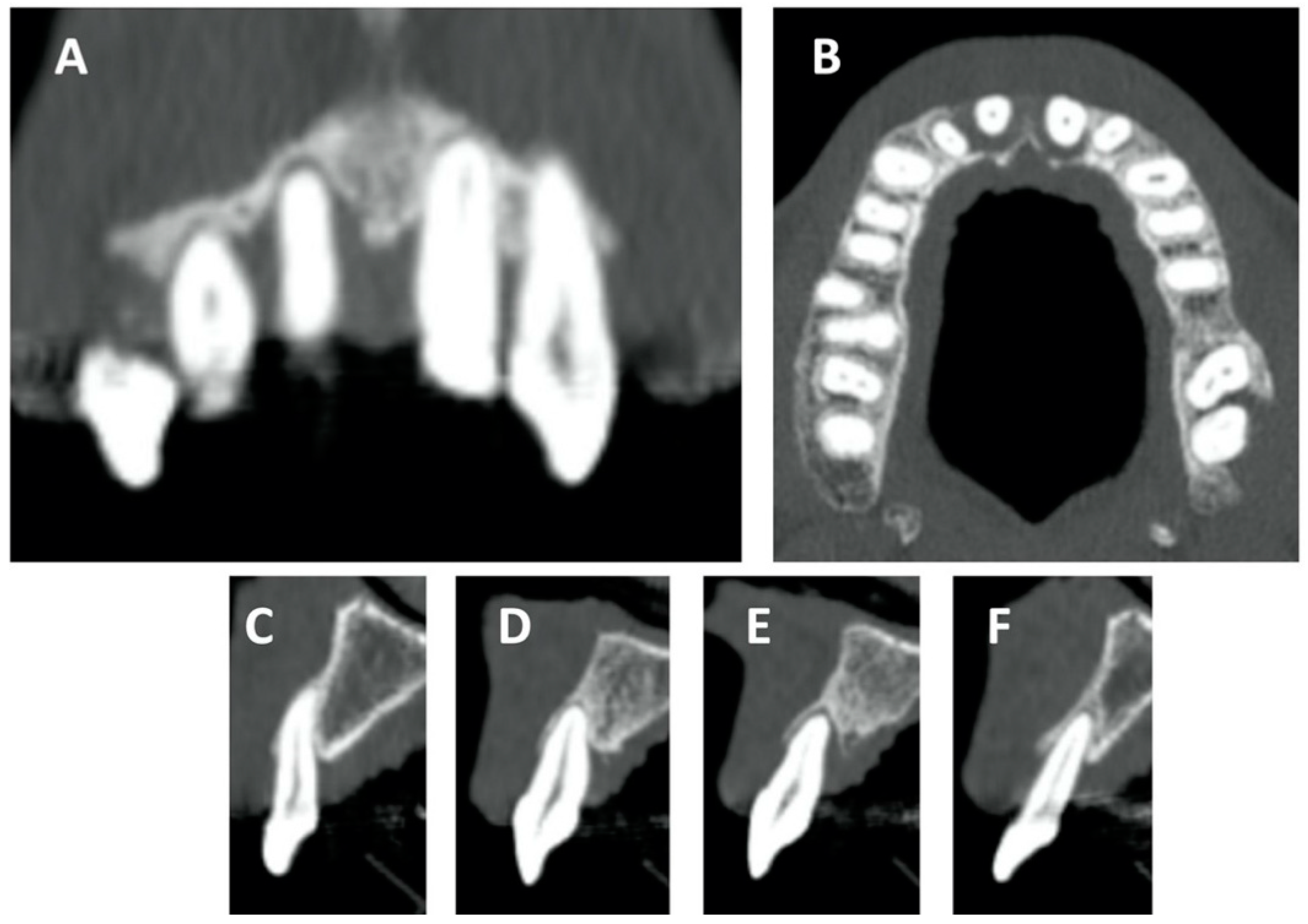
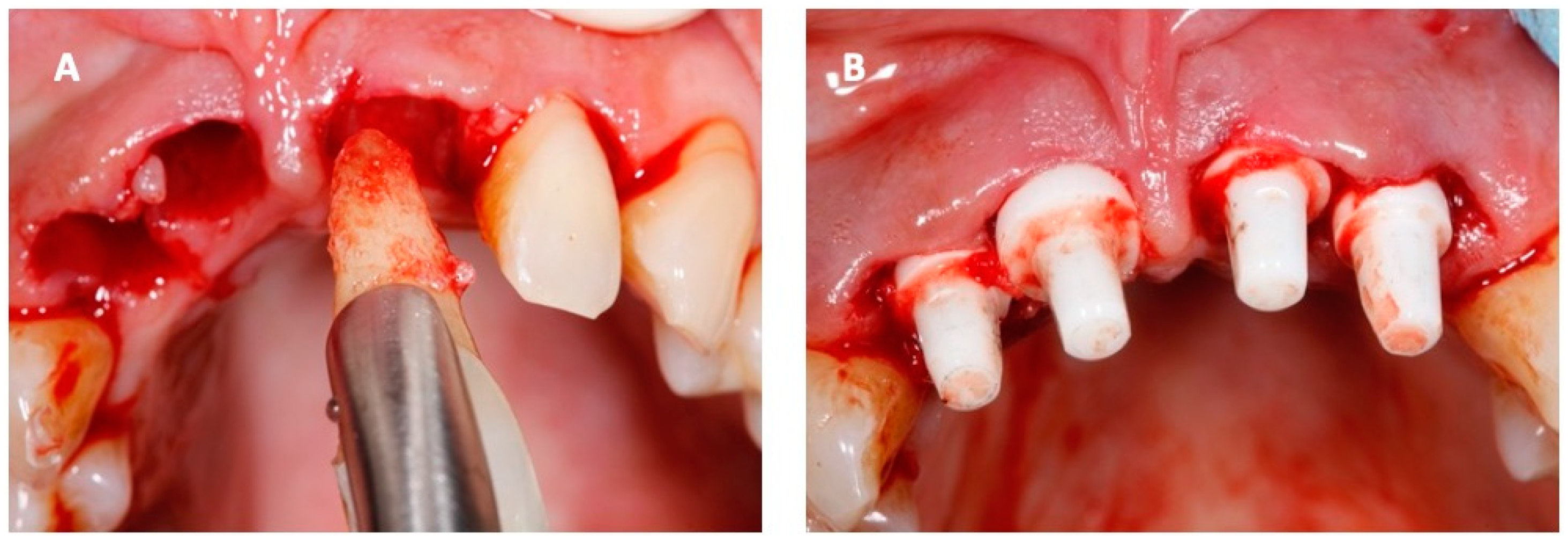
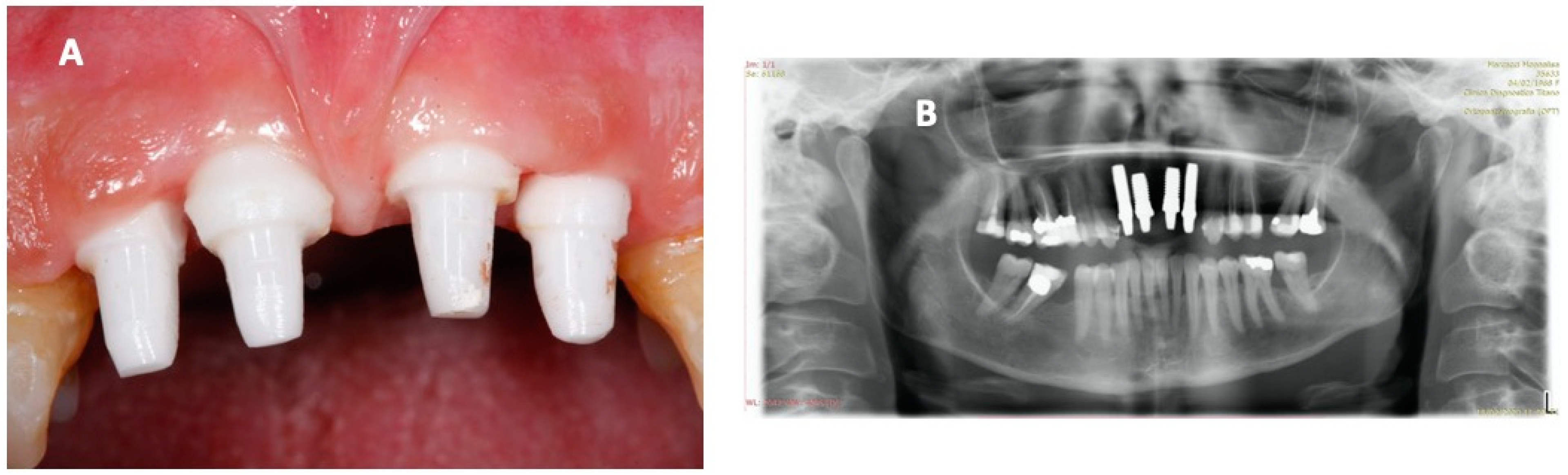
2. Case Report
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Camporesi, E.M.; Bosco, G. Mechanisms of action of hyperbaric oxygen therapy. Undersea Hyperb. Med. 2014, 41, 247–252. [Google Scholar] [PubMed]
- Thom, S.R. Hyperbaric oxygen: Its mechanisms and efficacy. Plast. Reconstr. Surg. 2011, 127 (Suppl. 1), 131S. [Google Scholar] [CrossRef] [PubMed]
- Kranke, P.; Bennett, M.H.; James, M.M.-S.; Schnabel, A.E.; Debus, S.; Weibel, S. Hyperbaric oxygen therapy for chronic wounds. Cochrane Database Syst. Rev. 2015, 2015, CD004123. [Google Scholar] [CrossRef] [PubMed]
- Hexdall, E.; Brave, R.; Kraft, K.; Siewers, J. Diving deep into hyperbaric oxygen therapy. Nursing2019 2016, 46, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Vatansever, F.; de Melo, W.C.M.A.; Avci, P.; Vecchio, D.; Sadasivam, M.; Gupta, A.; Chandran, R.; Karimi, M.; Parizotto, N.A.; Yin, R.; et al. Antimicrobial strategies centered around reactive oxygen species—Bactericidal antibiotics, photody-namic therapy, and beyond. FEMS Microbiol. Rev. 2013, 37, 955–989. [Google Scholar] [CrossRef]
- de Smet, G.H.J.; Kroese, L.F.; Menon, A.G.; Jeekel, J.; van Pelt, A.W.J.; Kleinrensink, G.J.; Lange, J.F. Oxygen therapies and their effects on wound healing. Wound Repair Regen. 2017, 25, 591–608. [Google Scholar] [CrossRef]
- Gardin, C.; Bosco, G.; Ferroni, L.; Quartesan, S.; Rizzato, A.; Tatullo, M.; Zavan, B. Hyperbaric oxygen therapy improves the osteo-genic and vasculogenic properties of mesenchymal stem cells in the presence of inflammation in vitro. Int. J. Mol. Sci. 2020, 21, 1452. [Google Scholar] [CrossRef]
- Bosco, G.; Vezzani, G.; Sposta, S.M.; Rizzato, A.; Enten, G.; Abou-Samra, A.; Malacrida, S.; Quartesan, S.; Vezzoli, A.; Camporesi, E. Hyperbaric oxygen therapy ameliorates osteonecrosis in patients by modulating inflammation and oxidative stress. J. Enzym. Inhib. Med. Chem. 2018, 33, 1501–1505. [Google Scholar] [CrossRef]
- Bosco, G.; Vezzani, G.; Enten, G.; Manelli, D.; Rao, N.; Camporesi, E. Femoral condylar necrosis: Treatment with hyperbaric oxygen therapy. Arthroplast. Today 2018, 4, 510–515. [Google Scholar] [CrossRef]
- Re, K.; Patel, S.; Gandhi, J.; Suh, Y.; Reid, I.; Joshi, G.; Smith, N.L.; Khan, S.A. Clinical utility of hyperbaric oxygen therapy in dentistry. Med. Gas Res. 2019, 9, 93–100. [Google Scholar] [CrossRef]
- Marx, R.E. A new concept in the treatment of osteoradionecrosis. J. Oral Maxillofac. Surg. 1983, 41, 351–357. [Google Scholar] [CrossRef]
- Pedersen, T.O.; Xing, Z.; Finne-Wistrand, A.; Hellem, S.; Mustafa, K. Hyperbaric oxygen stimulates vascularization and bone formation in rat calvarial defects. Int. J. Oral Maxillofac. Surg. 2013, 42, 907–914. [Google Scholar] [CrossRef]
- Park, K.-M.; Kim, C.; Park, I.; Park, Y.B.; Chung, M.-K.; Kim, S. Bone Regeneration Effect of Hyperbaric Oxygen Therapy Duration on Calvarial Defects in Irradiated Rats. BioMed Res. Int. 2019, 2019, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, P.A.D.; Oliveira, A.M.S.D.; Pablos, A.B.; Costa, F.O.; Silva, G.A.B.; Dos Santos, J.N.; Cury, P.R. Influence of hyperbaric oxygen therapy on peri-implant bone healing in rats with alloxan-induced diabetes. J. Clin. Periodontol. 2012, 39, 879–886. [Google Scholar] [CrossRef] [PubMed]
- Altug, H.A.; Tatli, U.; Coskun, A.T.; Erdogan, Ö.; Özkan, A.; Sencimen, M.; Kürkçü, M. Effects of hyperbaric oxygen treatment on implant osseointegration in experimental diabetes mellitus. J. Appl. Oral Sci. 2018, 26, e20180083. [Google Scholar] [CrossRef]
- KV, G.; Komala, J.; Mohsin, A.H.; Ahmed, M.A.; Sairam, G.; Sheethi, K.V. A study to evaluate the effect of hyperbaric oxygen on osseointegration of root-form endosseous titanium dental implants: An in vivo study. J. Contemp. Dent. Pract. 2019, 20, 460–465. [Google Scholar]
- Abdel-Bary, S.K.; El Dakrory, U.A. Effect of Hyperbaric Oxygen Therapy on the Osseointegration around Implants after Man-dibular Reconstruction by Destraction Osteogenesis. Undersea Hyperb. Med. 2017, 44, 357–364. [Google Scholar]
- Laudenbach, J.M.; Simon, Z. Common Dental and Periodontal Diseases: Evaluation and Management. Med. Clin. N. Am. 2014, 98, 1239–1260. [Google Scholar] [CrossRef]
- Wandawa, G.; Mustaqimah, D.N.; Sidik, S.; Saraswati, H.; Putri, F.A.; Auerkari, E.I. Efficacy of hyperbaric oxygen therapy as an ad-junctive therapy of chronic periodontitis. J. Int. Dent. Med. Res. 2017, 10, 72–75. [Google Scholar]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S173–S182. [Google Scholar] [CrossRef]
- Highfield, J. Diagnosis and classification of periodontal disease. Aust. Dent. J. 2009, 54, S11–S26. [Google Scholar] [CrossRef] [PubMed]
- Kullar, A.S.; Miller, C. Are There Contraindications for Placing Dental Implants? Dent. Clin. N. Am. 2019, 63, 345–362. [Google Scholar] [CrossRef]
- Mathieu, D.; Marroni, A.; Kot, J. Tenth european consensus conference on hyperbaric medicine: Recommendations for accepted and non-accepted clinical indications and practice of hyperbaric oxygen treatment. Diving Hyperb. Med. 2017, 47, 24–31. [Google Scholar] [CrossRef]
- Mountziaris, P.M.; Mikos, A.G. Modulation of the Inflammatory Response for Enhanced Bone Tissue Regeneration. Tissue Eng. Part B Rev. 2008, 14, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Al Hadi, H.; Smerdon, G.R.; Fox, S.W. Hyperbaric oxygen therapy accelerates osteoblast differentiation and promotes bone formation. J. Dent. 2015, 43, 382–388. [Google Scholar] [CrossRef]
- Zhang, Q.; Chen, B.; Zhu, D.; Yan, F. Biomarker levels in gingival crevicular fluid of subjects with different periodontal conditions: A cross-sectional study. Arch. Oral Biol. 2016, 72, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.L.; Xu, B.; Liu, J.C.; Li, S.G.; Li, D.Y.; Gong, G.C.; Wu, Z.F.; Lin, S.L.; Zhou, Y.J. Effects of hyperbaric oxygen on aggressive periodontitis and subgingival anaerobes in Chinese patients. J. Indian Soc. Periodontol. 2012, 16, 492–497. [Google Scholar] [CrossRef]
- Deepa, D.; Jain, N. Applications of hyperbaric oxygen therapy in dentistry: A mini review. J. Interdiscip. Dent. 2014, 4, 27. [Google Scholar] [CrossRef]
- Lombardo, G.; Pardo, A.; Signoretto, C.; Signoriello, A.; Simeoni, E.; Rovera, A.; Nocini, P.F. Hyperbaric oxygen therapy for the treatment of moderate to severe periodontitis: A clinical pilot study. Undersea Hyperb. Med. 2020, 571–580. [Google Scholar] [CrossRef]
- Kaide, C.G.; Khandelwal, S. Hyperbaric Oxygen: Applications in Infectious Disease. Emerg. Med. Clin. N. Am. 2008, 26, 571–595. [Google Scholar] [CrossRef]
- Marmo, M.; Villani, R.; Di Minno, R.M.; Noschese, G.; Paganini, M.; Quartesan, S.; Rizzato, A.; Bosco, G. Cave canem: HBO2 therapy efficacy on Capnocytophaga canimorsus infections: A case series. Undersea Hyperb. Med. 2017, 44, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Park, M.K.; Muhvich, K.H.; Myers, R.A.M.; Marzella, L. Hyperoxia prolongs the aminoglycoside-induced postantibiotic effect in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 1991, 35, 691–695. [Google Scholar] [CrossRef] [PubMed]
- Morabito, C.; Bosco, G.; Pilla, R.; Corona, C.; Mancinelli, R.; Yang, Z.; Camporesi, E.M.; Fanò, G.; Mariggiò, M.A. Effect of pre-breathing oxygen at different depth on oxidative status and calcium concentration in lymphocytes of scuba divers. Acta Physiol. 2011, 202, 69–78. [Google Scholar] [CrossRef]
- Crabbé, A.; Jensen, P.Ø.; Bjarnsholt, T.; Coenye, T. Antimicrobial Tolerance and Metabolic Adaptations in Microbial Biofilms. Trends Microbiol. 2019, 27, 850–863. [Google Scholar] [CrossRef] [PubMed]
- Møller, S.A.; Jensen, P.O.; Høiby, N.; Ciofu, O.; Kragh, K.N.; Bjarnsholt, T.; Kolpen, M. Hyperbaric oxygen treatment increases killing of aggregating Pseudomonas aeruginosa isolates from cystic fibrosis patients. J. Cyst. Fibros. 2019, 18, 657–664. [Google Scholar] [CrossRef]
- Gade, P.A.V.; Olsen, T.B.; Jensen, P.O.; Kolpen, M.; Høiby, N.; Henneberg, K.Å.; Sams, T. Modelling of ciprofloxacin killing enhanced by hyperbaric oxygen treatment in Pseudomonas aeruginosa PAO1 biofilms. PLoS ONE 2018, 13, e0198909. [Google Scholar] [CrossRef]
- Memar, M.Y.; Ghotaslou, R.; Samiei, M.; Adibkia, K. Antimicrobial use of reactive oxygen therapy: Current insights. Infect. Drug Resist. 2018, 11, 567–576. [Google Scholar] [CrossRef]
- Sanford, N.E.; Wilkinson, J.E.; Nguyen, H.; Diaz, G.; Wolcott, R. Efficacy of hyperbaric oxygen therapy in bacterial biofilm eradication. J. Wound Care 2018, 27, S20–S28. [Google Scholar] [CrossRef]
- Marx, R.E.; Ames, J.R. The use of hyperbaric oxygen therapy in bony reconstruction of the irradiated and tissue-deficient patient. J. Oral Maxillofac. Surg. 1982, 40, 412–420. [Google Scholar] [CrossRef]
- Marx, R.E.; Johnson, R.P.; Kline, S.N. Prevention of osteoradionecrosis: A randomized prospective clinical trial of hyperbaric oxygen versus penicillin. J. Am. Dent. Assoc. 1985, 111, 49–54. [Google Scholar] [CrossRef]
- Bennett, M.; Feldmeier, J.; Hampson, N.B.; Smee, R.; Milross, C. Hyperbaric oxygen therapy for late radiation tissue injury. Cochrane Database Syst. Rev. 2016, 2016, CD005005. [Google Scholar] [CrossRef] [PubMed]
- Bosco, G.; Camporesi, E.M. Hyperbaric oxygen pretreatment and preconditioning. Undersea Hyperb. Med. 2014, 41, 541–544. [Google Scholar] [CrossRef]
- Bethke, A.; Pieralli, S.; Kohal, R.J.; Burkhardt, F.; von Stein-Lausnitz, M.; Vach, K.; Spies, B.C. Fracture resistance of zirconia oral implants in vitro: A systematic review and meta-analysis. Materials 2020, 13, 562. [Google Scholar] [CrossRef] [PubMed]
- Adánez, M.H.; Nishihara, H.; Att, W. A systematic review and meta-analysis on the clinical outcome of zirconia implant–restoration complex. J. Prosthodont. Res. 2018, 62, 397–406. [Google Scholar] [CrossRef]
- Obradovic-Djuricic, K.; Medic, V.; Dodic, S.; Gavrilov, D.; Antonijevic, D.; Zrilic, M. Dilemmas in zirconia bonding: A review. Srpski Arhiv za Celokupno Lekarstvo 2013, 141, 395–401. [Google Scholar] [CrossRef]
- Van Hinsbergh, V.W.M.; Collen, A.; Koolwijk, P. Role of fibrin matrix in angiogenesis. Ann. N. Y. Acad. Sci. 2001, 936, 426–437. [Google Scholar] [CrossRef]
- Del Corso, M.; Vervelle, A.; Simonpieri, A.; Jimbo, R.; Inchingolo, F.; Sammartino, G.; M Dohan Ehrenfest, D. Current Knowledge and Perspectives for the Use of Platelet-Rich Plasma (PRP) and Platelet-Rich Fibrin (PRF) in Oral and Maxillofacial Surgery Part 1: Periodontal and Dentoalveolar Surgery. Curr. Pharm. Biotechnol. 2012, 13, 1207–1230. [Google Scholar] [CrossRef]
- Mostafa, D.; Aboushelib, M.N. Bioactive-hybrid-zirconia implant surface for enhancing osseointegration: An in vivo study. Int. J. Implant Dent. 2018, 4, 20. [Google Scholar] [CrossRef]
- Kämmerer, P.W.; Schiegnitz, E.; Palarie, V.; Dau, M.; Frerich, B.; Al-Nawas, B. Influence of platelet-derived growth factor on osse-ous remodeling properties of a variable-thread tapered dental implant in vivo. Clin. Oral Implant. Res. 2017, 28, 201–206. [Google Scholar] [CrossRef]
- Santana, R.B.; Santana, C.M.; Dibart, S. Platelet-Derived Growth Factor-Mediated Guided Bone Regeneration in Immediate Implant Placement in Molar Sites with Buccal Bone Defects. Int. J. Periodontics Restor. Dent. 2015, 35, 825–833. [Google Scholar] [CrossRef]
- Miron, R.J.; Zucchelli, G.; Pikos, M.A.; Salama, M.; Lee, S.; Guillemette, V.; Fujioka-Kobayashi, M.; Bishara, M.; Zhang, Y.; Wang, H.-L.; et al. Use of platelet-rich fibrin in regenerative dentistry: A systematic review. Clin. Oral Investig. 2017, 21, 1913–1927. [Google Scholar] [CrossRef] [PubMed]
- Pitzurra, L.; Jansen, I.D.C.; De Vries, T.J.; Hoogenkamp, M.A.; Loos, B.G. Effects of L-PRF and A-PRF+ on periodontal fibroblasts in in vitro wound healing experiments. J. Periodontal Res. 2020, 55, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Chai, J.; Fujioka-Kobayashi, M.; Sculean, A.; Zhang, Y. Evaluation of 24 protocols for the production of platelet-rich fibrin. BMC Oral Health 2020, 20, 1–13. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giacon, T.A.; Giancola, F.; Paganini, M.; Tiengo, C.; Camporesi, E.M.; Bosco, G. Hyperbaric Oxygen Therapy and A-PRF Pre-Treated Implants in Severe Periodontitis: A Case Report. Int. J. Environ. Res. Public Health 2021, 18, 413. https://doi.org/10.3390/ijerph18020413
Giacon TA, Giancola F, Paganini M, Tiengo C, Camporesi EM, Bosco G. Hyperbaric Oxygen Therapy and A-PRF Pre-Treated Implants in Severe Periodontitis: A Case Report. International Journal of Environmental Research and Public Health. 2021; 18(2):413. https://doi.org/10.3390/ijerph18020413
Chicago/Turabian StyleGiacon, Tommaso Antonio, Franco Giancola, Matteo Paganini, Cesare Tiengo, Enrico M. Camporesi, and Gerardo Bosco. 2021. "Hyperbaric Oxygen Therapy and A-PRF Pre-Treated Implants in Severe Periodontitis: A Case Report" International Journal of Environmental Research and Public Health 18, no. 2: 413. https://doi.org/10.3390/ijerph18020413
APA StyleGiacon, T. A., Giancola, F., Paganini, M., Tiengo, C., Camporesi, E. M., & Bosco, G. (2021). Hyperbaric Oxygen Therapy and A-PRF Pre-Treated Implants in Severe Periodontitis: A Case Report. International Journal of Environmental Research and Public Health, 18(2), 413. https://doi.org/10.3390/ijerph18020413








