Irrational Beliefs about COVID-19: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy and Data Sources
2.2. Inclusion Criteria
2.3. Exclusion Criteria
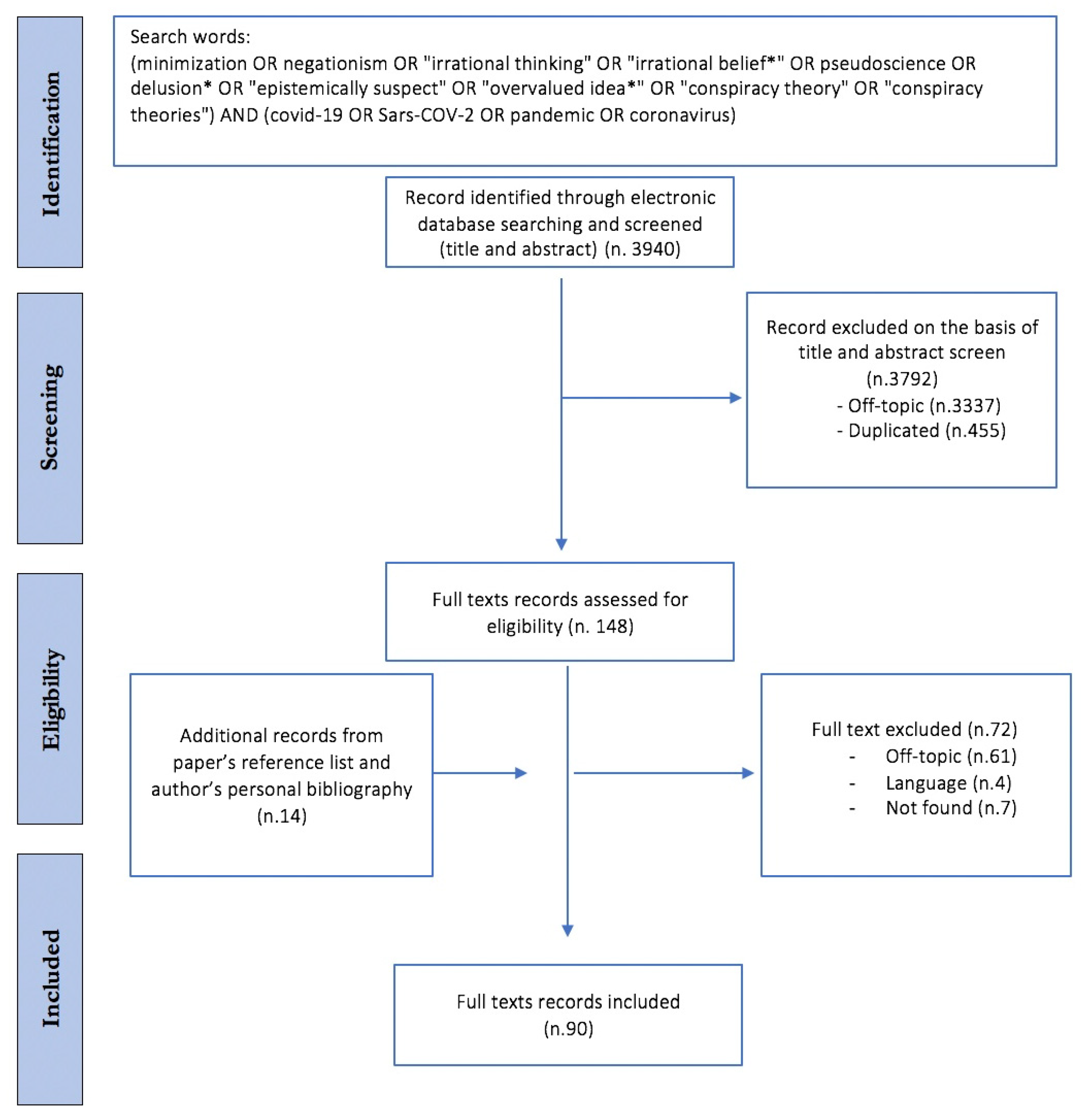
2.4. Study Selection
2.5. Charting the Data
2.6. Collating, Summarizing and Reporting the Results
3. Results
3.1. Misinformation as a Substrate and Adjuvant in the Development of COVID-19-Related CTs
3.1.1. The Role of Social and Mass Media
3.1.2. The Epistemic Mistrust: Is It Science to Blame?
3.1.3. Epistemic Mistrust’s Implications: Vaccine Hesitancy, Stigma and Risk-Taking Behaviours
3.1.4. The Psycho-Socio-Demographic Profile of Misinformation
3.2. The Dispositional and Situational Explanations of COVID-19 CTs
3.2.1. COVID-19 CT and Socio-Demographic Elements: Education
3.2.2. COVID-19 CT and Socio-Demographic Elements: Gender and Age
3.2.3. COVID-19 CTs Turned Out to Be Closely Related to Other CTs
3.2.4. Uncertainty, Stress and Anxiety
3.2.5. Epistemic Untrust
3.2.6. Political Affiliation
3.2.7. Personality/Psychological Traits
3.3. The Behavioural Effects of COVID-19 CT
3.3.1. Sense of Control vs. Violent Behaviours
3.3.2. Compliance with the Governments’ Rules
3.3.3. Intention to Get Vaccinated
3.3.4. Socio-Demographic Elements
3.3.5. Coping Strategies
3.3.6. Political Ideology
3.3.7. Risk Perception
3.3.8. Emotional Responses
3.3.9. Social Media
3.3.10. Cultural Elements
4. Limitations
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Munich Security Conference. Available online: https://www.who.int/director-general/speeches/detail/munich-security-conference (accessed on 6 August 2021).
- Vériter, S.L.; Bjola, C.; Koops, J.A. Tackling COVID-19 Disinformation: Internal and External Challenges for the European Union. Hague J. Dipl. 2020, 15, 569–582. [Google Scholar] [CrossRef]
- Bruns, A.; Harrington, S.; Hurcombe, E. ‘Corona? 5G? Or both?’: The dynamics of COVID-19/5G conspiracy theories on Facebook. Media Int. Aust. 2020, 177, 12–29. [Google Scholar] [CrossRef]
- Chisholm, R.M. Theory of Knowledge, 3rd ed.; Prentice-Hall Foundations of Philosophy Series; Prentice-Hall International: Englewood Cliffs, NJ, USA, 1989. [Google Scholar]
- Bortolotti, L. The Epistemic Innocence of Irrational Beliefs; Oxford University Press: Oxford, NY, USA, 2020. [Google Scholar]
- Douglas, K.M.; Sutton, R.M. Why conspiracy theories matter: A social psychological analysis. Eur. Rev. Soc. Psychol. 2018, 29, 256–298. Available online: https://www.tandfonline.com/doi/abs/10.1080/10463283.2018.1537428 (accessed on 6 August 2021). [CrossRef] [Green Version]
- Van Prooijen, J.-W.; Douglas, K. Conspiracy theories as part of history: The role of societal crisis situations. Mem. Stud. 2017, 10, 323–333. Available online: https://journals.sagepub.com/doi/full/10.1177/1750698017701615 (accessed on 6 August 2021). [CrossRef]
- Uscinski, J.E.; Parent, J.M. American Conspiracy Theories; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Cichocka, A. To counter conspiracy theories, boost well-being. Nature 2020, 587, 177. [Google Scholar] [CrossRef] [PubMed]
- Van Prooijen, J.-W.; Douglas, K.M. Belief in conspiracy theories: Basic principles of an emerging research domain. Eur. J. Soc. Psychol. 2018, 48, 897–908. [Google Scholar] [CrossRef] [PubMed]
- Bierwiaczonek, K.; Kunst, J.R.; Pich, O. Belief in COVID-19 Conspiracy Theories Reduces Social Distancing over Time. Appl. Psychol. Health Well-Being 2020, 12, 1270–1285. [Google Scholar] [CrossRef]
- Marinthe, G.; Brown, G.; Delouvée, S.; Jolley, D. Looking out for myself: Exploring the relationship between conspiracy mentality, perceived personal risk, and COVID-19 prevention measures. Br. J. Health Psychol. 2020, 25, 957–980. [Google Scholar] [CrossRef]
- Teovanović, P.; Lukić, P.; Zupan, Z.; Lazić, A.; Ninković, M.; Žeželj, I. Irrational beliefs differentially predict adherence to guidelines and pseudoscientific practices during the COVID-19 pandemic. Appl. Cogn. Psychol. 2020, 35, 486–496. [Google Scholar] [CrossRef] [PubMed]
- Schippers, M.C. For the Greater Good? The Devastating Ripple Effects of the COVID-19 Crisis. Front. Psychol. 2020, 11, 577740. [Google Scholar] [CrossRef] [PubMed]
- Mousavi, E.S.; Kananizadeh, N.; Martinello, R.A.; Sherman, J.D. COVID-19 Outbreak and Hospital Air Quality: A Systematic Review of Evidence on Air Filtration and Recirculation. Environ. Sci. Technol. 2020, 55, 4134–4147. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.-Q.; Chung, P.-K.; Liu, J.D.; Chan, D.K.C.; Hagger, M.S.; Hamilton, K. Health Beliefs of Wearing Facemasks for Influenza A/H1N1 Prevention: A Qualitative Investigation of Hong Kong Older Adults. Asia Pac. J. Public Health 2019, 31, 246–256. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.; Imani, V.; Majd, N.R.; Ghasemi, Z.; Griffiths, M.D.; Hamilton, K.; Hagger, M.S.; Pakpour, A.H. Using an integrated social cognition model to predict COVID-19 preventive behaviours. Br. J. Health Psychol. 2020, 25, 981–1005. [Google Scholar] [CrossRef] [PubMed]
- Chou, E.Y.; Murnighan, J.K. Life or Death Decisions: Framing the Call for Help. PLoS ONE 2013, 8, e57351. [Google Scholar] [CrossRef] [Green Version]
- Pyszczynski, T.; Solomon, S.; Greenberg, J. Thirty Years of Terror Management Theory. Adv. Exp. Soc. Psychol. 2015, 52, 1–70. [Google Scholar] [CrossRef]
- Kelman, H.C. Compliance, Identification, and Internalization: Three Processes of Attitude Change. J. Confl. Resolut. 1958, 2, 51–60. [Google Scholar] [CrossRef]
- Tong, A.; Flemming, K.; McInnes, E.; Oliver, S.; Craig, J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med. Res. Methodol. 2012, 12, 181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Gough, D.; Oliver, S.; Thomas, J. An Introduction to Systematic Reviews; SAGE: Newcastle upon Tyne, UK, 2017. [Google Scholar]
- Rathore, F.; Farooq, F. Information Overload and Infodemic in the COVID-19 Pandemic. J. Pak. Med. Assoc. 2020, 70, S162–S165. [Google Scholar] [CrossRef]
- Ferrara, E.; Cresci, S.; Luceri, L. Misinformation, manipulation, and abuse on social media in the era of COVID-19. J. Comput. Soc. Sci. 2020, 3, 271–277. [Google Scholar] [CrossRef]
- Nguyen, A.; Catalan-Matamoros, D. Digital Mis/Disinformation and Public Engagment with Health and Science Controversies: Fresh Perspectives from COVID-19. Media Commun. 2020, 8, 323–328. [Google Scholar] [CrossRef]
- Bin Naeem, S.; Bhatti, R.; Khan, A. An exploration of how fake news is taking over social media and putting public health at risk. Health Inf. Libr. J. 2020, 38, 143–149. [Google Scholar] [CrossRef]
- Chong, M. Network typology, information sources, and messages of the infodemic twitter network under COVID-19. Proc. Assoc. Inf. Sci. Technol. 2020, 57, e363. [Google Scholar] [CrossRef] [PubMed]
- Quinn, E.K.; Fazel, S.S.; Peters, C.E. The Instagram Infodemic: Cobranding of Conspiracy Theories, Coronavirus Disease 2019 and Authority-Questioning Beliefs. Cyberpsychol. Behav. Soc. Netw. 2021, 24, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Memon, S.A.; Carley, K.M. Characterizing COVID-19 Misinformation Communities Using a Novel Twitter Dataset. In Proceedings of the CEUR Workshop Proceedings, Galway, Ireland, 19–23 October 2020; Volume 2699. [Google Scholar]
- Mourad, A.; Srour, A.; Harmanani, H.; Jenainati, C.; Arafeh, M. Critical Impact of Social Networks Infodemic on Defeating Coronavirus COVID-19 Pandemic: Twitter-Based Study and Research Directions. IEEE Trans. Netw. Serv. Manag. 2020, 17, 2145–2155. [Google Scholar] [CrossRef]
- Pereira, P.S.; Silveira, A.D.S.; Pereira, A. Disinformation and Conspiracy Theories in the Age of COVID-19. Front. Sociol. 2020, 5, 560681. [Google Scholar] [CrossRef]
- Grimes, D.R. Health disinformation & social media: The Crucial Role of Information Hygiene in Mitigating Conspiracy Theory and Infodemics. EMBO Rep. 2020, 21, e51819. [Google Scholar] [CrossRef] [PubMed]
- López Cantos, F.; Millán Yeste, J. Diffusion of Pseudoscientific Discourses in Spanish Public Radio. The Program Complementarios by RNE-Radio 5 [La Difusión de Discursos Pseudocientíficos En La Radio Pública Española. El Programa Complementarios de RNE-Radio 5]. Rev. Lat. Comun. Soc. 2018, 73, 317–330. [Google Scholar] [CrossRef] [Green Version]
- Manganello, J.; Bleakley, A.; Schumacher, P. Pandemics and PSAs: Rapidly Changing Information in a New Media Landscape. Health Commun. 2020, 35, 1711–1714. [Google Scholar] [CrossRef]
- Ball, P.; Maxmen, A. The epic battle against coronavirus misinformation and conspiracy theories. Nature 2020, 581, 371–374. [Google Scholar] [CrossRef]
- Ahmed, W.; Vidal-Alaball, J.; Downing, J.; Seguí, F.L. COVID-19 and the 5G Conspiracy Theory: Social Network Analysis of Twitter Data. J. Med. Internet Res. 2020, 22, e19458. [Google Scholar] [CrossRef]
- Koerber, A. Is It Fake News or Is It Open Science? Science Communication in the COVID-19 Pandemic. J. Bus. Tech. Commun. 2020, 35, 22–27. [Google Scholar] [CrossRef]
- Scheirer, W. A pandemic of bad science. Bull. At. Sci. 2020, 76, 175–184. [Google Scholar] [CrossRef]
- Sasidharan, S.; Dhillon, H.S.; Singh, D.H.; Manalikuzhiyil, B. COVID-19: Pan(info)demic. Turk. J. Anaesthesiol. Reanim. 2020, 48, 438–442. [Google Scholar] [CrossRef] [PubMed]
- Kasapçopur, Ö. Science and pseudoscience during the COVID-19 pandemic [COVID-19 Pandemisi Sırasında Bilim ve Yalancı Bilim]. Turk. Pediatr. Arch. 2020, 55, 335–336. [Google Scholar] [CrossRef]
- Pimentel, J.V.C.; e Silva, T.D.O.S.; Filgueiras, A.B.T.; Neto, M.L.R. The Impact of Science-Unbased Measures against COVID-19 in Clinical Decision-Making Process. AAPS PharmSciTech 2020, 21, 1–2. [Google Scholar] [CrossRef]
- Corvo, E.; De Caro, W. The paradox of the link between health literacy and health promotion: The case of COVID-19. Prof. Inferm. 2020, 73, 219–222. [Google Scholar]
- Huidu, A. The Social Responsibility of Researchers in Combating Fake News and Conspiracy Theories during a Pandemic. Postmod. Open. 2020, 11, 39–48. [Google Scholar] [CrossRef]
- Khan, Y.H.; Mallhi, T.H.; Alotaibi, N.H.; AlZarea, A.I.; Alanazi, A.S.; Tanveer, N.; Hashmi, F.K. Threat of COVID-19 Vaccine Hesitancy in Pakistan: The Need for Measures to Neutralize Misleading Narratives. Am. J. Trop. Med. Hyg. 2020, 103, 603–604. [Google Scholar] [CrossRef]
- Etzioni-Friedman, T.; Etzioni, A. Adherence to Immunization: Rebuttal of Vaccine Hesitancy. Acta Haematol. 2021, 144, 57–61. [Google Scholar] [CrossRef]
- Ahmed, W.; Seguí, F.L.; Vidal-Alaball, J.; Katz, M.S. COVID-19 and the “Film Your Hospital” Conspiracy Theory: Social Network Analysis of Twitter Data. J. Med. Internet Res. 2020, 22, e22374. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Twersky, S.; Ignace, K.; Zhao, M.; Purandare, R.; Bennett-Jones, B.; Weaver, S. Constructing and Communicating COVID-19 Stigma on Twitter: A Content Analysis of Tweets during the Early Stage of the COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2020, 17, 6847. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.; Sarkar, T.; Khan, S.H.; Kamal, A.-H.M.; Hasan, S.M.M.; Kabir, A.; Yeasmin, D.; Islam, M.A.; Chowdhury, K.I.A.; Anwar, K.S.; et al. COVID-19–Related Infodemic and Its Impact on Public Health: A Global Social Media Analysis. Am. J. Trop. Med. Hyg. 2020, 103, 1621–1629. [Google Scholar] [CrossRef] [PubMed]
- Mian, A.; Khan, S. Coronavirus: The spread of misinformation. BMC Med. 2020, 18, 89. [Google Scholar] [CrossRef] [PubMed]
- Kalichman, S.C. The Psychology of AIDS Denialism: Pseudoscience, Conspiracy Thinking, and Medical Mistrust. Eur. Psychol. 2014, 19, 13–22. [Google Scholar] [CrossRef]
- Jaiswal, J.; LoSchiavo, C.; Perlman, D.C. Disinformation, Misinformation and Inequality-Driven Mistrust in the Time of COVID-19: Lessons Unlearned from AIDS Denialism. AIDS Behav. 2020, 24, 2776–2780. [Google Scholar] [CrossRef]
- Lee, J.J.; Kang, K.-A.; Wang, M.P.; Zhao, S.Z.; Wong, J.Y.H.; O’Connor, S.; Yang, S.C.; Shin, S. Associations Between COVID-19 Misinformation Exposure and Belief With COVID-19 Knowledge and Preventive Behaviors: Cross-Sectional Online Study. J. Med. Internet Res. 2020, 22, e22205. [Google Scholar] [CrossRef] [PubMed]
- Prandi, L.; Primiero, G. Effects of misinformation diffusion during a pandemic. Appl. Netw. Sci. 2020, 5, 1–20. [Google Scholar] [CrossRef]
- Erceg, N.; Ružojčić, M.; Galić, Z. Misbehaving in the Corona crisis: The role of anxiety and unfounded beliefs. Curr. Psychol. 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Agley, J.; Xiao, Y. Misinformation about COVID-19: Evidence for differential latent profiles and a strong association with trust in science. BMC Public Health 2021, 21, 89. [Google Scholar] [CrossRef]
- Lobato, E.J.C.; Powell, M.; Padilla, L.M.K.; Holbrook, C. Factors Predicting Willingness to Share COVID-19 Misinformation. Front. Psychol. 2020, 11, 2413. [Google Scholar] [CrossRef]
- Motta, M.; Stecula, D.; Farhart, C. How Right-Leaning Media Coverage of COVID-19 Facilitated the Spread of Misinformation in the Early Stages of the Pandemic in the U.S. Can. J. Polit. Sci. 2020, 53, 335–342. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Yaseen, A.; Al-Haidar, A.; Taim, D.; Eid, H.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. COVID-19 misinformation: Mere harmless delusions or much more? A knowledge and attitude cross-sectional study among the general public residing in Jordan. PLoS ONE 2020, 15, e0243264. [Google Scholar] [CrossRef]
- Mejova, Y.; Kalimeri, K. COVID-19 on Facebook Ads: Competing Agendas around a Public Health Crisis. In Proceedings of the COMPASS 2020—The 3rd ACM SIGCAS Conference on Computing and Sustainable Societies, Guayaquil, Ecuador, 15–17 June 2020. [Google Scholar] [CrossRef]
- Duplaga, M. The Determinants of Conspiracy Beliefs Related to the COVID-19 Pandemic in a Nationally Representative Sample of Internet Users. Int. J. Environ. Res. Public Health 2020, 17, 7818. [Google Scholar] [CrossRef]
- Shaeffer, K. A Look at the Americans Who Believe There Is Some Truth to the Conspiracy Theory That COVID-19 Was Planned. Pew Research Center. Available online: https://www.pewresearch.org/fact-tank/2020/07/24/a-look-at-the-americans-who-believe-there-is-some-truth-to-the-conspiracy-theory-that-covid-19-was-planned/ (accessed on 16 September 2021).
- Somma, A.; Gialdi, G.; Frau, C.; Barranca, M.; Fossati, A. COVID-19 pandemic preventive behaviors and causal beliefs among Italian community dwelling adults. J. Health Psychol. 2020, 1359105320962243. [Google Scholar] [CrossRef]
- Stoica, C.A.; Umbreș, R. Suspicious minds in times of crisis: Determinants of Romanians’ beliefs in COVID-19 conspiracy theories. Eur. Soc. 2020, 23, S246–S261. [Google Scholar] [CrossRef]
- Georgiou, N.; Delfabbro, P.; Balzan, R. COVID-19-related conspiracy beliefs and their relationship with perceived stress and pre-existing conspiracy beliefs. Pers. Individ. Differ. 2020, 166, 110201. [Google Scholar] [CrossRef] [PubMed]
- Robson, D. The Intelligence Trap: Why Smart People Make Dumb Mistakes; W. W. Norton: New York, NY, USA, 2019. [Google Scholar]
- Cassese, E.C.; Farhart, C.E.; Miller, J.M. Gender Differences in COVID-19 Conspiracy Theory Beliefs. Polit. Gend. 2020, 16, 1009–1018. [Google Scholar] [CrossRef]
- Allington, D.; Duffy, B.; Wessely, S.; Dhavan, N.; Rubin, J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol. Med. 2020, 51, 1763–1769. [Google Scholar] [CrossRef] [PubMed]
- Goertzel, T. Belief in Conspiracy Theories. Polit.-Psychol. 1994, 15, 731. [Google Scholar] [CrossRef]
- Lukić, P.; Žeželj, I.; Stanković, B. How (ir)rational is it to believe in contradictory conspiracy theories? Eur. J. Psychol. 2019, 15, 94–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wood, M.J.; Douglas, K.M.; Sutton, R.M. Dead and Alive: Beliefs in Contradictory Conspiracy Theories. Soc. Psychol. Pers. Sci. 2012, 3, 767–773. [Google Scholar] [CrossRef] [Green Version]
- Alper, S.; Bayrak, F.; Yilmaz, O. Psychological correlates of COVID-19 conspiracy beliefs and preventive measures: Evidence from Turkey. Curr. Psychol. 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Shahsavari, S.; Holur, P.; Wang, T.; Tangherlini, T.R.; Roychowdhury, V. Conspiracy in the time of corona: Automatic detection of emerging COVID-19 conspiracy theories in social media and the news. J. Comput. Soc. Sci. 2020, 3, 279–317. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M. Do COVID-19 Conspiracy Theory Beliefs Form a Monological Belief System? Can. J. Polit. Sci. 2020, 53, 319–326. [Google Scholar] [CrossRef]
- Sturm, T.; Albrecht, T. Constituent COVID-19 apocalypses: Contagious conspiracism, 5G, and viral vaccinations. Anthr. Med. 2020, 28, 122–139. [Google Scholar] [CrossRef]
- Douglas, K.M.; Uscinski, J.E.; Sutton, R.M.; Cichocka, A.; Nefes, T.; Ang, C.S.; Deravi, F. Understanding Conspiracy Theories. Polit. Psychol. 2019, 40, 3–35. [Google Scholar] [CrossRef] [Green Version]
- Van Prooijen, J.-W.; Acker, M. The Influence of Control on Belief in Conspiracy Theories: Conceptual and Applied Extensions. Appl. Cogn. Psychol. 2015, 29, 753–761. [Google Scholar] [CrossRef]
- Ali, I. Impacts of rumors and conspiracy theories surrounding COVID-19 on preparedness programs. Disaster Med. Public Health Prep. 2020, 1–15. [Google Scholar] [CrossRef]
- Egorova, M.S.; Parshikova, O.V.; Chertkova, Y.D.; Staroverov, V.M.; Mitina, O.V. COVID-19: Belief in Conspiracy Theories and the Need for Quarantine. Psychol. Russ. State Art 2020, 13, 3–25. [Google Scholar] [CrossRef]
- Miller, J.M. Psychological, Political, and Situational Factors Combine to Boost COVID-19 Conspiracy Theory Beliefs. Can. J. Polit. Sci. 2020, 53, 327–334. [Google Scholar] [CrossRef]
- Kim, S.; Kim, S. Searching for General Model of Conspiracy Theories and Its Implication for Public Health Policy: Analysis of the Impacts of Political, Psychological, Structural Factors on Conspiracy Beliefs about the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 18, 266. [Google Scholar] [CrossRef] [PubMed]
- Jovančević, A.; Milićević, N. Optimism-pessimism, conspiracy theories and general trust as factors contributing to COVID-19 related behavior—A cross-cultural study. Pers. Individ. Differ. 2020, 167, 110216. [Google Scholar] [CrossRef] [PubMed]
- Uscinski, J.E.; Enders, A.M.; Klofstad, C.; Seelig, M.; Funchion, J.; Everett, C.; Wuchty, S.; Premaratne, K.; Murthi, M. Why do people believe COVID-19 conspiracy theories? Harv. Kennedy Sch. Misinf. Rev. 2020, 1. [Google Scholar] [CrossRef]
- Oleksy, T.; Wnuk, A.; Maison, D.; Łyś, A. Content matters. Different predictors and social consequences of general and government-related conspiracy theories on COVID-19. Pers. Individ. Differ. 2020, 168, 110289. [Google Scholar] [CrossRef]
- Romer, D.; Jamieson, K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 2020, 263, 113356. [Google Scholar] [CrossRef]
- Pennycook, G.; Mcphetres, J.; Bago, B.; Rand, D. Predictors of Attitudes and Misperceptions about COVID-19 in Canada, the U.K., and the U.S.A. PsyArXiv 2020, 10, 1–25. [Google Scholar] [CrossRef]
- Sutton, R.M.; Douglas, K.M. Conspiracy theories and the conspiracy mindset: Implications for political ideology. Curr. Opin. Behav. Sci. 2020, 34, 118–122. [Google Scholar] [CrossRef]
- Calvillo, D.P.; Ross, B.J.; Garcia, R.J.B.; Smelter, T.J.; Rutchick, A.M. Political Ideology Predicts Perceptions of the Threat of COVID-19 (and Susceptibility to Fake News About It). Soc. Psychol. Pers. Sci. 2020, 11, 1119–1128. [Google Scholar] [CrossRef]
- Gruzd, A.; Mai, P. Going viral: How a single tweet spawned a COVID-19 conspiracy theory on Twitter. Big Data Soc. 2020, 7, 2053951720938405. [Google Scholar] [CrossRef]
- Ndinojuo, B.-C.E. 5G, Religion, and Misconceptions in Communication during COVID-19 in Nigeria. J. Messenger 2020, 12, 97–110. [Google Scholar] [CrossRef]
- Kibuuka, B.G.L. Complicity and Synergy between Bolsonaro and Brazilian Evangelicals in COVID-19 Times: Adherence to Scientific Negationism for Political-Religious Reasons. Int. J. Lat. Am. Relig. 2020, 4, 288–317. [Google Scholar] [CrossRef]
- Harper, C.A.; Satchell, L.P.; Fido, D.; Latzman, R.D. Functional Fear Predicts Public Health Compliance in the COVID-19 Pandemic. Int. J. Ment. Health Addict. 2020, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Hughes, S.; Machan, L. It’s a conspiracy: COVID-19 conspiracies link to psychopathy, Machiavellianism and collective narcissism. Pers. Individ. Differ. 2020, 171, 110559. [Google Scholar] [CrossRef] [PubMed]
- Sternisko, A.; Cichocka, A.; Cislak, A.; Bavel, J.J.V. Collective Narcissism Predicts the Belief and Dissemination of Conspiracy Theories during the COVID-19 Pandemic. PsyArXiv 2020. [Google Scholar] [CrossRef]
- Imhoff, R.; Lamberty, P. A Bioweapon or a Hoax? The Link between Distinct Conspiracy Beliefs about the Coronavirus Disease (COVID-19) Outbreak and Pandemic Behavior. Soc. Psychol. Pers. Sci. 2020, 11, 1110–1118. [Google Scholar] [CrossRef]
- Escolà-Gascón, Á.; Marín, F.-X.; Rusiñol, J.; Gallifa, J. Pseudoscientific beliefs and psychopathological risks increase after COVID-19 social quarantine. Glob. Health 2020, 16, 72. [Google Scholar] [CrossRef]
- Maftei, A.; Holman, A.-C. Beliefs in conspiracy theories, intolerance of uncertainty, and moral disengagement during the coronavirus crisis. Ethic Behav. 2020, 1–11. [Google Scholar] [CrossRef]
- Giner-Sorolla, R.; Russell, P.S. Not Just Disgust: Fear and Anger Also Relate to Intergroup Dehumanization. Collabra Psychol. 2019, 5, 56. [Google Scholar] [CrossRef]
- Plohl, N.; Musil, B. Modeling compliance with COVID-19 prevention guidelines: The critical role of trust in science. Psychol. Health Med. 2020, 26, 1–12. [Google Scholar] [CrossRef]
- Freeman, D.; Waite, F.; Rosebrock, L.; Petit, A.; Causier, C.; East, A.; Jenner, L.; Teale, A.-L.; Carr, L.; Mulhall, S.; et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol. Med. 2020, 1–13. [Google Scholar] [CrossRef]
- Pummerer, L.; Böhm, R.; Lilleholt, L.; Winter, K.; Zettler, I.; Sassenberg, K. Conspiracy Theories and Their Societal Effects During the COVID-19 Pandemic. Soc. Psychol. Pers. Sci. 2021. [Google Scholar] [CrossRef]
- Earnshaw, V.A.; Eaton, L.A.; Kalichman, S.C.; Brousseau, N.M.; Hill, E.C.; Fox, A.B. COVID-19 conspiracy beliefs, health behaviors, and policy support. Transl. Behav. Med. 2020, 10, 850–856. [Google Scholar] [CrossRef]
- Bertin, P.; Nera, K.; Delouvée, S. Conspiracy Beliefs, Rejection of Vaccination, and Support for hydroxychloroquine: A Conceptual Replication-Extension in the COVID-19 Pandemic Context. Front. Psychol. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, M.; Geçer, E.; Akgül, Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychol. Health Med. 2020, 26, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Carlucci, L.; D’Ambrosio, I.; Balsamo, M. Demographic and Attitudinal Factors of Adherence to Quarantine Guidelines during COVID-19: The Italian Model. Front. Psychol. 2020, 11, 559288. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, F.; Zhu, C.; Wang, Z. Willingness to Self-Isolate When Facing a Pandemic Risk: Model, Empirical Test, and Policy Recommendations. Int. J. Environ. Res. Public Health 2019, 17, 197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Urban, M.; Urban, K.; Urban, K. What Can We Learn from Gritty Persons? Coping Strategies Adopted during COVID-19 Lockdown. Mediterr. J. Clin. Psychol. 2020, 8, 1–21. [Google Scholar] [CrossRef]
- Gerhold, L. COVID-19: Risk Perception and Coping Strategies. PsyArXiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Prichard, E.C.; Christman, S.D. Authoritarianism, Conspiracy Beliefs, Gender and COVID-19: Links between Individual Differences and Concern about COVID-19, Mask Wearing Behaviors, and the Tendency to Blame China for the Virus. Front. Psychol. 2020, 11, 597671. [Google Scholar] [CrossRef]
- Latkin, C.A.; Dayton, L.; Moran, M.; Strickland, J.C.; Collins, K. Behavioral and psychosocial factors associated with COVID-19 skepticism in the United States. Curr. Psychol. 2021, 1–9. [Google Scholar] [CrossRef]
- Havey, N.F. Partisan public health: How does political ideology influence support for COVID-19 related misinformation? J. Comput. Soc. Sci. 2020, 3, 319–342. [Google Scholar] [CrossRef]
- Everett, J.A.; Colombatto, C.; Chituc, V.; Brady, W.J.; Crockett, M. The Effectiveness of Moral Messages on Public Health Behavioral Intentions during the COVID-19 Pandemic. PsyArXiv 2020. [Google Scholar] [CrossRef]
- Leung, G.; Quah, S.R.; Ho, L.-M.; Ho, S.-Y.; Hedley, A.J.; Lee, H.-P.; Lam, T.-H. A Tale of Two Cities: Community Psychobehavioral Surveillance and Related Impact on Outbreak Control in Hong Kong and Singapore during the Severe Acute Respiratory Syndrome Epidemic. Infect. Control. Hosp. Epidemiol. 2004, 25, 1033–1041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qian, M.; Wu, Q.; Wu, P.; Hou, Z.; Liang, Y.; Cowling, B.J.; Yu, H. Psychological Responses, Behavioral Changes and Public Perceptions during the Early Phase of the COVID-19 Outbreak in China: A Population Based Cross-Sectional Survey. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Orte, C.; Sánchez-Prieto, L.; Domínguez, D.C.; Barrientos-Báez, A. Evaluation of Distress and Risk Perception Associated with COVID-19 in Vulnerable Groups. Int. J. Environ. Res. Public Health 2020, 17, 9207. [Google Scholar] [CrossRef]
- Chittleborough, C.R.; Winefield, H.; Gill, T.K.; Koster, C.; Taylor, A.W. Age differences in associations between psychological distress and chronic conditions. Int. J. Public Health 2010, 56, 71–80. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Judgment under Uncertainty: Heuristics and Biases. Science 1974, 185, 1124–1131. [Google Scholar] [CrossRef]
- Pfattheicher, S.; Nockur, L.; Böhm, R.; Sassenrath, C.; Petersen, M.B. The Emotional Path to Action: Empathy Promotes Physical Distancing and Wearing of Face Masks During the COVID-19 Pandemic. Psychol. Sci. 2020, 31, 1363–1373. [Google Scholar] [CrossRef] [PubMed]
- Batson, C.D. Altruism in Humans; Oxford University Press: Oxford, UK, 2010. [Google Scholar] [CrossRef]
- Biddlestone, M.; Green, R.; Douglas, K.M. Cultural orientation, power, belief in conspiracy theories, and intentions to reduce the spread of COVID-19. Br. J. Soc. Psychol. 2020, 59, 663–673. [Google Scholar] [CrossRef]
- Boguszewski, R.; Makowska, M.; Bożewicz, M.; Podkowińska, M. The COVID-19 Pandemic’s Impact on Religiosity in Poland. Religions 2020, 11, 646. [Google Scholar] [CrossRef]
- Steeman, T.M.; Neal, S.M.A.; Potvin, R.H.; Reiss, P.J.; Black, M. Max Weber’s Sociology of Religion. Sociol. Anal. 1964, 25, 50–58. [Google Scholar] [CrossRef]
- The Elementary Forms of Religious Life|Work by Durkheim. Available online: https://www.britannica.com/topic/The-Elementary-Forms-of-Religious-Life (accessed on 6 August 2021).
- Hill, T.D.; Gonzalez, K.; Burdette, A.M. The Blood of Christ Compels Them: State Religiosity and State Population Mobility During the Coronavirus (COVID-19) Pandemic. J. Relig. Health 2020, 59, 2229–2242. [Google Scholar] [CrossRef]
- Mukhtar, S. Psychology and politics of COVID-19 misinfodemics: Why and how do people believe in misinfodemics? Int. Sociol. 2020, 36, 111–123. [Google Scholar] [CrossRef]
- Jakovljevic, M.; Bjedov, S.; Mustac, F.; Jakovljevic, I. COVID-19 Infodemic and Public Trust from the Perspective of Public and Global Mental Health. Psychiatr. Danub. 2020, 32, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Hardy, L.J. Connection, Contagion, and COVID-19. Med. Anthropol. 2020, 39, 655–659. [Google Scholar] [CrossRef]
- Audi, R. Epistemology: A Contemporary Introduction to the Theory of Knowledge, 3rd ed.; Routledge: New York, NY, USA, 2010. [Google Scholar] [CrossRef]
- Rescher, N. Epistemology: An Introduction to the Theory of Knowledge; SUNY Series in Philosophy; State University of New York: Albany, NY, USA, 2003. [Google Scholar]
- Eysenbach, G. How to Fight an Infodemic: The Four Pillars of Infodemic Management. J. Med. Internet Res. 2020, 22, e21820. [Google Scholar] [CrossRef]
- Paredes, M.R.; Apaolaza, V.; Fernandez-Robin, C.; Hartmann, P.; Yañez-Martinez, D. The impact of the COVID-19 pandemic on subjective mental well-being: The interplay of perceived threat, future anxiety and resilience. Pers. Individ. Differ. 2021, 170, 110455. [Google Scholar] [CrossRef] [PubMed]
- Jakovljevic, M.; Jakovljevic, I.; Bjedov, S.; Mustac, F. Psychiatry for Better World: COVID-19 and Blame Games People Play from Public and Global Metal Health Perspective. Psychiatr. Danub. 2020, 32, 221–228. [Google Scholar] [CrossRef] [PubMed]
| Socio-Demographic Elements | Situational Elements | Personality/Psychological Traits | |
|---|---|---|---|
| Contextual | Antecedents | ||
| Low educational level Limited scientific knowledge Younger age No gender difference | Experiencing situation-induced uncertainty High level of self-perceived risk and anxiety | Believing in other CT not related to COVID-19 Mistrusting toward the government Political or religious polarization Self-perceiving inability to respond to external threats | Low levels of epistemic trust Predisposition to reject expert information Conspiracy prone mindset Avoidance of uncertainty Low resilience predisposition Extraversion Machiavellianism and primary psychopathy External blame attitude Collective Narcissism Cognitive characteristics:
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magarini, F.M.; Pinelli, M.; Sinisi, A.; Ferrari, S.; De Fazio, G.L.; Galeazzi, G.M. Irrational Beliefs about COVID-19: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 9839. https://doi.org/10.3390/ijerph18199839
Magarini FM, Pinelli M, Sinisi A, Ferrari S, De Fazio GL, Galeazzi GM. Irrational Beliefs about COVID-19: A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(19):9839. https://doi.org/10.3390/ijerph18199839
Chicago/Turabian StyleMagarini, Federica Maria, Margherita Pinelli, Arianna Sinisi, Silvia Ferrari, Giovanna Laura De Fazio, and Gian Maria Galeazzi. 2021. "Irrational Beliefs about COVID-19: A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 19: 9839. https://doi.org/10.3390/ijerph18199839
APA StyleMagarini, F. M., Pinelli, M., Sinisi, A., Ferrari, S., De Fazio, G. L., & Galeazzi, G. M. (2021). Irrational Beliefs about COVID-19: A Scoping Review. International Journal of Environmental Research and Public Health, 18(19), 9839. https://doi.org/10.3390/ijerph18199839








