Association between Adverse Childhood Experiences and Time Spent Playing Video Games in Adolescents: Results from A-CHILD Study
Abstract
1. Introduction
2. Materials and Methods
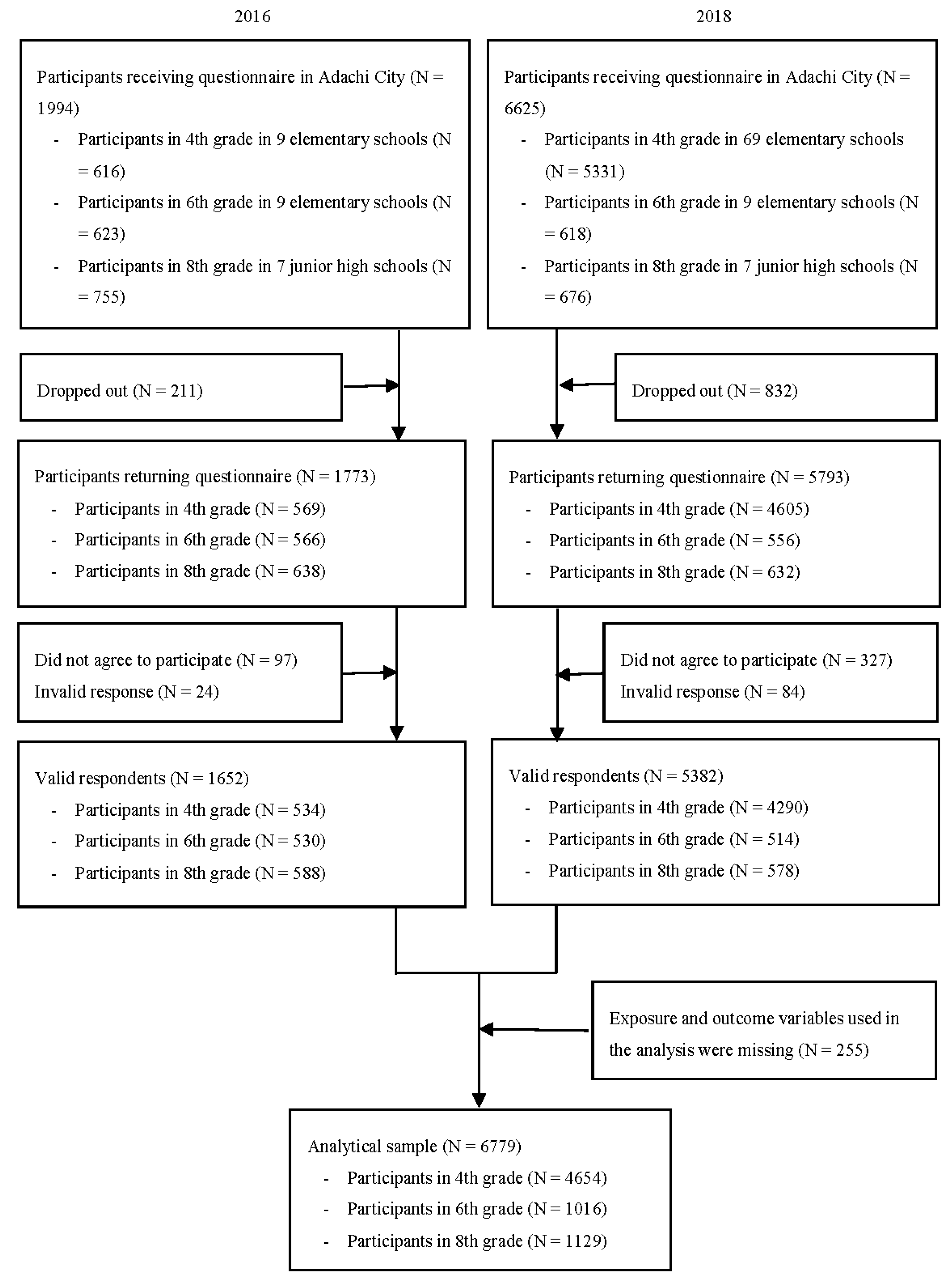
2.1. Participants
2.2. Measurements
2.3. Ethics
2.4. Statistical Analysis
3. Results
3.1. The Distribution of Characteristics
3.2. The Association between ACEs and Time Spent Playing Video Games
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (Dsm-5®); American Psychiatric Association Publising: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organization. International Classification of Diseases for Mortality and Morbidity Statistics (11th Revision). Available online: https://icd.who.int/browse11/l-m/en (accessed on 31 August 2021).
- Ferreira, F.D.M.; Bambini, B.B.; Tonsig, G.K.; Fonseca, L.; Picon, F.A.; Pan, P.M.; Salum, G.A.; Jackowski, A.; Miguel, E.C.; Rohde, L.A.; et al. Predictors of Gaming Disorder in Children and Adolescents: A School-Based Study. Braz. J. Psychiatry 2020, 43, 289–292. [Google Scholar] [CrossRef] [PubMed]
- Gentile, D.A.; Choo, H.; Liau, A.; Sim, T.; Li, D.; Fung, D.; Khoo, A. Pathological Video Game Use among Youths: A Two-Year Longitudinal Study. Pediatrics 2011, 127, e319–e329. [Google Scholar] [CrossRef] [PubMed]
- Marker, C.; Gnambs, T.; Appel, M. Exploring the Myth of the Chubby Gamer: A Meta-Analysis on Sedentary Video Gaming and Body Mass. Soc. Sci. Med. 2019, 112325. [Google Scholar] [CrossRef] [PubMed]
- Bélanger, R.E.; Akre, C.; Berchtold, A.; Michaud, P.A. A U-Shaped Association between Intensity of Internet Use and Adolescent Health. Pediatrics 2011, 127, e330–e335. [Google Scholar] [CrossRef] [PubMed]
- Weaver, E.; Gradisar, M.; Dohnt, H.; Lovato, N.; Douglas, P. The Effect of Presleep Video-Game Playing on Adolescent Sleep. J. Clin. Sleep Med. 2010, 6, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Coyne, S.M.; Stockdale, L.A.; Warburton, W.; Gentile, D.A.; Yang, C.; Merrill, B.M. Pathological Video Game Symptoms from Adolescence to Emerging Adulthood: A 6-Year Longitudinal Study of Trajectories, Predictors, and Outcomes. Dev. Psychol. 2020, 56, 1385. [Google Scholar] [CrossRef] [PubMed]
- Männikkö, N.; Ruotsalainen, H.; Miettunen, J.; Pontes, H.M.; Kääriäinen, M. Problematic Gaming Behaviour and Health-Related Outcomes: A Systematic Review and Meta-Analysis. J. Health Psychol. 2020, 25, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, C.J. Do Angry Birds Make for Angry Children? A Meta-Analysis of Video Game Influences on Children’s and Adolescents’ Aggression, Mental Health, Prosocial Behavior, and Academic Performance. Perspect. Psychol. Sci. 2015, 10, 646–666. [Google Scholar] [CrossRef]
- Schneider, L.A.; King, D.L.; Delfabbro, P.H. Family Factors in Adolescent Problematic Internet Gaming: A Systematic Review. J. Behav. Addict. 2017, 6, 321–333. [Google Scholar] [CrossRef]
- Bender, P.K.; Kim, E.L.; Gentile, D.A. Gaming Disorder in Children and Adolescents: Risk Factors and Preventive Approaches. Curr. Addict. Rep. 2020, 7, 553–560. [Google Scholar] [CrossRef]
- Yang, X.; Jiang, X.; Mo, P.K.H.; Cai, Y.; Ma, L.; Lau, J.T.F. Prevalence and Interpersonal Correlates of Internet Gaming Disorders among Chinese Adolescents. Int. J. Environ. Res. Public Health 2020, 17, 579. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, M.; Meilstrup, C.R.; Bendtsen, P.; Pedersen, T.P.; Nielsen, L.; Madsen, K.R.; Holstein, B.E. Perceived Problems with Computer Gaming and Internet Use Are Associated with Poorer Social Relations in Adolescence. Int. J. Public Health 2015, 60, 179–188. [Google Scholar] [CrossRef]
- Lee, C.; Kim, O. Predictors of Online Game Addiction among Korean Adolescents. Addict. Res. Theory 2017, 25, 58–66. [Google Scholar] [CrossRef]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. The Adverse Childhood Experiences (Ace) Study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef]
- Finkelhor, D.; Shattuck, A.; Turner, H.; Hamby, S. A Revised Inventory of Adverse Childhood Experiences. Child Abus. Negl. 2015, 48, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Marchica, L.A.; Keough, M.T.; Montreuil, T.C.; Derevensky, J.L. Emotion Regulation Interacts with Gambling Motives to Predict Problem Gambling among Emerging Adults. Addict. Behav. 2020, 106, 106378. [Google Scholar] [CrossRef]
- Afifi, T.O.; Taillieu, T.; Salmon, S.; Davila, I.G.; Stewart-Tufescu, A.; Fortier, J.; Struck, S.; Asmundson, G.J.G.; Sareen, J.; MacMillan, H.L. Adverse Childhood Experiences (Aces), Peer Victimization, and Substance Use among Adolescents. Child Abus. Negl. 2020, 106, 104504. [Google Scholar] [CrossRef]
- Sharma, A.; Sacco, P. Adverse Childhood Experiences and Gambling: Results from a National Survey. J. Soc. Work. Pract. Addict. 2015, 15, 25–43. [Google Scholar] [CrossRef]
- Grajewski, P.; Dragan, M. Adverse Childhood Experiences, Dissociation, and Anxious Attachment Style as Risk Factors of Gaming Disorder. Addict. Behav. Rep. 2020, 11, 100269. [Google Scholar] [CrossRef]
- Crews, F.; He, J.; Hodge, C. Adolescent Cortical Development: A Critical Period of Vulnerability for Addiction. Pharmacol. Biochem. Behav. 2007, 86, 189–199. [Google Scholar] [CrossRef]
- Ochi, M.; Isumi, A.; Kato, T.; Doi, S.; Fujiwara, T. Adachi Child Health Impact of Living Difficulty (a-Child) Study: Research Protocol and Profiles of Participants. J. Epidemiol. 2021, 31, 77–89. [Google Scholar] [CrossRef]
- Isumi, A.; TFujiwara, a.; Nawa, N.; Ochi, M.; Kato, T. Mediating Effects of Parental Psychological Distress and Individual-Level Social Capital on the Association between Child Poverty and Maltreatment in Japan. Child Abus. Negl. 2018, 83, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Zhang, X.; Chu, M.; Li, G. The Impact of Adverse Childhood Experiences on Mobile Phone Addiction in Chinese College Students: A Serial Multiple Mediator Model. Front. Psychol. 2020, 11, 834. [Google Scholar] [CrossRef]
- Cacioppo, M.; Barni, D.; Correale, C.; Mangialavori, S.; Danioni, F.; Gori, A. Do Attachment Styles and Family Functioning Predict Adolescents’ Problematic Internet Use? A Relative Weight Analysis. J. Child Fam. Stud. 2019, 28, 1263–1271. [Google Scholar] [CrossRef]
- Doidge, J.C.; Higgins, D.J.; Delfabbro, P.; Segal, L. Risk Factors for Child Maltreatment in an Australian Population-Based Birth Cohort. Child Abus. Negl. 2017, 64, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.-J.; Stewart, R.; Lee, J.; Kim, J.; Kim, S.; Shin, I.; Yoon, J. Prevalence and Correlates of Problematic Internet Experiences and Computer-Using Time: A Two-Year Longitudinal Study in Korean School Children. Psychiatry Investig. 2014, 11, 24. [Google Scholar] [CrossRef][Green Version]
- Yu, Q.; Zhang, L.; Wu, S.; Guo, Y.; Jin, S.; Sun, Y. The Influence of Juvenile Preference for Online Social Interaction on Problematic Internet Use: The Moderating Effect of Sibling Condition and the Moderated Moderating Effect of Age Cohort. Comput. Hum. Behav. 2017, 68, 345–351. [Google Scholar] [CrossRef]
- King, D.L.; Delfabbro, P.H. The Cognitive Psychopathology of Internet Gaming Disorder in Adolescence. J. Abnorm. Child Psychol. 2016, 44, 1635–1645. [Google Scholar] [CrossRef]
- Rehbein, F.; Baier, D. Family-, Media-, and School-Related Risk Factors of Video Game Addiction. J. Media Psychol. 2013, 25. [Google Scholar] [CrossRef]
- Yu, C.; Li, W.; Liang, Q.; Liu, X.; Zhang, W.; Lu, H.; Dou, K.; Xie, X.; Gan, X. School Climate, Loneliness, and Problematic Online Game Use among Chinese Adolescents: The Moderating Effect of Intentional Self-Regulation. Front. Public Health 2019, 7, 90. [Google Scholar] [CrossRef]
- Lam, L.T. Parental Mental Health and Internet Addiction in Adolescents. Addict. Behav. 2015, 42, 20–23. [Google Scholar] [CrossRef]
- Rehbein, F.; Psych, G.; Kleimann, M.; Mediasci, G.; Mößle, T. Prevalence and Risk Factors of Video Game Dependency in Adolescence: Results of a German Nationwide Survey. Cyberpsychol. Behav. Soc. Netw. 2010, 13, 269–277. [Google Scholar] [CrossRef]
- Vadlin, S.; Åslund, C.; Hellström, C.; Nilsson, K.W. Associations between Problematic Gaming and Psychiatric Symptoms among Adolescents in Two Samples. Addict. Behav. 2016, 61, 8–15. [Google Scholar] [CrossRef]
- Sugaya, N.; Shirasaka, T.; Takahashi, K.; Kanda, H. Bio-Psychosocial Factors of Children and Adolescents with Internet Gaming Disorder: A Systematic Review. Biopsychosoc. Med. 2019, 13, 3. [Google Scholar] [CrossRef]
- Nielsen, P.; Favez, N.; Rigter, H. Parental and Family Factors Associated with Problematic Gaming and Problematic Internet Use in Adolescents: A Systematic Literature Review. Curr. Addict. Rep. 2020, 7, 365–386. [Google Scholar] [CrossRef]
- Moilanen, K.L.; Shaw, D.S.; Criss, M.M.; Dishion, T.J. "Growth and Predictors of Parental Knowledge of Youth Behavior During Early Adolescence. J. Early Adolesc. 2009, 29, 800–825. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Zhang, W.; Yu, C.; Bao, Z. Early Adolescent Internet Game Addiction in Context: How Parents, School, and Peers Impact Youth. Comput. Hum. Behav. 2015, 50, 159–168. [Google Scholar] [CrossRef]
- Herzog, J.I.; Schmahl, C. Adverse Childhood Experiences and the Consequences on Neurobiological, Psychosocial, and Somatic Conditions across the Lifespan. Front. Psychiatry 2018, 9, 420. [Google Scholar] [CrossRef]
- Hall, J.R.; Bernat, E.M.; Patrick, C.J. Externalizing Psychopathology and the Error-Related Negativity. Psychol. Sci. 2007, 18, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Van Bodegom, M.; Homberg, J.R.; Henckens, M.J.A.G. Modulation of the Hypothalamic-Pituitary-Adrenal Axis by Early Life Stress Exposure. Front. Cell. Neurosci. 2017, 11, 87. [Google Scholar] [CrossRef]
- Lackner, C.L.; Santesso, D.L.; Dywan, J.; O’Leary, D.D.; Wade, T.J.; Segalowitz, S.J. Adverse Childhood Experiences Are Associated with Self-Regulation and the Magnitude of the Error-Related Negativity Difference. Biol. Psychol. 2018, 132, 244–251. [Google Scholar] [CrossRef]
- Wichstrøm, L.; Stenseng, F.; Belsky, J.; von Soest, T.; Hygen, B.W. Symptoms of Internet Gaming Disorder in Youth: Predictors and Comorbidity. J. Abnorm. Child Psychol. 2019, 47, 71–83. [Google Scholar] [CrossRef]
- Liau, A.K.; Neo, E.C.; Gentile, D.A.; Choo, H.; Sim, T.; Li, D.; Khoo, A. Impulsivity, Self-Regulation, and Pathological Video Gaming among Youth: Testing a Mediation Model. Asia Pac. J. Public Health 2015, 27, NP2188–NP2196. [Google Scholar] [CrossRef]
- Rasmussen, L.J.H.; Moffitt, T.E.; Arseneault, L.; Danese, A.; Eugen-Olsen, J.; Fisher, H.L.; Harrington, H.; Houts, R.; Matthews, T.; Sugden, K. Association of Adverse Experiences and Exposure to Violence in Childhood and Adolescence with Inflammatory Burden in Young People. JAMA Pediatrics 2020, 174, 38–47. [Google Scholar] [CrossRef]
- Fujiwara, T.; Kawakami, N.; Group World Mental Health Japan Survey. Association of Childhood Adversities with the First Onset of Mental Disorders in Japan: Results from the World Mental Health Japan, 2002–2004. J. Psychiatr. Res. 2011, 45, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Yoshihama, M.; Horrocks, J. Risk of Intimate Partner Violence: Role of Childhood Sexual Abuse and Sexual Initiation in Women in Japan. Child. Youth Serv. Rev. 2010, 32, 28–37. [Google Scholar] [CrossRef]
- Ishii, T.; Asukai, N.; Konishi, T.; Inamoto, E.; Kageyama, H. Mental Health Effects of Child Sexual Victimization in Japan. Jpn. J. Ment. Health 2002, 15, 23–28. [Google Scholar]
- Pandey, A.; Hale, D.; Das, S.; Goddings, A.; Blakemore, S.; Viner, R.M. Effectiveness of Universal Self-Regulation–Based Interventions in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatrics 2018, 172, 566–575. [Google Scholar] [CrossRef]
- Rose, T.; Barker, M.; Jacob, C.M.; Morrison, L.; Lawrence, W.; Strömmer, S.; Vogel, C.; Woods-Townsend, K.; Farrell, D.; Inskip, H. A Systematic Review of Digital Interventions for Improving the Diet and Physical Activity Behaviors of Adolescents. J. Adolesc. Health 2017, 61, 669–677. [Google Scholar] [CrossRef]
- Pluta, B.; Bronikowska, M.; Tomczak, M.; Laudańska-Krzemińska, I.; Bronikowski, M. Family Leisure-Time Physical Activities–Results of the “Juniors for Seniors” 15-Week Intervention Programme. Biomed. Hum. Kinet. 2017, 9, 165–174. [Google Scholar] [CrossRef]
- Cronholm, F.; Rosengren, B.E.; Karlsson, C.; Karlsson, M.K. A Physical Activity Intervention Program in School Is Also Accompanied by Higher Leisure-Time Physical Activity: A Prospective Controlled 3-Year Study in 194 Prepubertal Children. J. Phys. Act. Health 2017, 14, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Krossbakken, E.; Torsheim, T.; Mentzoni, R.A.; King, D.L.; Bjorvatn, B.; Lorvik, I.M.; Pallesen, S. The Effectiveness of a Parental Guide for Prevention of Problematic Video Gaming in Children: A Public Health Randomized Controlled Intervention Study. J. Behav. Addict. 2018, 7, 52–61. [Google Scholar] [CrossRef] [PubMed]
| Total | Grade | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 4th (n = 4654; 68.5%) | 6th (n = 1016; 14.9%) | 8th (n = 1129; 16.6%) | |||||||
| n or Mean | % or SD | n or Mean | % or SD | n or Mean | % or SD | n or Mean | % or SD | ||
| Child’s sex | Male | 3375 | 49.6 | 2342 | 50.3 | 491 | 48.3 | 542 | 48.0 |
| Female | 3422 | 50.3 | 2311 | 49.7 | 525 | 51.7 | 586 | 51.9 | |
| Missing | 2 | 0.1 | 1 | 0 | 0 | 0 | 1 | 0.1 | |
| Number of siblings | No sibling | 3334 | 49.0 | 2283 | 49.1 | 483 | 47.5 | 568 | 50.3 |
| 1 | 1725 | 25.4 | 1146 | 24.6 | 274 | 27.0 | 305 | 27.0 | |
| 2 | 351 | 5.2 | 257 | 5.5 | 39 | 3.8 | 55 | 4.9 | |
| 3+ | 92 | 1.4 | 61 | 1.3 | 15 | 1.5 | 16 | 1.4 | |
| Missing | 1297 | 19.1 | 907 | 19.5 | 205 | 20.2 | 185 | 16.4 | |
| Maternal age | <30 | 48 | 0.7 | 44 | 0.9 | 4 | 0.4 | 0 | 0 |
| 30–34 | 563 | 8.3 | 455 | 9.8 | 64 | 6.3 | 44 | 3.9 | |
| 35–39 | 1508 | 22.2 | 1162 | 25.0 | 208 | 20.5 | 138 | 12.2 | |
| 40–44 | 2460 | 36.2 | 1687 | 36.2 | 361 | 35.5 | 412 | 36.5 | |
| 45+ | 1967 | 28.9 | 1145 | 24.6 | 341 | 33.6 | 481 | 42.6 | |
| Missing | 253 | 3.7 | 161 | 3.5 | 38 | 3.7 | 54 | 4.8 | |
| Cumulative ACE total score | 0 | 4093 | 60.2 | 2719 | 58.4 | 659 | 64.9 | 715 | 63.3 |
| 1 | 1318 | 19.4 | 894 | 19.2 | 190 | 18.7 | 234 | 20.7 | |
| 2 | 946 | 13.9 | 688 | 14.8 | 120 | 11.8 | 138 | 12.2 | |
| 3+ | 442 | 6.5 | 353 | 7.6 | 47 | 4.6 | 42 | 3.7 | |
| Time spent playing video game per day (weekdays) | Not at all | 1553 | 22.8 | 1126 | 24.2 | 212 | 20.9 | 215 | 19.0 |
| 30 min | 1494 | 22.0 | 1124 | 24.2 | 198 | 19.5 | 172 | 15.2 | |
| 1 h | 1228 | 18.1 | 889 | 19.1 | 169 | 16.6 | 170 | 15.1 | |
| 1 h and a half | 714 | 10.5 | 466 | 10.0 | 132 | 13.0 | 116 | 10.3 | |
| 2 h | 569 | 8.4 | 338 | 7.3 | 104 | 10.2 | 127 | 11.2 | |
| 2 h and a half | 346 | 5.1 | 212 | 4.6 | 66 | 6.5 | 68 | 6.0 | |
| 3 h | 209 | 3.1 | 115 | 2.5 | 32 | 3.1 | 62 | 5.5 | |
| More than 3 h | 686 | 10.1 | 384 | 8.3 | 103 | 10.1 | 199 | 17.6 | |
| Total | 4th | 6th | 8th | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| 1. Single parenthood | 985 | 14.5 | 599 | 12.9 | 157 | 15.5 | 229 | 20.3 |
| 2. Parental history of psychiatric disorders | 505 | 7.4 | 354 | 7.6 | 59 | 5.8 | 92 | 8.1 |
| 3. Physical abuse from parents (hit, slap) | 616 | 9.1 | 461 | 9.9 | 76 | 7.5 | 79 | 7.0 |
| 4. Psychological abuse from parents (verb) | 294 | 4.3 | 213 | 4.6 | 41 | 4.0 | 40 | 3.5 |
| 5. Witness of domestic violence between parents | 291 | 4.3 | 201 | 4.3 | 47 | 4.6 | 43 | 3.8 |
| 6. Neglect from parents (out, unfed) | 543 | 8.0 | 423 | 9.1 | 54 | 5.3 | 66 | 5.8 |
| 7. Peer isolation | 875 | 12.9 | 679 | 14.6 | 99 | 9.7 | 97 | 8.6 |
| 8. Lower household income (<3,000,000) | 750 | 11.0 | 486 | 10.4 | 119 | 11.7 | 145 | 12.8 |
| N and Percent (%) Exposed to Another ACEs | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Single Parenthood | 2. Parental History of Psychiatric Disorders | 3. Physical Abuse from Parents (Hit, Slap) | 4. Psychological Abuse from Parents (Verb) | 5. Witness of Domestic Violence between Parents | 6. Neglect from Parents (Out, Unfed) | 7. Peer Isolation | 8. Lower Household Income (<3,000,000) | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| 1. Single parenthood | 112 | 11.4 | 119 | 12.4 | 46 | 4.8 | 30 | 3.1 | 102 | 10.6 | 140 | 14.7 | 487 | 61.5 | ||
| 2. Parental history of psychiatric disorders | 112 | 22.2 | 67 | 13.4 | 48 | 9.6 | 39 | 7.8 | 60 | 12.0 | 70 | 14.1 | 99 | 22.1 | ||
| 3. Physical abuse from parents (hit, slap) | 119 | 19.3 | 67 | 10.9 | 122 | 19.9 | 71 | 11.6 | 174 | 28.3 | 93 | 15.6 | 105 | 20.0 | ||
| 4. Psychological abuse from parents (verb) | 46 | 15.7 | 48 | 16.3 | 122 | 41.6 | 67 | 22.9 | 82 | 27.9 | 58 | 20.2 | 43 | 16.5 | ||
| 5. Witness of domestic violence between parents | 30 | 10.3 | 39 | 13.4 | 71 | 24.4 | 67 | 23.0 | 60 | 20.6 | 46 | 16.1 | 43 | 17.1 | ||
| 6. Neglect from parents (out, unfed) | 102 | 18.8 | 60 | 11.1 | 174 | 32.2 | 82 | 15.2 | 60 | 8.1 | 90 | 17.0 | 88 | 18.7 | ||
| 7. Peer isolation | 24 | 26.4 | 70 | 8.0 | 93 | 10.8 | 58 | 6.7 | 46 | 5.3 | 90 | 10.5 | 119 | 15.5 | ||
| 8. Lower household income (<3,000,000) | 487 | 64.9 | 99 | 13.2 | 105 | 14.4 | 43 | 5.9 | 43 | 5.9 | 88 | 12.0 | 119 | 16.3 | ||
| Crude | Model 1 | Model 2 | Model 3 | ||
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| ACE total score | 0 | Ref | Ref | ||
| 1 | 1.29 (1.12–1.48) | 1.28 (1.10–1.48) | |||
| 2 | 1.49 (1.28–1.75) | 1.25 (1.06–1.48) | |||
| 3+ | 1.67 (1.34–2.06) | 1.44 (1.14–1.82) | |||
| p for trend < 0.001 | p for trend < 0.001 | ||||
| Single parenthood | No | Ref | Ref | Ref | |
| Yes | 1.58 (1.35–1.84) | 1.60 (1.35–1.90) | 1.55 (1.21–1.97) | ||
| Parental history of psychiatric disorders | No | Ref | Ref | Ref | |
| Yes | 1.64 (1.34–2.02) | 1.68 (1.35–2.10) | 1.62 (1.28–2.04) | ||
| Physical abuse from parents (hit, slap) | No | Ref | Ref | ||
| Yes | 1.05 (0.86–1.27) | 0.93 (0.76–1.14) | |||
| Psychological abuse from parents (verb) | No | Ref | Ref | ||
| Yes | 1.04 (0.79–1.37) | 1.05 (0.78–1.41) | |||
| Witness of domestic violence between parents | No | Ref | Ref | ||
| Yes | 1.08 (0.83–1.39) | 1.14 (0.87–1.50) | |||
| Neglect from parents (out, unfed) | No | Ref | Ref | ||
| Yes | 1.05 (0.85–1.28) | 0.95 (0.77–1.17) | |||
| Peer isolation | No | Ref | Ref | Ref | |
| Yes | 1.60 (1.37–1.86) | 1.31 (1.10–1.54) | 1.32 (1.10–1.58) | ||
| Lower household income (<3,000,000) | No | Ref | Ref | Ref | |
| Yes | 1.49 (1.25–1.77) | 1.51 (1.24–1.83) | 1.15 (0.90–1.47) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doi, S.; Isumi, A.; Fujiwara, T. Association between Adverse Childhood Experiences and Time Spent Playing Video Games in Adolescents: Results from A-CHILD Study. Int. J. Environ. Res. Public Health 2021, 18, 10377. https://doi.org/10.3390/ijerph181910377
Doi S, Isumi A, Fujiwara T. Association between Adverse Childhood Experiences and Time Spent Playing Video Games in Adolescents: Results from A-CHILD Study. International Journal of Environmental Research and Public Health. 2021; 18(19):10377. https://doi.org/10.3390/ijerph181910377
Chicago/Turabian StyleDoi, Satomi, Aya Isumi, and Takeo Fujiwara. 2021. "Association between Adverse Childhood Experiences and Time Spent Playing Video Games in Adolescents: Results from A-CHILD Study" International Journal of Environmental Research and Public Health 18, no. 19: 10377. https://doi.org/10.3390/ijerph181910377
APA StyleDoi, S., Isumi, A., & Fujiwara, T. (2021). Association between Adverse Childhood Experiences and Time Spent Playing Video Games in Adolescents: Results from A-CHILD Study. International Journal of Environmental Research and Public Health, 18(19), 10377. https://doi.org/10.3390/ijerph181910377






