Characteristics of Presentations to the Emergency Department Following Attempted Suicide with Drugs
Abstract
:1. Introduction
2. Materials and Methods
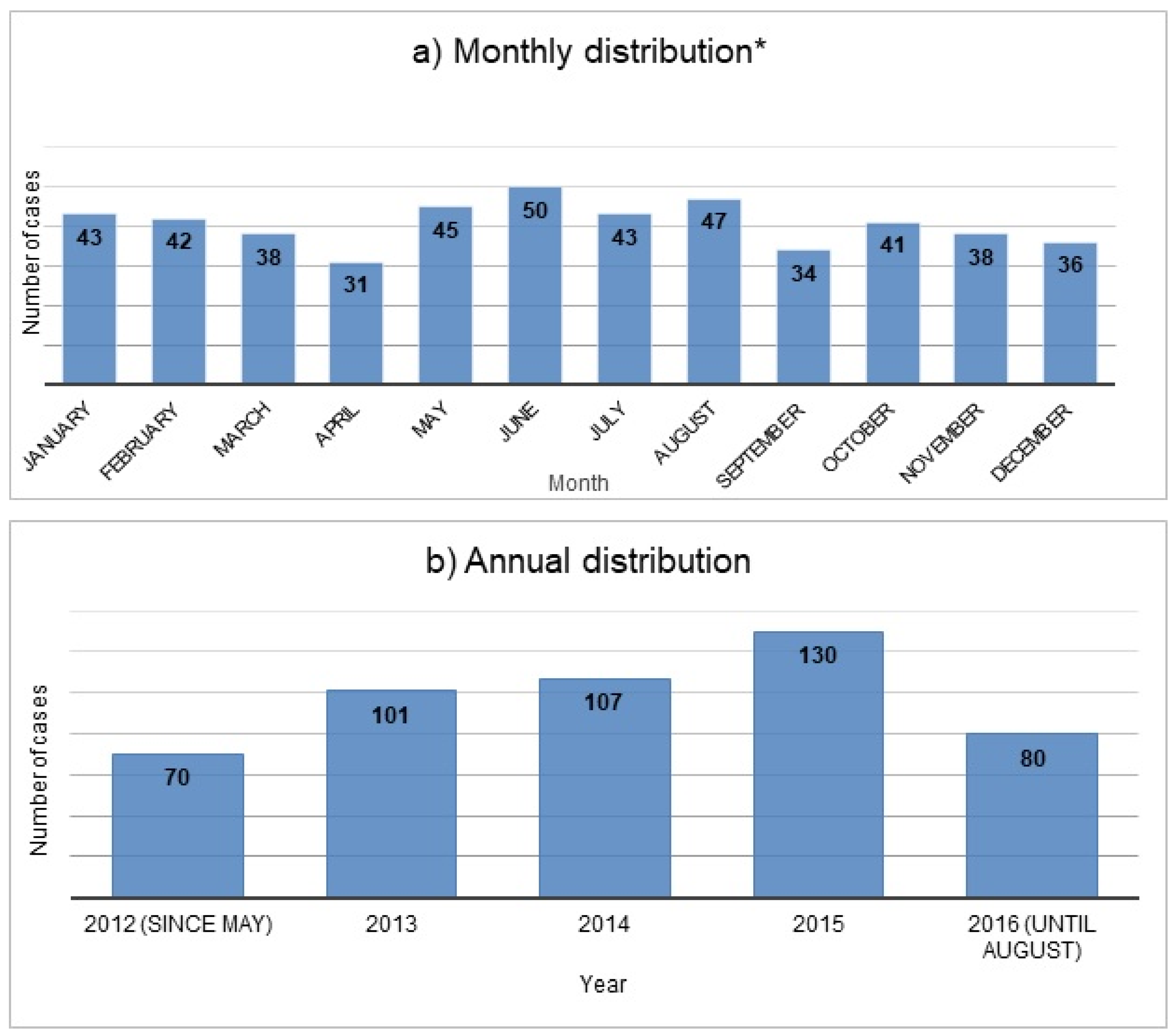
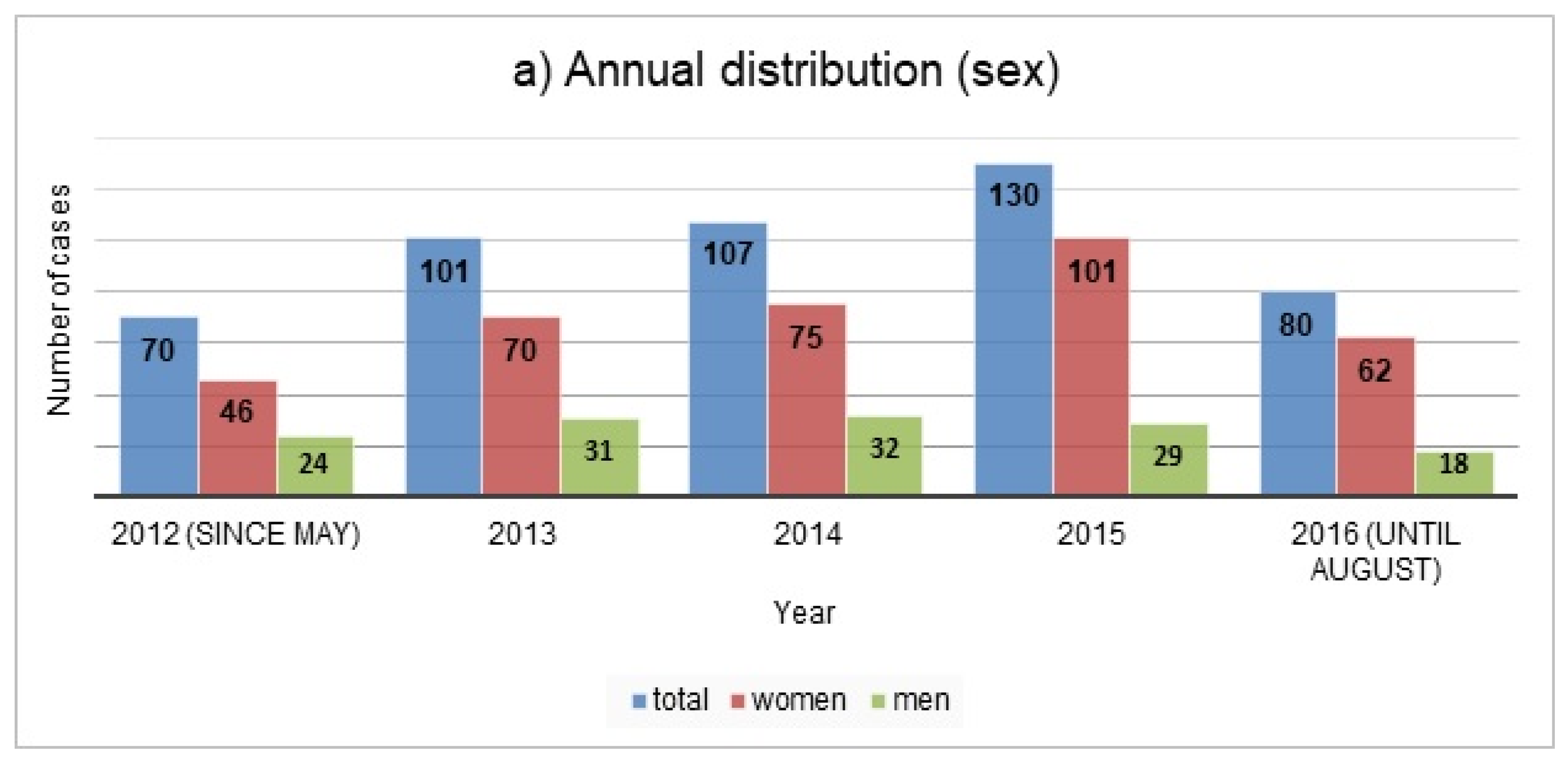
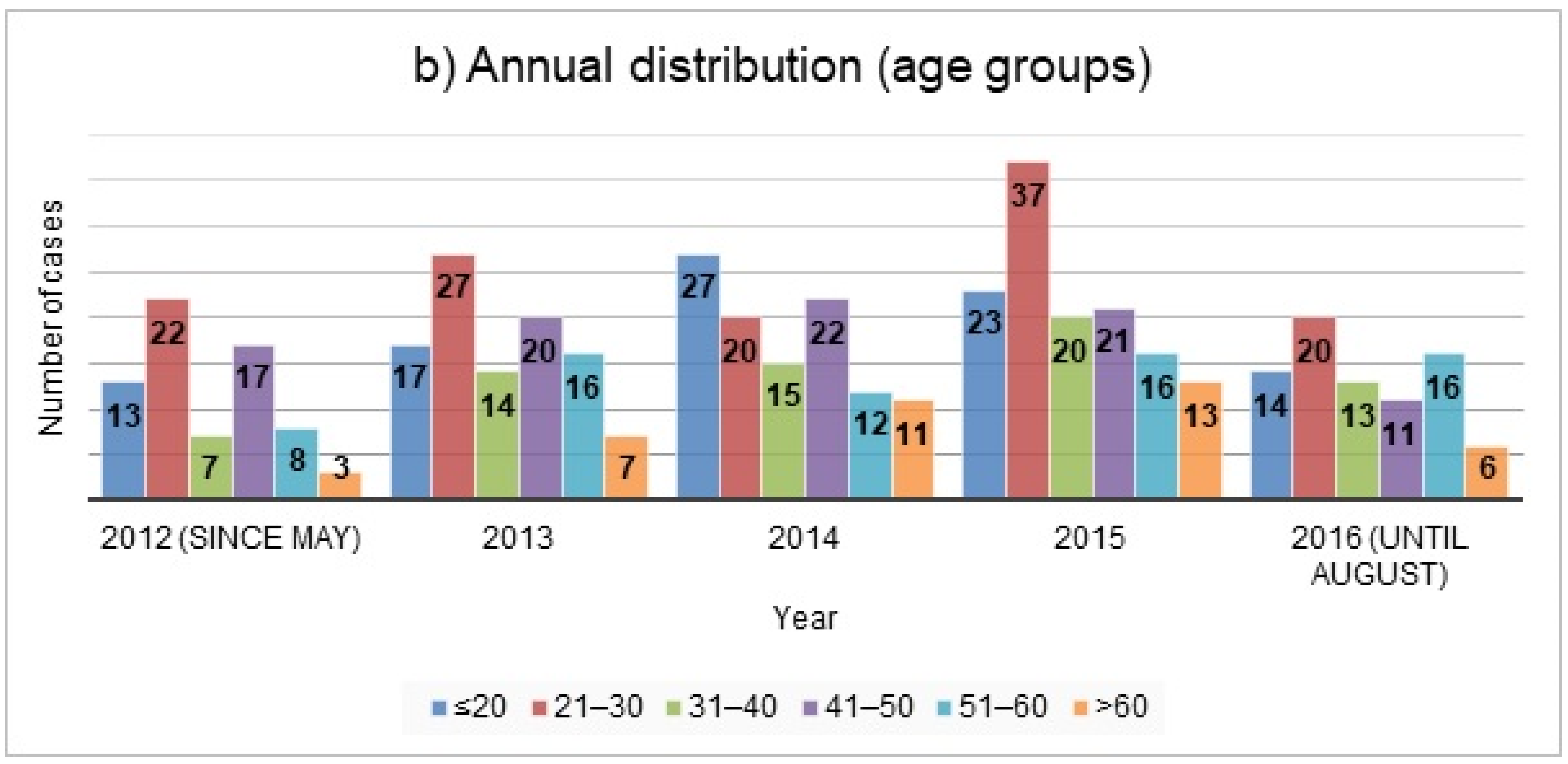
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Suicide. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 25 August 2021).
- Borges, G.; Nock, M.K.; Abad, J.M.H.; Hwang, I.; Sampson, N.A.; Alonso, J.; Andrade, L.H.; Angermeyer, M.C.; Beautrais, A.; Bromet, E.; et al. Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J. Clin. Psychiatry 2010, 71, 1617–1628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). Preventing Suicide-a Global Imperative. 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/131056/97892?sequence=1 (accessed on 23 September 2021).
- Bostwick, J.M.; Pabbati, C.; Geske, J.R.; McKean, A.J. Suicide Attempt as a Risk Factor for Completed Suicide: Even More Lethal Than We Knew. Am. J. Psychiatry 2016, 173, 1094–1100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peter, C.; Tuch, A. Suizidgedanken und Suizidversuche in der Schweizer Bevölkerung. Obsan Bulletin, 2019, 7/2019, Neuchâtel: Schweizerisches Gesundheitsobservatorium; Available also in French (BFS-Number: 1034-1907); Schweizerisches Gesundheitsobservatorium (Obsan): Neuchâtel, Switzerland, 2019. [Google Scholar]
- Muster, C.; Exadaktylos, A.; Haberkern, M. Dosis sola facit venenum? Welches Outcome haben Intoxikationen in einem Universitätsspital der Schweiz [Dosis sola facit venenum: Outcome of intoxications in a Swiss university hospital]. Praxis (Bern 1994) 2012, 101, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Steffen, T.; Maillart, A.; Michel, K.; Reisch, T. Monitoring des suizidalen Verhaltens in der Agglomeration Bern im Rahmen der WHO/MONSUE Multicenter Study on Suicidal Behaviour und des Berner Bündnisses gegen Depressionen. Bericht im Auftrag des Bundesamtes für Gesundheit. Bern: Universitäre Psychiatrische Dienste Bern (UPD). 2011. Available online: https://www.npg-rsp.ch/fileadmin/npg-rsp/Themen/Fachthemen/Reisch_2011_Suizidales_Verhalten_Bern.pdf (accessed on 25 August 2021).
- Muheim, F.; Eichhorn, M.; Berger, P.; Czernin, S.; Stoppe, G.; Keck, M.; Riecher-Rössler, A. Suicide attempts in the county of Basel: Results from the WHO/EURO Multicentre Study on Suicidal Behaviour. Swiss Med Wkly 2013, 143, w13759. [Google Scholar] [CrossRef]
- Maier, R.; Stieglitz, R.D.; Marsch, S.C.; Riecher-Rossler, A. Patienten mit intensivpflichtigen medikamentösen Suizidversuchen—Risikoprofil und Verlauf [Patients in intensive care after a suicide attempt with legal drugs—risk profile and course]. Fortschr. Neurol. Psychiatr. 2011, 79, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Albert, M.; McCaig, L.F.; Uddin, S. Emergency department visits for drug poisoning: United States, 2008–2011. NCHS Data Brief 2015, 196, 1–8. [Google Scholar]
- Griffin, E.; Corcoran, P.; Cassidy, L.; O’Carroll, A.; Perry, I.J.; Bonner, B. Characteristics of hospital-treated intentional drug overdose in Ireland and Northern Ireland. BMJ Open 2014, 4, e005557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vancayseele, N.; Portzky, G.; van Heeringen, K. Increase in Self-Injury as a Method of Self-Harm in Ghent, Belgium: 1987–2013. PLoS ONE 2016, 11, e0156711. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Kim, M.; Kim, Y.R.; Choi, K.H.; Lee, K.U. High Prevalence of Psychotropics Overdose among Suicide Attempters in Korea. Clin. Psychopharmacol. Neurosci. 2015, 13, 302–307. [Google Scholar] [CrossRef] [Green Version]
- University of Oxford, Department of Psychiatry, Multicentre Study of Self-Harm in England. Available online: https://www.psych.ox.ac.uk/research/csr/ahoj (accessed on 23 September 2021).
- Casey, D.; Geulayov, G.; Bale, E.; Brand, F.; Clements, C.; Kapur, N.; Ness, J.; Patel, A.; Waters, K.; Hawton, K. Paracetamol self-poisoning: Epidemiological study of trends and patient characteristics from the multicentre study of self-harm in England. J. Affect. Disord. 2020, 276, 699–706. [Google Scholar] [CrossRef]
- Groupe Romand Prévention Suicide. Observatoire Romand des Tentatives de Suicide. 2019. Available online: https://www.bag.admin.ch/bag/de/home/strategie-und-politik/politische-auftraege-und-aktionsplaene/aktionsplan-suizidpraevention/praxisbeispiele-suche/P032_orts.html (accessed on 23 September 2021).
- Datenlage zu Suiziden und Suizidversuchen in der Schweiz. Available online: https://www.bag.admin.ch/bag/de/home/strategie-und-politik/politische-auftraege-und-aktionsplaene/aktionsplan-suizidpraevention/Datenlage-Suizide-Suizidversuche-Schweiz.html (accessed on 25 August 2021).
- Doak, M.W.; Nixon, A.C.; Lupton, D.J.; Waring, W.S. Self-poisoning in older adults: Patterns of drug ingestion and clinical outcomes. Age Ageing 2009, 38, 407–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawton, K.; Simkin, S.; Deeks, J.J.; O’Connor, S.; Keen, A.; Altman, D.G.; Philo, G.; Bulstrode, C. Effects of a drug overdose in a television drama on presentations to hospital for self poisoning: Time series and questionnaire study. BMJ 1999, 318, 972–977. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCullumsmith, C. Laying the groundwork for standardized assessment of suicidal behavior. J. Clin. Psychiatry 2015, 76, e1333-5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nock, M.K. Self-injury. Annu. Rev. Clin. Psychol. 2010, 6, 339–363. [Google Scholar] [CrossRef] [PubMed]
- Aithal, G.P.; Watkins, P.B.; Andrade, R.J.; Larrey, D.; Molokhia, M.; Takikawa, H.; Hunt, C.M.; Wilke, R.A.; Avigan, M.; Kaplowitz, N.; et al. Case definition and phenotype standardization in drug-induced liver injury. Clin. Pharmacol. Ther. 2011, 89, 806–815. [Google Scholar] [CrossRef] [PubMed]
- Drew, B.J.; Ackerman, M.J.; Funk, M.; Gibler, W.B.; Kligfield, P.; Menon, V.; Philippides, G.J.; Roden, D.M.; Zareba, W.; American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology; et al. Prevention of torsade de pointes in hospital settings: A scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation 2010, 121, 1047–1060. [Google Scholar] [CrossRef]
- Alere TM Triage® TOX Drug Screen Product Insert. Rapid Qualitative Simultaneous Detection of Drug and/or the Major Urinary Metabolites of 10 different Drug Classes (11 Unique Assays). Quidel 2020. Available online: /www.alere.com/en/home/product-details/triage-tox-drug-screen-au.html (accessed on 23 September 2021).
- Persson, H.E.; Sjoberg, G.K.; Haines, J.A.; de Garbino, J.P. Poisoning severity score. Grading of acute poisoning. J. Toxicol. Clin. Toxicol. 1998, 36, 205–213. [Google Scholar] [CrossRef]
- Hepp, U.; Ring, M.; Frei, A.; Rössler, W.; Schnyder, U.; Ajdacic-Gross, V. Suicide trends diverge by method: Swiss suicide rates 1969–2005. Eur. Psychiatry 2010, 25, 129–135. [Google Scholar] [CrossRef]
- Townsend, E.; Hawton, K.; Harriss, L.; Bale, E.; Bond, A. Substances used in deliberate self-poisoning 1985-1997: Trends and associations with age, gender, repetition and suicide intent. Soc. Psychiatry Psychiatr. Epidemiol. 2001, 36, 228–234. [Google Scholar] [CrossRef]
- Gjerden, P.; Bramness, J.G.; Tvete, I.F.; Slørdal, L. The antipsychotic agent quetiapine is increasingly not used as such: Dispensed prescriptions in Norway 2004–2015. Eur. J. Clin. Pharmacol. 2017, 73, 1173–1179. [Google Scholar] [CrossRef]
- Helsana Arzneimittelreport. 2020. Available online: file:///C:/Users/MDPI/AppData/Local/Temp/arzneimittelreport-2020.pdf (accessed on 25 August 2021).
- Rudd, R.A.; Seth, P.; David, F.; Scholl, L. Increases in Drug and Opioid-Involved Overdose Deaths—United States, 2010–2015. Morb. Mortal. Wkly. Rep. 2016, 65, 1445–1452. [Google Scholar] [CrossRef] [Green Version]
- Xiang, Y.; Zhao, W.; Xiang, H.; Smith, G.A. ED visits for drug-related poisoning in the United States, 2007. Am. J. Emerg. Med. 2012, 30, 293–301. [Google Scholar] [CrossRef]
- Daly, C.; Griffin, E.; Ashcroft, D.M.; Webb, R.T.; Perry, I.J.; Arensman, E. Frequently used drug types and alcohol involvement in intentional drug overdoses in Ireland: A national registry study. Eur. J. Public Health 2018, 28, 681–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arzneimittelinformation-Publikationssystem (AIPS) (Electronic Version). Available online: http://www.swissmedicinfo.ch/ (accessed on 25 August 2021).
- Hawton, K.; Bergen, H.; Casey, D.; Simkin, S.; Palmer, B.; Cooper, J.; Kapur, N.; Horrocks, J.; House, A.; Lilley, R.; et al. Self-harm in England: A tale of three cities. Multicentre study of self-harm. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Hughes, B.; Durran, A.; Langford, N.J.; Mutimer, D. Paracetamol poisoning--impact of pack size restrictions. J. Clin. Pharm. Ther. 2003, 28, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Hawton, K.; Townsend, E.; Deeks, J.; Appleby, L.; Gunnell, D.; Bennewith, O.; Cooper, J. Effects of legislation restricting pack sizes of paracetamol and salicylate on self poisoning in the United Kingdom: Before and after study. BMJ 2001, 322, 1203–1207. [Google Scholar] [CrossRef] [Green Version]
- Sheen, C.L.; Dillon, J.F.; Bateman, D.N.; Simpson, K.J.; MacDonald, T.M. Paracetamol-related deaths in Scotland, 1994–2000. Br. J. Clin. Pharmacol. 2002, 54, 430–432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morgan, O.; Majeed, A. Restricting paracetamol in the United Kingdom to reduce poisoning: A systematic review. J. Public Health (Oxf.) 2005, 27, 12–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conejero, I.; Olié, E.; Courtet, P.; Calati, R. Suicide in older adults: Current perspectives. Clin. Interv. Aging 2018, 13, 691–699. [Google Scholar] [CrossRef] [Green Version]
- Shah, A.; Bhat, R.; Zarate-Escudero, S.; DeLeo, D.; Erlangsen, A. Suicide rates in five-year age-bands after the age of 60 years: The international landscape. Aging Ment. Health 2016, 20, 131–138. [Google Scholar] [CrossRef]
- Erlangsen, A.; Lind, B.D.; Stuart, E.A.; Qin, P.; Stenager, E.; Larsen, K.J.; Wang, A.G.; Hvid, M.; Nielsen, A.C.; Pedersen, C.M.; et al. Short-term and long-term effects of psychosocial therapy for people after deliberate self-harm: A register-based, nationwide multicentre study using propensity score matching. Lancet Psychiatry 2015, 2, 49–58. [Google Scholar] [CrossRef]
| Number of Cases (%) | |
|---|---|
| Sex | |
| Male | 134 (27) |
| Female | 354 (73) |
| Age group (years) | |
| ≤20 | 94 (19) |
| 21–30 | 126 (26) |
| 31–40 | 69 (14) |
| 41–50 | 91 (19) |
| 51–60 | 68 (14) |
| >60 | 40 (8) |
| Time of Presentation | |
| Night arrival | 141 (29) |
| Weekend arrival | 144 (30) |
| Admission to ED | |
| Self-presentation | 84 (17) |
| Brought by rescue services/police | 404 (83) |
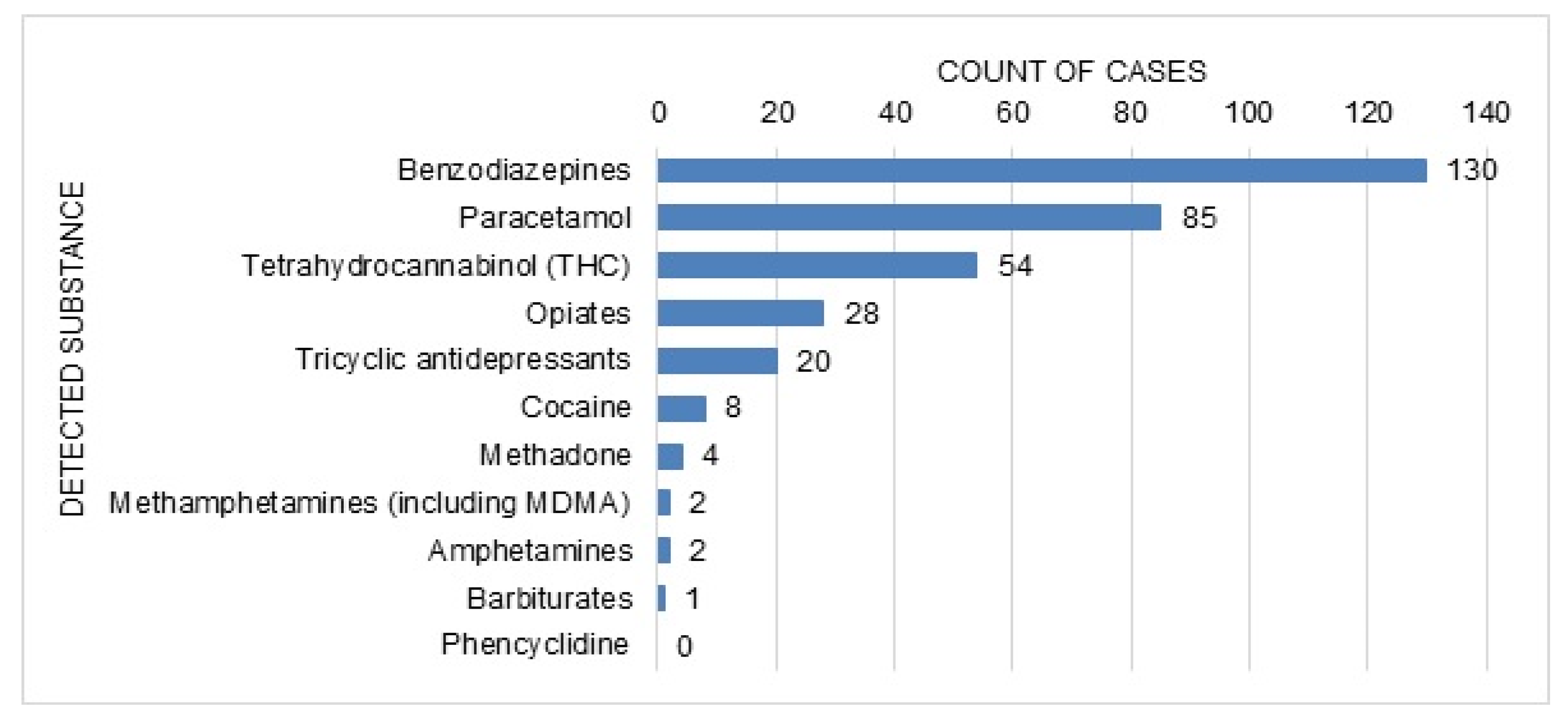
| Reported Concomitant Use | |
| Ethanol | 138 (28) |
| Recreational drug use | 20 (4) |
| Consumption of multiple drugs | |
| Yes | 258 (53) |
| No | 230 (47) |
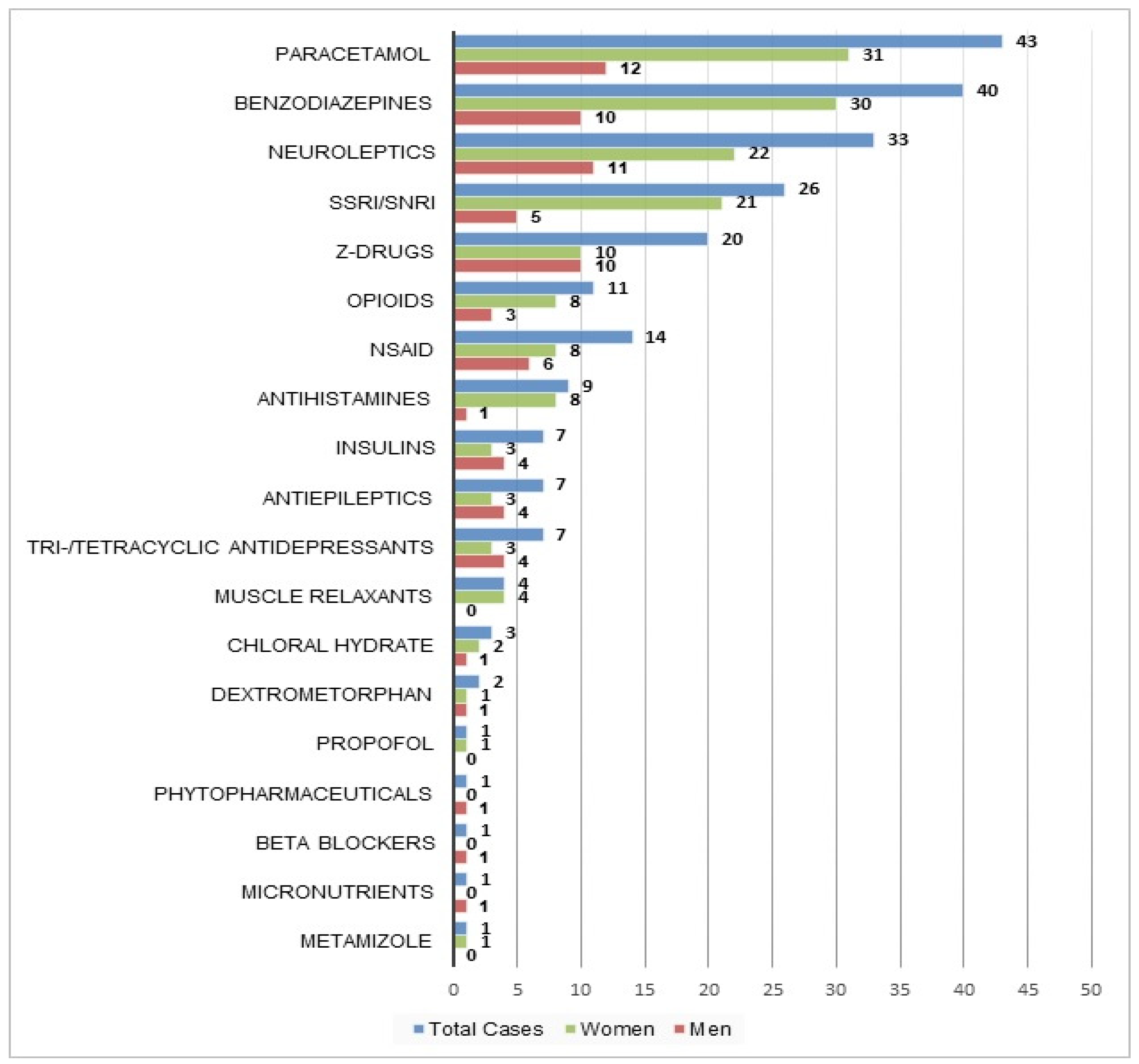
| Substance/Drug Class | Number of Total Cases (% of Total Cases) | Number of Monointoxication Cases (% of Monointoxication Cases) |
|---|---|---|
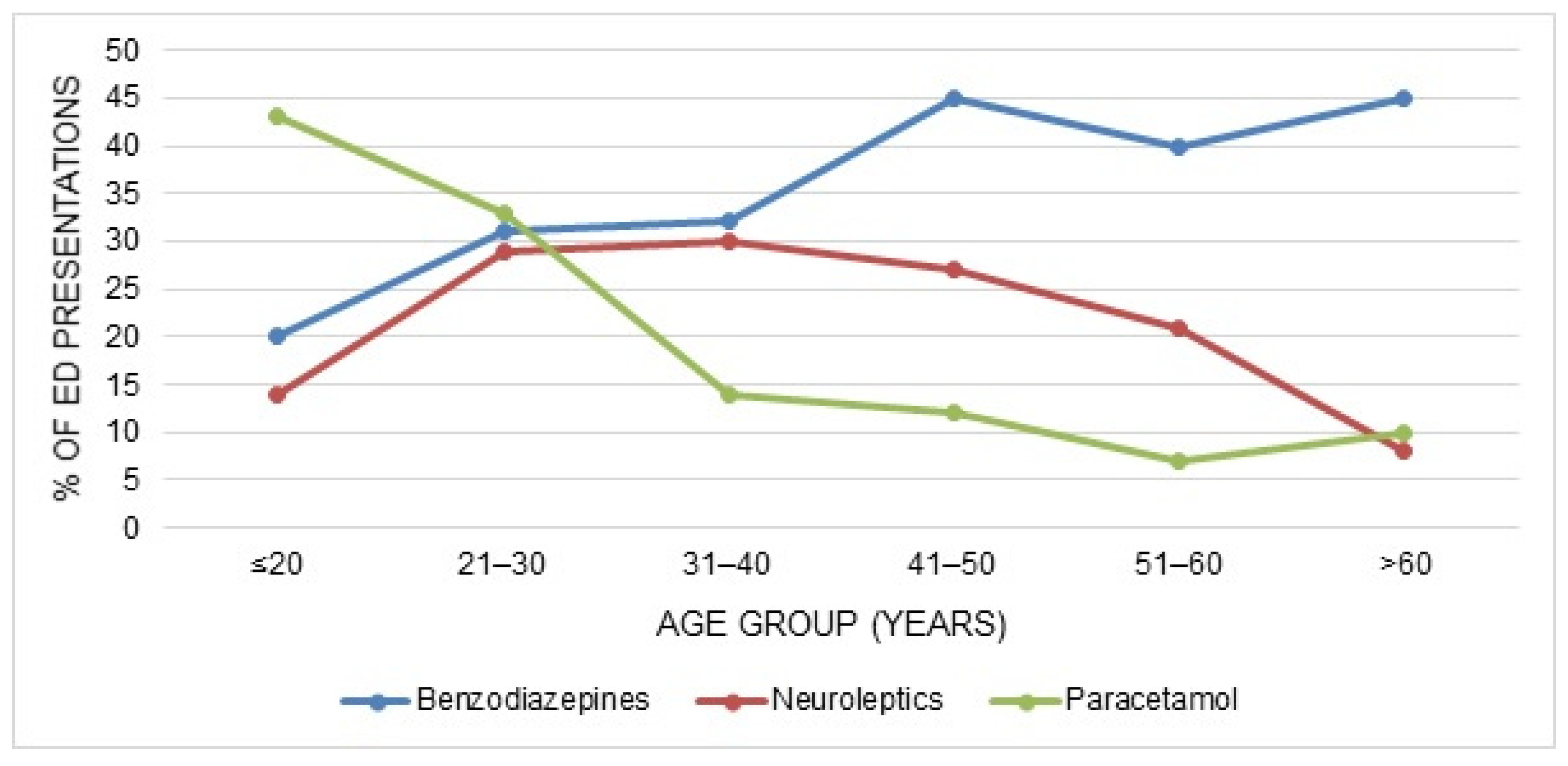
| Benzodiazepines | 167 (34) | 40 (17) |
| Neuroleptics | 114 (23) | 33 (14) |
| Paracetamol | 111 (23) | 43 (19) |
| SSRI/SNRI | 94 (19) | 26 (11) |
| NSAID | 77 (16) | 14 (6) |
| Z-Drugs | 72 (15) | 20 (9) |
| Opioids | 46 (9) | 11 (5) |
| Tri-/Tetracyclic antidepressants | 41 (8) | 7 (3) |
| Antiepileptics | 28 (6) | 7 (3) |
| Antihistamines | 25 (5) | 9 (4) |
| Lithium | 22 (5) | |
| Metamizole | 16 (3) | 1 (<1) |
| PPI | 15 (3) | |
| Muscle relaxants | 11 (2) | 4 (2) |
| Insulins | 11 (2) | 7 (3) |
| Micronutrients | 8 (2) | 1 (<1) |
| ACE inhibitors | 7 (1) | |
| Diuretics | 7 (1) | |
| Antispasmotics | 7 (1) | |
| Beta blockers | 6 (1) | 1 (<1) |
| Lipid reducers/statins | 6 (1) | |
| Dextrometorphan | 5 (1) | 2 (1) |
| Phytopharmaceuticals | 5 (1) | 1 (<1) |
| Calcium antagonists | 4 (1) | |
| Sympathomimetics | 4 (1) | |
| Chloral hydrate | 3 (1) | 3 (1) |
| Methylphenidate | 3 (1) | |
| Thyroid hormones | 3 (1) | |
| Antibiotics | 3 (1) | |
| Anticoagulants | 2 (<1) | |
| Agomelatine | 2 (<1) | |
| Levodopa | 2 (<1) | |
| Antiemetics | 2 (<1) | |
| Loperamide | 2 (<1) | |
| Propofol | 2 (<1) | 1 (<1) |
| Metformin | 2 (<1) | |
| Allopurinol | 2 (<1) | |
| Laxatives | 1 (<1) | |
| Mycophenolate | 1 (<1) | |
| Digoxin | 1 (<1) | |
| Nicorandil | 1 (<1) | |
| Erdosteine | 1 (<1) | |
| Estrogen | 1 (<1) |
| Number of Cases (%) | |
|---|---|
| On arrival | |
| Mildly impaired consciousness, GCS 13–14 | 115 (24) |
| Moderately impaired consciousness, GCS 9–12 | 33 (7) |
| Unconscious, GCS <9 | 21 (4) |
| Tachycardia | 95 (19) |
| Tachypnoea | 49 (10) |
| Bradycardia | 13 (3) |
| Hypertension | 9 (2) |
| Hypotension | 8 (2) |
| Hypothermia | 6 (1) |
| Before or during the presentation | |
| Cardiovascular symptoms | |
| Tachycardia | 119 (24) |
| Hypotension | 33 (7) |
| Hypertension | 28 (6) |
| Bradycardia | 12 (2) |
| Arrhythmias | 1 (<0.5) |
| Cardiovascular arrest | 1 (<0.5) |
| Respiratory symptoms | |
| Tachypnoea | 51 (10) |
| Hypoxia | 13 (3) |
| Bradypnoea | 8 (2) |
| Respiratory depression | 8 (2) |
| Dyspnea | 5 (1) |
| Neurological symptoms | |
| Somnolence | 245 (50) |
| Unconsciousness (defined as lowest GCS <9) | 50 (10) |
| Agitation | 26 (5) |
| Confusion/Desorientation | 20 (4) |
| Vertigo | 19 (4) |
| Cephalgia | 13 (3) |
| Dysarthria | 13 (3) |
| Seizures | 10 (2) |
| Mydriasis | 7 (1) |
| Nystagmus | 5 (1) |
| Miosis | 4 (1) |
| Myoclonia | 4 (1) |
| Extrapyramidal symptoms | 4 (1) |
| Ataxia | 3 (1) |
| Tremor | 3 (1) |
| Hallucinations | 2 (<0.5) |
| Paresthaesia | 2 (<0.5) |
| Amnesia | 1 (<0.5) |
| Gastrointestinal symptoms | |
| Nausea or vomiting | 76 (16) |
| Abdominal pain | 26 (5) |
| Diarrhoea | 3 (1) |
| Laboratory findings | |
| Elevated creatine kinase (CK) | 35 (7) |
| CK >5 ULN | 4 (1) |
| Impaired renal function (eGFR <59 mL/min/1.73 m2) | 21 (4) |
| Drug Induced Liver Injury (DILI) | 6 (1) |
| Miscellanous | |
| Hypothermia | 9 (2) |
| Hypoglycemia | 5 (1) |
| Dry mouth | 3 (1) |
| (Lactic-)acidosis | 3 (1) |
| Sweating | 3 (1) |
| Urinary retention | 2 (<0.5) |
| Tinnitus | 1 (<0.5) |
| Coagulation disorder | 1 (<0.5) |
| Hyperthermia | 1 (<0.5) |
| Number of Cases (%) | |
|---|---|
| Poisoning Severity Score | |
| None | 71 (15) |
| Minor | 231 (47) |
| Moderate | 131 (27) |
| Severe | 55 (11) |
| Outcome | |
| Discharged | 61 (13) |
| Hospitalisation (ICU) | 100 (20) |
| Hospitalisation (normal ward or IMC) | 58 (12) |
| Transfer to psychiatric ward/external psychiatric hospital | 264 (54) |
| Transfer to external hospital | 5 (1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kummer, M.; Müller, T.; Exadaktylos, A.K.; Krähenbühl, S.; Liakoni, E. Characteristics of Presentations to the Emergency Department Following Attempted Suicide with Drugs. Int. J. Environ. Res. Public Health 2021, 18, 10232. https://doi.org/10.3390/ijerph181910232
Kummer M, Müller T, Exadaktylos AK, Krähenbühl S, Liakoni E. Characteristics of Presentations to the Emergency Department Following Attempted Suicide with Drugs. International Journal of Environmental Research and Public Health. 2021; 18(19):10232. https://doi.org/10.3390/ijerph181910232
Chicago/Turabian StyleKummer, Mirjam, Thomas Müller, Aristomenis K. Exadaktylos, Stephan Krähenbühl, and Evangelia Liakoni. 2021. "Characteristics of Presentations to the Emergency Department Following Attempted Suicide with Drugs" International Journal of Environmental Research and Public Health 18, no. 19: 10232. https://doi.org/10.3390/ijerph181910232
APA StyleKummer, M., Müller, T., Exadaktylos, A. K., Krähenbühl, S., & Liakoni, E. (2021). Characteristics of Presentations to the Emergency Department Following Attempted Suicide with Drugs. International Journal of Environmental Research and Public Health, 18(19), 10232. https://doi.org/10.3390/ijerph181910232







