Effectiveness of a Mindfulness and Self-Compassion Standard Training Program versus an Abbreviated Training Program on Stress in Tutors and Resident Intern Specialists of Family and Community Medicine and Nursing in Spain
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Setting
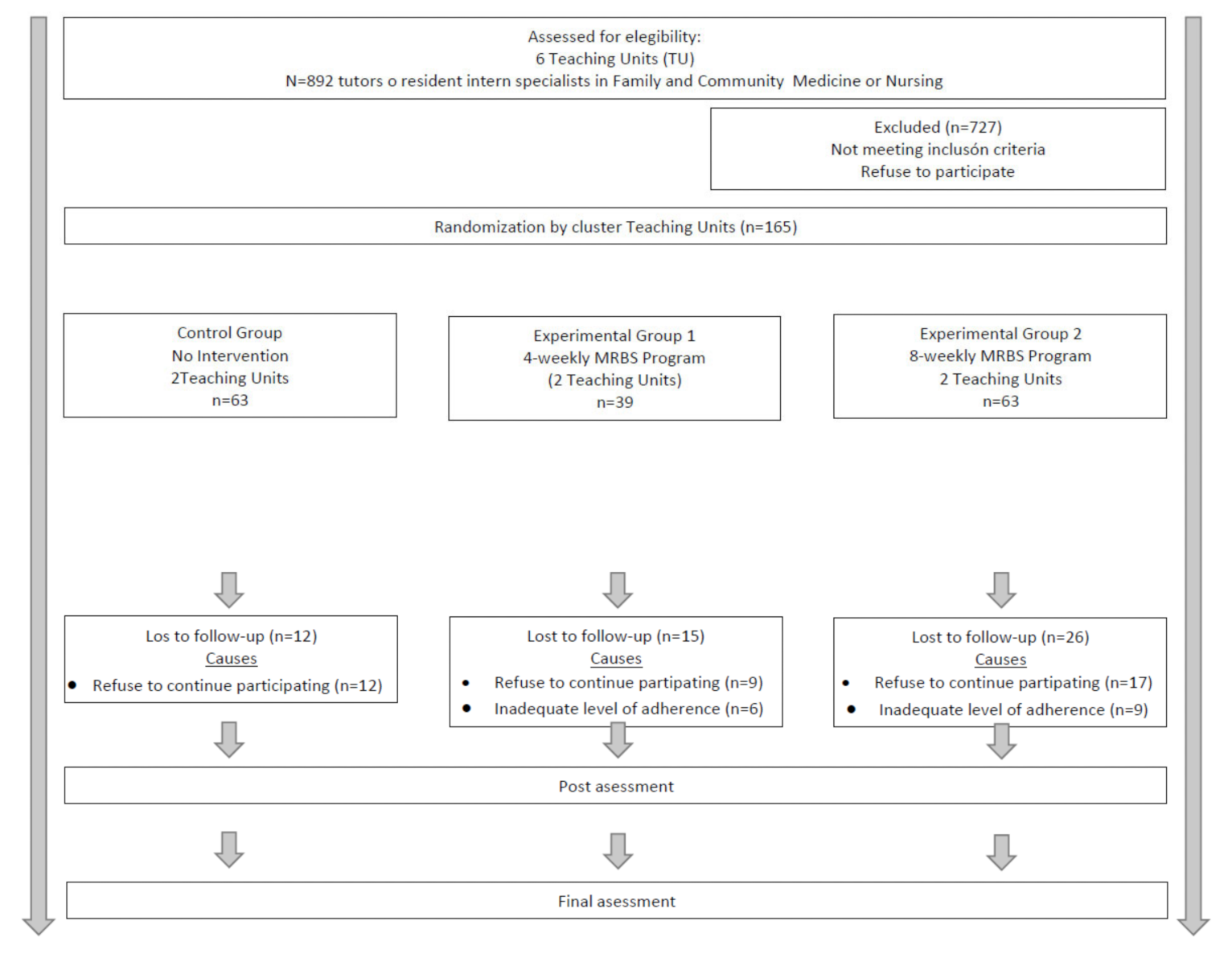
2.2. Study Participants and Recruitment
2.3. Sample Size
2.4. Procedure and Randomisation
2.5. Intervention
2.6. Main Outcomes
2.7. Data Collecption Procedure, Data Management and Monitoring
2.8. Ethical Considerations
2.9. Statistical Analyses
3. Results
3.1. Baseline Characterists of the Study Participants
3.2. Mindfulness and Stress Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: Berlin, Germany, 1984. [Google Scholar]
- Siegrist, J. Adverse health effects of high-effort/low-reward conditions. J. Occup. Health Psychol. 1996, 1, 27–41. [Google Scholar] [CrossRef]
- Jurado, M.D.M.M.; Pérez-Fuentes, M.D.C.; Ruiz, N.F.O.; Márquez, M.D.M.S.; Linares, J.J.G. Self-Efficacy and Emotional Intelligence as Predictors of Perceived Stress in Nursing Professionals. Medicina 2019, 55, 237. [Google Scholar] [CrossRef] [PubMed]
- Viehmann, A.; Kersting, C.; Thielmann, A.; Weltermann, B. Prevalence of chronic stress in general practitioners and practice assistants: Personal, practice and regional characteristics. PLoS ONE 2017, 12, e0176658. [Google Scholar] [CrossRef] [PubMed]
- Schindler, B.A.; Novack, D.H.; Cohen, D.G.; Yager, J.; Wang, D.; Shaheen, N.J.; Guze, P.; Wilkerson, L.; Drossman, D.A. The Impact of the Changing Health Care Environment on the Health and Well-Being of Faculty at Four Medical Schools. Acad. Med. 2006, 81, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Twigg, D.; McCullough, K. Nurse retention: A review of strategies to create and enhance positive practice environments in clinical settings. Int. J. Nurs. Stud. 2014, 51, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Masiero, M.; Cutica, I.; Russo, S.; Mazzocco, K.; Pravettoni, G. Psycho-cognitive predictors of burnout in healthcare professionals working in emergency departments. J. Clin. Nurs. 2018, 27, 2691–2698. [Google Scholar] [CrossRef]
- García-Campayo, J.; Puebla-Guedea, M.; Herrera-Mercadal, P.; Daudén, E. Desmotivación del personal sanitario y síndrome de burnout. Control de las situaciones de tensión. La importancia del trabajo en equipo. Actas Dermo-Sifiliográficas 2016, 107, 400–406. [Google Scholar] [CrossRef]
- Riley, R.; Kokab, F.; Buszewicz, M.; Gopfert, A.; Van Hove, M.; Taylor, A.K.; Teoh, K.; Martin, J.; Appleby, L.; Chew-Graham, C. Protective factors and sources of support in the workplace as experienced by UK foundation and junior doctors: A qualitative study. BMJ Open 2021, 11, e045588. [Google Scholar] [CrossRef]
- Xiang, Y.-T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef]
- Shanafelt, T.; Ripp, J.; Trockel, M. Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. JAMA 2020, 323, 2133. [Google Scholar] [CrossRef]
- Abdoli, N.; Farnia, V.; Jahangiri, S.; Radmehr, F.; Alikhani, M.; Abdoli, P.; Davarinejad, O.; Dürsteler, K.; Brühl, A.; Sadeghi-Bahmani, D.; et al. Sources of Sleep Disturbances and Psychological Strain for Hospital Staff Working during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 6289. [Google Scholar] [CrossRef]
- Shayganfard, M.; Mahdavi, F.; Haghighi, M.; Sadeghi-Bahmani, D.; Brand, S. Sources of Health Anxiety for Hospital Staff Working during the Covid-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 3094. [Google Scholar] [CrossRef]
- Vandevala, T.; Pavey, L.; Chelidoni, O.; Chang, N.-F.; Creagh-Brown, B.; Cox, A. Psychological rumination and recovery from work in intensive care professionals: Associations with stress, burnout, depression and health. J. Intensiv. Care 2017, 5, 1–8. [Google Scholar] [CrossRef]
- Gao, Y.-Q.; Pan, B.-C.; Sun, W.; Wu, H.; Wang, J.-N.; Wang, L. Anxiety symptoms among Chinese nurses and the associated factors: A cross sectional study. BMC Psychiatry 2012, 12, 141. [Google Scholar] [CrossRef] [PubMed]
- Givens, J.L.; Tjia, J. Depressed Medical Studentsʼ Use of Mental Health Services and Barriers to Use. Acad. Med. 2002, 77, 918–921. [Google Scholar] [CrossRef]
- Shapiro, S.L.; Astin, J.A.; Bishop, S.R.; Cordova, M. Mindfulness-Based Stress Reduction for Health Care Professionals: Results From a Randomized Trial. Int. J. Stress Manag. 2005, 12, 164–176. [Google Scholar] [CrossRef]
- Lin, H.-S.; Probst, J.C.; Hsu, Y.-C. Depression among female psychiatric nurses in southern Taiwan: Main and moderating effects of job stress, coping behaviour and social support. J. Clin. Nurs. 2010, 19, 2342–2354. [Google Scholar] [CrossRef]
- Bryant, C.; Fairbrother, G.; Fenton, P. The relative influence of personal and workplace descriptors on stress. Br. J. Nurs. 2000, 9, 876–880. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad. Consumo Programa Formativo de la Especialidad de Medicina Familiar y Comunitaria; Ministerio de Sanidad: Madrid, Spain, 2005.
- Ministerio de Sanidad. Política Social Programa Formativo de la Especialidad de Enfermería Familiar y Comunitaria; España; Ministerio de Sanidad: Madrid, Spain, 2010.
- Magallón-Botaya, R.; Torres, L.A.P.-D.; Atalaya, J.C.V.-M.; Pérula-Jiménez, C.; Lietor-Villajos, N.; Bartolomé-Moreno, C.; Garcia-Campayo, J.; Moreno-Martos, H.; the Minduudd Collaborative Study Group. Mindfulness in primary care healthcare and teaching professionals and its relationship with stress at work: A multicentric cross-sectional study. BMC Fam. Pr. 2021, 22, 1–9. [Google Scholar] [CrossRef]
- Oliver, E.B.; De Albornoz, P.A.C.; López, H.C.; Oliver, E.B. Herramientas para el autocuidado del profesional que atiende a personas que sufren. FMC Form. Medica Contin. Aten. Primaria 2011, 18, 59–65. [Google Scholar] [CrossRef]
- Grossman, P.; Niemann, L.; Schmidt, S.; Walach, H. Mindfulness-based stress reduction and health benefits. J. Psychosom. Res. 2004, 57, 35–43. [Google Scholar] [CrossRef]
- Atanes, A.C.M.; Andreoni, S.; Hirayama, M.S.; Montero-Marin, J.; Barros, V.V.; Ronzani, T.M.; Kozasa, E.H.; Soler, J.; Cebolla, A.; García-Campayo, J.; et al. Mindfulness, perceived stress, and subjective well-being: A correlational study in primary care health professionals. BMC Complement. Altern. Med. 2015, 15, 303. [Google Scholar] [CrossRef]
- Demarzo, M.; Montero-Marin, J.; Cuijpers, P.; del Olmo, E.Z.; Mahtani, K.R.; Vellinga, A.; Vicens, C.; López-Del-Hoyo, Y.; García-Campayo, J. The Efficacy of Mindfulness-Based Interventions in Primary Care: A Meta-Analytic Review. Ann. Fam. Med. 2015, 13, 573–582. [Google Scholar] [CrossRef]
- Asuero, A.M.; Rodriguez-Blanco, T.; Ribera, E.P.; Berenguera, A.; Queraltó, J.M. Evaluación de la efectividad de un programa de mindfulness en profesionales de atención primaria. Gac. Sanit. 2013, 27, 521–528. [Google Scholar] [CrossRef][Green Version]
- Pérula, C.; Pérula de Torres, L.A.; Jiménez García, C.; Pérula de Torres, C.J.; Vaquero Abellán, M. Mindfulness en Enfermería de Atención Primaria y su Relación con el Estrés Laboral. NURE Investig. 2016, 14, 1–9. [Google Scholar]
- Kabat-Zinn, J. Mindfulness-based interventions in context: Past, present, and future. Clin. Psychol. Sci. Pr. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Lomas, T.; Ivtzan, I.; Fu, C. A systematic review of the neurophysiology of mindfulness on EEG oscillations. Neurosci. Biobehav. Rev. 2015, 57, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Walsh, R.; Shapiro, S.L. The meeting of meditative disciplines and western psychology: A mutually enriching dialogue. Am. Psychol. 2006, 61, 227–239. [Google Scholar] [CrossRef]
- Neff, K.D. The Development and Validation of a Scale to Measure Self-Compassion. Self Identit- 2003, 2, 223–250. [Google Scholar] [CrossRef]
- Derksen, F.; Bensing, J.; Lagro-Janssen, A. Effectiveness of empathy in general practice: A systematic review. Br. J. Gen. Pr. 2013, 63, e76–e84. [Google Scholar] [CrossRef] [PubMed]
- Brito, G. Secular Compassion Training: An Empirical Review. J. Transpers. Res. 2014, 6, 61–71. [Google Scholar]
- Gilbert, P. Therapy Centered on Compassion. Distinctive Features, 1st ed.; Desclée de Brouwer, S.A.: Bilbao, Spain, 2015. [Google Scholar]
- Tirch, D.D. Mindfulness as a Context for the Cultivation of Compassion. Int. J. Cogn. Ther. 2010, 3, 113–123. [Google Scholar] [CrossRef]
- Gozalo, R.G.; Tarrés, J.F.; Ayora, A.A.; Herrero, M.A.; Kareaga, A.A.; Roca, R.F. Application of a mindfulness program among healthcare professionals in an intensive care unit: Effect on burnout, empathy and self-compassion. Med. Intensiv. 2019, 43, 207–216. [Google Scholar] [CrossRef]
- Dev, V.; Fernando, A.T.; Consedine, N.S. Self-compassion as a Stress Moderator: A Cross-sectional Study of 1700 Doctors, Nurses, and Medical Students. Mindfulness 2020, 11, 1170–1181. [Google Scholar] [CrossRef] [PubMed]
- Conversano, C.; Ciacchini, R.; Orrù, G.; Di Giuseppe, M.; Gemignani, A.; Poli, A. Mindfulness, Compassion, and Self-Compassion Among Health Care Professionals: What’s New? A Systematic Review. Front. Psychol. 2020, 11, 1683. [Google Scholar] [CrossRef]
- Justo, C.F. Reducción de los niveles de estrés y ansiedad en médicos de Atención Primaria mediante la aplicación de un programa de entrenamiento en conciencia plena (mindfulness). Atención Primaria 2010, 42, 564–570. [Google Scholar] [CrossRef]
- Auserón, G.A.; Viscarret, M.R.E.; Goñi, C.F.; Rubio, V.G.; Pascual, P.P.; Galdeano, E.S.D.M.G.D. Evaluación de la efectividad de un programa de mindfulness y autocompasión para reducir el estrés y prevenir el burnout en profesionales sanitarios de atención primaria. Atención Primaria 2018, 50, 141–150. [Google Scholar] [CrossRef]
- Klein, A.; Taieb, O.; Xavier, S.; Baubet, T.; Reyre, A. The benefits of mindfulness-based interventions on burnout among health professionals: A systematic review. EXPLORE 2019, 16, 35–43. [Google Scholar] [CrossRef]
- Scheepers, R.A.; Emke, H.; Epstein, R.M.; Lombarts, K. The impact of mindfulness-based interventions on doctors’ well-being and performance: A systematic review. Med. Educ. 2019, 54, 138–149. [Google Scholar] [CrossRef]
- Rn, N.S.; Rn, J.L.G.; Aguayo-Estremera, R.; La Fuente, G.A.C.; De La Fuente-Solana, E.I.; Rn, L.A. The effect of mindfulness training on burnout syndrome in nursing: A systematic review and meta-analysis. J. Adv. Nurs. 2020, 76, 1124–1140. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen. Hosp. Psychiatry 1982, 4, 33–47. [Google Scholar] [CrossRef]
- Baer, R.A. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin. Psychol. Sci. Pr. 2003, 10, 125–143. [Google Scholar] [CrossRef]
- Lane, J.D.; Seskevich, E.J.; Pieper, C.F. Brief meditation training can improve perceived stress and negative mood. Altern. Ther. Health Med. 2007, 13, 38–44. [Google Scholar]
- Carmody, J.; Baer, R.A. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. J. Clin. Psychol. 2009, 65, 627–638. [Google Scholar] [CrossRef]
- Kriakous, S.A.; Elliott, K.A.; Lamers, C.; Owen, R. The Effectiveness of Mindfulness-Based Stress Reduction on the Psychological Functioning of Healthcare Professionals: A Systematic Review. Mindfulness 2020, 12, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Torres, L.-A.P.-D.; Atalaya, J.C.V.-M.; García-Campayo, J.; Roldán-Villalobos, A.; Magallón-Botaya, R.; Bartolomé-Moreno, C.; Moreno-Martos, H.; Melús-Palazón, E.; Liétor-Villajos, N.; Valverde-Bolívar, F.J.; et al. Controlled clinical trial comparing the effectiveness of a mindfulness and self-compassion 4-session programme versus an 8-session programme to reduce work stress and burnout in family and community medicine physicians and nurses: MINDUUDD study protocol. BMC Fam. Pr. 2019, 20, 1–10. [Google Scholar] [CrossRef]
- Torres, L.P.-D.; Verdes-Montenegro-Atalaya, J.; Melús-Palazón, E.; Vinuesa, L.G.-D.; Valverde, F.; Rodríguez, L.; Lietor-Villajos, N.; Bartolomé-Moreno, C.; Moreno-Martos, H.; García-Campayo, J.; et al. Comparison of the Effectiveness of an Abbreviated Program versus a Standard Program in Mindfulness, Self-Compassion and Self-Perceived Empathy in Tutors and Resident Intern Specialists of Family and Community Medicine and Nursing in Spain. Int. J. Environ. Res. Public Health 2021, 18, 4340. [Google Scholar] [CrossRef]
- Boellinghaus, I.; Jones, F.W.; Hutton, J. The Role of Mindfulness and Loving-Kindness Meditation in Cultivating Self-Compassion and Other-Focused Concern in Health Care Professionals. Mindfulness 2012, 5, 129–138. [Google Scholar] [CrossRef]
- Silva, L.C. Sampling for Research in Health Sciences, 1st ed.; Diaz de Santos: Madrid, Spain, 1993. [Google Scholar]
- Campbell, M.; Grimshaw, J.; Steen, N. Changing Professional Practice in Europe Group (EU BIOMED II Concerted Action) Sample Size Calculations for Cluster Randomised Trials. J. Health Serv. Res. Policy 2000, 5, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J.; de Torrijos, F.; Skillings, A.H.; Blacker, M.; Mumford, G.T.; Alvares, D.L.; Santorelli, S.; Rosal, M.C. Delivery and Effectiveness of a Dual Language (English/Spanish) Mindfulness-Based Stress Reduction (MBSR). Mindfulness Compassion 2016, 1, 2–13. [Google Scholar] [CrossRef]
- Sanz-Carrillo, C.; Garcia-Campayo, J.; Rubio, A.; Santed, M.; Montoro, M. Validation of the Spanish version of the Perceived Stress Questionnaire. J. Psychosom. Res. 2002, 52, 167–172. [Google Scholar] [CrossRef]
- Ferguson, C.J. An effect size primer: A guide for clinicians and researchers. Prof. Psychol. Res. Pr. 2009, 40, 532–538. [Google Scholar] [CrossRef]
- Montero-Marín, J.; Zubiaga, F.; Cereceda, M.; DeMarzo, M.M.P.; Trenc, P.; García-Campayo, J. Burnout Subtypes and Absence of Self-Compassion in Primary Healthcare Professionals: A Cross-Sectional Study. PLoS ONE 2016, 11, e0157499. [Google Scholar] [CrossRef] [PubMed]
- Montero-Marin, J.; Garcia-Campayo, J.; Pérez-Yus, M.C.; Zabaleta-Del-Olmo, E.; Cuijpers, P. Meditation techniques v. relaxation therapies when treating anxiety: A meta-analytic review. Psychol. Med. 2019, 49, 2118–2133. [Google Scholar] [CrossRef] [PubMed]
- Khusid, M.A.; Vythilingam, M. The Emerging Role of Mindfulness Meditation as Effective Self-Management Strategy, Part 1: Clinical Implications for Depression, Post-Traumatic Stress Disorder, and Anxiety. Mil. Med. 2016, 181, 961–968. [Google Scholar] [CrossRef]
- Juul, L.; Pallesen, K.J.; Bjerggaard, M.; Nielsen, C.; Fjorback, L.O. A pilot randomised trial comparing a mindfulness-based stress reduction course, a locally-developed stress reduction intervention and a waiting list control group in a real-life municipal health care setting. BMC Public Health 2020, 20, 1–16. [Google Scholar] [CrossRef]
- Burton, A.; Burgess, C.; Dean, S.; Koutsopoulou, G.Z.; Hugh-Jones, S. How Effective are Mindfulness-Based Interventions for Reducing Stress Among Healthcare Professionals? A Systematic Review and Meta-Analysis. Stress Health 2016, 33, 3–13. [Google Scholar] [CrossRef]
- Lo, K.; Waterland, J.; Todd, P.; Gupta, T.; Bearman, M.; Hassed, C.; Keating, J.L. Group interventions to promote mental health in health professional education: A systematic review and meta-analysis of randomised controlled trials. Adv. Health Sci. Educ. 2017, 23, 413–447. [Google Scholar] [CrossRef]
- Escuriex, B.F.; Labbé, E.E. Health Care Providers’ Mindfulness and Treatment Outcomes: A Critical Review of the Research Literature. Mindfulness 2011, 2, 242–253. [Google Scholar] [CrossRef]
- Smith, S.A. Mindfulness-Based Stress Reduction: An Intervention to Enhance the Effectiveness of Nurses’ Coping With Work-Related Stress. Int. J. Nurs. Knowl. 2014, 25, 119–130. [Google Scholar] [CrossRef]
- Oró, P.; Esquerda, M.; Mas, B.; Viñas, J.; Yuguero, O.; Pifarré, J. Effectiveness of a Mindfulness-Based Programme on Perceived Stress, Psychopathological Symptomatology and Burnout in Medical Students. Mindfulness 2021, 1–10. [Google Scholar] [CrossRef]
- Spinelli, C.; Wisener, M.; Khoury, B. Mindfulness training for healthcare professionals and trainees: A meta-analysis of randomized controlled trials. J. Psychosom. Res. 2019, 120, 29–38. [Google Scholar] [CrossRef]
- Fendel, J.C.; Bürkle, J.J.; Göritz, A.S. Mindfulness-Based Interventions to Reduce Burnout and Stress in Physicians: A Systematic Review and Meta-Analysis. Acad. Med. 2021, 96, 751–764. [Google Scholar] [CrossRef]
- Lomas, T.; Medina, J.C.; Ivtzan, I.; Rupprecht, S.; Eiroa-Orosa, F.J. A systematic review of the impact of mindfulness on the well-being of healthcare professionals. J. Clin. Psychol. 2017, 74, 319–355. [Google Scholar] [CrossRef]
- Ameli, R.; Sinaii, N.; West, C.P.; Luna, M.J.; Panahi, S.; Zoosman, M.; Rusch, H.L.; Berger, A. Effect of a Brief Mindfulness-Based Program on Stress in Health Care Professionals at a US Biomedical Research Hospital. JAMA Netw. Open 2020, 3, e2013424. [Google Scholar] [CrossRef]
- Fortney, L.; Luchterhand, C.; Zakletskaia, L.; Zgierska, A.; Rakel, D. Abbreviated Mindfulness Intervention for Job Satisfaction, Quality of Life, and Compassion in Primary Care Clinicians: A Pilot Study. Ann. Fam. Med. 2013, 11, 412–420. [Google Scholar] [CrossRef]
- Hallman, I.S.; O’Connor, N.; Hasenau, S.; Brady, S. Improving the culture of safety on a high-acuity inpatient child/adolescent psychiatric unit by mindfulness-based stress reduction training of staff. J. Child Adolesc. Psychiatr. Nurs. 2017, 30, 175–180. [Google Scholar] [CrossRef]
- Brady, S.; O’Connor, N.; Burgermeister, D.; Hanson, P. The Impact of Mindfulness Meditation in Promoting a Culture of Safety on an Acute Psychiatric Unit. Perspect. Psychiatr. Care 2011, 48, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Pipe, T.B.; Bortz, J.J.; Dueck, A.; Pendergast, D.; Buchda, V.; Summers, J. Nurse Leader Mindfulness Meditation Program for Stress Management. JONA J. Nurs. Adm. 2009, 39, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, D.A.; Stephens, E.; Colgan, D.; Hunsinger, M.; Rubin, D.; Christopher, M.S. A Brief Mindfulness-Based Intervention for Primary Care Physicians: A Pilot Randomized Controlled Trial. Am. J. Lifestyle Med. 2016, 12, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Khoury, B.; Sharma, M.; Rush, S.E.; Fournier, C. Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J. Psychosom. Res. 2015, 78, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Gilmartin, H.; Goyal, A.; Hamati, M.C.; Mann, J.; Saint, S.; Chopra, V. Brief Mindfulness Practices for Healthcare Providers—A Systematic Literature Review. Am. J. Med. 2017, 130, 1219-e1. [Google Scholar] [CrossRef] [PubMed]
- Zakiei, A.; Khazaie, H.; Rostampour, M.; Lemola, S.; Esmaeili, M.; Dürsteler, K.; Brühl, A.; Sadeghi-Bahmani, D.; Brand, S. Acceptance and Commitment Therapy (ACT) Improves Sleep Quality, Experiential Avoidance, and Emotion Regulation in Individuals with Insomnia—Results from a Randomized Interventional Study. Life 2021, 11, 133. [Google Scholar] [CrossRef] [PubMed]
- Geary, C.; Rosenthal, S.L. Sustained Impact of MBSR on Stress, Well-Being, and Daily Spiritual Experiences for 1 Year in Academic Health Care Employees. J. Altern. Complement. Med. 2011, 17, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Fuertes, M.; Aranda, G.; Rezola, N.; Erramuzpe, A.; Palacios, C.; Ibañez, B. Long-term effects of a mindfulness and self-compassion program with Primary Healthcare professionals. An. del Sist. Sanit. de Navar. 2019, 42, 269–280. [Google Scholar] [CrossRef]
| Variable | Total n = 112 | CG n = 51 | EG1 n = 24 | EG2 n = 37 | p-Value | η2 |
|---|---|---|---|---|---|---|
| Age (years): mean ± SD | 41.61 ± 12.61 | 40.34 ± 13.22 | 47.66 ± 13.67 | 35.73 ± 12.04 | <0.001 | 0.109 * |
| Sex: n (%) | ||||||
| Male | 26 (23.21) | 11 (21.57) | 6 (25.00) | 9 (24.32) | 0.978 | 0.016 ** |
| Female | 86 (76.79) | 40 (78.43) | 18 (75.00) | 28 (75.68) | ||
| Occupation: n (%) | ||||||
| Physician | 95 (84.82) | 41 (80.39) | 20 (83.33) | 34 (91.89) | 0.165 | 0.146 ** |
| Nurse | 17 (15.18) | 10 (19.61) | 4 (16.67) | 3 (8.11) | ||
| Professional type: n (%) | ||||||
| Tutor | 50 (44.64) | 24 (47.06) | 15 (62.50) | 11 (29.73) | <0.001 | 0.317 ** |
| Resident | 62 (55.36) | 27 (52.94) | 9 (37.50) | 26 (70.27) | ||
| Workplace: n (%) | ||||||
| Health Center | 95 (84.82) | 40 (78.43) | 22 (91.67) | 33 (89.19) | 0.217 | 0.135 ** |
| Hospital | 17 (15.18) | 11 (21.57) | 2 (8.33) | 4 (10.81) | ||
| Work experience (years): mean ± SD | 12.88 ± 13.15 | 13.13 ± 12.95 | 19.49 ± 13.91 | 8.91 ± 11.06 | <0.001 | 0.117 * |
| Evaluation | Outcome | CG | EG1 | EG2 | F | p-Value | η2 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | DS | Mean | DS | Mean | DS | |||||
| Pretest | PSQ Tension–Instability–Fatigue | 23.825 | 4.316 | 22.846 | 4.749 | 23.159 | 4.674 | 0.636 | 0.531 | 0.008 |
| PSQ Social Acceptance of Conflicts | 13.778 | 3.250 | 13.897 | 3.705 | 13.937 | 3.136 | 0.038 | 0.963 | 0.000 | |
| PSQ Energy and Fun | 13.746 | 2.609 | 13.231 | 2.146 | 13.191 | 2.429 | 0.959 | 0.385 | 0.012 | |
| PSQ-Overload | 10.032 | 1.565 | 10.513 | 1.315 | 10.159 | 1.677 | 1.178 | 0.311 | 0.014 | |
| PSQ Self-Fulfillment Satisfaction | 6.809 | 1.378 | 6.744 | 1.332 | 6.460 | 1.280 | 1.184 | 0.309 | 0.014 | |
| PSQ Fear and Anxiety | 3.984 | 1.277 | 4.051 | 1.169 | 4.349 | 1.138 | 1.596 | 0.206 | 0.019 | |
| PSQ Total | 69.250 | 10.910 | 68.430 | 12.180 | 68.740 | 11.650 | 0.100 | 0.905 | 0.001 | |
| Post-test | PSQ Tension–Instability–Fatigue | 23.750 * | 5.501 | 21.357 | 6.696 | 20.195 * | 5.016 | 4.972 | 0.008 | 0.075 |
| PSQ Social Acceptance of Conflicts | 14.536 * | 4.191 | 13.250 | 4.766 | 12.146 * | 3.403 | 4.086 | 0.019 | 0.063 | |
| PSQ Energy and Fun | 12.911 * | 3.354 | 11.536 | 3.328 | 10.854 * | 3.062 | 4.989 | 0.008 | 0.076 | |
| PSQ-Overload | 10.732 | 2.416 | 11.393 | 2.439 | 10.171 | 2.397 | 2.142 | 0.122 | 0.034 | |
| PSQ Self-Fulfillment Satisfaction | 6.607 * | 1.775 | 5.893 | 1.873 | 5.122 * | 1.327 | 9.440 | <0.001 | 0.134 | |
| PSQ Fear and Anxiety | 3.929 | 1.373 | 4.143 | 1.484 | 3.830 | 1.181 | 0.463 | 0.631 | 0.008 | |
| PSQ Total | 69.660 * | 15.230 | 65.210 | 17.590 | 59.900 * | 12.810 | 4.970 | 0.008 | 0.075 | |
| Follow-up | PSQ Tension–Instability–Fatigue | 24.039 | 6.591 | 21.375 | 6.889 | 21.324 | 5.318 | 2.568 | 0.081 | 0.045 |
| PSQ Social Acceptance of Conflicts | 14.745 | 4.462 | 13.833 | 5.346 | 12.540 | 3.114 | 2.837 | 0.063 | 0.049 | |
| PSQ Energy and Fun | 12.529 | 3.596 | 11.750 | 3.542 | 11.216 | 2.678 | 1.733 | 0.182 | 0.031 | |
| PSQ-Overload | 11.059 | 2.525 | 10.833 | 2.914 | 10.459 | 2.479 | 0.572 | 0.566 | 0.010 | |
| PSQ Self-Fulfillment Satisfaction | 6.686 * | 2.131 | 6.417 | 2.104 | 5.513 * | 1.539 | 4.006 | 0.021 | 0.068 | |
| PSQ Fear and Anxiety | 4.000 | 1.456 | 4.208 | 1.532 | 3.784 | 1.228 | 0.685 | 0.506 | 0.012 | |
| PSQ Total | 70.390 | 16.950 | 66.040 | 19.570 | 62.450 | 13.200 | 2.531 | 0.084 | 0.044 | |
| Group | Outcome | Pretest | Post-Test | Follow-Up | MS | F | p-Value | η2 | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | DS | Mean | DS | Mean | DS | ||||||
| CG | PSQ Tension–Instability–Fatigue | 24.273 | 3.660 | 23.485 | 5.723 | 23.818 | 6.217 | 5.162 | 0.283 | 0.755 | 0.009 |
| PSQ Social Acceptance of Conflicts | 14.000 | 3.419 | 14.758 | 4.451 | 14.364 | 4.227 | 4.737 | 0.748 | 0.477 | 0.023 | |
| PSQ Energy and Fun | 14.091 * | 2.542 | 13.181 * | 3.548 | 12.576 | 3.410 | 19.192 | 4.780 | 0.012 | 0.130 | |
| PSQ-Overload | 10.212 | 1.453 | 10.879 | 2.434 | 10.939 | 2.573 | 8.727 | 3.662 | 0.065 | 0.103 | |
| PSQ Self-Fulfillment Satisfaction | 6.818 | 1.530 | 6.697 | 1.845 | 6.727 | 2.212 | 0.131 | 0.069 | 0.934 | 0.002 | |
| PSQ Fear and Anxiety | 3.879 | 1.317 | 3.939 | 1.345 | 4.000 | 1.346 | 0.121 | 0.116 | 0.891 | 0.004 | |
| PSQ Total | 69.250 | 10.910 | 69.660 | 15.230 | 70.390 | 16.950 | 2.303 | 0.022 | 0.978 | 0.001 | |
| EG1 | PSQ Tension–Instability–Fatigue | 22.118 | 4.386 | 21.588 | 6.423 | 20.941 | 6.590 | 5.902 | 0.369 | 0.694 | 0.023 |
| PSQ Social Acceptance of Conflicts | 13.353 | 3.622 | 13.353 | 4.015 | 14.118 | 4.885 | 3.314 | 0.518 | 0.601 | 0.031 | |
| PSQ Energy and Fun | 12.823 * | 1.846 | 11.235 * | 3.093 | 11.353 | 3.517 | 13.314 | 3.758 | 0.034 | 0.190 | |
| PSQ-Overload | 10.647 | 1.169 | 11.294 | 2.312 | 10.706 | 2.995 | 2.176 | 0.839 | 0.441 | 0.050 | |
| PSQ Self-Fulfillment Satisfaction | 6.588 | 1.004 | 5.765 | 1.562 | 6.412 | 2.293 | 3.196 | 2.498 | 0.098 | 0.135 | |
| PSQ Fear and Anxiety | 3.941 | 1.088 | 4.000 | 1.275 | 4.294 | 1.359 | 0.608 | 0.967 | 0.391 | 0.057 | |
| PSQ Total | 68.430 | 12.180 | 65.210 | 17.590 | 66.040 | 19.570 | 13.549 | 0.156 | 0.857 | 0.010 | |
| EG2 | PSQ Tension–Instability–Fatigue | 23.167 * | 4.146 | 20.500 * | 5.626 | 21.083 | 4.880 | 47.167 | 3.505 | 0.038 | 0.132 |
| PSQ Social Acceptance of Conflicts | 13.917 | 3.035 | 12.583 | 3.106 | 12.667 | 3.185 | 13.389 | 2.134 | 0.130 | 0.085 | |
| PSQ Energy and Fun | 13.042 * | 2.349 | 10.833 * | 3.046 | 11.333 | 2.408 | 32.181 | 9.471 | <0.001 | 0.292 | |
| PSQ-Overload | 10.542 | 1.587 | 10.625 | 2.651 | 10.292 | 2.216 | 0.722 | 0.206 | 0.815 | 0.009 | |
| PSQ Self-Fulfillment Satisfaction | 6.542 $ | 1.503 | 5.250 | 1.189 | 5.458 $ | 1.587 | 11.542 | 11.479 | <0.001 | 0.333 | |
| PSQ Fear and Anxiety | 4.292 * | 1.083 | 3.958 * | 1.122 | 3.667 | 1.341 | 2.347 | 3.242 | 0.048 | 0.124 | |
| PSQ Total | 68.740 * | 11.650 | 59.900 * | 12.810 | 62.450 | 13.200 | 393.431 | 4.587 | 0.015 | 0.166 | |
| Evaluation | Outcome | Source | Type III Sum of Square | df | MS | F | p-Value | η2 |
|---|---|---|---|---|---|---|---|---|
| Post-test | PSQ Tension–Instability–Fatigue | Pretest PSQ Tension–Instability–Fatigue | 536.007 | 1 | 536.007 | 20.144 | <0.001 | 0.181 |
| CG/EG1/EG2 | 172.882 | 2 | 86.441 | 3.249 | 0.043 | 0.067 | ||
| Error | 2421.378 | 91 | 26.609 | |||||
| PSQ Social Acceptance of Conflicts | Pretest PSQ Social Acceptance of Conflicts | 352.796 | 1 | 352.796 | 30.146 | <0.001 | 0.249 | |
| CG/EG1/EG2 | 114.431- | 2 | 57.216 | 4.889 | 0.010 | 0.097 | ||
| Error | 1064.951 | 91 | 11.703 | |||||
| PSQ Energy and Fun | Pretest PSQ Energy and Fun | 251.198 | 1 | 251.198 | 34.118 | <0.001 | 0.273 | |
| CG/EG1/EG2 | 52.589 | 2 | 26.294 | 3.571 | 0.032 | 0.073 | ||
| Error | 669.991 | 91 | 7.363 | |||||
| PSQ Overload | Pretest PSQ Overload | 92.181 | 1 | 92.181 | 19.326 | <0.001 | 0.175 | |
| CG/EG1/EG2 | 17.248 | 2 | 8.624 | 1.808 | 0.170 | 0.038 | ||
| Error | 434.053 | 91 | 4.770 | |||||
| PSQ Self-Fulfillment Satisfaction | Pretest PSQ Self-Fulfillment Satisfaction | 41.923 | 1 | 41.923 | 21.435 | <0.001 | 0.191 | |
| CG/EG1/EG2 | 35.168 | 2 | 17.584 | 8.991 | <0.001 | 0.165 | ||
| Error | 177.977 | 91 | 1.956 | |||||
| PSQ Fear and Anxiety | Pretest PSQ Fear and Anxiety | 40.719 | 1 | 40.719 | 34.263 | <0.001 | 0.274 | |
| CG/EG1/EG2 | 1.870 | 2 | 0.935 | 0.787 | 0.458 | 0.017 | ||
| Error | 108.146 | 91 | 1.188 | |||||
| PSQ Total | Pretest PSQ Total | 4255.714 | 1 | 4255.714 | 26.222 | <0.001 | 0.224 | |
| CG/EG1/EG2 | 1676.611 | 2 | 838.305 | 5.165 | 0.008 | 0.102 | ||
| Error | 14,768.788 | 91 | 162.294 | |||||
| Follow-up | PSQ Tension– Instability-Fatigue | Pretest PSQ Tension–Instability–Fatigue | 207.608 | 1 | 207.608 | 6.241 | 0.015 | 0.073 |
| CG/EG1/EG2 | 77.888 | 2 | 38.944 | 1.171 | 0.315 | 0.029 | ||
| Error | 2628.146 | 79 | 33.268 | |||||
| PSQ Social Acceptance of Conflicts | Pretest PSQ Social Acceptance of Conflicts | 279.122 | 1 | 279.122 | 20.781 | <0.001 | 0.208 | |
| CG/EG1/EG2 | 43.832 | 2 | 21.916 | 1.632 | 0.202 | 0.040 | ||
| Error | 1061.119 | 79 | 13.432 | |||||
| PSQ Energy and Fun | Pretest PSQ Energy and Fun | 200.447 | 1 | 200.447 | 23.134 | 0.001 | 0.227 | |
| CG/EG1/EG2 | 2.880 | 2 | 1.440 | 0.166 | 0.847 | 0.004 | ||
| Error | 684.514 | 79 | 8.665 | |||||
| PSQ Overload | Pretest PSQ Overload | 48.077 | 1 | 48.077 | 8.358 | 0.005 | 0.096 | |
| CG/EG1/EG2 | 12.184 | 2 | 6.092 | 1.059 | 0.352 | 0.026 | ||
| Error | 454.429 | 79 | 5.752 | |||||
| PSQ Self-Fulfillment Satisfaction | Pretest PSQ Self-Fulfillment Satisfaction | 63.076 | 1 | 63.076 | 19.201 | <0.001 | 0.196 | |
| CG/EG1/EG2 | 13.817 | 2 | 6.908 | 2.103 | 0.129 | 0.051 | ||
| Error | 259.523 | 79 | 3.285 | |||||
| PSQ Fear and Anxiety | Pretest PSQ Fear and Anxiety | 26.231 | 1 | 26.231 | 17.133 | <0.001 | 0.178 | |
| CG/EG1/EG2 | 6.806 | 2 | 3.403 | 2.223 | 0.115 | 0.053 | ||
| Error | 120.954 | 79 | 1.531 | |||||
| PSQ Total | Pretest PSQ Total | 2647.821 | 1 | 2647.821 | 12.098 | 0.001 | 0.133 | |
| CG/EG1/EG2 | 621.887 | 2 | 310.943 | 1.421 | 0.248 | 0.035 | ||
| Error | 17,290.561 | 79 | 218.868 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verdes-Montenegro-Atalaya, J.C.; Pérula-de Torres, L.Á.; Lietor-Villajos, N.; Bartolomé-Moreno, C.; Moreno-Martos, H.; Rodríguez, L.A.; Grande-Grande, T.; Pardo-Hernández, R.; León-del-Barco, B.; Santamaría-Peláez, M.; et al. Effectiveness of a Mindfulness and Self-Compassion Standard Training Program versus an Abbreviated Training Program on Stress in Tutors and Resident Intern Specialists of Family and Community Medicine and Nursing in Spain. Int. J. Environ. Res. Public Health 2021, 18, 10230. https://doi.org/10.3390/ijerph181910230
Verdes-Montenegro-Atalaya JC, Pérula-de Torres LÁ, Lietor-Villajos N, Bartolomé-Moreno C, Moreno-Martos H, Rodríguez LA, Grande-Grande T, Pardo-Hernández R, León-del-Barco B, Santamaría-Peláez M, et al. Effectiveness of a Mindfulness and Self-Compassion Standard Training Program versus an Abbreviated Training Program on Stress in Tutors and Resident Intern Specialists of Family and Community Medicine and Nursing in Spain. International Journal of Environmental Research and Public Health. 2021; 18(19):10230. https://doi.org/10.3390/ijerph181910230
Chicago/Turabian StyleVerdes-Montenegro-Atalaya, Juan Carlos, Luis Ángel Pérula-de Torres, Norberto Lietor-Villajos, Cruz Bartolomé-Moreno, Herminia Moreno-Martos, Luis Alberto Rodríguez, Teresa Grande-Grande, Rocío Pardo-Hernández, Benito León-del-Barco, Mirian Santamaría-Peláez, and et al. 2021. "Effectiveness of a Mindfulness and Self-Compassion Standard Training Program versus an Abbreviated Training Program on Stress in Tutors and Resident Intern Specialists of Family and Community Medicine and Nursing in Spain" International Journal of Environmental Research and Public Health 18, no. 19: 10230. https://doi.org/10.3390/ijerph181910230
APA StyleVerdes-Montenegro-Atalaya, J. C., Pérula-de Torres, L. Á., Lietor-Villajos, N., Bartolomé-Moreno, C., Moreno-Martos, H., Rodríguez, L. A., Grande-Grande, T., Pardo-Hernández, R., León-del-Barco, B., Santamaría-Peláez, M., Mínguez, L. A., González-Santos, J., Soto-Cámara, R., González-Bernal, J. J., & on behalf of the MINDUUDD Collaborative Study Group. (2021). Effectiveness of a Mindfulness and Self-Compassion Standard Training Program versus an Abbreviated Training Program on Stress in Tutors and Resident Intern Specialists of Family and Community Medicine and Nursing in Spain. International Journal of Environmental Research and Public Health, 18(19), 10230. https://doi.org/10.3390/ijerph181910230










