Weather Trumps Festivity? More Cardiovascular Disease Events Occur in Winter than in December Holidays in Queensland, Australia
Abstract
1. Introduction
2. Methods
2.1. Data
2.2. Outcomes
2.3. Statistical Analyses
3. Results
3.1. Descriptive Results
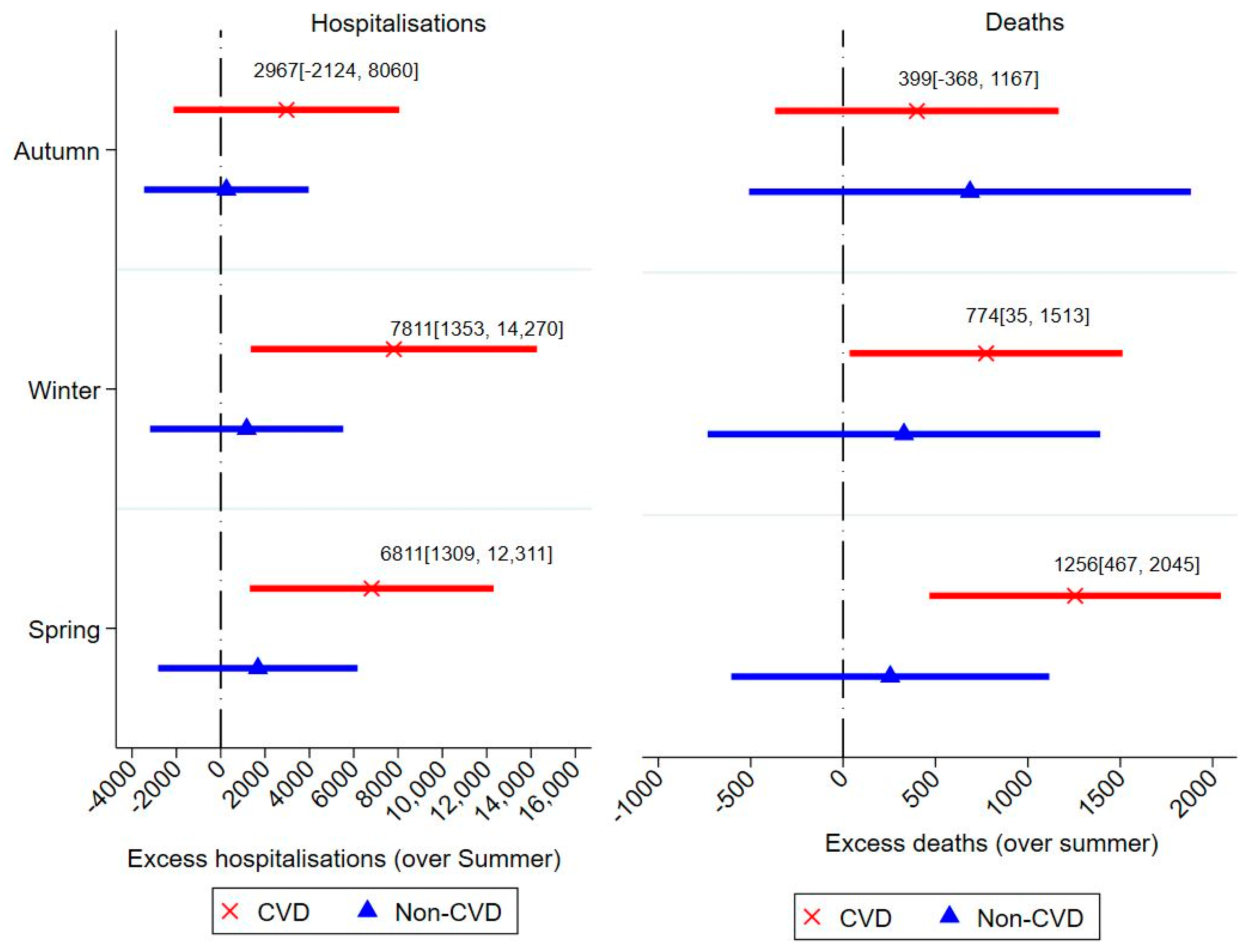
3.2. Seasonality in CVD Hospitalisations and Deaths
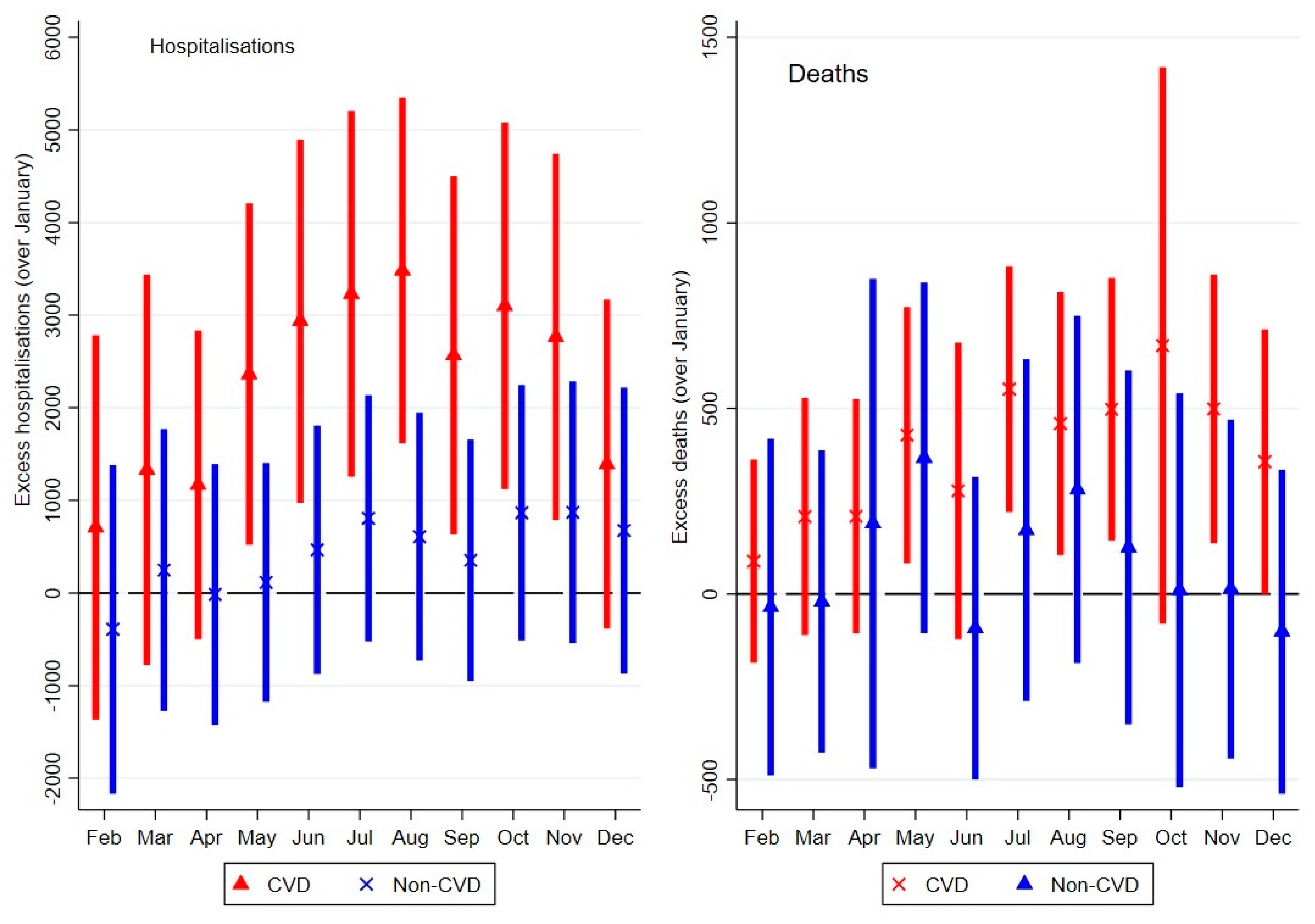
3.3. Monthly Variations in CVD and Non-CVD-Related Events
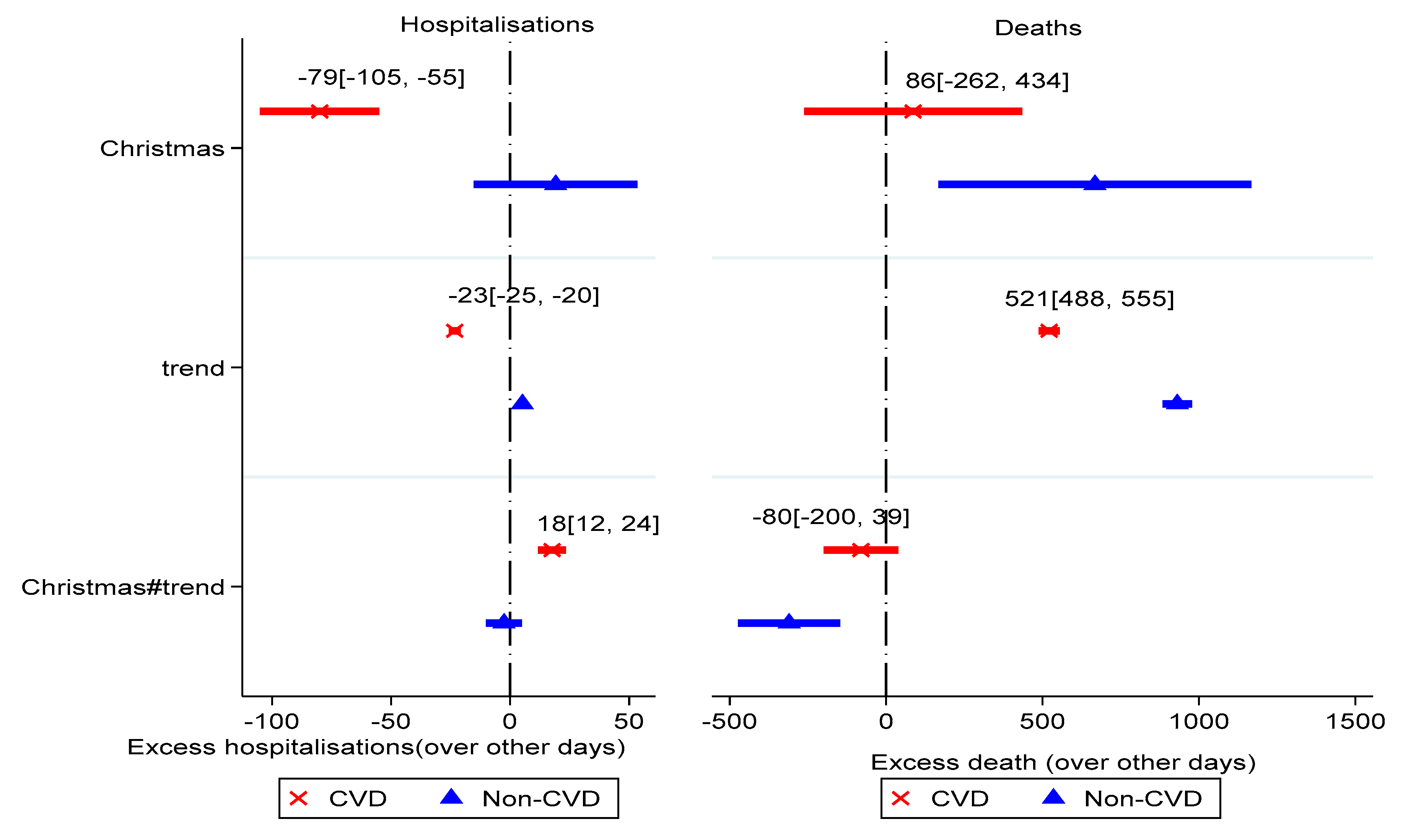
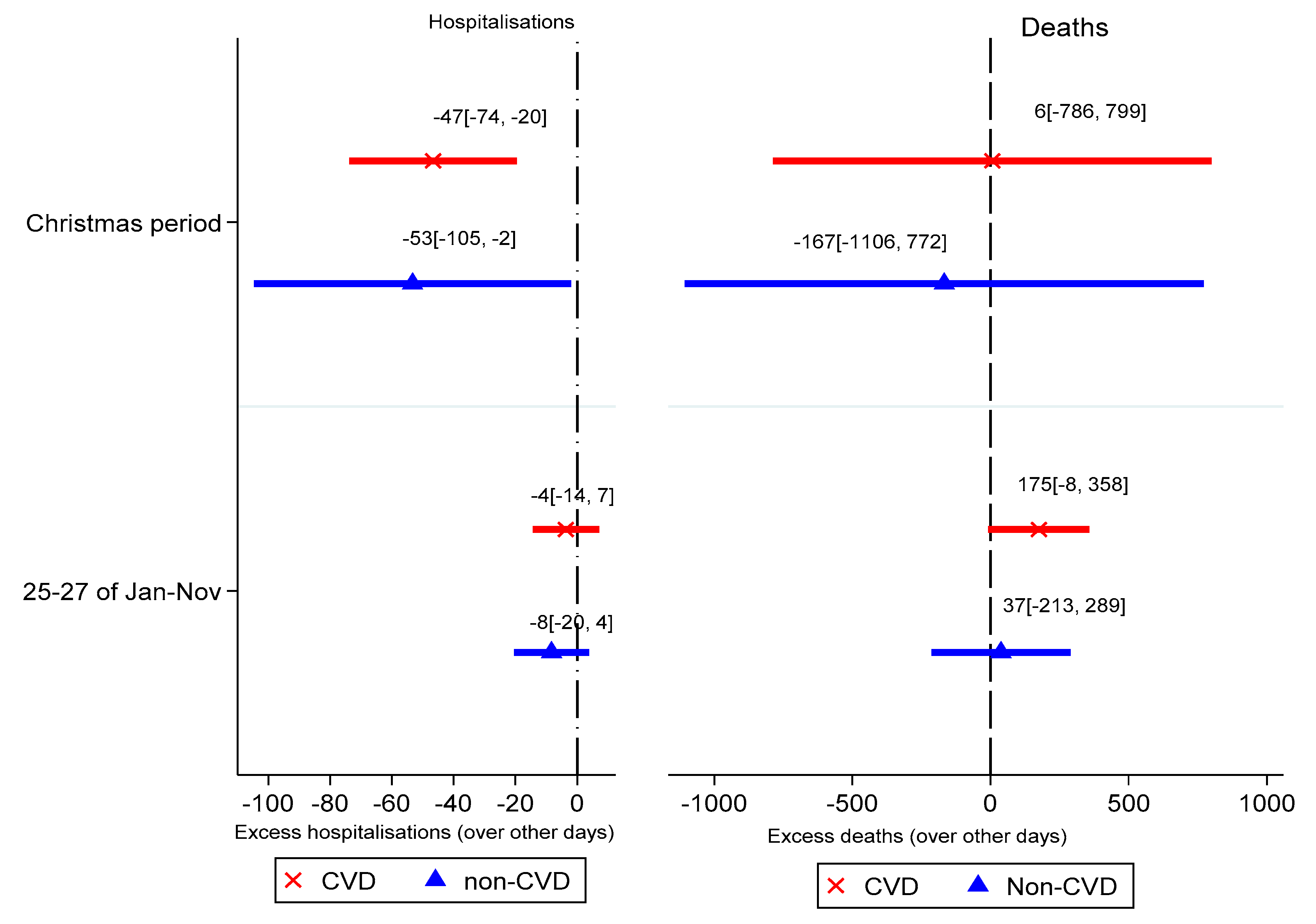
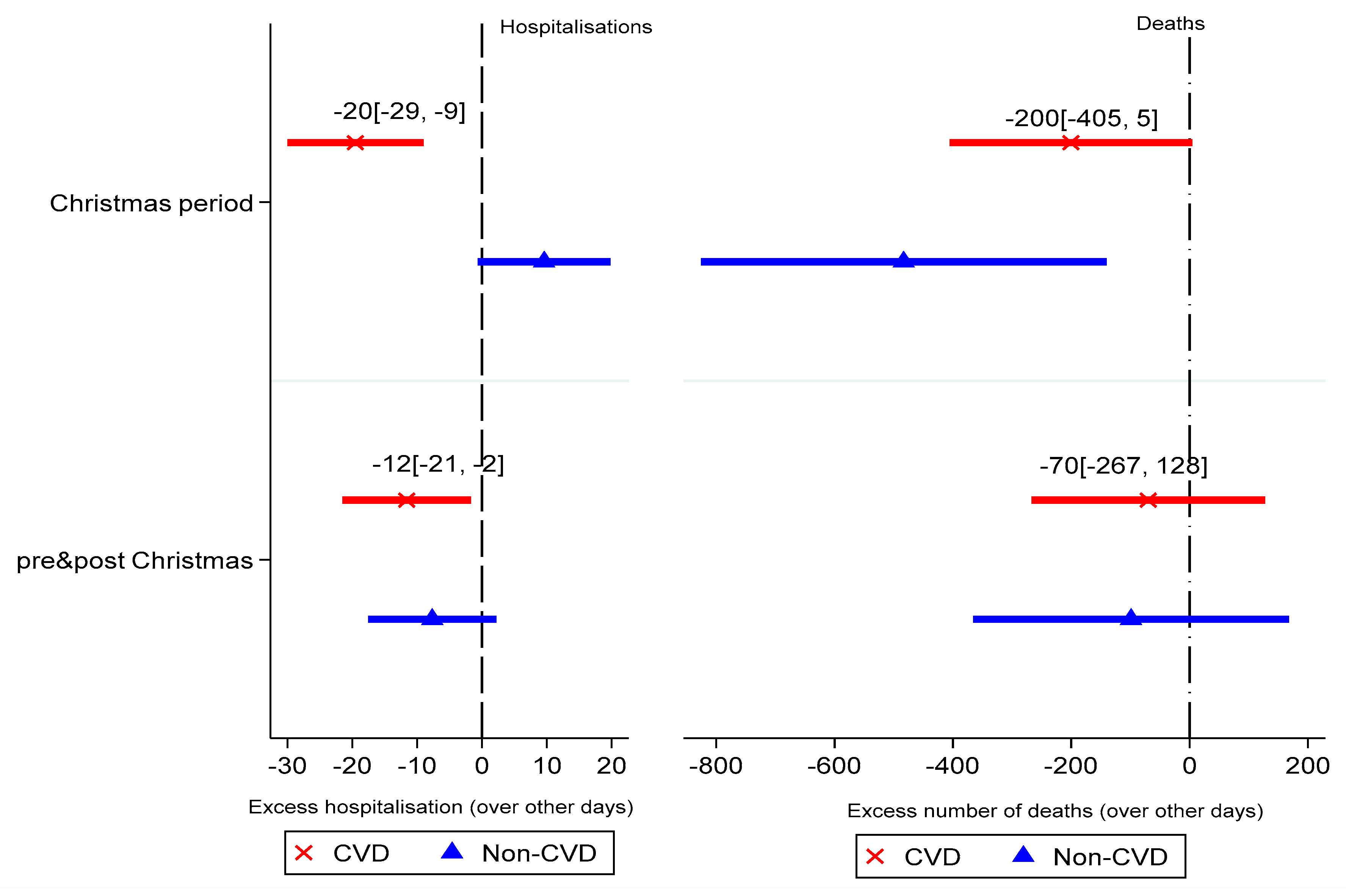
3.4. CVD- and Non-CVD-Related Events during December Holidays
3.5. Sensitivity Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Boulay, F.; Berthier, F.; Sisteron, O.; Gendreike, Y.; Gibelin, P. Seasonal variation in chronic heart failure hospitalizations and mortality in France. Circulation 1999, 100, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Stewart, S.; McIntyre, K.; Capewell, S.; McMurray, J.J. Heart failure in a cold climate: Seasonal variation in heart failure-related morbidity and mortality. J. Am. Coll. Cardiol. 2002, 39, 760–766. [Google Scholar] [CrossRef]
- Martínez-Sellés, M.; Robles, J.A.G.; Prieto, L.; Serrano, J.A.; Muñoz, R.; Frades, E.; Almendral, J. Annual rates of admission and seasonal variations in hospitalizations for heart failure. Eur. J. Heart Fail. 2002, 4, 779–786. [Google Scholar] [CrossRef]
- Barnett, A.G.; De Looper, M.; Fraser, J.F. The seasonality in heart failure deaths and total cardiovascular deaths. Aust. N. Z. J. Public Health 2008, 32, 408–413. [Google Scholar] [CrossRef]
- Weerasinghe, D.P.; MacIntyre, C.; Rubin, G. Seasonality of coronary artery deaths in New South Wales, Australia. Heart 2002, 88, 30–34. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Moholdt, T.; Afoakwah, C.; Scuffham, P.; McDonald, C.F.; Burrell, L.M.; Stewart, S. Excess mortality at Christmas due to cardiovascular disease in the HUNT study prospective population-based cohort in Norway. BMC Public Health 2021, 21, 549. [Google Scholar] [CrossRef] [PubMed]
- Knight, J.; Schilling, C.; Barnett, A.; Jackson, R.; Clarke, P. Revisiting the “Christmas holiday effect” in the southern hemisphere. J. Am. Heart Assoc. 2016, 5, e005098. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D.; Barker, G.E.; Brewer, K.M. Christmas and New Year as risk factors for death. Soc. Sci. Med. 2010, 71, 1463–1471. [Google Scholar] [CrossRef]
- Phillips, D.P.; Jarvinen, J.R.; Abramson, I.S.; Phillips, R.R. Cardiac mortality is higher around Christmas and New Year’s than at any other time: The holidays as a risk factor for death. Circulation 2004, 110, 3781–3788. [Google Scholar] [CrossRef]
- Mohammad, M.A.; Karlsson, S.; Haddad, J.; Cederberg, B.; Jernberg, T.; Lindahl, B.; Fröbert, O.; Koul, S.; Erlinge, D. Christmas, national holidays, sport events, and time factors as triggers of acute myocardial infarction: SWEDEHEART observational study 1998–2013. BMJ 2018, 363, k4811. [Google Scholar] [CrossRef]
- Kloner, R.A.; Poole, W.K.; Perritt, R.L. When throughout the year is coronary death most likely to occur? A 12-year population-based analysis of more than 220,000 cases. Circulation 1999, 100, 1630–1634. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, C.D. Recent evidence supporting psychologic and social risk factors for coronary disease. N. Engl. J. Med. 1976, 294, 1033–1038. [Google Scholar] [CrossRef] [PubMed]
- Leor, J.; Poole, W.K.; Kloner, R.A. Sudden cardiac death triggered by an earthquake. N. Engl. J. Med. 1996, 334, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Burrell, L.M.; Stewart, S. Peak Winter! A Report on the Seasonal Impact of Heart Failure in Australia! Available online: https://research.torrens.edu.au/en/publications/peak-winter-a-report-on-the-seasonal-impact-of-heart-failure-in-a-2 (accessed on 4 May 2021).
- Byrnes, J.; Nghiem, S.; Afoakwah, C.; Scuffham, P. Queensland Cardiovascular Data Linkage (QCard): A population-based cohort study [version 1; peer review: Awaiting peer review]. F1000Research 2020, 9, 282. [Google Scholar] [CrossRef]
- Queensland Health. Queensland Health the Health of Queenslanders—Cardiovascular Disease. Available online: https://www.health.qld.gov.au/__data/assets/pdf_file/0031/644854/cardiovascular-disease-factsheet.pdf (accessed on 2 February 2021).
- Marti-Soler, H.; Gonseth, S.; Gubelmann, C.; Stringhini, S.; Bovet, P.; Chen, P.-C.; Wojtyniak, B.; Paccaud, F.; Tsai, D.-H.; Zdrojewski, T. Seasonal variation of overall and cardiovascular mortality: A study in 19 countries from different geographic locations. PLoS ONE 2014, 9, e113500. [Google Scholar]
- Stewart, S.; Moholdt, T.T.; Burrell, L.M.; Sliwa, K.; Mocumbi, A.O.; McMurray, J.J.; Keates, A.K.; Hawley, J. Winter peaks in heart failure: An inevitable or preventable consequence of seasonal vulnerability? Card. Fail. Rev. 2019, 5, 83. [Google Scholar] [CrossRef]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklöv, J.; Forsberg, B.J.T.L. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Eccles, R. An explanation for the seasonality of acute upper respiratory tract viral infections. Acta Oto-Laryngol. 2002, 122, 183–191. [Google Scholar] [CrossRef]
- Barnett, A.G.; Dobson, A.J.; McElduff, P.; Salomaa, V.; Kuulasmaa, K.; Sans, S. Cold periods and coronary events: An analysis of populations worldwide. J. Epidemiol. Community Health 2005, 59, 551–557. [Google Scholar] [CrossRef]
- Afoakwah, C.; Nghiem, S.; Scuffham, P.; Huynh, Q.; Marwick, T.; Byrnes, J. Impacts of air pollution on health: Evidence from longitudinal cohort data of patients with cardiovascular diseases. Eur. J. Health Econ. 2020, 21, 1025–1038. [Google Scholar] [CrossRef]
- Lapointe-Shaw, L.; Austin, P.C.; Ivers, N.M.; Luo, J.; Redelmeier, D.A.; Bell, C.M. Death and readmissions after hospital discharge during the December holiday period: Cohort study. BMJ 2018, 363, k4481. [Google Scholar] [CrossRef] [PubMed]
| Hospitalisations | Death | |||||||
|---|---|---|---|---|---|---|---|---|
| All-Cause n = 592,296 | CVD n = 181,890 | Non-CVD n = 410,406 | All-Cause n = 14,035 | CVD n = 7366 | Non-CVD n = 6669 | |||
| % | % | % | p-value | % | % | % | p-value | |
| Male | 53.5 | 53.6 | 53.4 | p = 0.128 | 52.4 | 50.1 | 54.8 | p < 0.01 |
| Indigenous | 2.8 | 2.5 | 3.0 | p < 0.01 | 2.2 | 2.0 | 2.6 | p < 0.01 |
| Age | ||||||||
| 17–44 | 11.2 | 10.1 | 11.4 | p < 0.01 | 2.8 | 1.1 | 4.7 | p < 0.01 |
| 45–64 | 31.5 | 30.2 | 32.0 | 16.1 | 9.6 | 23.3 | ||
| 65–74 | 25.0 | 23.2 | 25.8 | 22.1 | 17.1 | 27.5 | ||
| >74 | 32.3 | 36.5 | 30.7 | 65.9 | 77.9 | 52.6 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Afoakwah, C.; Nghiem, S.; Scuffham, P.; Stewart, S.; Byrnes, J. Weather Trumps Festivity? More Cardiovascular Disease Events Occur in Winter than in December Holidays in Queensland, Australia. Int. J. Environ. Res. Public Health 2021, 18, 10158. https://doi.org/10.3390/ijerph181910158
Afoakwah C, Nghiem S, Scuffham P, Stewart S, Byrnes J. Weather Trumps Festivity? More Cardiovascular Disease Events Occur in Winter than in December Holidays in Queensland, Australia. International Journal of Environmental Research and Public Health. 2021; 18(19):10158. https://doi.org/10.3390/ijerph181910158
Chicago/Turabian StyleAfoakwah, Clifford, Son Nghiem, Paul Scuffham, Simon Stewart, and Joshua Byrnes. 2021. "Weather Trumps Festivity? More Cardiovascular Disease Events Occur in Winter than in December Holidays in Queensland, Australia" International Journal of Environmental Research and Public Health 18, no. 19: 10158. https://doi.org/10.3390/ijerph181910158
APA StyleAfoakwah, C., Nghiem, S., Scuffham, P., Stewart, S., & Byrnes, J. (2021). Weather Trumps Festivity? More Cardiovascular Disease Events Occur in Winter than in December Holidays in Queensland, Australia. International Journal of Environmental Research and Public Health, 18(19), 10158. https://doi.org/10.3390/ijerph181910158










