Sex/Gender-Differences in the Health Effects of Environmental Noise Exposure on Hypertension and Ischemic Heart Disease—A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Selection of Studies
2.3. Eligibility Criteria
2.4. Data Extraction and Risk of Bias Assessment
3. Results
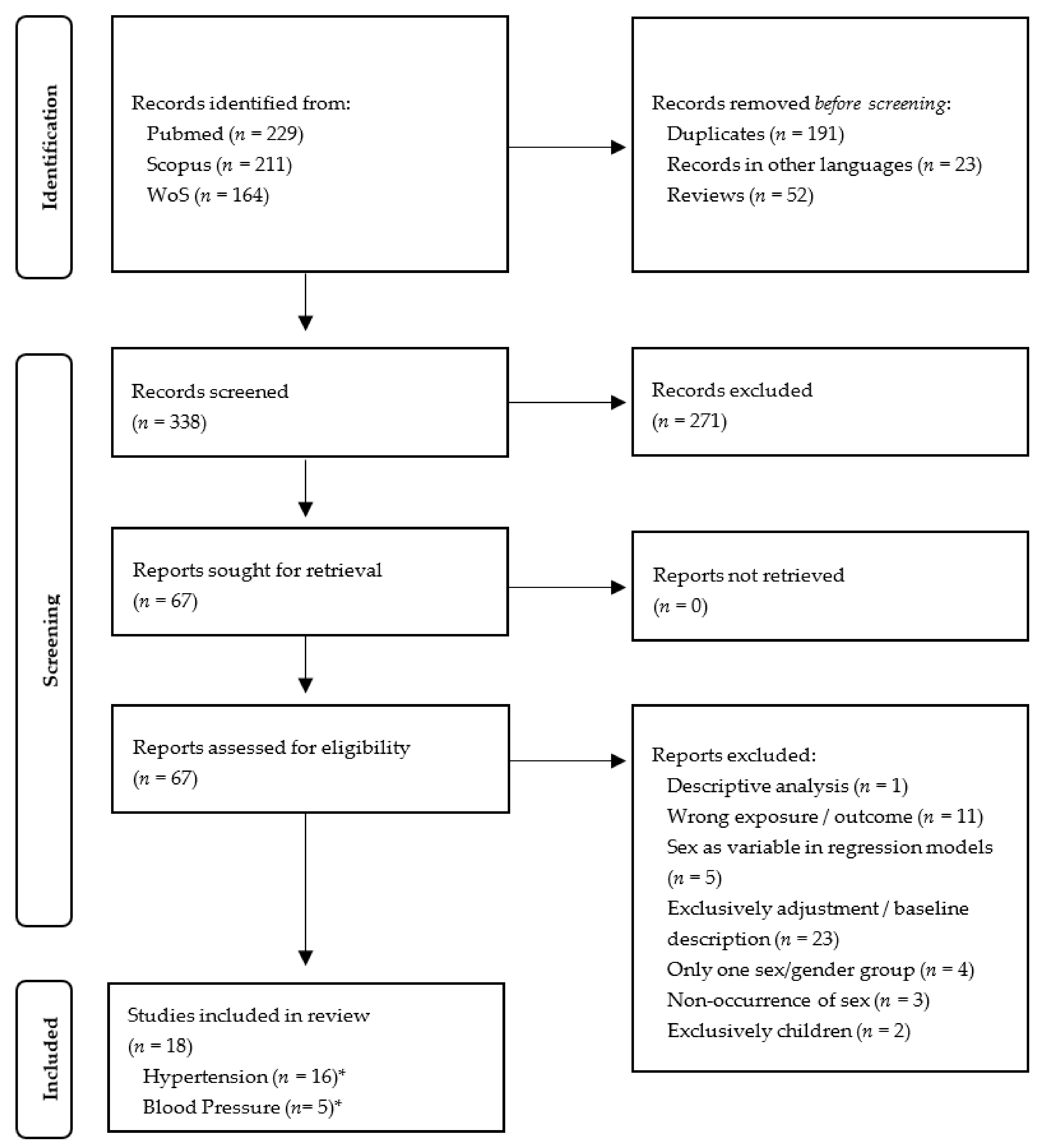
3.1. Comprehensive Literature Search
3.2. Risk of Bias of the Included Studies
3.3. General Study Characteristics
3.4. Conceptualization, Operationalization, Rationale and Discussion of Results
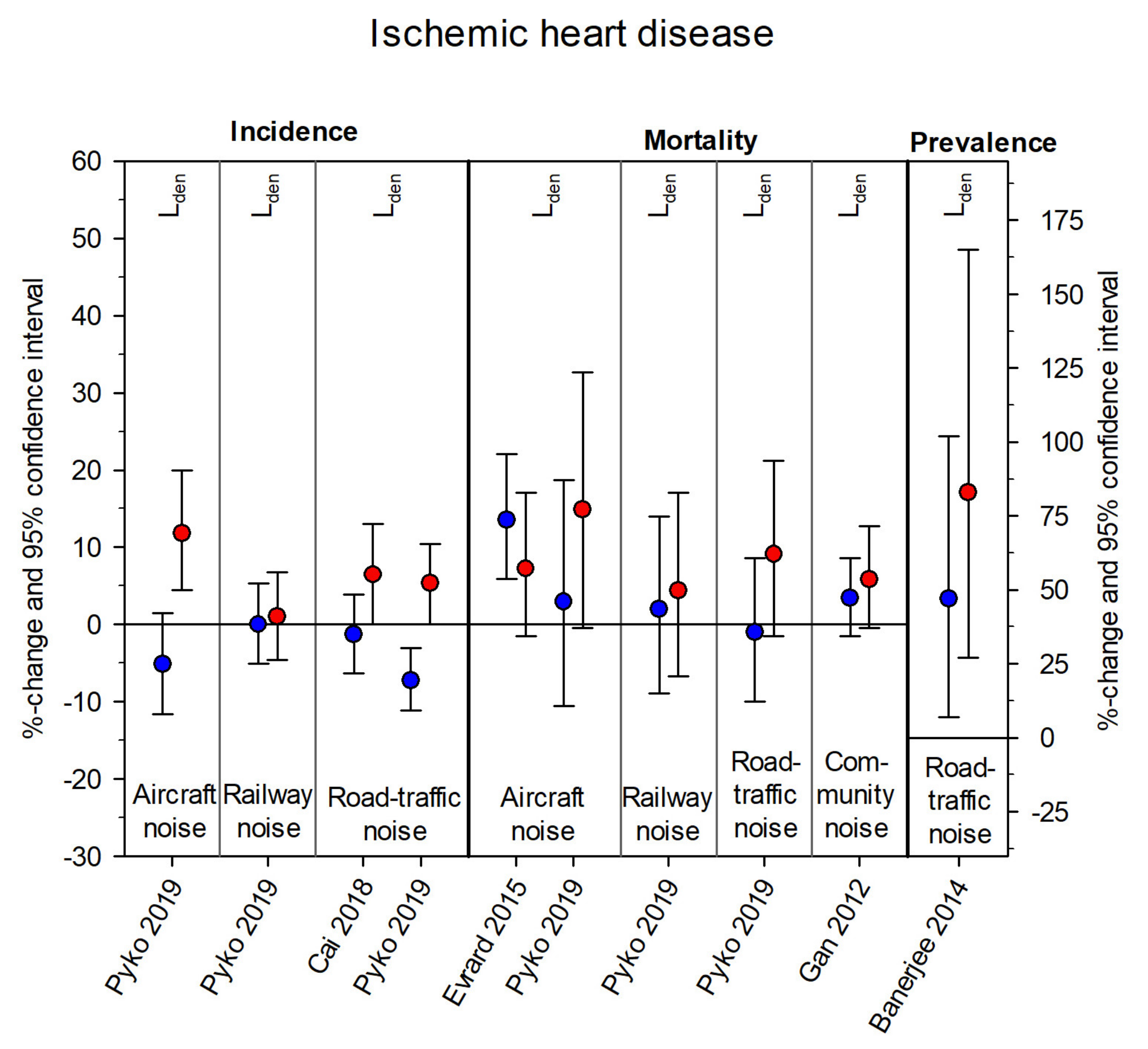
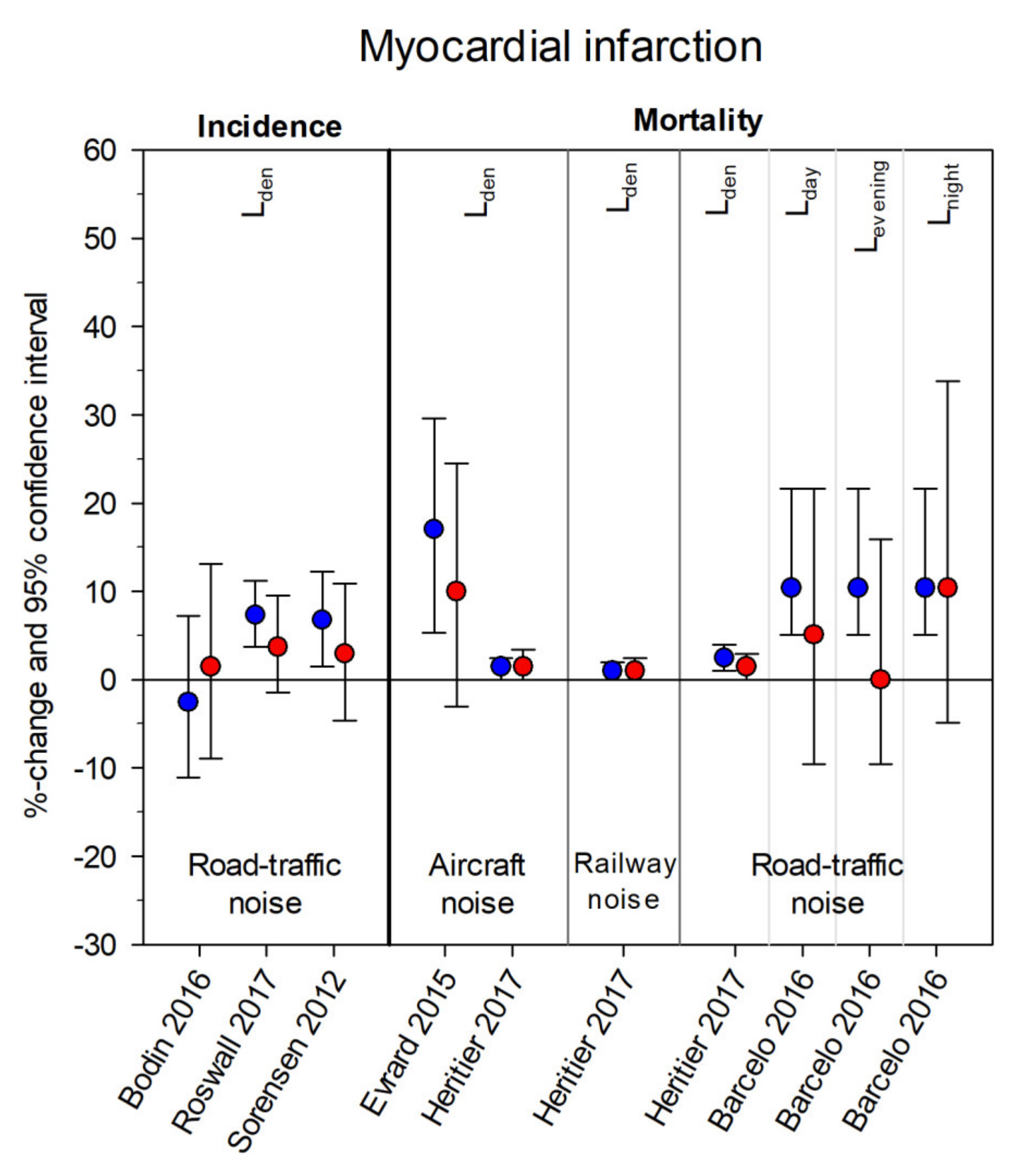
3.5. Sex/Gender Differences in the Association of Environmental Noise and Cardiovascular Diseases
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Regional Office for Europe. Burden of Disease from Environmental Noise—Quantification of Healthy Life Years los in Europe; Report No. 978 92 890 0229 5; World Health Organization: Copenhagen, Denmark, 2011. [Google Scholar]
- Hänninen, O.; Knol, A.B.; Jantunen, M.; Lim, T.A.; Conrad, A.; Rappolder, M.; Carrer, P.; Fanetti, A.C.; Kim, R.; Buekers, J.; et al. Environmental burden of disease in Europe: Assessing nine risk factors in six countries. Environ. Health Perspect. 2014, 122, 439–446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Environment Agency. Health Risks Caused by Environmental Noise in Europe. Briefing no. 21/2020. Available online: https://www.eea.europa.eu/publications/health-risks-caused-by-environmental (accessed on 22 December 2020).
- Münzel, T.; Gori, T.; Babisch, W.; Basner, M. Cardiovascular effects of environmental noise exposure. Eur. Heart J. 2014, 35, 829–836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Babisch, W. The Noise/Stress Concept, Risk Assessment and Research Needs. Noise Health 2002, 4, 1–11. [Google Scholar]
- Münzel, T.; Sørensen, M.; Schmidt, F.; Schmidt, E.; Steven, S.; Kröller-Schön, S.; Daiber, A. The Adverse Effects of Environmental Noise Exposure on Oxidative Stress and Cardiovascular Risk. Antioxid. Redox Signal. 2018, 28, 873–908. [Google Scholar] [CrossRef]
- Al’Absi, M. The Neurosciences of Pain, Stress and Emotion—Psychological and Clinical Implications; Academic Press: Cambdrige, MA, USA, 2016. [Google Scholar]
- Kajantie, E.; Phillips, D.I. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology 2006, 31, 151–178. [Google Scholar] [CrossRef]
- Day, S.; Mason, R.; Lagosky, S.; Rochon, A.P. Integrating and evaluating sex and gender in health research. Health Res. Policy Syst. 2016, 14, 75. [Google Scholar] [CrossRef] [Green Version]
- Vlassoff, C. Gender differences in determinants and consequences of health and illness. J. Health Popul. Nutr. 2007, 25, 47–61. [Google Scholar] [PubMed]
- Krieger, N. Genders, sexes, and health: What are the connections—And why does it matter? Int. J. Epidemiol. 2003, 32, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Hammarström, A.; Johansson, K.; Annandale, E.; Ahlgren, C.; Aléx, L.; Christianson, M.; Elwér, S.; Eriksson, C.; Fjellman-Wiklund, A.; Gilenstam, K.; et al. Central gender theoretical concepts in health research: The state of the art. J. Epidemiol. Community Health 2014, 68, 185–190. [Google Scholar] [CrossRef]
- Krieger, N. Embodiment: A conceptual glossary for epidemiology. J. Epidemiol. Community Health 2005, 59, 350–355. [Google Scholar] [CrossRef]
- Springer, K.W.; Mager Stellman, J.; Jordan-Young, R.M. Beyond a catalogue of differences: A theoretical frame and good practice guidelines for researching sex/gender in human health. Social Sci. Med. 2012, 74, 1817–1824. [Google Scholar] [CrossRef]
- Bolte, G.; Nanninga, S.; Dandolo, L. Sex/Gender Differences in the Association between Residential Green Space and Self-Rated Health-A Sex/Gender-Focused Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 4818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heidari, S.; Babor, T.F.; De Castro, P.; Tort, S.; Curno, M. Sex and Gender Equity in Research: Rationale for the SAGER guidelines and recommended use. Res. Integr. Peer Rev. 2016, 1, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Environmental Noise Guidelines for the European Region; World Health Organization: Geneva, Switzerland, 2018; p. 160. [Google Scholar]
- Van Kempen, E.E.M.M.; Casas, M.; Pershagen, G.; Foraster, M. Cardiovascular and Metabolic Effects of Environmental Noise—Systematic Evidence Review in the Framework of the Development of the WHO Environmental Noise Guidelines for the European Region; RIVM Report 2017-0078; National Institute for Public Health and the Environment: Bilthoven, The Netherlands, 2018. [Google Scholar]
- van Kamp, I.; Simon, S.; Notley, H.; Baliatsas, C.; van Kempen, E. Evidence Relating to Environmental Noise Exposure and Annoyance, Sleep Disturbance, Cardio-Vascular and Metabolic Health Outcomes in the Context of IGCB (N): A Scoping Review of New Evidence. Int. J. Environ. Res. Public Health 2020, 17, 3016. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- WHO Global Air Quality Guidelines Working Group on Risk of Bias Assessment. Risk of Bias Assessment Instrument for Systematic Reviews Informing WHO Global Air Quality Guidelines; World Health Organization: Copenhagen, Denmark, 2020. [Google Scholar]
- Babisch, W.; Wolke, G.; Heinrich, J.; Straff, W. Road traffic noise and hypertension--accounting for the location of rooms. Environ. Res. 2014, 133, 380–387. [Google Scholar] [CrossRef]
- Banerjee, D.; Das, P.P.; Fouzdar, A. Urban residential road traffic noise and hypertension: A cross-sectional study of adult population. J. Urban. Health Bull. N. Y. Acad. Med. 2014, 91, 1144–1157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banerjee, D.; Das, P.P.; Foujdar, A. Association between road traffic noise and prevalence of coronary heart disease. Environ. Monit. Assess. 2014, 186, 2885–2893. [Google Scholar] [CrossRef]
- Barcelo, M.A.; Varga, D.; Tobias, A.; Diaz, J.; Linares, C.; Saez, M. Long term effects of traffic noise on mortality in the city of Barcelona, 2004-2007. Environ. Res. 2016, 147, 193–206. [Google Scholar] [CrossRef]
- Barregard, L.; Bonde, E.; Ohrstrom, E. Risk of hypertension from exposure to road traffic noise in a population-based sample. Occup. Environ. Med. 2009, 66, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Bluhm, G.L.; Berglind, N.; Nordling, E.; Rosenlund, M. Road traffic noise and hypertension. Occup. Environ. Med. 2007, 64, 122–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bodin, T.; Bjork, J.; Mattisson, K.; Bottai, M.; Rittner, R.; Gustavsson, P.; Jakobsson, K.; Ostergren, P.O.; Albin, M. Road traffic noise, air pollution and myocardial infarction: A prospective cohort study. Int. Arch. Occup. Environ. Health 2016, 89, 793–802. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Hodgson, S.; Blangiardo, M.; Gulliver, J.; Morley, D.; Fecht, D.; Vienneau, D.; de Hoogh, K.; Key, T.; Hveem, K.; et al. Road traffic noise, air pollution and incident cardiovascular disease: A joint analysis of the HUNT, EPIC-Oxford and UK Biobank cohorts. Environ. Int. 2018, 114, 191–201. [Google Scholar] [CrossRef] [PubMed]
- de Kluizenaar, Y.; Gansevoort, R.T.; Miedema, H.M.; de Jong, P.E. Hypertension and road traffic noise exposure. J. Occup. Environ. Med. 2007, 49, 484–492. [Google Scholar] [CrossRef]
- Dratva, J.; Phuleria, H.C.; Foraster, M.; Gaspoz, J.M.; Keidel, D.; Kunzli, N.; Liu, L.J.; Pons, M.; Zemp, E.; Gerbase, M.W.; et al. Transportation noise and blood pressure in a population-based sample of adults. Environ. Health Perspect. 2012, 120, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Dzhambov, A.M.; Dimitrova, D.D. Association between Noise Pollution and Prevalent Ischemic Heart Disease. Folia Med. 2016, 58, 273–281. [Google Scholar] [CrossRef] [Green Version]
- Eriksson, C.; Bluhm, G.; Hilding, A.; Ostenson, C.G.; Pershagen, G. Aircraft noise and incidence of hypertension—Gender specific effects. Environ. Res. 2010, 110, 764–772. [Google Scholar] [CrossRef]
- Eriksson, C.; Nilsson, M.E.; Willers, S.M.; Gidhagen, L.; Bellander, T.; Pershagen, G. Traffic noise and cardiovascular health in Sweden: The roadside study. Noise Health 2012, 14, 140–147. [Google Scholar] [CrossRef] [Green Version]
- Evrard, A.S.; Bouaoun, L.; Champelovier, P.; Lambert, J.; Laumon, B. Does exposure to aircraft noise increase the mortality from cardiovascular disease in the population living in the vicinity of airports? Results of an ecological study in France. Noise Health 2015, 17, 328–336. [Google Scholar] [CrossRef]
- Evrard, A.S.; Lefevre, M.; Champelovier, P.; Lambert, J.; Laumon, B. Does aircraft noise exposure increase the risk of hypertension in the population living near airports in France? Occup. Environ. Med. 2017, 74, 123–129. [Google Scholar] [CrossRef] [Green Version]
- Foraster, M.; Kunzli, N.; Aguilera, I.; Rivera, M.; Agis, D.; Vila, J.; Bouso, L.; Deltell, A.; Marrugat, J.; Ramos, R.; et al. High blood pressure and long-term exposure to indoor noise and air pollution from road traffic. Environ. Health Perspect. 2014, 122, 1193–1200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gan, W.Q.; Davies, H.W.; Koehoorn, M.; Brauer, M. Association of long-term exposure to community noise and traffic-related air pollution with coronary heart disease mortality. Am. J. Epidemiol. 2012, 175, 898–906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halonen, J.I.; Dehbi, H.M.; Hansell, A.L.; Gulliver, J.; Fecht, D.; Blangiardo, M.; Kelly, F.J.; Chaturvedi, N.; Kivimaki, M.; Tonne, C. Associations of night-time road traffic noise with carotid intima-media thickness and blood pressure: The Whitehall II and SABRE study cohorts. Environ. Int. 2017, 98, 54–61. [Google Scholar] [CrossRef] [Green Version]
- Heritier, H.; Vienneau, D.; Foraster, M.; Eze, I.C.; Schaffner, E.; Thiesse, L.; Rudzik, F.; Habermacher, M.; Kopfli, M.; Pieren, R.; et al. Transportation noise exposure and cardiovascular mortality: A nationwide cohort study from Switzerland. Eur. J. Epidemiol. 2017, 32, 307–315. [Google Scholar] [CrossRef]
- Huss, A.; Spoerri, A.; Egger, M.; Roosli, M. Aircraft noise, air pollution, and mortality from myocardial infarction. Epidemiology 2010, 21, 829–836. [Google Scholar] [CrossRef]
- Jarup, L.; Babisch, W.; Houthuijs, D.; Pershagen, G.; Katsouyanni, K.; Cadum, E.; Dudley, M.L.; Savigny, P.; Seiffert, I.; Swart, W.; et al. Hypertension and exposure to noise near airports: The HYENA study. Environ. Health Perspect. 2008, 116, 329–333. [Google Scholar] [CrossRef]
- Pitchika, A.; Hampel, R.; Wolf, K.; Kraus, U.; Cyrys, J.; Babisch, W.; Peters, A.; Schneider, A. Long-term associations of modeled and self-reported measures of exposure to air pollution and noise at residence on prevalent hypertension and blood pressure. Sci. Total Environ. 2017, 593–594, 337–346. [Google Scholar] [CrossRef]
- Pyko, A.; Lind, T.; Mitkovskaya, N.; Ogren, M.; Ostenson, C.G.; Wallas, A.; Pershagen, G.; Eriksson, C. Transportation noise and incidence of hypertension. Int. J. Hyg. Environ. Health 2018, 221, 1133–1141. [Google Scholar] [CrossRef] [Green Version]
- Pyko, A.; Andersson, N.; Eriksson, C.; de Faire, U.; Lind, T.; Mitkovskaya, N.; Ogren, M.; Ostenson, C.G.; Pedersen, N.L.; Rizzuto, D.; et al. Long-term transportation noise exposure and incidence of ischaemic heart disease and stroke: A cohort study. Occup. Environ. Med. 2019, 76, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Rhee, M.Y.; Kim, H.Y.; Roh, S.C.; Kim, H.J.; Kwon, H.J. The effects of chronic exposure to aircraft noise on the prevalence of hypertension. Hypertens. Res. 2008, 31, 641–647. [Google Scholar] [CrossRef]
- Roswall, N.; Raaschou-Nielsen, O.; Ketzel, M.; Gammelmark, A.; Overvad, K.; Olsen, A.; Sorensen, M. Long-term residential road traffic noise and NO2 exposure in relation to risk of incident myocardial infarction—A Danish cohort study. Environ. Res. 2017, 156, 80–86. [Google Scholar] [CrossRef]
- Selander, J.; Nilsson, M.E.; Bluhm, G.; Rosenlund, M.; Lindqvist, M.; Nise, G.; Pershagen, G. Long-term exposure to road traffic noise and myocardial infarction. Epidemiology 2009, 20, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, M.; Hvidberg, M.; Hoffmann, B.; Andersen, Z.J.; Nordsborg, R.B.; Lillelund, K.G.; Jakobsen, J.; Tjonneland, A.; Overvad, K.; Raaschou-Nielsen, O. Exposure to road traffic and railway noise and associations with blood pressure and self-reported hypertension: A cohort study. Environ. Health A Glob. Access Sci. Source 2011, 10, 92. [Google Scholar] [CrossRef] [Green Version]
- Sorensen, M.; Andersen, Z.J.; Nordsborg, R.B.; Jensen, S.S.; Lillelund, K.G.; Beelen, R.; Schmidt, E.B.; Tjonneland, A.; Overvad, K.; Raaschou-Nielsen, O. Road traffic noise and incident myocardial infarction: A prospective cohort study. PLoS ONE 2012, 7, e39283. [Google Scholar] [CrossRef]
- Zeeb, H.; Hegewald, J.; Schubert, M.; Wagner, M.; Droge, P.; Swart, E.; Seidler, A. Traffic noise and hypertension—Results from a large case-control study. Environ. Res. 2017, 157, 110–117. [Google Scholar] [CrossRef]
- Altman, D.G.; Bland, J.M. Interaction revisited: The difference between two estimates. BMJ 2003, 326, 219. [Google Scholar] [CrossRef] [Green Version]
- Gahagan, J.; Gray, K.; Whynacht, A. Sex and gender matter in health research: Addressing health inequities in health research reporting. Int. J. Equity Health 2015, 14, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, J.L.; Greaves, L.; Repta, R. Better science with sex and gender: Facilitating the use of a sex and gender-based analysis in health research. Int. J. Equity Health 2009, 8, 14. [Google Scholar] [CrossRef] [Green Version]
- Johnson, J.L.; Repta, R. Sex and Gender—Beyond the Binaries. In Designing and Conducting Gender, Sex, & Health Research; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Lindqvist, A.; Sendén, M.G.; Renström, E.A. What is gender, anyway: A review of the options for operationalising gender. Psychol. Sex. 2020. [Google Scholar] [CrossRef]
- Bolte, G.; David, M.; Dębiak, M.; Fiedel, L.; Hornberg, C.; Kolossa-Gehring, M.; Kraus, U.; Lätzsch, R.; Paeck, T.; Palm, K.; et al. Integration of sex/gender into environmental health research. Results of the interdisciplinary research network Sex/Gender-Environment-Health (GeUmGe-NET). Bundesgesundheitsblatt Gesundh. Gesundh. 2018, 61, 737–746. [Google Scholar] [CrossRef]
- Runnels, V.; Tudiver, S.; Doull, M.; Boscoe, M. The challenges of including sex/gender analysis in systematic reviews: A qualitative survey. Syst. Rev. 2014, 3, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Münzel, T.; Sørensen, M.; Daiber, A. Transportation noise pollution and cardiovascular disease. Nat. Reviews. Cardiol. 2021. [Google Scholar] [CrossRef]
- Bauer, G.R. Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Soc. Sci. Med. 2014, 110, 10–17. [Google Scholar] [CrossRef] [Green Version]
- Kapilashrami, A.; Hankivsky, O. Intersectionality and why it matters to global health. Lancet 2018, 391, 2589–2591. [Google Scholar] [CrossRef]
- Pelletier, R.; Khan, N.A.; Cox, J.; Daskalopoulou, S.S.; Eisenberg, M.J.; Bacon, S.L.; Lavoie, K.L.; Daskupta, K.; Rabi, D.; Humphries, K.H.; et al. Sex Versus Gender-Related Characteristics: Which Predicts Outcome After Acute Coronary Syndrome in the Young? J. Am. Coll. Cardiol. 2016, 67, 127–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Annandale, E.; Hunt, K. Masculinity, femininity and sex: An exploration of their relative contribution to explaining gender differences in health. Soc. Health Illnes 1990, 12, 24–46. [Google Scholar] [CrossRef]
- Clougherty, J.E. A growing role for gender analysis in air pollution epidemiology. Environ. Health Perspect. 2010, 118, 167–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Csikszentmihalyi, M.; Larson, R. Validity and reliability of the Experience-Sampling Method. J. Nerv. Ment. Dis. 1987, 175. [Google Scholar] [CrossRef]
- Dimotakis, N.; Ilies, R.; Judge, T.A. Experience Sampling Methodology. In Modern Research Methods for the Study of Behaviour in Organizations; Cortina, J.M., Landis, R.S., Eds.; Routledge: London, UK, 2013; pp. 319–348. [Google Scholar]



| Reference | Study Type | Study Population | Cardio- Vascular Outcome | Operationalization of Sex/Gender | Assessment of Sex/Gender | Terminology | Rationale for Testing Sex/Gender Differences | Discussion of Sex/Gender-Specific Results |
|---|---|---|---|---|---|---|---|---|
| Babisch et al. (2014) [22] | Cross- Sectional | N = 1766 (57.3% Female) Berlin, Germany | HT | Binary | Not Reported | Sex, Gender (Inter- changeably) | Different Distribution of Sex/Gender in Study Sample and Source Population | Only Summary of Results |
| Banerjee et al. (2014a) [23] | Cross- Sectional | N = 909 (58.7% Female) Asansol, India | HT | Binary | Not Reported | Gender | Previous Research on Gender Differences in Arterial Hypertension in Relation to Noise Exposure | Comparison with Other Results, Explanations Provided |
| Banerjee et al. (2014b) [24] | Cross- Sectional | N = 909 (58.6% Female) Asansol, India | IHD | Binary | Not Reported | Gender | Previous Research on Gender Differences in Coronary Disease Risk in Relation to Noise Exposure | Comparison with Other Results, Explanations Provided |
| Barcelo et al. (2016) [25] | Case-Control | Ncases HT = 4412, Ncontrols HT = 4412 Ncases MI = 6439, Ncontrols MI = 6439 Barcelona, Spain | HT, MI | Binary | Death Certificates | Sex | Previous Research on Gender Differences in Adverse Health Effects in Relation to Noise Exposure | Comparison with Other Results |
| Barregard et al. (2009) [26] | Cross- Sectional | N = 1953 (53.0% Female) Lerum, Sweden | HT | Binary | Not Reported | Sex, Gender (Inter- changeably) | Not Reported | Comparison with Other Results |
| Bluhm et al. (2014) [27] | Cross- Sectional | N = 667 (53.5% Female) Municipality 15 km north of Stockholm City, Sweden | HT | Binary | National Population Register | Sex | Not Reported | Comparison with Other Results, Explanations Provided |
| Bodin et al. (2016) [28] | Cohort | N = 12,843 (55.0% Female) Skane, Sweden | MI | Binary | Not Reported | Sex | Not Reported | Comparison with Other Results, Explanations Provided |
| Cai et al. (2018) [29] | Cohort (HUNT, EPIC Oxford, UK Biobank) | N = 355,732 (58.0% Female) Norway; United Kingdom | IHD | Binary | Not Reported | Sex | Not Reported | Only Summary of Results |
| De Kluizenaar et al. (2007) [30] | Cross- Sectional (PREVENT-Study) | N = 7744 (54.7% Female) Groningen, the Netherlands | HT | Binary | Not Reported | Sex, Gender (Inter- changeably) | Not Reported | Comparison with Other Results |
| Dratva et al. (2012) [31] | Cross- Sectional | N = 6450 (51.1% Female) from the Second Survey of the SAPALDIA Cohort Study Switzerland | SBP, DBP | Binary | Not Reported | Sex | Not Reported | – |
| Dzhambov et al. (2016) [32] | Cross- Sectional | N = 513 (64.3% Female) Plovdiv, Bulgaria | IHD | Binary | Questionnaire | Gender | Not Reported | – |
| Eriksson et al. (2010) [33] | Cohort (SDDP) | N = 3902 (63.5% Female) Stockholm County, Sweden | HT | Binary | Not Reported | Sex, Gender (Inter- changeably) | Previous Research on Hypertension in Relation to Aircraft Noise. Uncertainties Regarding Potential Sex/Gender Differences | Comparison with Other Results, Explanations Provided |
| Eriksson et al. (2012) [34] | Cross- Sectional | N = 2493 (55.7% Female) Sweden | HT, IHD | Binary | Not Reported | Sex | Not Reported | Comparison with Other Results |
| Evrard et al. (2015) [35] | Ecological | N = 1.9 million France | IHD, MI | Binary | Not Reported | Gender | Not Reported | Only Summary of Results |
| Evrard et al. (2017) [36] | Cohort (HYENA-Study) | N = 1230 (55.9% Female) France | HT SBP-and DBP-Changes | Binary | Not Reported | Sex, Gender (Inter- changeably) | No Consistent Evidence on Gender Differences in the Risk of Hypertension Related to Aircraft Noise Exposure | Comparison with Other Results, Explanations Provided |
| Foraster et al. (2014) [37] | Cohort (REGICOR-Study) | N = 1929 (54.4% Female) Girona, Spain | HT | Binary | Not Reported | Sex | Not Reported | Comparison with Other Results |
| Gan et al. (2012) [38] | Cohort | N = 445,868 (54.0% Female) Vancouver, Canada | IHD | Binary | Not Reported | Sex | Not Reported | Comparison with Other Results, Explanations Provided |
| Halonen et al. (2017) [39] | Cross- Sectional (WHII and SABRE Study) | N = 4392 (41.0% Female) London, United Kingdom | SBP-and DBP-Changes | Binary | Not Reported | Sex | Not Reported | – |
| Hertitier et al. (2017) [40] | Cohort (SNC) | N = 4,415,206 (47.9% Female) Switzerland | MI | Binary | Not Reported | Sex | Not Reported | Comparison with Other Results |
| Huss et al. (2010) [41] | Cohort (SNC) | N = 4.6 million Switzerland | MI | Binary | National census database | Sex | Not Reported | Comparison with Other Results |
| Jarup et al. (2008) [42] | Cross- Sectional (HYENA-Study) | N = 1076 (50.7% Female) United Kingdom, Germany, the Netherlands, Sweden, Italy, Greece | HT | Binary | Not Reported | Sex | Not Reported | Comparison with Other Results, Explanations Provided |
| Pitchika et al. (2017) [43] | Cohort (KORA F4) | N = 2452 (50.5% Female) Augsburg, Germany | HT SBP- and DBP-Changes | Binary | Not Reported | Sex | Not Reported | Comparison with Other Results |
| Pyko et al. (2018) [44] | Cohort (SDPP) | N = 4854 (59.1% Female) Stockholm county, Sweden | HT | Binary | Not Reported | Sex | Not Reported | Comparison with Other Results |
| Pyko et al. (2019) [45] | Cohort (SDPP, SIXTY, SALT, SNAC-K) | N = 20,012 (57.4% Female) Sweden | IHD | Binary | Not Reported | Sex, Gender (Inter- changeably) | Not Reported | Comparison with Other Results, Explanations Provided |
| Rhee et al. (2008) [46] | Cross- Sectional | Nexposed = 308 (58.4% Female), Ncontrol = 105 (59.0% Female) Korea | HT | Binary | Not Reported | Sex, Gender (Inter- changeably) | Not Reported | Comparison with Other Results, Explanations Provided |
| Roswall et al. (2017) [47] | Cohort (Diet, Cancer and Health Cohort) | N = 50,744 (53.5% Female) Copenhagen or Aarhus, Denmark | MI | Binary | Not Reported | Sex | Sex was the Only Variable for Which no Deviation of the Proportional Hazard Assumption of the Cox Models was Found | - |
| Selander et al. (2009) [48] | Case-Control (SHEEP) | Ncases = 1517 (28.6% Female), Ncontrols = 2059 (33.7% Female) Stockholm County, Sweden | MI | Binary | Not Reported | Sex | Not Reported | Only Summary of Results |
| Sørensen et al. (2011) [49] | Cohort (Diet, Cancer and Health Cohort) | N = 32,635 Copenhagen or Aarhus, Denmark | HT SBP- and DBP-Changes | Binary | Not Reported | Gender | Not Reported | Comparison with Other Results |
| Sørensen et al. (2012) [50] | Cohort (Diet, Cancer and Health Cohort) | N = 50,614 (52.0% Female) Copenhagen or Aarhus, Denmark | MI | Binary | Not Reported | Sex | Not Reported | Comparison with Other Results |
| Zeeb et al. (2017) [51] | Case-Control (NORAH) | Ncases = 137,577 (54.3% Female), Ncontols = 355,591 (54.0% Female) Frankfurt, Germany | HT | Binary | Not Reported | Sex | Not Reported | Comparison with Other Results |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rompel, S.; Schneider, A.; Peters, A.; Kraus, U.; on behalf of the INGER Study Group. Sex/Gender-Differences in the Health Effects of Environmental Noise Exposure on Hypertension and Ischemic Heart Disease—A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 9856. https://doi.org/10.3390/ijerph18189856
Rompel S, Schneider A, Peters A, Kraus U, on behalf of the INGER Study Group. Sex/Gender-Differences in the Health Effects of Environmental Noise Exposure on Hypertension and Ischemic Heart Disease—A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(18):9856. https://doi.org/10.3390/ijerph18189856
Chicago/Turabian StyleRompel, Sarah, Alexandra Schneider, Annette Peters, Ute Kraus, and on behalf of the INGER Study Group. 2021. "Sex/Gender-Differences in the Health Effects of Environmental Noise Exposure on Hypertension and Ischemic Heart Disease—A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 18: 9856. https://doi.org/10.3390/ijerph18189856






