Previous Intensive Running or Swimming Negatively Affects CPR Effectiveness
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
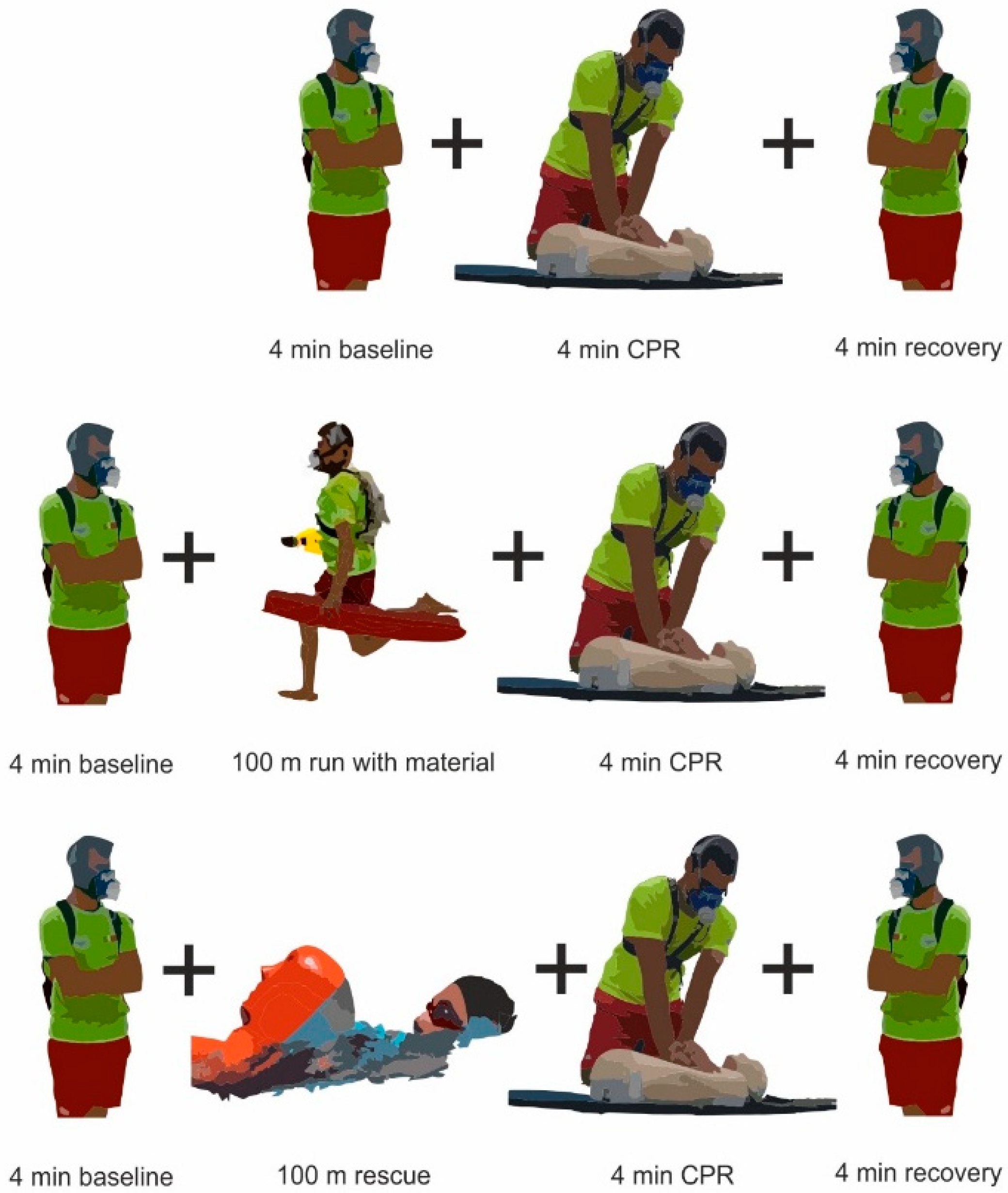
2.2. Protocol
2.3. Measurement Equipment and Data Acquisition
2.4. Data Filtering and Processing Prior to Analysis
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abraldes, J.A.; Fernandes, R.J.; Rodríguez, N.; Sousa, A. Is Rescuer Cardiopulmonary Resuscitation Jeopardised by Previous Fatiguing Exercise? Int. J. Environ. Res. Public Health 2020, 17, 6668. [Google Scholar] [CrossRef]
- Sousa, A.; Fernandes, R.J.; Rodríguez, N.; Abraldes, J.A. Influence of a 100-M simulated in-water rescue on cardiopulmonary parameters. Prehosp. Emerg. Care 2017, 21, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Barcala-Furelos, R.; Fernández-Méndez, M.; Cano-Noguera, F.; Otero-Agra, M.; Morán-Navarro, R.; Martínez-Isasi, S. Measuring the physiological impact of extreme heat on lifeguards during cardiopulmonary resuscitation. Randomized simulation study. Am. J. Emerg Med. 2020, 38, 2019–2027. [Google Scholar] [CrossRef]
- Yazar, M.A.; Açikgöz, M.B.; Bayram, A. Does chest compression during cardiopulmonary resuscitation provide sufficient cerebral oxygenation? Turk. J. Med. Sci. 2019, 49, 311–317. [Google Scholar] [CrossRef]
- Safar, P. Cerebral resuscitation after cardiac arrest: A review. Circulation 1986, 74, 138–153. [Google Scholar]
- Meaney, P.A.; Bobrow, B.J.; Mancini, M.E.; Christenson, J.; de Caen, A.R.; Bhanji, F.; Abella, B.S.; Kleinman, M.E.; Edelson, D.P.; Berg, R.A.; et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: A consensus statement from the American Heart Association. Circulation 2013, 128, 417–435. [Google Scholar] [CrossRef]
- Vadeboncoeur, T.; Stolz, U.; Panchal, A.; Silver, A.; Venuti, M.; Tobin, J.; Smith, G.; Nunez, M.; Karamooz, M.; Spaite, D.; et al. Chest compression depth and survival in out-of-hospital cardiac arrest. Resuscitation 2014, 85, 182–188. [Google Scholar] [CrossRef]
- Stiell, I.G.; Brown, S.P.; Nichol, G.; Cheskes, S.; Vaillancourt, C.; Callaway, C.W.; Morrison, L.J.; Christenson, J.; Aufderheide, T.P.; Davis, D.P.; et al. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation 2014, 130, 1962–1970. [Google Scholar] [CrossRef]
- Idris, A.H.; Guffey, D.; Pepe, P.E.; Brown, S.P.; Brooks, S.C.; Callaway, C.W.; Christenson, J.; Davis, D.P.; Daya, M.R.; Gray, R.; et al. Chest compression rates and survival following out-of-hospital cardiac arrest. Crit. Care Med. 2015, 43, 840–848. [Google Scholar] [CrossRef] [PubMed]
- Christenson, J.; Andrusiek, D.; Everson-Stewart, S.; Kudenchuk, P.; Hostler, D.; Powell, J.; Callaway, C.W.; Bishop, D.; Vaillancourt, C.; Davis, D.; et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation 2009, 120, 1241–1247. [Google Scholar] [CrossRef]
- Neumar, R.; Shuster, M.; Callaway, C.; Gent, L.; Atkins, D.; Bhanji, F.; Brooks, S.; Caen, A.; Donnino, M.W.; Ferrer, J.M.E.; et al. 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015, 115, S315–S367. [Google Scholar] [CrossRef] [PubMed]
- Perkins, G.D.; Handley, A.J.; Koster, R.W.; Castrén, M.; Smyth, M.A.; Olasveengen, T.; Monsieurs, K.G.; Raffay, V.; Gräsner, J.T.; Wenzel, V. European resuscitation council guidelines for resuscitation 2015: Section 2. Adult basic life support and automated external defibrillation. Resuscitation 2015, 95, 81–99. [Google Scholar] [CrossRef]
- Sugerman, T.; Edelson, P.; Leary, M.; Weidman, K.; Herzberg, L.; Hoek, L.V.; Becker, B.; Abella, S. Rescuer fatigue during actual in-hospital cardiopulmonary resuscitation with audiovisual feedback: A prospective multicenter study. Resuscitation 2009, 80, 981–984. [Google Scholar] [CrossRef]
- Ochoa, F.J.; Ramalle-Gomara, E.; Lisa, V.; Saralegui, I. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation 1998, 37, 149–152. [Google Scholar] [CrossRef]
- Ashton, A.; McCluskey, A.; Gwinnutt, C.; Keenan, A. Effect of rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation 2002, 55, 151–155. [Google Scholar] [CrossRef]
- Hightower, D.; Thomas, S.; Stone, C.; Dunn, K.; March, J. Decay in quality of closed-chest compressions over time. Ann. Emerg. Med. 1995, 26, 300–303. [Google Scholar] [CrossRef]
- Pallarés, J.G.; Lillo-Bevia, J.R.; Morán-Navarro, R.; Cerezuela-Espejo, V.; Mora-Rodriguez, R. Time to exhaustion during cycling is not well predicted by critical power calculations. Appl. Physiol. Nutr. Metab. 2020, 45, 753–760. [Google Scholar] [CrossRef]
- Fernandes, R.; Vilas-Boas, J. Time to exhaustion at the VO2max velocity in swimming: A review. J. Hum. Kinet. 2012, 32, 121–134. [Google Scholar] [CrossRef]
- Santos, J.A.; Affonso, H.O.; Boullosa, D.; Pereira, T.M.C.; Fernandes, R.J.; Conceição, F. Extreme blood lactate rising after very short efforts in top-level track and field male sprinters. Res. Sports Med. 2021. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, M.; Laursen, P.B. High-intensity interval training, solutions to the programming puzzle. Sports Med. 2013, 43, 313–338. [Google Scholar] [CrossRef] [PubMed]
- Pallarés, J.G.; López-Samanes, Á.; Fernández-Elías, V.E.; Aguado-Jiménez, R.; Ortega, J.F.; Gómez, C.; Ventura, R.; Segura, J.; Mora-Rodríguez, R. Pseudoephedrine and circadian rhythm interaction on neuromuscular performance. Scand. J. Med. Sci. Sports 2015, 25, e603–e612. [Google Scholar] [CrossRef]
- Abraldes, J.A.; Fernandes, R.J.; Soares, S.; Lima, A.B.; Vilas-Boas, J.P. Assessment of a lifesaver’s instantaneous velocity in mannequin carry using different types of fins. Open Sports Sci. J. 2010, 3, 19–21. [Google Scholar] [CrossRef][Green Version]
- Fernandes, R.J.; de Jesus, K.; Baldari, C.; de Jesus, K.; Sousa, A.C.; Vilas-Boas, J.P.; Guidetti, L. Different VO2max time-averaging intervals in swimming. Int. J. Sports Med. 2012, 33, 1010–1015. [Google Scholar] [CrossRef]
- de Jesus, K.; Guidetti, L.; de Jesus, K.; Vilas-Boas, J.P.; Baldari, C.; Fernandes, R.J. Which are the best VO2 sampling intervals to characterize low to severe swimming intensities? Int. J. Sports Physiol. Perform. 2014, 35, 1030–1036. [Google Scholar] [CrossRef]
- Sarafian, D.; Schutz, Y.; Montani, J.P.; Dulloo, A.G.; Miles-Chan, J.L. Gender difference in substrate oxidation during low- intensity isometric exercise in young adults. Appl. Physiol. Nutrit. Metabol. 2016, 41, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Sheak, K.; Douglas, W.; Leary, M.; Babaeizadeh, S.; Uyuen, T.; Zive, D.; Owens, P.; Edelson, D.; Daya, M.; Idris, A.; et al. Quantitative relationship between end-tidal carbon dioxide and CPR quality during both in-hospital and out-of-hospital cardiac arrest. Resuscitation 2015, 89, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Kern, K.B.; Sanders, A.B.; Voorhees, W.D.; Babbs, C.F.; Tacker, W.A.; Ewy, G.A. Changes in expired end-tidal carbon dioxide during cardiopulmonary resuscitation in dogs: A prognostic guide for resuscitation efforts. J. Am. Coll. Cardiol. 1989, 13, 1184–1189. [Google Scholar] [CrossRef]
- Wang, A.Y.; Huang, C.H.; Chang, W.T.; Tsai, M.S.; Wang, C.H.; Chen, W.J. Initial end-tidal CO2 partial pressure predicts outcomes of in-hospital cardiac arrest. Am. J. Emerg. Med. 2016, 34, 2367–2371. [Google Scholar] [CrossRef] [PubMed]
- Iserbyt, P.; Schouppe, G.; Charlier, N. A multiple linear regression analysis of factors affecting the simulated Basic Life Support (BLS) performance with Automated External Defibrillator (AED) in Flemish lifeguards. Resuscitation 2015, 89, 70–74. [Google Scholar] [CrossRef]
- Buono, M.J.; Golding, L. The energy cost of performing cardiopulmonary resuscitation. Med. Sci. Sports Exerc. 1980, 12, 118. [Google Scholar]
- Gómez, C.A.; Pérez, V.R.; Barcala-Furelos, R.J.; Palacios-Aguilar, J. Efecto de la fatiga física del socorrista en los primeros cuatro minutos de la reanimación cardiopulmonar posrescate acuático. Emergencias 2013, 25, 184–190. [Google Scholar]
- Wallace, S.; Abella, S.; Becker, B. Quantifying the effect of cardiopulmonary resuscitation quality on cardiac arrest outcome. A systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes 2013, 6, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Nolan, J.P.; Monsieurs, K.G.; Bossaert, L.; Böttiger, B.W.; Greif, R.; Lott, C.; Madar, J.; Olasveengen, T.M.; Roehr, C.C.; Semeraro, F.; et al. European Resuscitation Council COVID-19 guidelines executive summary. Resuscitation 2020, 153, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Meursing, B.J. The history of resuscitation. In Handbook on Drowning: Prevention, Rescue, Treatment; Bierens, J., Ed.; Verlag: Amsterdam, The Netherlands; Berlin/Heidelberg, Germany, 2014; pp. 25–36. [Google Scholar]
- Adelborg, K.; Dalgas, C.; Grove, E.L.; Jørgensen, C.; Al-Mashhadi, R.H.; Løfgren, B. Mouth-to-mouth ventilation is superior to mouth-to-pocket mask and bag-valve-mask ventilation during lifeguard CPR: A randomized study. Resuscitation 2011, 82, 618–622. [Google Scholar] [CrossRef] [PubMed]
- Winkler, B.E.; Eff, A.M.; Eff, S.; Ehrmann, U.; Koch, A.; KÁhler, W.; Muth, C. Efficacy of ventilation and ventilation adjuncts during in-water-resuscitation—A randomized cross-over trial. Resuscitation 2013, 84, 1137–1142. [Google Scholar] [CrossRef]
| Variables | Rf (b·min−1) | TV (l) | VE (L·min−1) | VO2 (mL/kg/min) | R | VCO2 (mL·min−1) | HR (bpm) | PetCO2 (mmHg) | |
|---|---|---|---|---|---|---|---|---|---|
| CPRbase | Baseline | 16.6 ± 4.3 | 1.2 ± 0.5 | 18.0 ± 3.6 | 11.9 ± 3.8 | 0.95 ± 0.2 | 0.49 ± 0.1 | 88 ± 13 | 33.6 ± 4.0 |
| Cycle 3 | 28.7 ± 8.1 1 | 1.4 ± 0.4 | 36.3 ± 7.8 1 | 14.1 ± 5.3 1 | 1.14 ± 0.2 1 | 0.96 ± 0.3 1 | 112 ± 15 1 | 29.5 ± 4.2 1 | |
| Cycle 6 | 29.1 ± 8.5 2 | 1.5 ± 0.4 2 | 39.7 ± 9.1 2 | 14.9 ± 6.3 2 | 0.86 ± 0.2 2 | 1.13 ± 0.3 2 | 114 ± 14 2 | 31.6 ± 6.2 2 | |
| Cycle 9 | 27.7 ± 7.0 3 | 1.6 ± 0.4 3 | 43.2 ± 9.3 3 | 13.1 ± 4.4 3 | 0.88 ± 0.2 3 | 1.26 ± 0.3 3 | 114 ± 15 3 | 32.9 ± 5.6 | |
| Cycle 12 | 27.6 ± 7.1 4 | 1.6 ± 0.5 4 | 42.4 ± 9.9 4 | 11.6 ± 8.0 | 0.90 ± 0.2 4 | 1.21 ± 0.3 4 | 114 ± 16 4 | 33.1 ± 4.4 | |
| Total CPR | 28.2 ± 7.6 5 | 1.5 ± 0.4 5 | 40.4 ± 9.4 5 | 13.5 ± 6.2 5 | 0.94 ± 0.2 5 | 1.14 ± 0.3 5 | 114 ± 15 5 | 31.7 ± 5.3 5 | |
| Recovery | 19.2 ± 4.9 | 1.4 ± 0.4 | 24.8 ± 4.6 | 14.1 ± 5.2 | 0.91 ± 0.2 | 0.70 ± 0.2 | 95 ± 16 | 34.1 ± 3.6 | |
| CPRrun | Baseline | 16.8 ± 4.4 | 1.3 ± 0.6 | 17.9 ± 3.5 | 12.2 ± 3.6 | 0.96 ± 0.2 | 0.49 ± 0.2 | 89 ± 15 | 33.9 ± 3.8 |
| Cycle 3 | 30.1 ± 3.8 | 2.7 ± 0.5 * | 81.7 ± 16.3 1 | 22.3 ± 9.8 1 | 1.14 ± 0.3 | 2.83 ± 0.9 1 | 147 ± 16 1 | 39.2 ± 7.7 1 | |
| Cycle 6 | 29.5 ± 4.0 | 2.6 ± 0.5 * | 76.6 ± 17.9 2 | 25.5 ± 8.3 2 | 1.25 ± 0.3 2 | 2.35 ± 0.8 2 | 137 ± 18 2 | 36.5 ± 7.7 2 | |
| Cycle 9 | 30.4 ± 4.7 3 | 2.3 ± 0.5 * | 70.3 ± 17.2 3 | 23.5 ± 7.7 3 | 1.18 ± 0.3 3 | 2.04 ± 0.6 3 | 132 ± 19 3 | 35.3 ± 3.5 3 | |
| Cycle 12 | 29.9 ± 4.9 | 2.3 ± 0.5 * | 66.3 ± 15.9 4 | 20.7 ± 13.1 4 | 1.15 ± 0.3 4 | 1.85 ± 0.5 4 | 130 ± 17 4 | 34.7 ± 3.7 | |
| Total CPR | 29.9 ± 4.3 5 | 2.5 ± 0.5 * | 73.8 ± 17.7 *,5 | 23.0 ± 9.9 *,5 | 1.18 ± 0.3 *,5 | 2.27 ± 0.8 *,5 | 137 ± 19 *,5 | 36.4 ± 6.2 *,5 | |
| Recovery | 22.5 ± 5.2 * | 1.7 ± 0.5 * | 37.5 ± 9.5 * | 22.7 ± 8.7 * | 1.05 ± 0.2 * | 1.01 ± 0.3 * | 111 ± 15 * | 33.5 ± 3.3 | |
| CPRswim | Baseline | 16.7 ± 4.2 | 1.3 ± 0.4 | 17.7 ± 3.4 | 11.7 ± 3.6 | 0.96 ± 0.4 | 0.50 ± 0.1 | 92 ± 16 | 34.0 ± 3.9 |
| Swim | 21.8 ± 4.4 *,† | 1.0 ± 0.3 *,† | 93.4 ± 23.5 *,† | 19.1 ± 9.1 *,† | 1.19 ± 0.1 *,† | 2.94 ± 0.7 *,† | 77 ± 15 * | 30.01 ± 1.7 * | |
| Cycle 3 | 33.8 ± 6.3 1,† | 2.8 ± 0.7 1 | 93.4 ± 23.5 1,† | 19.8 ± 7.7 1 | 1.19 ± 0.1 | 2.58 ± 0.6 1 | 152 ± 15 1 | 37.02 ± 5.0 1,† | |
| Cycle 6 | 33.9 ± 5.1 2,† | 2.7 ± 0.6 2 | 91.3 ± 18.2 2 | 20.5 ± 8.3 2 | 1.25 ± 0.2 2 | 2.03 ± 0.3 2 | 144 ± 18 2 | 32.3 ± 4.9 † | |
| Cycle 9 | 33.3 ± 5.9 3,† | 2.4 ± 0.5 3 | 79.4 ± 14.8 3 | 19.8 ± 9.2 3 | 1.19 ± 0.1 3 | 1,77 ± 0.3 3 | 138 ± 17 3 | 30.9 ± 4.1 3,† | |
| Cycle 12 | 33.2 ± 6.3 4 | 2.3 ± 0.5 4 | 73.6 ± 13.6 4 | 23.3 ± 10.6 4 | 1.03 ± 0.1 | 1.58 ± 0.4 4 | 134 ± 16 4 | 28.8 ± 3.9 4,† | |
| Total CPR | 31.8 ± 4.4 *,5 | 2.2 ± 0.5 *,5 | 67.9 ± 14.8 *,5 | 20.6 ± 9.1 *,5 | 1.16 ± 0.1 *,5 | 2.18 ± 0.7 *,5 | 133 ± 15 *,5 | 30.0 ± 4.7 *,5 | |
| Recovery | 22.5 ± 3.9 * | 1.7 ± 0.4 * | 37.4 ± 10.1 * | 18.8 ± 8.9 * | 1.01 ± 0.1 * | 0.80 ± 0.2 *,† | 108 ± 14 * | 26.3 ± 2.9 *,† | |
| Variables | Duration (s) | Compressions Rate (n/min) | Ventilationef (%) | Compressionef (%) | |
|---|---|---|---|---|---|
| CPRbase | Cycle 3 | 72.2 ± 13.5 | 77.6 ± 11.9 | 32.6 ± 40.1 | 81.1 ± 34.7 |
| Cycle 6 | 60.8 ±13.4 | 92.6 ± 15.6 | 39.1 ± 39.9 | 78.9 ± 35.5 | |
| Cycle 9 | 56.9 ± 6.8 | 96.1 ± 11.6 | 38.4 ± 39.1 | 75.6 ± 33.8 | |
| Cycle 12 | 44.6 ± 13.1 | 97.4 ± 10.8 | 23.9 ± 34.2 | 41.1 ± 28.0 | |
| Total CPR | 240.2 ± 2.8 | 87.4 ± 14.8 | 33.5 ± 38.3 | 69.2 ± 28.0 | |
| CPRrun | Cycle 3 | 72.5 ± 8.9 | 76.5 ± 10.1 | 47.8 ± 42.0 * | 68.9 ± 36.0 * |
| Cycle 6 | 58.5 ± 7.9 | 92.5 ± 12.7 | 52.2 ± 42.6 * | 68.9 ± 36.0 * | |
| Cycle 9 | 58.8 ± 7.9 | 93.4 ± 11.8 * | 55.8 ± 42.2 * | 67.8 ± 36.6 * | |
| Cycle 12 | 43.8 ± 12.4 | 96.2 ± 9.0 | 42.0 ± 42.4 * | 47.8 ± 29.5 * | |
| Total CPR | 235.3 ± 28.2 | 86.9 ± 10.4 | 49.5 ± 42.3 * | 63.3 ± 29.5 * | |
| CPRswim | Cycle 3 | 69.9 ± 13.1 | 83.0 ± 13.2 *,† | 55.9 ± 40.7 *,† | 63.3 ± 37.5 *,† |
| Cycle 6 | 55.3 ± 9.0 *,† | 103.2 ± 15.6 *,† | 54.8 ± 41.8 * | 76.7 ± 32.9 † | |
| Cycle 9 | 56.5 ± 9.8 | 100.9 ± 15.8 *,† | 53.8 ± 41.9 * | 67.8 ± 36.6 * | |
| Cycle 12 | 42.2 ± 12.9 | 101.6 ± 15.6 *,† | 43.0 ± 39.6 * | 41.1 ± 39.8 † | |
| Total CPR | 240.7 ± 2.7 | 95.5 ± 15.8 *,† | 51.9 ± 41.0 * | 62.2 ± 28.3 * | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abraldes, J.A.; Fernandes, R.J.; Morán-Navarro, R. Previous Intensive Running or Swimming Negatively Affects CPR Effectiveness. Int. J. Environ. Res. Public Health 2021, 18, 9843. https://doi.org/10.3390/ijerph18189843
Abraldes JA, Fernandes RJ, Morán-Navarro R. Previous Intensive Running or Swimming Negatively Affects CPR Effectiveness. International Journal of Environmental Research and Public Health. 2021; 18(18):9843. https://doi.org/10.3390/ijerph18189843
Chicago/Turabian StyleAbraldes, J. Arturo, Ricardo J. Fernandes, and Ricardo Morán-Navarro. 2021. "Previous Intensive Running or Swimming Negatively Affects CPR Effectiveness" International Journal of Environmental Research and Public Health 18, no. 18: 9843. https://doi.org/10.3390/ijerph18189843
APA StyleAbraldes, J. A., Fernandes, R. J., & Morán-Navarro, R. (2021). Previous Intensive Running or Swimming Negatively Affects CPR Effectiveness. International Journal of Environmental Research and Public Health, 18(18), 9843. https://doi.org/10.3390/ijerph18189843








