Processing Cycle Efficiency to Monitor the Performance of an Intelligent Tube Preparation System for Phlebotomy Services
Abstract
1. Introduction
2. Materials and Methods
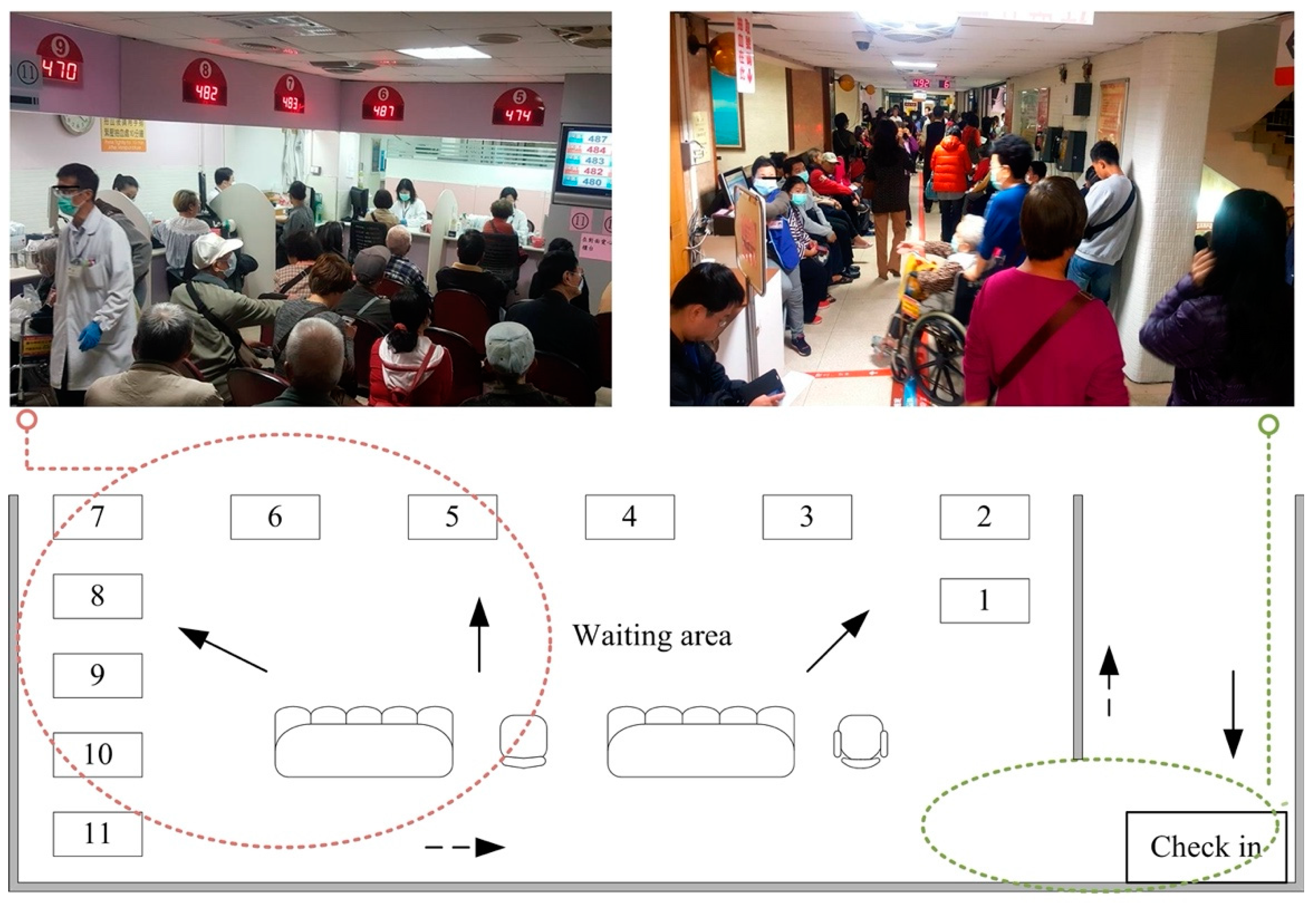
2.1. Blood Drawing Counters at Baseline
2.2. The Establishment of ITPS
2.3. Blood Drawing Counters after the Establishment of ITPS
2.4. Satisfaction Survey
2.5. Data Analysis
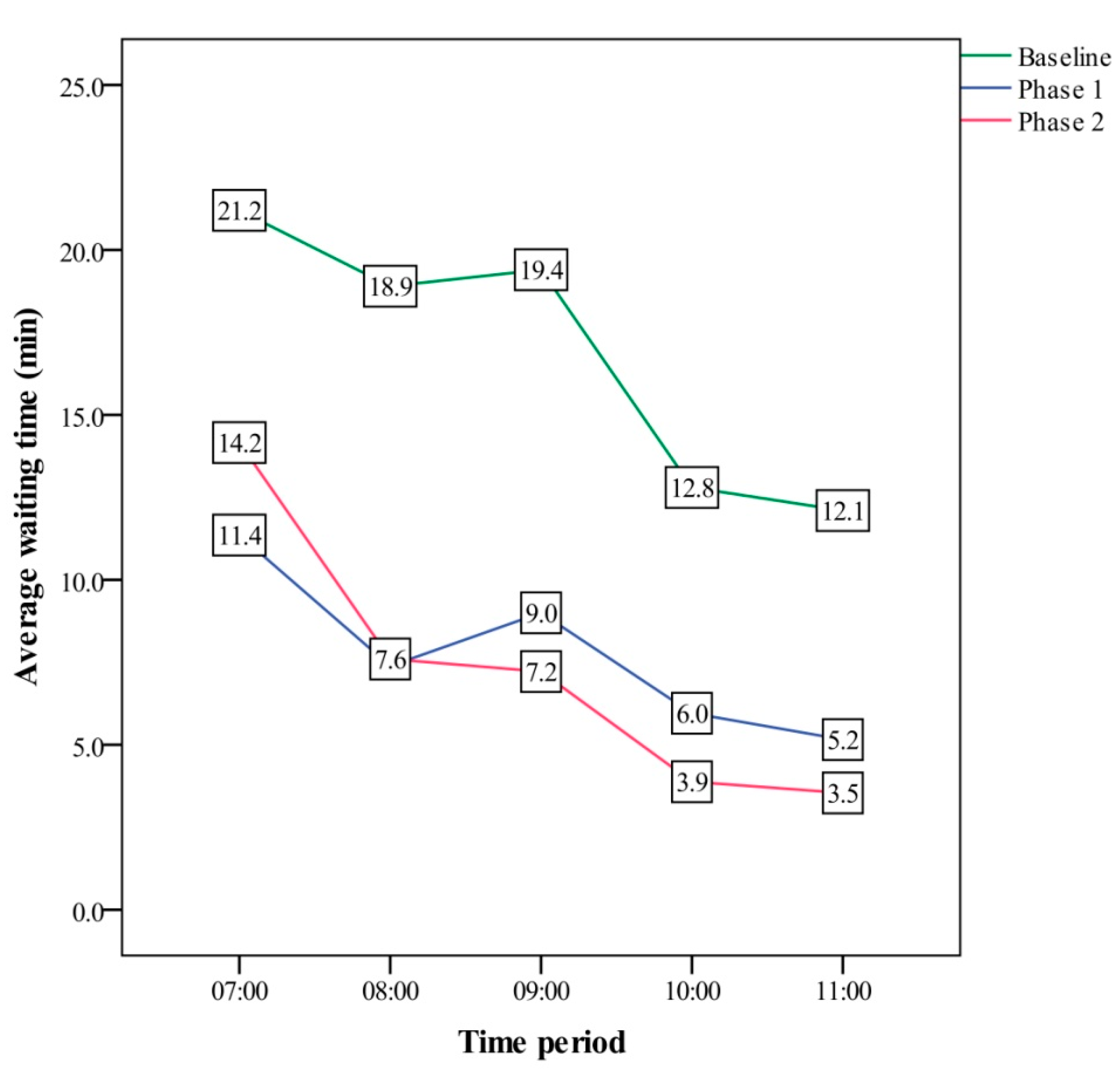
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jeon, B.R.; Seo, M.; Lee, Y.W.; Shin, H.B.; Lee, S.H.; Lee, Y.K. Improving the blood collection process using the active-phlebotomist phlebotomy system. Clin. Lab. 2011, 57, 21–27. [Google Scholar]
- Almomani, I.; AlSarheed, A. Enhancing outpatient clinics management software by reducing patients’ waiting time. J. Infect. Public Health 2016, 9, 734–743. [Google Scholar] [CrossRef] [PubMed]
- Le, V.; Wagar, E.A.; Phipps, R.A.; Del Guidice, R.E.; Le, H.; Middleton, L.P. Improving patient experience of wait times and courtesy through electronic sign-in and notification in the phlebotomy clinic. Arch. Pathol. Lab. Med. 2020, 144, 769–775. [Google Scholar] [CrossRef]
- Mijailovic, A.S.; Tanasijevic, M.J.; Goonan, E.M.; Le, R.D.; Baum, J.M.; Melanson, S.E.F. Optimizing outpatient phlebotomy staffing: Tools to assess staffing needs and monitor effectiveness. Arch. Pathol. Lab. Med. 2014, 138, 929–935. [Google Scholar] [CrossRef]
- Flory, N.; Lang, E.V. Distress in the radiology waiting room. Radiology 2011, 260, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Hammond, S.; Means, J.; O’Neill, N.; Khang, M.; Ladmirault, J.; Kroll, M. Reducing patient waiting times for phlebotomy. Am. J. Clin. Pathol. 2012, 138, A075. [Google Scholar] [CrossRef][Green Version]
- Woo, Y.S.; Kwon, Y.D.; Lee, M.; Cha, Y.J.; Kim, H.R. A real-time computer simulation program for reducing outpatients phlebotomy wait time. J. Clin. Lab. Anal. 2015, 29, 255–258. [Google Scholar] [CrossRef]
- Mengistu, B.; Ray, D.; Lockett, P.; Dorsey, V.; Phipps, R.A.; Subramanian, H.; Atkins, J.T.; El Osta, B.; Falchook, G.S.; Karp, D.D. Innovative strategies for decreasing blood collection wait times for patients in early-phase cancer clinical trials. J. Oncol. Pract. 2016, 12, e784–e791. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Dwivedi, T.; Sadhana, R.C. Analysis of patient’s satisfaction with phlebotomy services in NABH accredited neuropsychiatric hospital: An effective tool for improvement. J. Clin. Diagn. Res. 2017, 11, EC05–EC08. [Google Scholar] [CrossRef]
- Jackson, J.; Woeste, L.A. Using lean six sigma to reduce patient wait times. Lab. Med. 2008, 39, 134–136. [Google Scholar] [CrossRef]
- Kim, Y.K.; Song, K.E.; Lee, W.K. Reducing patient waiting time for the outpatient phlebotomy service using six sigma. Korean J. Lab. Med. 2009, 29, 171–177. [Google Scholar] [CrossRef]
- Osoba, M.Y.; Rao, A.K.; Agrawal, S.K.; Lalwani, A.K. Balance and gait in the elderly: A contemporary review. Laryngoscope Investig. Otolaryngol. 2019, 4, 143–153. [Google Scholar] [CrossRef]
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. Age-related differences in walking stability. Age Ageing 2003, 32, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Frost, K.L.; Bertocci, G.; Stillman, M.D.; Smalley, C.; Williams, S. Accessibility of outpatient healthcare providers for wheelchair users: Pilot study. J. Rehabil. Res. Dev. 2015, 52, 653–662. [Google Scholar] [CrossRef] [PubMed]
- Jamil, N.; Gholami, H.; Muhamad Zameri, M.S.; Streimikiene, D.; Sharif, S.; Zakuan, N. DMAIC-based approach to sustainable value stream mapping: Towards a sustainable manufacturing system. Econ. Res. Ekon. Istraz. 2020, 33, 331–360. [Google Scholar]
- Langstrand, J. An Introduction to Value Stream Mapping and Analysis. 2016. Available online: https://www.diva-portal.org/smash/get/diva2:945581/FULLTEXT01.pdf (accessed on 23 May 2020).
- Kobayashi Create Co., Ltd. Automatic Blood Collection Tube Labeler. 2021. Available online: https://www.tokyo-kosha.or.jp/TTC/product/rmepal0000021yl6-att/R2-038_Kobayashi.pdf (accessed on 23 May 2021).
- Gastwirth, J.L.; Gel, Y.R.; Miao, W. The impact of Levene’s test of equality of variances on satistical theory and practice. Stat. Sci. 2009, 24, 343–360. [Google Scholar] [CrossRef]
- Mishra, P.; Pandey, C.M.; Singh, U.; Gupta, A.; Sahu, C.; Keshri, A. Descriptive statistics and normality tests for statistical data. Ann. Card. Anaesth. 2019, 22, 67–72. [Google Scholar]
- Melanson, S.E.; Goonan, E.M.; Lobo, M.M.; Baum, J.M.; Paredes, J.D.; Santos, K.S.; Gustafson, M.L.; Tanasijevic, M.J. Applying Lean/Toyota production system principles to improve phlebotomy patient satisfaction and workflow. Am. J. Clin. Pathol. 2009, 132, 914–919. [Google Scholar] [CrossRef]
- Marin-Garcia, J.A.; Vidal-Carreras, P.I.; Garcia-Sabater, J.J. The role of value stream mapping in healthcare services: A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 951. [Google Scholar] [CrossRef]
- Koelling, C.P.; Eitel, D.; Mahapatra, S.; Messner, K.; Grove, L. Value Stream Mapping the Emergency Department. 2009. Available online: http://www.iienet.org/uploadedfiles/SHS/Resource_Library/Details/180.pdf (accessed on 23 January 2021).
- Saraswat, P.; Sain, M.K.; Kumar, D. A review on waste reduction through value stream mapping analysis. Int. J. Res. 2014, 1, 200–207. [Google Scholar]
- Bergmark, A.; Parker, M.G.; Thorslund, M. Priorities in care and services for elderly people: A path without guidelines? J. Med. Ethics 2000, 26, 312–318. [Google Scholar] [CrossRef]
- Ishijima, H.; Eliakimu, E.; Mshana, J.M. The “5S” approach to improve a working environment can reduce waiting time: Findings from hospitals in Northern Tanzania. TQM J. 2016, 28, 664–680. [Google Scholar] [CrossRef]
- de Jonge, N.; Herpers, R.; Roelofs, M.; van Dongen, E. Blood sampling after COVID-19—How to organize large scale phlebotomy services in the post SARS-CoV-2 era. Clin. Chem. Lab. Med. 2020, 58, e155–e157. [Google Scholar] [CrossRef] [PubMed]
- Baraniuk, C. COVID-19: People are gathering again, but can crowds be made safe? BMJ 2020, 371, m3511. [Google Scholar] [CrossRef] [PubMed]
- Tan, T.W.; Tan, H.L.; Chang, M.N.; Lin, W.S.; Chang, C.M. Effectiveness of epidemic preventive policies and hospital strategies in combating COVID-19 outbreak in Taiwan. Int. J. Environ. Res. Public Health 2021, 18, 3456. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Piot, P. The potential future of the COVID-19 pandemic: Will SARS-CoV-2 become a recurrent seasonal infection? JAMA 2021, 325, 1249–1250. [Google Scholar] [CrossRef]
- Orbatu, D.; Yıldırım, O.; Yaşar, E.; Sişman, A.R.; Sevinc, S. Predicting Patient Wait Times in the Phlebotomy Unit. Glob. J. Med. Res. 2020, 20, 1–5. [Google Scholar] [CrossRef]
- Yun, S.G.; Shin, J.W.; Park, E.S.; Bang, H.I.; Kang, J.G. Efficiency of an automated reception and turnaround time management system for the phlebotomy room. Ann. Lab. Med. 2016, 36, 49–54. [Google Scholar] [CrossRef] [PubMed][Green Version]


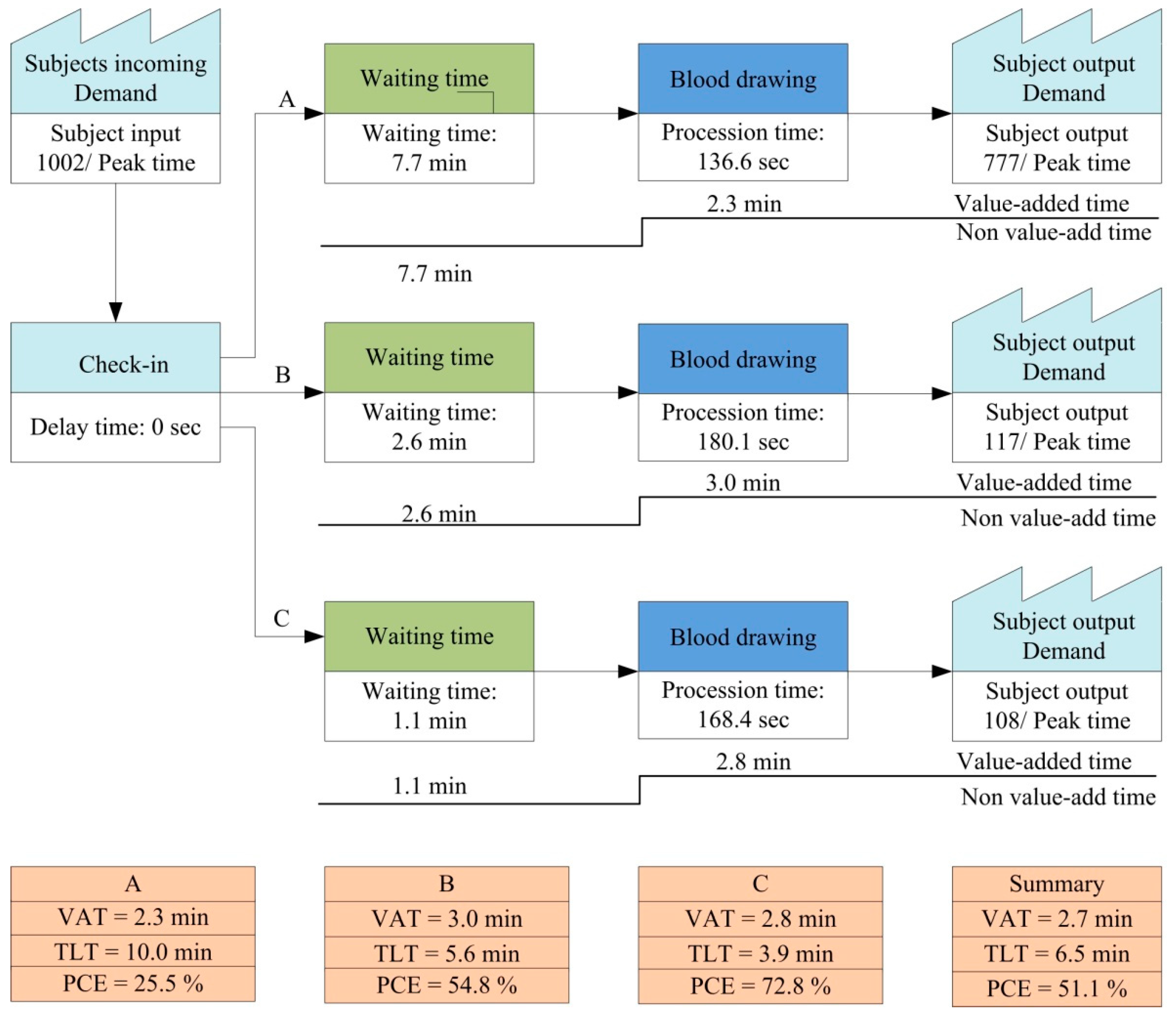
| (A) | |||||||||
| Characteristic | Baseline | After the Establishment of the ITPS | |||||||
| Phase 1 | Phase 2 | F | p-Value | ||||||
| Per Day | PT | Per Day | PT | Per Day | PT | ||||
| Total service number λ | 1027 | 654 (63.7%) | 1570 | 1002 (64.1%) | 1453 | 933 (64.2%) | - | 0.220 | |
| Service number per hour λ | 64 | 131 | 101 | 200 | 92 | 187 | - | 0.063 | |
| RSS λ | 13 | 14 | 16 | 18 | 14 | 17 | - | 0.253 | |
| Service time (s) κ α (p = 0.185); β (p = 0.801); γ (p = 0.070) | 167 ± 27.0 | 141.8 ± 9.4 | 146.0 ± 17.0 | 161.7 ± 22.7 | 147.8 ± 27.1 | 153.7 ± 24.1 | 3.866 | 0.023 * | |
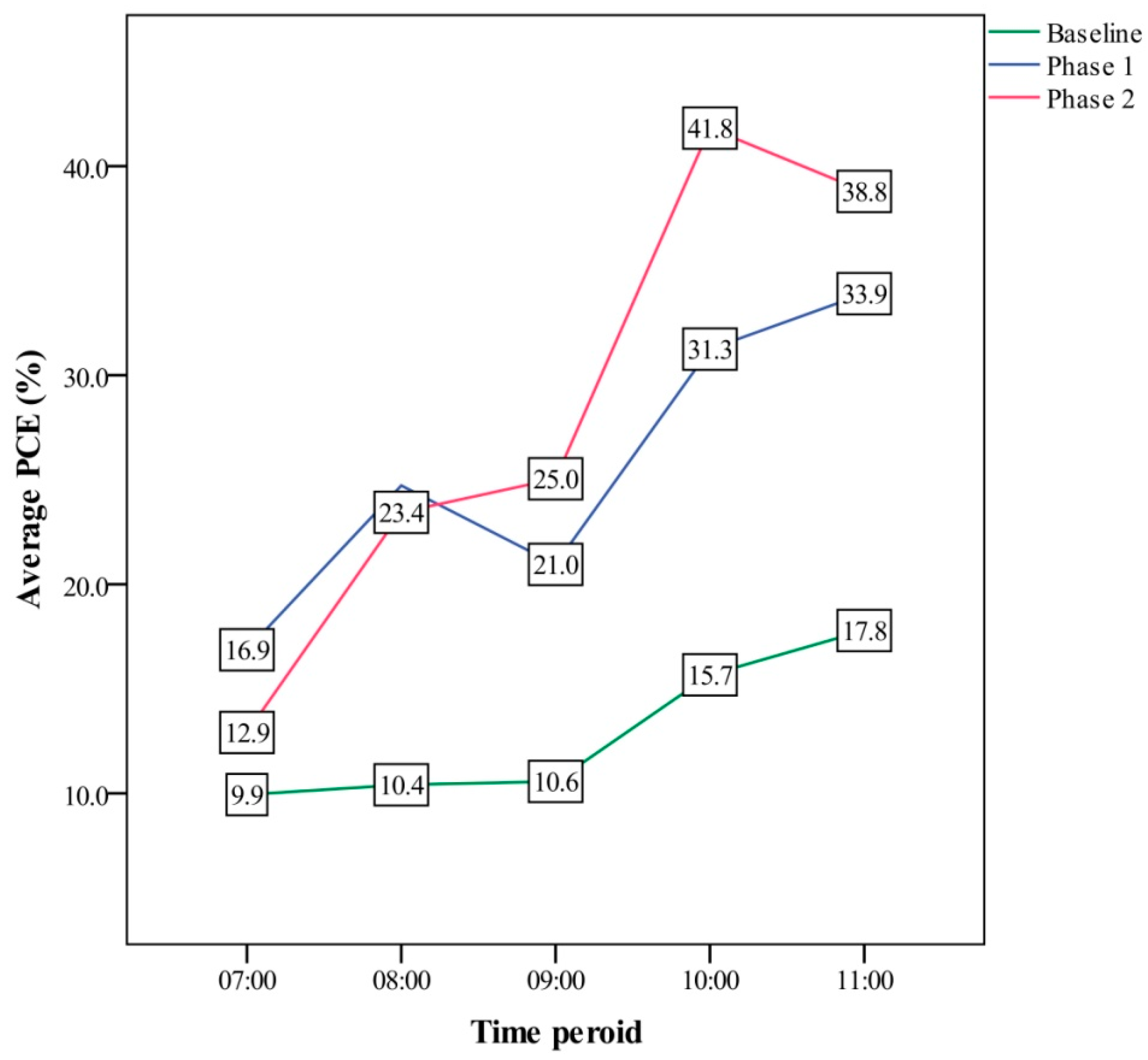
| Waiting time (min) κ α (p < 0.001 *); β (p < 0.001 *); γ (p = 1.000) | 11.1 ± 6.1 | 16.9 ± 4.2 | 8.1 ± 5.3 | 3.8 ± 3.5 | 8.7 ± 6.4 | 3.6 ± 3.9 | 30.865 | <0.001 * | |
| PCE (%) λ α (p < 0.001 *); β (p < 0.001 *); γ (p = 1.000) | 26.1 ± 19.4 | 12.9 ± 3.6 | 28.6 ± 13.4 | 51.1 ± 21.9 | 29.2 ± 15.1 | 53.0 ± 22.4 | - | 0.001 * | |
| (B) | |||||||||
| Characteristic | General Population | Wheelchair Users | The Elderly | ||||||
| Phase 1 | Phase 2 | p-Value | Phase 1 | Phase 2 | p-Value | Phase 1 | Phase 2 | p-Value | |
| Service number per hour | 155 | 141 | 0.504 ξ | 23 | 24 | 0.910 ξ | 22 | 22 | 0.314 ξ |
| Service time (s) | 136.6 ± 4.9 | 130.1 ± 8.0 | 0.001 *,Φ | 180.1 ± 19.7 | 170.2 ± 25.4 | 0.110 Φ | 168.4 ± 10.7 | 160.8 ± 13.2 | 0.017 *,Φ |
| Waiting time (min) | 7.7 ± 3.5 | 7.3 ± 4.5 | 0.635 Φ | 2.6 ± 0.9 | 2.5 ± 1.8 | 0.126 ξ | 1.1 ± 0.7 | 1.0 ± 0.7 | 0.109 ξ |
| PCE (%) | 25.5 ± 9.1 | 28.4 ± 13.4 | 0.328 Φ | 54.8 ± 9.0 | 56.3 ± 9.9 | 0.557 Φ | 72.8 ± 11.3 | 74.2 ± 12.4 | 0.239 ξ |
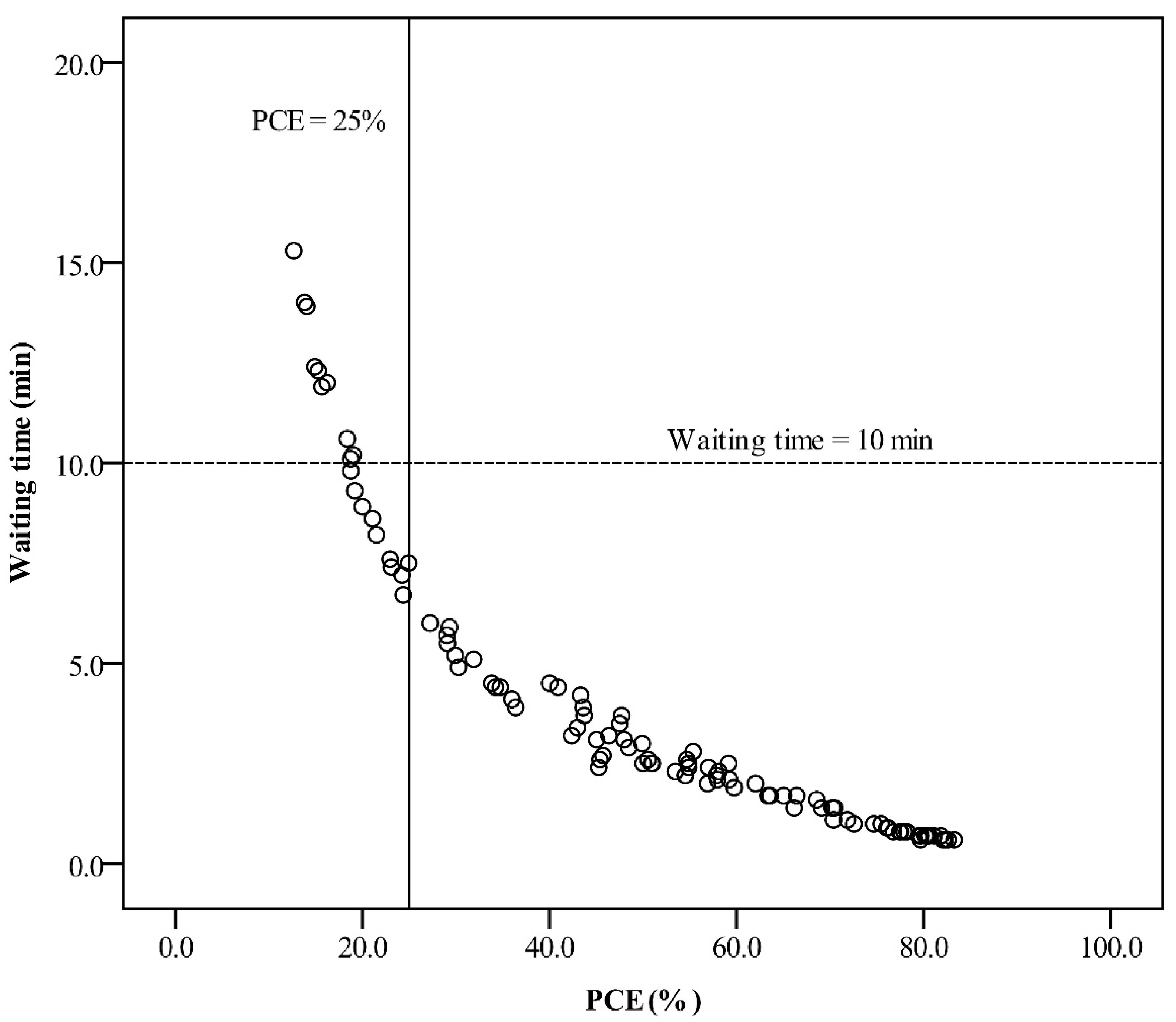
| PCE ≥ 25% | WT < 10 Min | PCE < 25% When WT < 10 Min | |
|---|---|---|---|
| Service number: general (per hour) | 40 (8, 161) | 53 (8, 178) | 162 (114, 178) |
| Service number: wheelchair (per hour) | 19 (8, 32) | 24 (8, 38) | 31 (10, 38) |
| Service number: aging (per hour) | 15 (8, 28) | 19 (8, 50) | 26 (16, 50) |
| Service time (s) | 167.7 (119.1, 217.3) | 164.3 (119.1, 217.3) | 135.9 (129.4, 149.5) |
| RSS | 14 (11, 16) | 15 (11, 21) | 18 (15, 21) |
| Waiting time (min) | 2.3 (0.6, 6.0) | 2.9 (0.6, 9.8) | 8.1 (6.7, 9.8) |
| PCE (%) | 58.6 (27.2, 83.3) | 54.8 (18.8, 83.3) | 22.0 (18.8, 24.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, M.-F.; Li, J.-Y.; Lin, Y.-H.; Huang, W.-C.; He, C.-C.; Wang, J.-M. Processing Cycle Efficiency to Monitor the Performance of an Intelligent Tube Preparation System for Phlebotomy Services. Int. J. Environ. Res. Public Health 2021, 18, 9386. https://doi.org/10.3390/ijerph18179386
Wu M-F, Li J-Y, Lin Y-H, Huang W-C, He C-C, Wang J-M. Processing Cycle Efficiency to Monitor the Performance of an Intelligent Tube Preparation System for Phlebotomy Services. International Journal of Environmental Research and Public Health. 2021; 18(17):9386. https://doi.org/10.3390/ijerph18179386
Chicago/Turabian StyleWu, Ming-Feng, Jen-Ying Li, Yu-Hsuan Lin, Wei-Chang Huang, Chi-Chih He, and Jiunn-Min Wang. 2021. "Processing Cycle Efficiency to Monitor the Performance of an Intelligent Tube Preparation System for Phlebotomy Services" International Journal of Environmental Research and Public Health 18, no. 17: 9386. https://doi.org/10.3390/ijerph18179386
APA StyleWu, M.-F., Li, J.-Y., Lin, Y.-H., Huang, W.-C., He, C.-C., & Wang, J.-M. (2021). Processing Cycle Efficiency to Monitor the Performance of an Intelligent Tube Preparation System for Phlebotomy Services. International Journal of Environmental Research and Public Health, 18(17), 9386. https://doi.org/10.3390/ijerph18179386






