Exploration of Preventable Hospitalizations for Colorectal Cancer with the National Cancer Control Program in Taiwan
Abstract
1. Introduction
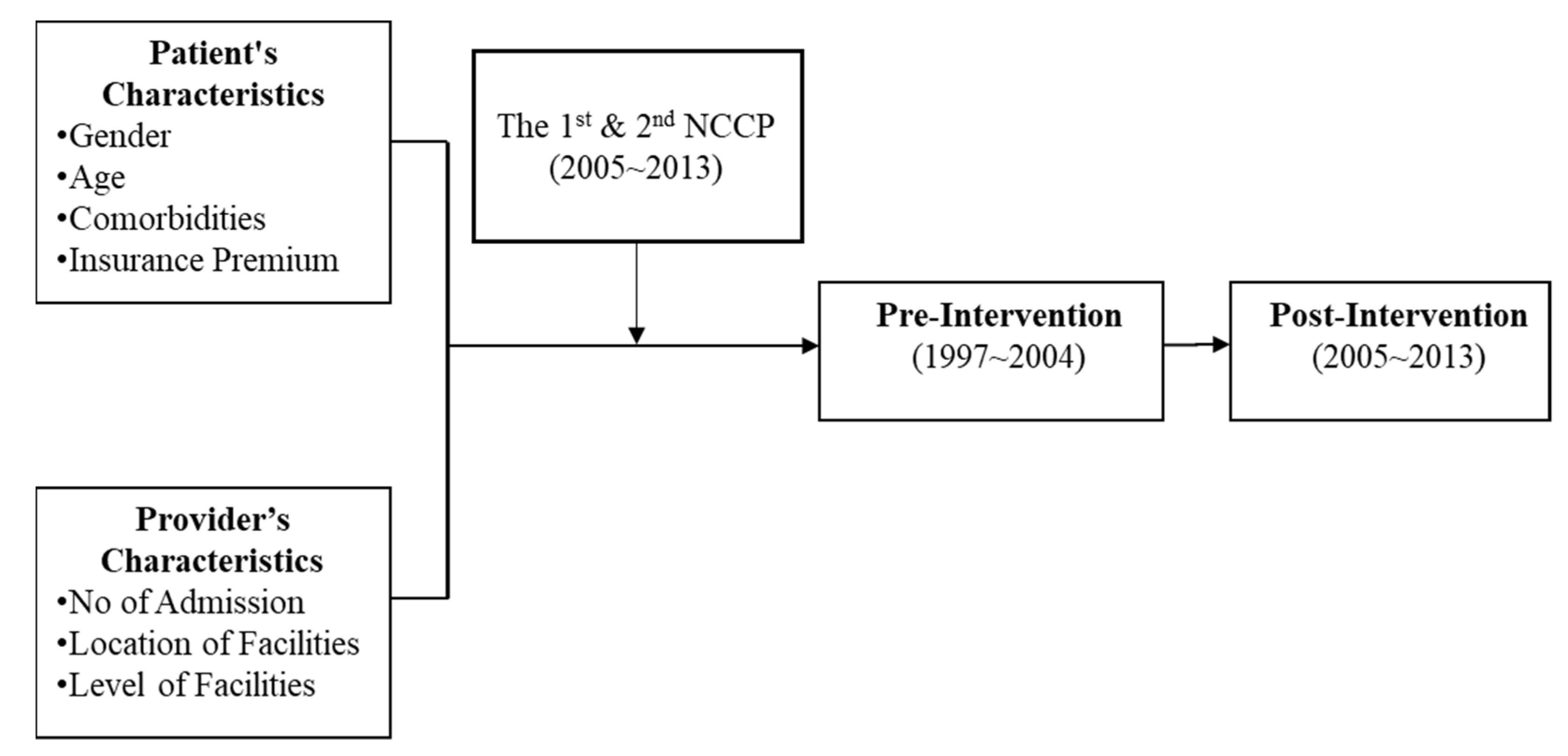
2. Materials and Methods
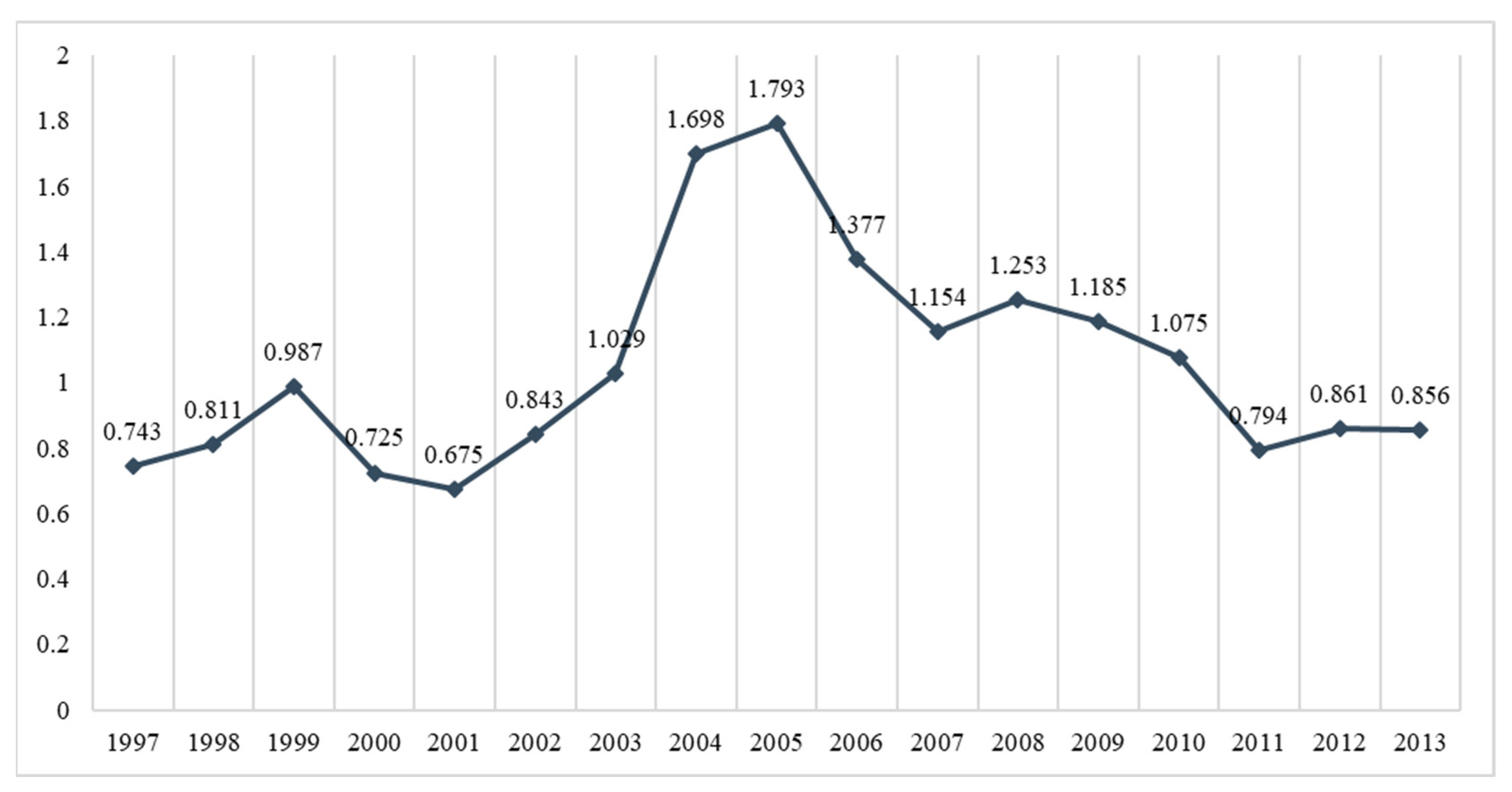
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Chiang, C.-J.; Wang, Y.-W.; Lee, W.-C. Taiwan’s nationwide cancer registry system of 40 years: Past, present, and future. J. Formos. Med. Assoc. 2019, 118, 856–858. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.S.; Yoon, M.; Song, S.H.; Suh, M.; Park, B.; Jung, K.W.; Jun, J.K. Effect of mammography screening on stage at breast cancer diagnosis: Results from the Korea National Cancer Screening Program. Sci. Rep. 2018, 8, 8882. [Google Scholar] [CrossRef] [PubMed]
- Bindman, A.B.; Grumbach, K.; Osmond, D.; Komaromy, M.; Vranizan, K.; Lurie, N.; Billings, J.; Stewart, A. Preventable hospitalizations and access to health care. JAMA 1995, 274, 305–311. [Google Scholar] [CrossRef]
- Wen, H.; Johnston, K.J.; Allen, L.; Waters, T.M. Medicaid expansion associated with reductions in preventable hospitalizations. Health Aff. 2019, 38, 1845–1849. [Google Scholar] [CrossRef] [PubMed]
- Muench, U.; Simon, M.; Guerbaai, R.-A.; De Pietro, C.; Zeller, A.; Kressig, R.W.; Zúñiga, F. Preventable hospitalizations from ambulatory care sensitive conditions in nursing homes: Evidence from Switzerland. Int. J. Public Health 2019, 64, 1273–1281. [Google Scholar] [CrossRef]
- Liang, Y.-W.; Chen, W.-Y.; Lin, Y.-H.; Lee, J.-L.; Chang, H.-F. A literature review of preventable hospitalizations: Implications for primary care in Taiwan. Taiwan Gong Gong Wei Sheng Za Zhi 2011, 30, 409. [Google Scholar]
- Billings, J.; Zeitel, L.; Lukomnik, J.; Carey, T.S.; Blank, A.E.; Newman, L. Impact of socioeconomic status on hospital use in New York City. Health Aff. 1993, 12, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.M.; Park, J.H.; Yoon, T.H.; Kim, Y. Hospitalizations for ambulatory care sensitive conditions as an indicator of access to primary care and excess of bed supply. BMC Health Serv. Res. 2019, 19, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.; Santos, J.V.; Souza, J.; Viana, J.; Costa Santos, C.; Lobo, M.; Freitas, A. Comparison and Impact of Four Different Methodologies for Identification of Ambulatory Care Sensitive Conditions. Int. J. Environ. Res. Public Health 2020, 17, 8121. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.-W.; Chang, H.-F.; Lin, Y.-H. Effects of health-information-based diabetes shared care program participation on preventable hospitalizations in Taiwan. BMC Health Serv. Res. 2019, 19, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.-W.; Chen, W.-Y.; Chang, H.-F. Effects of continuity of care on emergency department use and non-urgent emergency department visits among the elderly. Taiwan Gong Gong Wei Sheng Za Zhi 2016, 35, 152. [Google Scholar]
- Pappas, G.; Hadden, W.C.; Kozak, L.J.; Fisher, G.F. Potentially avoidable hospitalizations: Inequalities in rates between US socioeconomic groups. Am. J. Public Health 1997, 87, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Rizza, P.; Bianco, A.; Pavia, M.; Angelillo, I.F. Preventable hospitalization and access to primary health care in an area of Southern Italy. BMC Health Serv. Res. 2007, 7, 134. [Google Scholar] [CrossRef] [PubMed]
- Ramalho, A.; Lobo, M.; Duarte, L.; Souza, J.; Santos, P.; Freitas, A. Landscapes on Prevention Quality Indicators: A Spatial Analysis of Diabetes Preventable Hospitalizations in Portugal (2016–2017). Int. J. Environ. Res. Public Health 2020, 17, 8387. [Google Scholar] [CrossRef]
- Dimitrovová, K.; Costa, C.; Santana, P.; Perelman, J. Evolution and financial cost of socioeconomic inequalities in ambulatory care sensitive conditions: An ecological study for Portugal, 2000–2014. Int. J. Equity Health 2017, 16, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Millman, M. Access to Health Care in America; National Academies Press (US): Washington, DC, USA, 1993. [Google Scholar]
- Erickson, S.M.; Outland, B.; Joy, S.; Rockwern, B.; Serchen, J.; Mire, R.D.; Goldman, J.M. Envisioning a better US health care system for all: Health care delivery and payment system reforms. Ann. Intern. Med. 2020, 172, S33–S49. [Google Scholar] [CrossRef] [PubMed]
- Bindman, A.B.; Chattopadhyay, A.; Osmond, D.H.; Huen, W.; Bacchetti, P. The impact of Medicaid managed care on hospitalizations for ambulatory care sensitive conditions. Health Serv. Res. 2005, 40, 19–38. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, S.; Zielinski, T. The meaning of ambulatory care sensitive admissions: Urban and rural perspectives. J. Rural Health 1997, 13, 276. [Google Scholar] [CrossRef]
- Daly, M.R.; Mellor, J.M.; Millones, M. Do avoidable hospitalization rates among older adults differ by geographic access to primary care physicians? Health Serv. Res. 2018, 53, 3245–3264. [Google Scholar] [CrossRef] [PubMed]
- Zeng, F.; O’Leary, J.F.; Sloss, E.M.; Lopez, M.S.; Dhanani, N.; Melnick, G. The effect of medicare health maintenance organizations on hospitalization rates for ambulatory care-sensitive conditions. Med. Care 2006, 44, 900–907. [Google Scholar] [CrossRef] [PubMed]
- Starfield, B. Primary health care and hospitalizations in ambulatory care sensitive conditions in Catalonia. Rev. Clin. Esp. 2001, 201, 501–507. [Google Scholar]
- Vuik, S.I.; Fontana, G.; Mayer, E.; Darzi, A. Do hospitalisations for ambulatory care sensitive conditions reflect low access to primary care? An observational cohort study of primary care usage prior to hospitalisation. BMJ Open 2017, 7, e015704. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.L.; Starfield, B.; Anderson, G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch. Intern. Med. 2002, 162, 2269–2276. [Google Scholar] [CrossRef] [PubMed]
- Edwards, S.T.; Peterson, K.; Chan, B.; Anderson, J.; Helfand, M. Effectiveness of intensive primary care interventions: A systematic review. J. Gen. Intern. Med. 2017, 32, 1377–1386. [Google Scholar] [CrossRef]
- Ansari, Z.; Laditka, J.N.; Laditka, S.B. Access to health care and hospitalization for ambulatory care sensitive conditions. Med. Care Res. Rev. 2006, 63, 719–741. [Google Scholar] [CrossRef] [PubMed]
- Cloutier-Fisher, D.; Penning, M.J.; Zheng, C.; Druyts, E.-B.F. The devil is in the details: Trends in avoidable hospitalization rates by geography in British Columbia, 1990–2000. BMC Health Serv. Res. 2006, 6, 104. [Google Scholar] [CrossRef] [PubMed]
- Muenchberger, H.; Kendall, E. Predictors of preventable hospitalization in chronic disease: Priorities for change. J. Public Health Policy 2010, 31, 150–163. [Google Scholar] [CrossRef] [PubMed]
- Laditka, J.N.; Laditka, S.B.; Probst, J.C. Health care access in rural areas: Evidence that hospitalization for ambulatory care-sensitive conditions in the United States may increase with the level of rurality. Health Place 2009, 15, 761–770. [Google Scholar] [CrossRef]
- Huang, Y.-C.; Chen, Y.-H. Cancer Incidence Characteristic Evolution Based on the National Cancer Registry in Taiwan. J. Oncol. 2020, 2020, 1408793. [Google Scholar] [CrossRef]
- Wang, Y.-W.; Chen, H.-H.; Wu, M.-S.; Chiu, H.-M. Current status and future challenge of population-based organized colorectal cancer screening: Lesson from the first decade of Taiwanese program. J. Formos. Med. Assoc. 2018, 117, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-S.; Hsu, C.-C.; Weng, S.-F.; Lin, H.-J.; Wang, J.-J.; Su, S.-B.; Huang, C.-C.; Guo, H.-R. Cancer incidence in physicians: A Taiwan national population-based cohort study. Medicine 2015, 94, e2079. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.W.; Lee, S.; Ahn, S. Is Colorectal Cancer Screening Associated with Stages of Weight Control Among Korean Americans Aged 50–75 Years Old?: Implications for Weight Control Practice. J. Racial Ethn. Health Disparities 2020, 8, 1026–1034. [Google Scholar] [CrossRef] [PubMed]
- Davies, S.; McDonald, K.M.; Schmidt, E.; Schultz, E.; Geppert, J.; Romano, P.S. Expanding the uses of AHRQ’s prevention quality indicators: Validity from the clinician perspective. Med. Care 2011, 49, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Manzoli, L.; Flacco, M.E.; De Vito, C.; Arca, S.; Carle, F.; Capasso, L.; Marzuillo, C.; Muraglia, A.; Samani, F.; Villari, P. AHRQ prevention quality indicators to assess the quality of primary care of local providers: A pilot study from Italy. Eur. J. Public Health 2014, 24, 745–750. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Variables | Pre—(1997–2004) N = 3990 | Post—(2005–2013) N = 4061 | Total—(1997–2013) N = 8051 | |||
|---|---|---|---|---|---|---|
| N (%) | p | N (%) | p | N (%) | p | |
| Patient’s Characteristics | ||||||
| Gender | <0.0001 | <0.0001 | <0.0001 | |||
| Male | 2149 (53.9%) | 2255 (55.5%) | 4404 (54.7%) | |||
| Female | 1841 (46.1%) | 1806 (44.5%) | 3647 (45.3%) | |||
| Age | 0.442 | 0.068 | 0.746 | |||
| MEAN ± SD | 61.43 ± 9.53 | 62.09 ± 9.88 | 61.76 ± 9.71 | |||
| CCI | <0.0001 | <0.0001 | <0.0001 | |||
| MEAN ± SD | 3.68 ± 1.81 | 3.37 ± 1.88 | 3.52 ± 1.86 | |||
| None | 496 (12.4%) | 593 (14.6%) | 1089 (13.5%) | |||
| Low (<5) | 500 (12.5%) | 695 (17.1%) | 1195 (14.8%) | |||
| Median | 737 (18.5%) | 863 (21.3%) | 1600 (19.9%) | |||
| High (>8) | 2257 (56.6%) | 1910 (47.0%) | 4167 (51.8%) | |||
| Premium/Month | <0.0001 | <0.0001 | <0.0001 | |||
| Dependency | 1369 (34.3%) | 1328 (32.7%) | 2697 (33.5%) | |||
| <620 USD | 867 (21.7%) | 783 (19.3%) | 1650 (20.5%) | |||
| 620–760 USD | 1084 (27.2%) | 1065 (26.2%) | 2149 (26.7%) | |||
| 761–1210 USD | 252 (6.3%) | 312 (7.7%) | 564 (7.0%) | |||
| 1211–1526 USD | 209 (5.2%) | 283 (7.0%) | 492 (6.1%) | |||
| >1526 USD | 209 (5.2%) | 290 (7.1%) | 499 (6.2%) | |||
| Provider’s Characteristics | ||||||
| No of PH (Person No/Year) | 0.939 ± 2.449 | 1.151 ± 5.815 | 1.051 ± 4.231 | |||
| Location | <0.0001 | <0.0001 | <0.0001 | |||
| North | 2073 (52.0%) | 2131 (52.5%) | 4204 (52.2%) | |||
| West | 750 (18.8%) | 713 (17.6%) | 1463 (18.2%) | |||
| South | 1058 (26.5%) | 1140 (28.1%) | 2198 (27.3%) | |||
| East | 81 (2.0%) | 65 (1.6%) | 146 (1.8%) | |||
| Off-Island | 28 (0.7%) | 12 (0.3%) | 40 (0.5%) | |||
| Level | <0.0001 | 0.061 | <0.0001 | |||
| Medical Center | 2066 (51.8%) | 2766 (68.1%) | 4832 (60.0%) | |||
| Regional Hospital | 647 (16.2%) | 429 (10.6%) | 1076 (13.4%) | |||
| District Hospital | 596 (14.9%) | 489 (12.0%) | 1085 (13.5%) | |||
| Clinics | 681 (17.1%) | 377 (9.3%) | 1058 (13.1%) | |||
| Variables | No of PH (Person No/Person Year) | ||||
|---|---|---|---|---|---|
| Total (1997–2013) | |||||
| RR | 95% CI | p | |||
| Lower | Upper | ||||
| Pre vs. Post | Pre (Baseline) | - | - | - | - |
| Post | 0.739 | 0.722 | 0.757 | <0.0001 | |
| Patient’s Characteristics | |||||
| Gender | Female (Baseline) Male | - | - | - | - |
| 1.146 | 1.119 | 1.173 | <0.0001 | ||
| Age | Every 10 years old | 1.005 | 0.988 | 1.012 | 0.977 |
| Comorbidities (CCI) | Every 1 score | 2.152 | 2.116 | 2.188 | <0.0001 |
| Insurance Premium | <USD 620 (Baseline) | - | - | - | - |
| Dependency | 0.945 | 0.918 | 0.973 | 0.001 | |
| USD 620–760 | 0.868 | 0.841 | 0.897 | <0.0001 | |
| USD 761–1210 | 0.765 | 0.720 | 0.813 | <0.0001 | |
| USD 1211–1526 | 0.721 | 0.672 | 0.773 | <0.0001 | |
| >USD 1526 | 0.725 | 0.673 | 0.780 | <0.0001 | |
| Provider’s Characteristics | |||||
| Location | North (Baseline) | - | - | - | - |
| West | 1.182 | 1.147 | 1.219 | <0.0001 | |
| South | 1.122 | 1.092 | 1.152 | <0.0001 | |
| East | 1.196 | 1.104 | 1.296 | <0.0001 | |
| Off-Island | 1.150 | 1.061 | 0.914 | 0.436 | |
| Level | Med Center (Baseline) | - | - | - | - |
| Reginal Hospital | 1.057 | 1.016 | 1.099 | 0.006 | |
| District Hospital | 0.985 | 0.946 | 1.026 | 0.473 | |
| Clinics | 0.834 | 0.807 | 0.862 | <0.0001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, Y.-H.; Chung, Y.-C.; Lee, P.-Y.; Kao, H.-Y. Exploration of Preventable Hospitalizations for Colorectal Cancer with the National Cancer Control Program in Taiwan. Int. J. Environ. Res. Public Health 2021, 18, 9327. https://doi.org/10.3390/ijerph18179327
Hung Y-H, Chung Y-C, Lee P-Y, Kao H-Y. Exploration of Preventable Hospitalizations for Colorectal Cancer with the National Cancer Control Program in Taiwan. International Journal of Environmental Research and Public Health. 2021; 18(17):9327. https://doi.org/10.3390/ijerph18179327
Chicago/Turabian StyleHung, Yu-Han, Yu-Chieh Chung, Pi-Yueh Lee, and Hao-Yun Kao. 2021. "Exploration of Preventable Hospitalizations for Colorectal Cancer with the National Cancer Control Program in Taiwan" International Journal of Environmental Research and Public Health 18, no. 17: 9327. https://doi.org/10.3390/ijerph18179327
APA StyleHung, Y.-H., Chung, Y.-C., Lee, P.-Y., & Kao, H.-Y. (2021). Exploration of Preventable Hospitalizations for Colorectal Cancer with the National Cancer Control Program in Taiwan. International Journal of Environmental Research and Public Health, 18(17), 9327. https://doi.org/10.3390/ijerph18179327






