Clinical Risk Factors for Uterine Cervical Elongation among Women with Pelvic Organ Prolapse
Abstract
:1. Introduction
2. Material and Methods
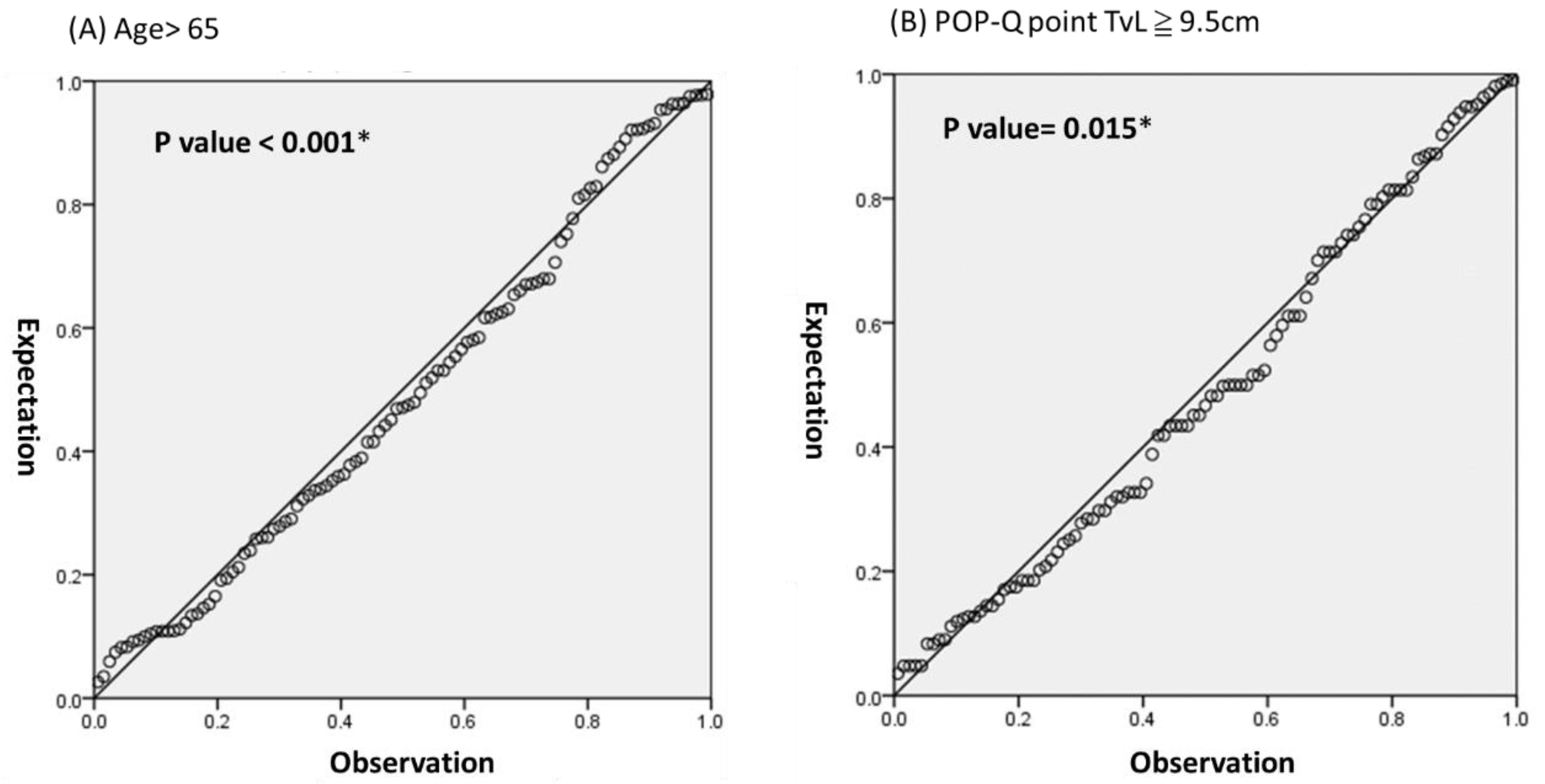
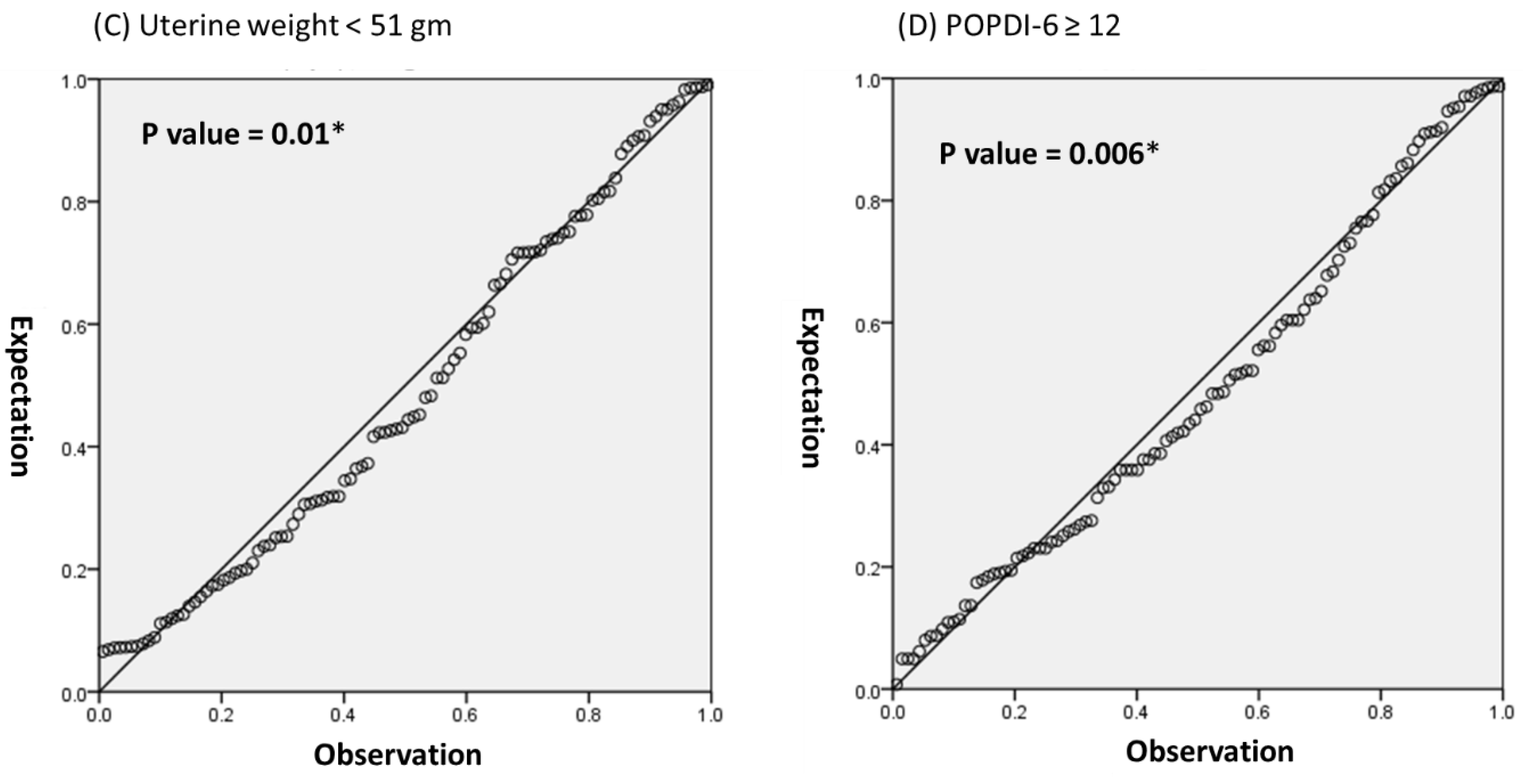
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Olsen, A.L.; Smith, V.J.; Bergstrom, J.O.; Colling, J.C.; Clark, A.L. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet. Gynecol. 1997, 89, 501–506. [Google Scholar] [CrossRef]
- Wu, M.-P.; Long, C.-Y.; Huang, K.-H.; Chu, C.-C.; Liang, C.-C.; Tang, C.-H. Changing trends of surgical approaches for uterine prolapse: An 11-year population-based nationwide descriptive study. Int. Urogynecol. J. 2012, 23, 865–872. [Google Scholar] [CrossRef]
- Veit-Rubin, N.; Lange, S.; Eperon, I.; Dubuisson, J.-B.; Dubuisson, J. Uterus-preserving laparoscopic lateral suspension with mesh for pelvic organ prolapse: A patient-centred outcome report and video of a continuous series of 245 patients. Int. Urogynecol. J. 2015, 27, 491–493. [Google Scholar] [CrossRef]
- Long, C.-Y.; Wang, C.-L.; Lin, K.-L.; Ker, C.-R.; Loo, Z.; Liu, Y.; Wu, P.-C. Laparoscopic Long Mesh Surgery with Augmented Round Ligaments: A Novel Uterine Preservation Procedure for Apical Pelvic Organ Prolapse. Sci. Rep. 2020, 10, 6615. [Google Scholar] [CrossRef] [Green Version]
- Meriwether, K.V.; Antosh, D.D.; Olivera, C.K.; Kim-Fine, S.; Balk, E.M.; Murphy, M.; Grimes, C.L.; Sleemi, A.; Singh, R.; Dieter, A.A.; et al. Uterine preservation vs. hysterectomy in pelvic organ prolapse surgery: A systematic review with meta-analysis and clinical practice guidelines. Am. J. Obstet. Gynecol. 2018, 219, 129–146.e2. [Google Scholar] [CrossRef] [PubMed]
- Ker, C.-R.; Lin, K.-L.; Loo, Z.-X.; Juan, Y.-S.; Long, C.-Y. Comparison of UpholdTM Vaginal Mesh Procedure with Hysterectomy or Uterine Preservation for the Treatment of Pelvic Organ Prolapse. Sci. Rep. 2018, 8, 9438. [Google Scholar] [CrossRef]
- Long, C.-Y.; Lo, T.-S.; Wang, C.-L.; Wu, C.-H.; Liu, C.-M.; Su, J.-H. Risk factors of surgical failure following transvaginal mesh repair for the treatment of pelvic organ prolapse. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012, 161, 224–227. [Google Scholar] [CrossRef]
- Geoffrion, R.; Louie, K.; Hyakutake, M.T.; Koenig, N.A.; Lee, T.; Filipenko, J.D. Study of Prolapse-Induced Cervical Elongation. J. Obstet. Gynaecol. Can. 2016, 38, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Hyakutake, M.T.; Cundiff, G.W.; Geoffrion, R. Cervical elongation following sacrospinous hysteropexy: A case series. Int. Urogynecol. J. 2013, 25, 851–854. [Google Scholar] [CrossRef]
- Vierhout, M.E.; Fütterer, J.J. Extreme cervical elongation after sacrohysteropexy. Int. Urogynecol. J. 2012, 24, 1579–1580. [Google Scholar] [CrossRef] [PubMed]
- Bump, R.C.; Mattiasson, A.; Bo, K.; Brubaker, L.P.; DeLancey, J.O.; Klarskov, P.; Shull, B.L.; Smith, A.R.B. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am. J. Obstet. Gynecol. 1996, 175, 10–17. [Google Scholar] [CrossRef]
- Berger, M.B.; Ramanah, R.; Guire, K.E.; DeLancey, J.O.L. Is cervical elongation associated with pelvic organ prolapse? Int. Urogynecol. J. 2012, 23, 1095–1103. [Google Scholar] [CrossRef] [Green Version]
- Finamore, P.S.; Goldstein, H.B.; Vakili, B. Comparison of Estimated Cervical Length from the Pelvic Organ Prolapse Quantification Exam and Actual Cervical Length at Hysterectomy. J. Pelvic Med. Surg. 2009, 15, 17–19. [Google Scholar] [CrossRef]
- Ibeanu, O.A.; Chesson, R.R.; Sandquist, D.; Perez, J.; Santiago, K.; Nolan, T.E. Hypertrophic cervical elongation: Clinical and histological correlations. Int. Urogynecol. J. 2010, 21, 995–1000. [Google Scholar] [CrossRef] [PubMed]
- Nosti, P.A.; Gutman, R.E.; Iglesia, C.B.; Park, A.J.; Tefera, E.; Sokol, A.I. Defining Cervical Elongation: A Prospective Observational Study. J. Obstet. Gynaecol. Can. 2017, 39, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Mothes, A.R.; Mothes, H.; Fröber, R.; Radosa, M.P.; Runnebaum, I.B. Systematic classification of uterine cervical elongation in patients with pelvic organ prolapse. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 200, 40–44. [Google Scholar] [CrossRef]
- Dancz, C.E.; Werth, L.; Sun, V.; Lee, S.; Walker, D.; Özel, B. Comparison of the POP-Q examination, transvaginal ultrasound, and direct anatomic measurement of cervical length. Int. Urogynecol. J. 2013, 25, 457–464. [Google Scholar] [CrossRef]
- Swift, S.; Woodman, P.; O’Boyle, A.; Kahn, M.; Valley, M.; Bland, D.; Wang, W.; Schaffer, J. Pelvic Organ Support Study (POSST): The distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am. J. Obstet. Gynecol. 2005, 192, 795–806. [Google Scholar] [CrossRef]
- Merz, P.E.; Miric-Tesanic, D.; Bahlmann, F.; Weber, G.; Wellek, S. Sonographic size of uterus and ovaries in pre- and postmenopausal women. Ultrasound Obstet. Gynecol. 1996, 7, 38–42. [Google Scholar] [CrossRef]
- Kung, F.T.; Chang, S.Y. The relationship between ultrasonic volume and actual weight of pathologic uterus. Gynecol. Obstet. Investig. 1996, 42. [Google Scholar] [CrossRef]
- Hsiao, S.-M.; Chang, T.-C.; Chen, C.-H.; Li, Y.-I.; Shun, C.-T.; Lin, H.-H. Risk factors for coexistence of cervical elongation in uterine prolapse. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 229, 94–97. [Google Scholar] [CrossRef]
- Barber, M.D.; Kuchibhatla, M.N.; Pieper, C.F.; Bump, R.C. Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am. J. Obstet. Gynecol. 2001, 185, 1388–1395. [Google Scholar] [CrossRef] [PubMed]
- DeLancey, J.O. What’s new in the functional anatomy of pelvic organ prolapse? Curr. Opin. Obstet. Gynecol. 2016, 28, 420–429. [Google Scholar] [CrossRef] [Green Version]
- Girgis, M.; Shek, K.L.; Dietz, H.P. Total vaginal length: Does it matter for assessing uterine prolapse? Int. Urogynecol. J. 2018, 30, 1279–1282. [Google Scholar] [CrossRef] [PubMed]
- Groutz, A.; Blaivas, J.G.; Chaikin, D.C. Bladder outlet obstruction in women: Definition and characteristics. Neurourol. Urodyn. 2000, 19, 213–220. [Google Scholar] [CrossRef]
- Romanzi, L.J.; Chaikin, D.C.; Blaivas, J.G. The effect of genital prolapse on voiding. J. Urol. 1999, 161, 581–586. [Google Scholar] [CrossRef]
- Hove, M.C.P.S.-T.; Pool-Goudzwaard, A.; Eijkemans, M.J.C.; Steegers-Theunissen, R.P.M.; Burger, C.W.; Vierhout, M.E. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int. Urogynecol. J. 2009, 20, 1037–1045. [Google Scholar] [CrossRef] [Green Version]
- Geoffrion, R.; Hyakutake, M.T.; Koenig, N.A.; Lee, T.; Cundiff, G.W. Bilateral Sacrospinous Vault Fixation With Tailored Synthetic Mesh Arms: Clinical Outcomes at One Year. J. Obstet. Gynaecol. Can. 2015, 37, 129–137. [Google Scholar] [CrossRef] [Green Version]

| Mean age (years) | 66.4 ± 8.7 |
| Mean parity | 3.3 ± 1.3 |
| Mean BMI (kg/m2) | 24.2 ± 3.2 |
| Menopause | 133 (100) |
| Current hormone therapy | 23 (17.3) |
| Current smokers | 1 (0.8) |
| Diabetes mellitus | 24 (18.1) |
| Hypertension | 55 (41.4) |
| History of POP and/or SUI Surgery | 6 (4.5) |
| Concomitant mid-urethral sling suegry | 29 (21.8) |
| Cervical Elongation (n = 43) | Normal Cervix (n = 90) | OR (95% CI) | p Value | ||
|---|---|---|---|---|---|
| Age | ≤65 | 14 (32.6) | 52 (57.8) | ||
| >65 | 29 (67.4) | 38 (42.2) | 3.88 (1.13–13.29) | 0.007 ** | |
| Parity | <3 | 10 (23.3) | 25 (27.8) | ||
| ≥3 | 33 (76.7) | 65 (72.2) | 0.65 (0.13–3.19) | 0.58 | |
| BMI healthy | <24 | 24 (55.8) | 51 (56.7) | ||
| Over weight | ≥24 | 19 (44.2) | 39 (43.3) | 0.85 (0.26–2.82) | 0.93 |
| Past history | H/T | 18 (41.9) | 37 (41.1) | 0.85 (0.26–2.82) | 0.94 |
| HT | 6 (14.0) | 17 (18.9) | 0.70 (0.36–2.70) | 0.48 | |
| DM | 6 (14.0) | 18 (20.0) | 0.97 (0.24–3.88) | 0.4 | |
| Previous POP or SUI surgery | 0 | 6 (6.7) | 0.18 * | ||
| Prolapse stage | Ⅱ | 4 (9.3) | 7 (7.8) | ||
| Ⅲ–Ⅳ | 39 (90.7) | 83 (92.2) | 1.11 (0.13–9.63) | 0.75 * | |
| POP-Q point | Ba ≥ 3 | 27 (62.8) | 45 (50.0) | 1.69 (0.22–2.96) | 0.17 |
| C ≥ 3 | 21 (48.8) | 37 (41.1) | 2.41(0.32–8.86) | 0.4 | |
| TvL ≥ 9.5 | 28 (65.1) | 41 (45.6) | 2.23(1.12–11.2) | 0.035 ** | |
| Involved compartment | Anterior wall | 37 (86.1) | 76 (84.4) | 1.14(0.23–3.12) | 0.81 |
| Uterine prolapse | 41 (95.3) | 80 (88.9) | 0.69 (0.21–2.29) | 0.34 | |
| Posterior wall | 8 (18.6) | 16 (17.8) | 0.80 (0.09–6.86) | 0.91 | |
| Uterine weight | <51 g | 31 (72.1) | 47 (52.2) | 2.83(1.13–12.2) | 0.03 ** |
| Preop symptoms | Frequency | 23 (53.5) | 45 (50.0) | 0.93 (0.27–3.12) | 0.71 |
| SUI | 12 (27.9) | 37 (41.1) | 0.44 (0.11–1.74) | 0.14 | |
| UI | 18 (41.9) | 44 (48.9) | 0.78 (0.23–2.61) | 0.45 | |
| Incomplete emptying | 38 (88.4) | 70 (77.8) | 2.31 (0.28–19.10) | 0.14 | |
| Hesitancy | 36 (83.7) | 63 (70.0) | 4.40 (0.54–35.70) | 0.09 | |
| Questionnaires | OABSS ≥ 10 | 6 (14.0) | 15 (16.7) | 2.77 (0.74–10.36) | 0.69 |
| UDI-6 ≥ 6 | 21 (48.8) | 36 (40.0) | 1.23 (0.37–4.07) | 0.34 | |
| POPDI-6 ≥ 12 | 13 (30.2) | 13 (14.4) | 4.13 (1.16–14.72) | 0.032 ** | |
| Cervical Elongation (n = 43) | Normal Cervix (n = 90) | OR (95% CI) | p Value * | ||
|---|---|---|---|---|---|
| DO | 10 (23.3) | 18 (20.0) | 1.21 (0.32–3.88) | 0.67 | |
| Q max (mL/s) | <15 | 33 (76.1) | 67 (74.4) | 1.23 (0.37–4.07) | 0.77 |
| ≧15 | 10 (23.3) | 23 (25.6) | |||
| RU (mL) | <50 | 18 (41.9) | 49 (43.3) | ||
| ≧50 | 25 (58.1) | 51 (56.7) | 2.41 (0.71–8.16) | 0.87 | |
| MCC (mL) | <350 | 7 (16.3) | 16 (17.8) | 0.54 (0.15–1.92) | 0.83 |
| ≧350 | 36 (83.7) | 74 (82.8) | |||
| Pdet (cm H2O) | <15 | 2 (4.7) | 3 (3.3) | 2.93 (0.68–12.65) | 0.66 * |
| ≧15 | 41 (95.3) | 87 (96.7) | |||
| FUL (mm) | <25 | 6 (14.0) | 15 (16.7) | 1.13 (0.34–3.75) | 0.69 |
| ≧25 | 37 (86.0) | 75 (83.3) | |||
| MUCP (cm H2O) | <40 | 7 (16.3) | 77 (7.8) | 0.97 (0.24–3.88) | 0.14 |
| ≧40 | 36 (83.7) | 81 (92.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.-Y.; Wang, C.-L.; Loo, Z.-X.; Lin, K.-L.; Long, C.-Y. Clinical Risk Factors for Uterine Cervical Elongation among Women with Pelvic Organ Prolapse. Int. J. Environ. Res. Public Health 2021, 18, 9255. https://doi.org/10.3390/ijerph18179255
Liu Y-Y, Wang C-L, Loo Z-X, Lin K-L, Long C-Y. Clinical Risk Factors for Uterine Cervical Elongation among Women with Pelvic Organ Prolapse. International Journal of Environmental Research and Public Health. 2021; 18(17):9255. https://doi.org/10.3390/ijerph18179255
Chicago/Turabian StyleLiu, Yi-Yin, Chiu-Lin Wang, Zi-Xi Loo, Kun-Ling Lin, and Cheng-Yu Long. 2021. "Clinical Risk Factors for Uterine Cervical Elongation among Women with Pelvic Organ Prolapse" International Journal of Environmental Research and Public Health 18, no. 17: 9255. https://doi.org/10.3390/ijerph18179255
APA StyleLiu, Y.-Y., Wang, C.-L., Loo, Z.-X., Lin, K.-L., & Long, C.-Y. (2021). Clinical Risk Factors for Uterine Cervical Elongation among Women with Pelvic Organ Prolapse. International Journal of Environmental Research and Public Health, 18(17), 9255. https://doi.org/10.3390/ijerph18179255





