A Digital Fabrication of Dental Prosthesis for Preventing Self-Injurious Behavior Related to Autism Spectrum Disorder: A Case Report
Abstract
1. Introduction
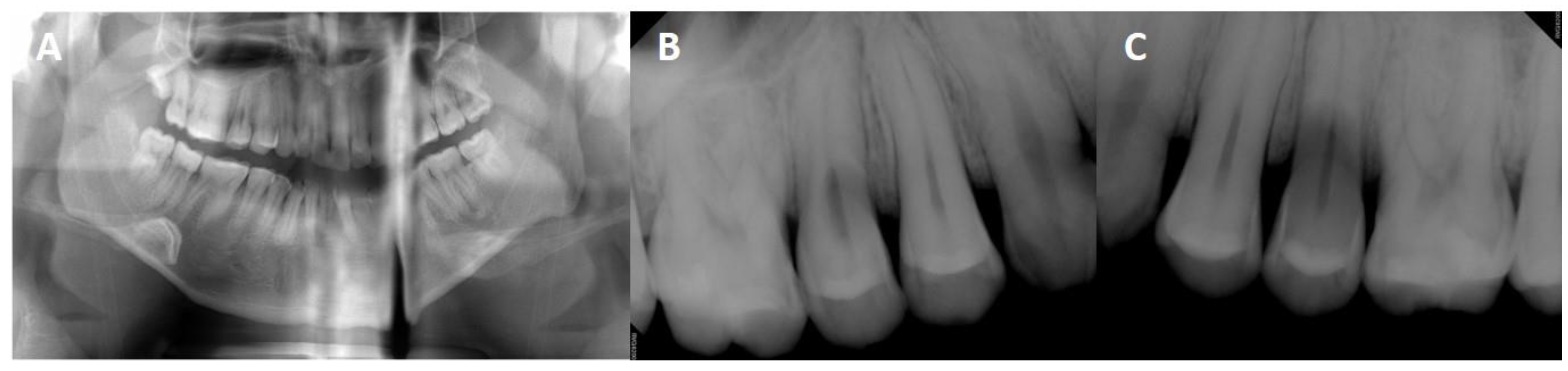
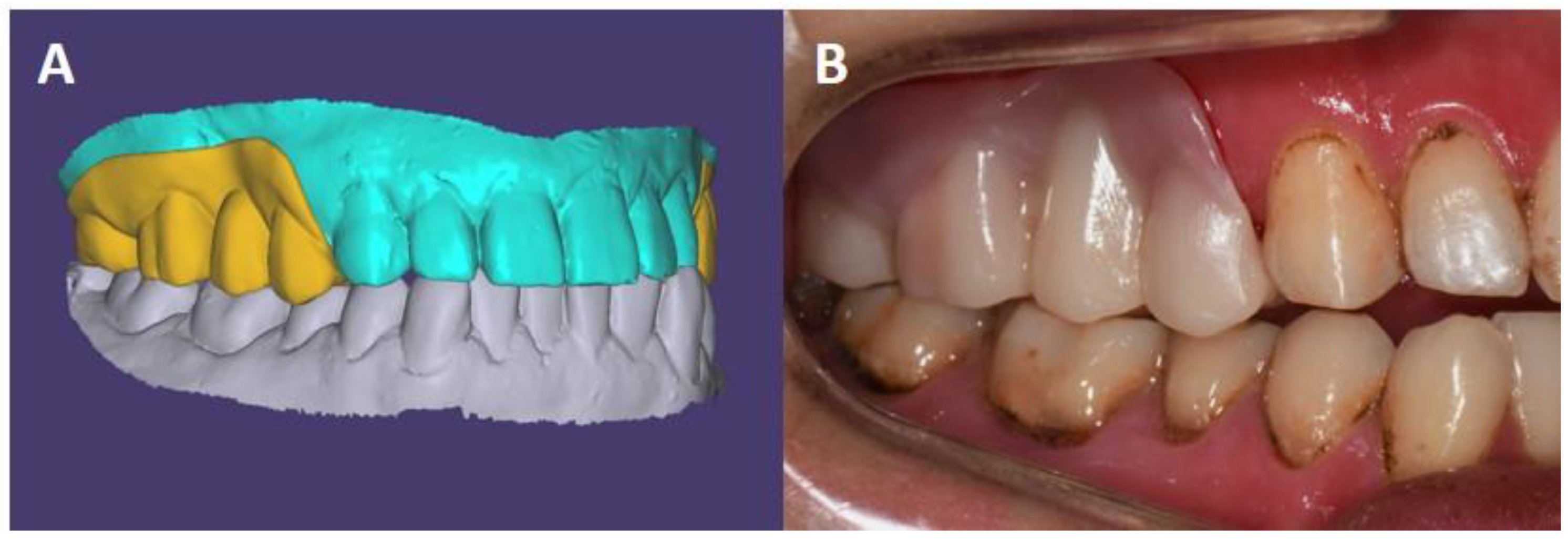
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013; Volume 21. [Google Scholar]
- Oh, T.J.; Nam, O.H.; Kim, M.S.; Choi, S.C.; Lee, H.S. Oral Health of Patients with Special Health Care Needs After General Anesthesia: A 25-Year Retrospective Study. Pediatr. Dent. 2018, 40, 215–219. [Google Scholar] [PubMed]
- Armstrong, D.; Matt, M. Autoextraction in an autistic dental patient: A case report. Spec. Care Dent. 1999, 19, 72–74. [Google Scholar] [CrossRef] [PubMed]
- Medina, A.C.; Sogbe, R.; Gómez-Rey, A.M.; Mata, M. Factitial oral lesions in an autistic paediatric patient. Int. J. Paediatr. Dent. 2003, 13, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Cannavale, R.; Itro, A.; Campisi, G.; Compilato, D.; Colella, G. Oral self-injuries: Clinical findings in a series of 19 patients. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e123–e129. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.; Shi, H.; Wang, H.; Wang, M.; Chen, F. Oral Health Status of Chinese Children With Autism Spectrum Disorders. Front. Psychiatry 2020, 11, 398. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, S.; McGlone, F.; Poole, H.; Moore, D.J. A Quantitative Sensory Testing Approach to Pain in Autism Spectrum Disorders. J. Autism Dev. Disord. 2020, 50, 1607–1620. [Google Scholar] [CrossRef] [PubMed]
- Failla, M.D.; Moana-Filho, E.J.; Essick, G.K.; Baranek, G.T.; Rogers, B.P.; Cascio, C.J. Initially intact neural responses to pain in autism are diminished during sustained pain. Autism 2018, 22, 669–683. [Google Scholar] [CrossRef] [PubMed]
- Olson, L.; Houlihan, D. A review of behavioral treatments used for Lesch-Nyhan syndrome. Behav. Modif. 2000, 24, 202–222. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.D.; Matt, M.K.; Dennison, D.; Brown, R.S.; Koh, S. Preventing factitious gingival injury in an autistic patient. J. Am. Dent. Assoc. 1996, 127, 244–247. [Google Scholar] [CrossRef] [PubMed]
- Steenfeldt-Kristensen, C.; Jones, C.A.; Richards, C. The Prevalence of Self-injurious Behaviour in Autism: A Meta-analytic Study. J. Autism Dev. Disord. 2020, 50, 3857–3873. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.R.; da Fonseca, M.A. Self-injurious behavior as a challenge for the dental practice: A case report. Pediatr. Dent. 2003, 25, 62–66. [Google Scholar] [PubMed]
- Kwon, I.J.; Kim, S.M.; Park, H.K.; Myoung, H.; Lee, J.H.; Lee, S.K. Successful treatment of self-inflicted tongue trauma patient using a special oral appliance. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 1938–1941. [Google Scholar] [CrossRef] [PubMed]
- Kiat-Amnuay, S.; Koh, S.H.; Powner, D.J. An occlusal guard for preventing and treating self-inflicted tongue trauma in a comatose patient: A clinical report. J. Prosthet. Dent. 2008, 99, 421–424. [Google Scholar] [CrossRef]
- Hong, S.J.; Lee, H.; Paek, J.; Pae, A.; Kim, H.S.; Kwon, K.R.; Noh, K. Combining Conventional Impressions and Intraoral Scans: A Technique for the Treatment of Complete Denture Patients with Flabby Tissue. J. Prosthodont. 2019, 28, 592–595. [Google Scholar] [CrossRef] [PubMed]
- Farwell, D.G.; Reilly, D.F.; Weymuller, E.A., Jr.; Greenberg, D.L.; Staiger, T.O.; Futran, N.A. Predictors of perioperative complications in head and neck patients. Arch. Otolaryngol. Head Neck Surg. 2002, 128, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Baydas, S.; Bayindir, F.; Akyil, M.S. Effect of processing variables (different compression packing processes and investment material types) and time on the dimensional accuracy of polymethyl methacrylate denture bases. Dent. Mater. J. 2003, 22, 206–213. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cionca, N.; Hashim, D.; Mombelli, A. Zirconia dental implants: Where are we now, and where are we heading? Periodontol. 2000 2017, 73, 241–258. [Google Scholar] [CrossRef] [PubMed]
- Jones, E.; Allen, D.; Moore, K.; Phillips, B.; Lowe, K. Restraint and self-injury in people with intellectual disabilities: A review. J. Intellect. Disabil. 2007, 11, 105–118. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, S.-J.; Chae, Y.K.; Lee, C.; Choi, S.C.; Nam, O.H. A Digital Fabrication of Dental Prosthesis for Preventing Self-Injurious Behavior Related to Autism Spectrum Disorder: A Case Report. Int. J. Environ. Res. Public Health 2021, 18, 9249. https://doi.org/10.3390/ijerph18179249
Hong S-J, Chae YK, Lee C, Choi SC, Nam OH. A Digital Fabrication of Dental Prosthesis for Preventing Self-Injurious Behavior Related to Autism Spectrum Disorder: A Case Report. International Journal of Environmental Research and Public Health. 2021; 18(17):9249. https://doi.org/10.3390/ijerph18179249
Chicago/Turabian StyleHong, Seoung-Jin, Yong Kwon Chae, Chunui Lee, Sung Chul Choi, and Ok Hyung Nam. 2021. "A Digital Fabrication of Dental Prosthesis for Preventing Self-Injurious Behavior Related to Autism Spectrum Disorder: A Case Report" International Journal of Environmental Research and Public Health 18, no. 17: 9249. https://doi.org/10.3390/ijerph18179249
APA StyleHong, S.-J., Chae, Y. K., Lee, C., Choi, S. C., & Nam, O. H. (2021). A Digital Fabrication of Dental Prosthesis for Preventing Self-Injurious Behavior Related to Autism Spectrum Disorder: A Case Report. International Journal of Environmental Research and Public Health, 18(17), 9249. https://doi.org/10.3390/ijerph18179249







