Diagnosis-Specific Work Disability before and after Lumbar Spine Decompression Surgery—A Register Study from Sweden
Abstract
1. Introduction
2. Materials and Methods
2.1. Registers
2.2. Study Populations
2.3. Outcome Measures
2.4. Covariates
2.5. Statistical Analyses
3. Results
4. Discussion
Strengths and Limitations
5. Ethical Considerations
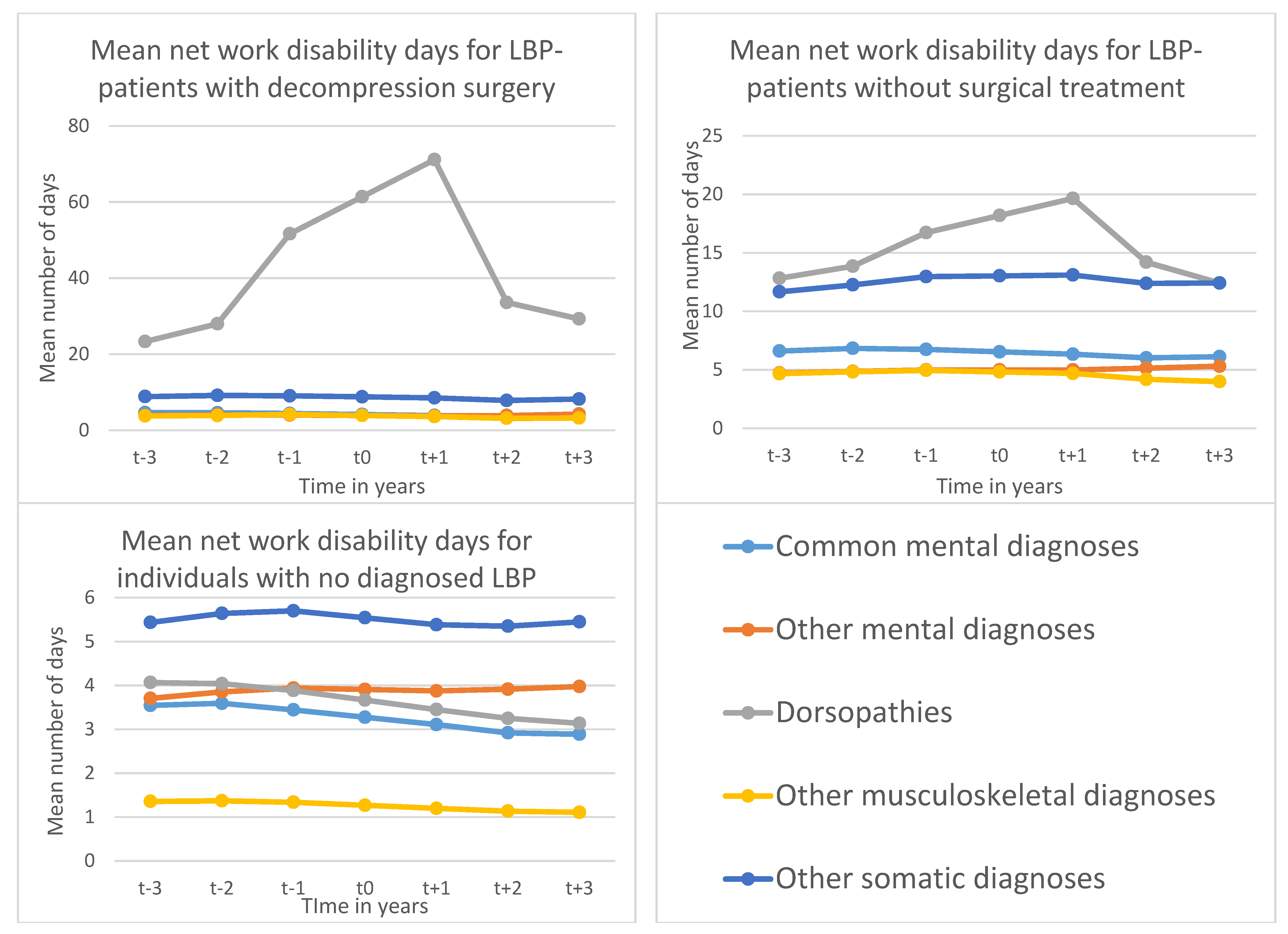
- This is the first register-based prospective cohort study on work disability following lumber decompression surgery, covering all individuals living in Sweden aged between 19–60 years.
- LBP-patients undergoing lumber spine decompression surgery (LSDS) had higher work disability during three years following surgery than patients without surgery and individuals without diagnosed LBP.
- LBP-patients undergoing LSDS had higher work disability three years following surgery than three years before, indicating unfavourable work disability prognosis, due to degenerative spine diseases.
- LSDS seems to be able to restrict the increasing work disability trend due to degenerative spine disease in the LBP-patients in the long run.
- Interventions and disability policy should focus on LBP-patients with degenerative spine disease.
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mittendorfer-Rutz, E.; Dorner, T.E. Socio-economic factors associated with the 1-year prevalence of severe pain and pain-related sickness absence in the Austrian population. Wien. Klin. Wochenschr. 2017, 130, 4–13. [Google Scholar] [CrossRef]
- Dorner, T.E.; Alexanderson, K.; Svedberg, P.; Ropponen, A.; Stein, K.; Mittendorfer-Rutz, E. Sickness absence due to back pain or depressive episode and the risk of all-cause and diagnosis-specific disability pension: A Swedish cohort study of 4,823,069 individuals. Eur. J. Pain 2015, 19, 1308–1320. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef]
- Strömqvist, B.; Fritzell, P.; Hägg, O.; Jönsson, B.; Sandén, B. Swespine: The Swedish spine register, 2012 report. Eur Spine J. 2013, 22, 953–974. [Google Scholar] [CrossRef] [PubMed]
- Dorner, T.E.; Helgesson, M.; Nilsson, K.; Pazarlis, K.A.; Ropponen, A.; Svedberg, P.; Mittendorfer-Rutz, E. Course and characteristics of work disability 3 years before and after lumbar spine decompression surgery- a national population-based study. Sci. Rep. 2018, 8, 11811. [Google Scholar] [CrossRef]
- Lurie, J.; Tomkins-Lane, C. Management of lumbar spinal stenosis. BMJ 2016, 352, h6234. [Google Scholar] [CrossRef]
- Zaina, F.; Tomkins-Lane, C.; Carragee, E.; Negrini, S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst. Rev. 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Weber, H. Lumbar disc herniation: A controlled, prospective study with ten years of observation. Spine 1983, 8, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, J.N.; Lurie, J.D.; Tosteson, T.D.; Zhao, W.; Blood, E.A.; Tosteson, A.N.A.; Birkmeyer, N.; Herkowitz, H.; Longley, M.; Lenke, L.; et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J. Bone. Jt. Surg. Am. 2009, 91, 1295–1304. [Google Scholar] [CrossRef] [PubMed]
- Dorner, T.E.; Alexanderson, K.; Svedberg, P.; Tinghög, P.; Ropponen, A.; Mittendorfer-Rutz, E. Synergistic effect between back pain and common mental disorders and the risk of future disability pension: A nationwide study from Sweden. Psychol. Med. 2015, 46, 425–436. [Google Scholar] [CrossRef]
- Pieber, K.; A Stamm, T.; Hoffmann, K.; Dorner, T.E. Synergistic effect of pain and deficits in ADL towards general practitioner visits. Fam. Pr. 2015, 32, 426–430. [Google Scholar] [CrossRef][Green Version]
- Nordstoga, A.L.; Nilsen, T.I.L.; Vasseljen, O.; Unsgaard-Tøndel, M.; Mork, P.J. The influence of multisite pain and psychological comorbidity on prognosis of chronic low back pain: Longitudinal data from the Norwegian HUNT Study. BMJ Open 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Festin, K.; Alexanderson, K. Changes in sick-leave diagnoses over eleven years in a cohort of young adults initially sick-listed due to low back, neck, or shoulder diagnoses. J. Rehabil. Med. 2009, 41, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Sumanen, H.; Pietiläinen, O.; Lahti, J.; Lahelma, E.; Rahkonen, O. Interrelationships between education, occupational class and income as determinants of sickness absence among young employees in 2002–2007 and 2008. BMC Public Health 2015, 15, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F.; Otterblad-Olausson, P.; Pettersson, B.U.; Ekbom, A.; Otterblad-olausson, J.F.L.P.; Pettersson, B.U.; Ekbom, A. The Swedish personal identity number: Possibilities and pitfalls in healthcare and medical research. Eur. J. Epidemiol. 2009, 24, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.; Svedberg, P.; Olén, O.; Bruze, G.; Neovius, M. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur. J. Epidemiol. 2019, 34, 423–437. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, L.; Rydh, H.; Björkenstam, E.; Jacobsson, A.; Nyqvist, K.; Heurgren, M. Kvalitet och Innehåll i Patientregistret. Utskrivningar Från Slutenvården 1964–2007 och Besök i Specialiserad Öppenvård; Report No.: 2008-125-1; The National Board of Health and Welfare (Socialstyrelsen): Stockholm, Sweden, 2008. (In Swedish)
- Ludvigsson, J.; Andersson, E.; Ekbom, A.; Feychting, M.; Kim, J.-L.; Reuterwall, C.; Heurgren, M.; Olausson, P.O. External review and validation of the Swedish national inpatient register. BMC Public Health 2011, 11, 450. [Google Scholar] [CrossRef]
- Wettermark, B.; Hammar, N.; Fored, C.M.; Leimanis, A.; Olausson, P.O.; Bergman, U.; Persson, I.; Sundström, A.; Westerholm, B.; Rosén, M. The new Swedish Prescribed Drug Register—Opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol. Drug Saf. 2007, 16, 726–735. [Google Scholar] [CrossRef] [PubMed]
- Brooke, H.L.; Talbäck, M.; Hörnblad, J.; Johansson, L.A.; Ludvigsson, J.F.; Druid, H.; Feychting, M.; Ljung, R. The Swedish cause of death register. Eur. J. Epidemiol. 2017, 32, 765–773. [Google Scholar] [CrossRef]
- WHO. International Statistical Classification of Diseases and Related Health Problems; 10 revision (ICD 10); WHO: Geneva, Switzerland, 2010. [Google Scholar]
- WHOCC. WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index 2016. Available online: http://www.whocc.no/atc_ddd_index/ (accessed on 7 February 2016).
- Ballinger, G.A. Using Generalized Estimating Equations for Longitudinal Data Analysis. Organ. Res. Methods 2004, 7, 127–150. [Google Scholar] [CrossRef]
- Dagenais, S.; Tricco, A.C.; Haldeman, S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine J. 2010, 10, 514–529. [Google Scholar] [CrossRef]
- Watters, W.C. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J. 2009, 9, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Wilson, C.A.; Roffey, D.; Chow, D.; Alkherayf, F.; Wai, E.K. A systematic review of preoperative predictors for postoperative clinical outcomes following lumbar discectomy. Spine J. 2016, 16, 1413–1422. [Google Scholar] [CrossRef] [PubMed]
- Helgesson, M.; Marklund, S.; Gustafsson, K.; Aronsson, G.; Leineweber, C. Interaction Effects of Physical and Psychosocial Working Conditions on Risk for Sickness Absence: A Prospective Study of Nurses and Care Assistants in Sweden. Int. J. Environ. Res. Public Health 2020, 17, 7427. [Google Scholar] [CrossRef]
- Niedhammer, I.; Sultan-Taïeb, H.; Parent-Thirion, A.; Chastang, J.-F. Update of the fractions of cardiovascular diseases and mental disorders attributable to psychosocial work factors in Europe. Int. Arch. Occup. Environ. Health 2021, 2021, 1–15. [Google Scholar] [CrossRef]
- Dorner, T.E.; Crevenna, R. Preventive aspects regarding back pain. Wien. Med. Wochenschr. 2016, 166, 15–21. [Google Scholar] [CrossRef]
- Ludvigsson, J.F.; Almqvist, C.; Bonamy, A.-K.E.; Ljung, R.; Michaëlsson, K.; Neovius, M.; Stephansson, O.; Ye, W. Registers of the Swedish total population and their use in medical research. Eur. J. Epidemiol. 2016, 31, 125–136. [Google Scholar] [CrossRef]
| Socio-Demographic Factors | N (%) =10,800 (100%) |
| Sex | |
| Women | 5100 (52.8) |
| Men | 5700 (47.2) |
| Age (in years) | |
| 19–24 | 376 (3.5) |
| 25–34 | 1339 (12.4) |
| 35–44 | 2662 (24.7) |
| 45–54 | 2623 (24.3) |
| 55–60 | 3800 (35.2) |
| Education (in years) | |
| Low (<10) | 2161 (20.0) |
| Medium (10–12) | 5632 (52.2) |
| High (>12) | 3007 (27.8) |
| Type of living area 1 | |
| Big cities | 4107 (38.0) |
| Medium-sized cities | 3688 (34.2) |
| Small cities/villages | 3005 (27.8) |
| Region of birth | |
| Sweden | 9127 (84.5) |
| Nordic countries (except Sweden) | 503 (4.7) |
| EU-25 Europe (except Nordic countries) | 226 (2.1) |
| Rest of the world | 944 (8.7) |
| Family situation | |
| Married/cohabiting without children living at home | 2424 (22.4) |
| Married/cohabiting with children living at home | 3332 (30.9) |
| Single 2 without children living at home | 3983 (36.9) |
| Single with children living at home | 905 (8.4) |
| Aged ≤ 20 years living with parents | 156 (1.4) |
| LSDS n (%) 10,800 (100%) | LBP No LSDS n (%) 109,179 (100%) | No Diagnosed LBP n (%) 472,191 (100%) | |
|---|---|---|---|
| Previous in- or specialised outpatient care due to | |||
| Common mental disorders 1* | 644 (6.0) | 8981 (8.2) | 17,492 (3.7) |
| Other mental disorders 2* | 974 (9.0) | 13,309 (12.2) | 29,579 (6.3) |
| LBP 3* | 9725 (90.1) | 15,342 (14.1) | - |
| Degenerative spine diseases other than LBP 4* | 922 (8.5) | 6453 (5.9) | - |
| Somatic diagnoses other than musculoskeletal diseases 5* | 7453 (69.0) | 79,533 (72.8) | 241,467 (51.1) |
| Sickness absence in the year prior to inclusion * | |||
| 1–90 days | 2791 (25.8) | 17,084 (15.7) | 32,453 (6.9) |
| 91–180 days | 1148 (10.6) | 5175 (4.7) | 5792 (1.2) |
| 181–365 days | 992 (9.2) | 5017 (4.6) | 4887 (1.0) |
| Initiated in the year prior to inclusion | 373 (3.5) | 2069 (1.9) | 1631 (0.4) |
| Analgesics during the year prior to inclusion (N02A and N02B in DDDs) * | |||
| Low (>0 to 0.5) | 5909 (54.7) | 38,811 (35.6) | 46,280 (9.8) |
| Medium (>0.5 to 1.5) | 2073 (19.2) | 2214 (8.1) | 6106 (1.3) |
| High (>1.5) | 605 (5.6) | 3672 (3.4) | 1725 (0.4) |
| Anxiolytics during the year prior to inclusion (N05B in DDDs) * | |||
| Low (>0 to 0.5) | 1315 (12.2) | 10,444 (9.6) | 19,355 (4.1) |
| Medium (>0.5 to 1.5) | 147 (1.4) | 1624 (1.5) | 2734 (0.6) |
| High (>1.5) | 75 (0.7) | 943 (0.9) | 1336 (0.3) |
| Antidepressants during the year prior to inclusion (N06A in DDDs) * | |||
| Low (>0 to 0.5) | 920 (8.5) | 8511 (7.8) | 13,829 (2.9) |
| Medium (>0.5 to 1.5) | 826 (7.7) | 7599 (7.0) | 19,651 (4.2) |
| High (>1.5) | 439 (4.1) | 3856 (3.5) | 8425 (1.8) |
| Sedative/hypnotics during the year prior to inclusion (N05C in DDDs) * | |||
| Low (>0 to 0.5) | 1024 (9.5) | 9812 (9.0) | 20,471 (4.3) |
| Medium (>0.5 to 1.5) | 564 (5.2) | 5003 (4.6) | 8946 (1.9) |
| High (>1.5) | 299 (2.8) | 2482 (2.3) | 3603 (0.8) |
| Outcome Measures in Relation to Diagnosis-Specific Work Disability Days | Pre-Inclusion Period (Year t − 1 vs. t − 3 ^) RR (95% CI) | Near Inclusion Period (Year t + 1 vs. t − 1 ^) RR (95% CI) | Post-Inclusion Period (Year t + 3 vs. t + 1 ^) RR (95% CI) |
|---|---|---|---|
| Work disability days due to degenerative spine diseases | |||
| LSDS | 2.21 (2.12–2.32) | 1.38 (1.35–1.41) | 0.41 (0.39–0.43) |
| LBP no LSDS | 1.30 (1.29–1.32) | 1.18 (1.16–1.19) | 0.63 (0.62–0.64) |
| No diagnosed LBP | 0.91 (0.90–0.92) | 0.89 (0.88–0.90) | 0.86 (0.82–0.91) |
| Work disability days due to other musculoskeletal diseases | |||
| LSDS | 1.10 (1.05–1.16) | 0.87 (0.83–0.90) | 0.89 (0.83–0.96) |
| LBP no LSDS | 1.06 (1.04–1.08) | 0.95 (0.94–0.96) | 0.85 (0.83–0.87) |
| No diagnosed LBP | 0.99 (0.98–1.00) | 0.90 (0.89–0.90) | 0.93 (0.91–0.94) |
| Work disability days due to CMDs | |||
| LSDS | 0.95 (0.89–1.03) | 0.88 (0.83–0.93) | 1.00 (0.90–1.11) |
| LBP no LSDS | 1.02 (1.00–1.04) | 0.94 (0.92–0.96) | 0.97 (0.94–0.99) |
| No diagnosed LBP | 0.97 (0.96–0.98) | 0.90 (0.89–0.91) | 0.93 (0.92–0.94) |
| Work disability days due to other mental disorders | |||
| LSDS | 1.03 (0.95–1.10) | 0.94 (0.89–0.99) | 1.13 (1.02–1.25) |
| LBP no LSDS | 1.06 (1.04–1.08) | 1.00 (0.99–1.02) | 1.07 (1.04–1.09) |
| No diagnosed LBP | 1.06 (1.06–1.07) | 0.98 (0.98–0.99) | 1.03 (1.02–1.04) |
| Work disability days due to other somatic diagnoses | |||
| LSDS | 1.02 (0.98–1.07) | 0.94 (0.91–0.98) | 0.96 (0.90–1.03) |
| LBP no LSDS | 1.11 (1.10–1.13) | 1.01 (1.00–1.02) | 0.95 (0.93–0.96) |
| No diagnosed LBP | 1.05 (1.04–1.06) | 0.95 (0.94–0.95) | 1.01 (1.00–1.02) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dorner, T.E.; Mittendorfer-Rutz, E.; Helgesson, M.; Lallukka, T.; Ervasti, J.; Pazarlis, K.; Ropponen, A.; Svedberg, P.; Wang, M.; Rahman, S. Diagnosis-Specific Work Disability before and after Lumbar Spine Decompression Surgery—A Register Study from Sweden. Int. J. Environ. Res. Public Health 2021, 18, 8937. https://doi.org/10.3390/ijerph18178937
Dorner TE, Mittendorfer-Rutz E, Helgesson M, Lallukka T, Ervasti J, Pazarlis K, Ropponen A, Svedberg P, Wang M, Rahman S. Diagnosis-Specific Work Disability before and after Lumbar Spine Decompression Surgery—A Register Study from Sweden. International Journal of Environmental Research and Public Health. 2021; 18(17):8937. https://doi.org/10.3390/ijerph18178937
Chicago/Turabian StyleDorner, Thomas E., Ellenor Mittendorfer-Rutz, Magnus Helgesson, Tea Lallukka, Jenni Ervasti, Konstantinos Pazarlis, Annina Ropponen, Pia Svedberg, Mo Wang, and Syed Rahman. 2021. "Diagnosis-Specific Work Disability before and after Lumbar Spine Decompression Surgery—A Register Study from Sweden" International Journal of Environmental Research and Public Health 18, no. 17: 8937. https://doi.org/10.3390/ijerph18178937
APA StyleDorner, T. E., Mittendorfer-Rutz, E., Helgesson, M., Lallukka, T., Ervasti, J., Pazarlis, K., Ropponen, A., Svedberg, P., Wang, M., & Rahman, S. (2021). Diagnosis-Specific Work Disability before and after Lumbar Spine Decompression Surgery—A Register Study from Sweden. International Journal of Environmental Research and Public Health, 18(17), 8937. https://doi.org/10.3390/ijerph18178937








