Reduction of Fatigue and Musculoskeletal Complaints in Garment Sewing Operator through a Combination of Stretching Brain Gym® and Touch for Health
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subject
2.2. Intervention Program
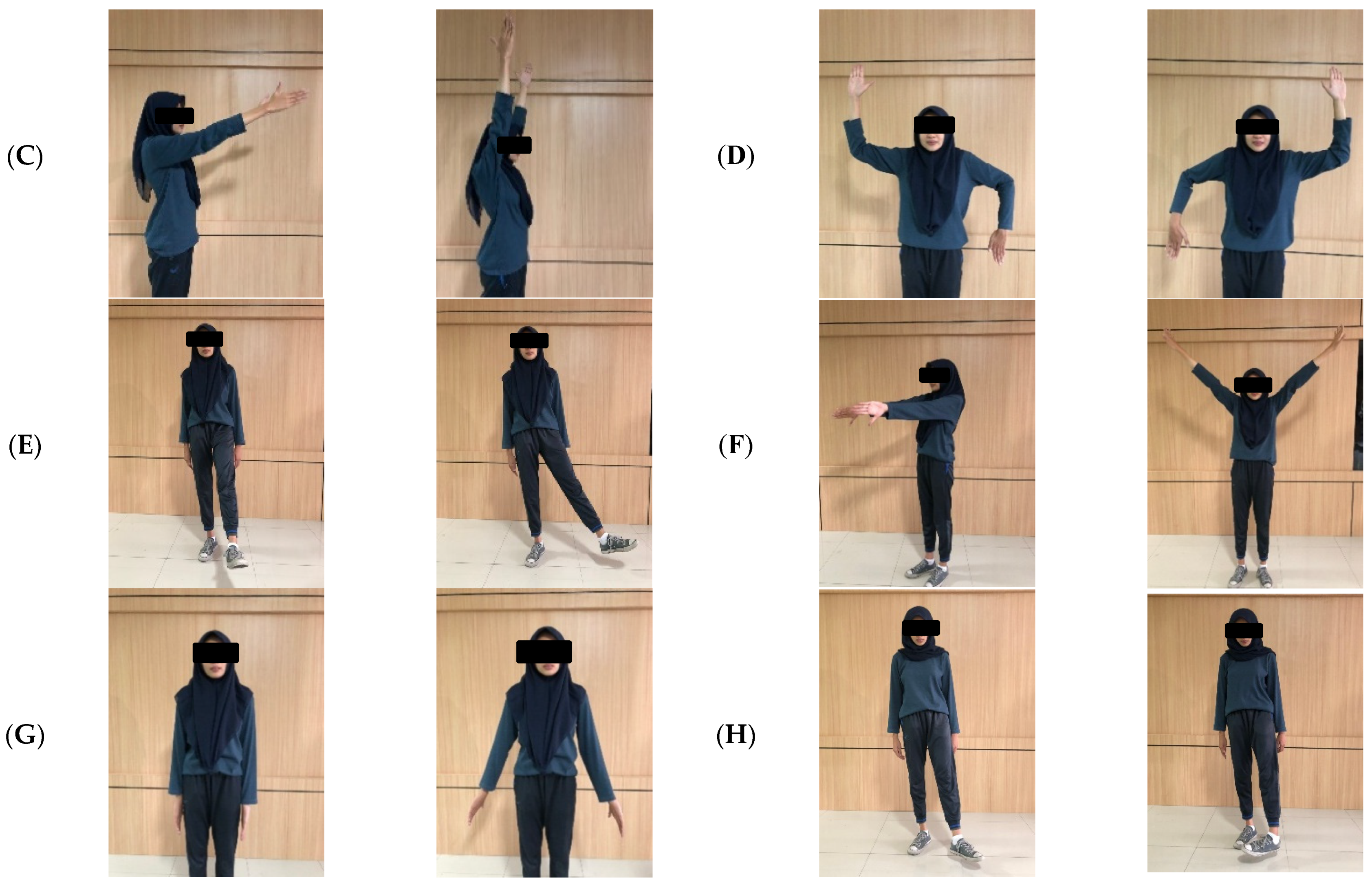
2.2.1. Stretching Movement
2.2.2. Combination BG + TfH Movements
2.3. Instrument and Measurement Protocol
2.4. Statistical Analysis
2.5. Ethics Approval
3. Results
3.1. Variation in Fatigue
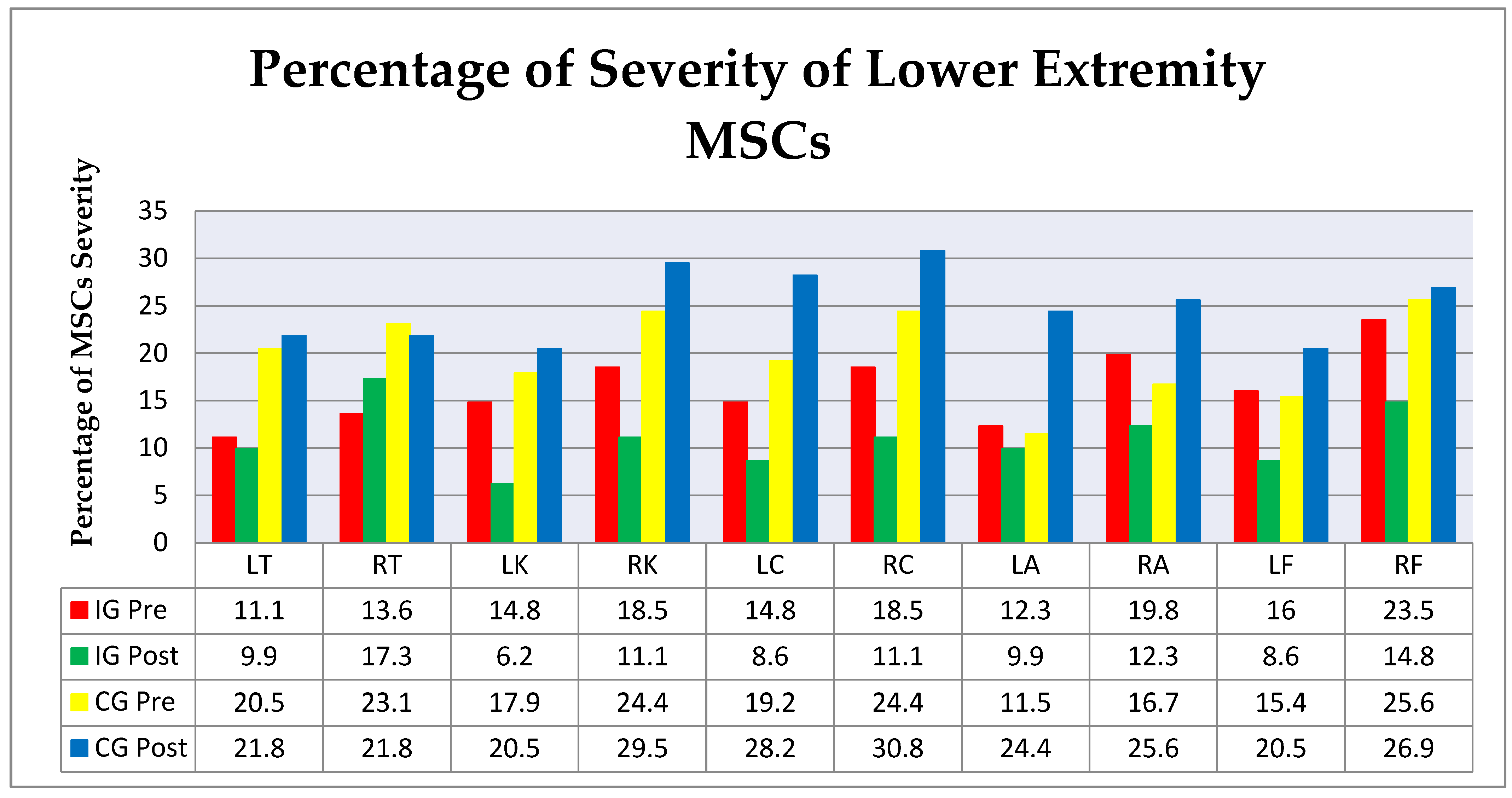
3.2. Variation in Musculoskeletal Complaints
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shafiqul, I. Informal Labor Incentives and Firm Performance: A Case Study of RMG Industry in Bangladesh. Int. Bus. Manag. 2014, 8, 19–27. [Google Scholar]
- Perry, P.; Wood, S.; Fernie, J. Corporate Social Responsibility in Garment Sourcing Networks: Factory Management Perspectives on Ethical Trade in Sri Lanka. J. Bus. Ethics 2015, 130, 737–752. [Google Scholar] [CrossRef]
- Saha, T.K.; Dasgupta, A.; Butt, A.; Chattopadhyay, O. Health status of workers engaged in the small-scale garment industry: How healthy are they. Indian J. Community Med. 2010, 35, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Telaprolu, N.; Siresha, M. Visual and Musculoskeletal Problems Among Sewing Machine Operators in A Readymade Garment Industry Neeraja Telaprolu Metta Siresha. Int. J. Sci. Res. 2016, 5, 529–532. [Google Scholar]
- Gearhart, J. Women Human Rights Defenders; International Labor Rights Forum: Washington, DC, USA, 2019. [Google Scholar]
- Nagaraj, T.S.; Jeyapaul, R. Ergonomic Study on Work Postures of Sewing Machine Operators in Government Industry: A Case in Lean Environment Garment Industry. In Ergonomic Design of Products and Worksystems-21st Century Perspectives of Asia; Springer: Singapore, 2018; ISBN 978-981-10-5457-0. [Google Scholar]
- Ahmed, S. Health Status of the Female Workers in the Garment Sector of Bangladesh. J. Fac. Econ. Adm. Sci. 2014, 4, 43–58. [Google Scholar]
- Biadgo, G.H.; Tsegay, G.S.; Mohammednur, S.A.; Gebremeskel, B.F. Burden of Neck Pain and Associated Factors Among Sewing Machine Operators of Garment Factories in Mekelle City, Northern Part of Ethiopia, 2018, A Cross-Sectional Study. Saf. Health Work 2021, 12, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Kanniappan, V.; Palani, V. Prevalence of Musculoskeletal Disorders among Sewing Machine Workers in a Leather Industry. J. Lifestyle Med. 2020, 10, 121–125. [Google Scholar] [CrossRef]
- Kennedy, C.A.; Amick, B.C.; Dennerlein, J.T.; Brewer, S.; Catli, S.; Williams, R.; Serra, C.; Gerr, F.; Irvin, E.; Mahood, Q.; et al. Systematic Review of the Role of Occupational Health and Safety Interventions in the Prevention of Upper Extremity Musculoskeletal Symptoms, Signs, Disorders, Injuries, Claims and Lost Time; Springer: New York, NY, USA, 2010; Volume 20, ISBN 1092600992112. [Google Scholar]
- Huibers, M.J.H.; Beurskens, A.J.H.M.; Prins, J.B.; Kant, I.J.; Bazelmans, E.; Van Schayck, C.P.; Knottnerus, J.A.; Bleijenberg, G. Fatigue, burnout, and chronic fatigue syndrome among employees on sick leave: Do attributions make the difference? Occup. Environ. Med. 2003, 60, 26–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Raeve, L.; Jansen, N.W.H.; IJmert, K. Health effects of transitions in work schedule, workhours and overtime in a prospective cohort study. Scand. J. Work Environ. Health 2007, 33, 105–113. [Google Scholar] [CrossRef] [Green Version]
- Janssen, N.; Kant, I.J.; Swaen, G.M.H.; Janssen, P.P.M.; Schröer, C.A.P. Fatigue as a predictor of sickness absence: Results from the Maastricht cohort study on fatigue at work. Occup. Environ. Med. 2003, 60, 71–77. [Google Scholar] [CrossRef] [Green Version]
- Dos Leite, W.K.S.; da Araújo, A.J.S.; Norte da Silva, J.M.; Gontijo, L.A.; de Vieira, E.M.A.; Lopes de Souza, E.; Colaço, G.A.; Bueno da Silva, L. Risk factors for work-related musculoskeletal disorders among workers in the footwear industry: A cross-sectional study. Int. J. Occup. Saf. Ergon. 2021, 27, 393–409. [Google Scholar] [CrossRef] [PubMed]
- Mahdavi, N.; Dianat, I.; Heidarimoghadam, R.; Khotanlou, H. International Journal of Industrial Ergonomics Review article A review of work environment risk factors influencing muscle fatigue. Int. J. Ind. Ergon. 2020, 80, 1–18. [Google Scholar] [CrossRef]
- Kebede Deyyas, W.; Tafese, A. Environmental and organizational factors associated with Elbow/Forearm and Hand/Wrist disorder among sewing machine operators of garment industry in Ethiopia. J. Environ. Public Health 2014, 2014, 732731. [Google Scholar] [CrossRef]
- Ravichandran, S.P.; Shah, P.B.; Lakshminarayanan, K.; Ravichandran, A.P. Musculoskeletal problems among workers in a garment industry, at Tirupur, Tamil Nadu. Indian J. Community Health 2016, 28, 269–274. [Google Scholar]
- Öztürk, N.; Esin, M.N. Investigation of musculoskeletal symptoms and ergonomic risk factors among female sewing machine operators in Turkey. Int. J. Ind. Ergon. 2011, 41, 585–591. [Google Scholar] [CrossRef]
- Aghili, M.M.M.; Asilian, H.; Poursafa, P. Evaluation of musculoskeletal disorders in sewing machine operators of a shoe manufacturing factory in iran. J. Pak. Med. Assoc. 2012, 62, S-20–S-25. [Google Scholar]
- Merisalu, E.; Mannaste, M.; Hiir, K.; Traumann, A. Predictors and prevalence of musculoskeletal disorders among sewing machine operators. Agron. Res. 2016, 14, 1417–1426. [Google Scholar]
- Senarath, M.K.I.D.; Rajeev, P.R.; Ranathunga, R.M.R.U.; Rasenthiram, A.; Senavirathna, S.A.D.C.S.; Senavirathna, D.N.K.M.; Somarathna, H.N.T.M.; Maduwanthika, K.S.P.; Rajarathne, A.A.J. Prevalence of Neck Pain among Female Sewing Workers due to Bad Posture in Garment Factories of Kurunegala. In Proceedings of the Peradeniya Univ. International Research Sessions, Sri Lanka, Kandy, Sri Lanka, 4–5 July 2014; Volume 18, p. 2014. [Google Scholar]
- Bulduk, S.; Bulduk, E.Ö.; Süren, T. Reduction of Work-Related Musculoskeletal Risk Factors Following Ergonomics Education of Sewing Machine Operators. Int. J. Occup. Saf. Ergon. 2017, 23, 347–352. [Google Scholar] [CrossRef]
- Lugay, C.I.P.; Matias, A.C. Predictive Models of Work-Related Musculoskeletal Disorders (WMSDs) among Sewing Machine Operators in the Garments Industry. Asia Pac. J. Multidiscip. Res. 2015, 3, 56–64. [Google Scholar]
- OHSCO. MSD Musculoskeletal Disorders Occupational Health and Safety Council of Ontario (OHSCO) MSD Prevention Guideline for Ontario Disclaimer; OHSCO: Ontario, ON, Canada, 2006. [Google Scholar]
- Shariat, A.; Cleland, J.A.; Danaee, M.; Kargarfard, M.; Sangelaji, B.; Bahri, S.; Tamrin, M. Brazilian Journal of Effects of stretching exercise training and ergonomic modifications on musculoskeletal discomforts of office workers: A randomized controlled trial. Braz. J. Phys. Ther. 2018, 22, 144–153. [Google Scholar] [CrossRef]
- Nimbarte, A.D. International Journal of Industrial Ergonomics Risk of neck musculoskeletal disorders among males and females in lifting exertions. Int. J. Ind. Ergon. 2014, 44, 253–259. [Google Scholar] [CrossRef]
- Hassanlouei, H.; Arendt-nielsen, L.; Kersting, U.G.; Falla, D. Effect of exercise-induced fatigue on postural control of the knee. J. Electromyogr. Kinesiol. 2012, 22, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Santos, H.G.; Chiavegato, L.D.; Valentim, D.P.; Padula, R.S. Effectiveness of a progressive resistance exercise program for industrial workers during breaks on perceived fatigue control: A cluster randomized controlled trial. BMC Public Health 2020, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- de Vries, J.D.; van Hooff, M.L.M.; Geurts, S.A.E.; Kompier, M.A.J. Exercise to reduce work-related fatigue among employees: A randomized controlled trial. Scand. J. Work. Environ. Health 2017, 43, 337–349. [Google Scholar] [CrossRef] [PubMed]
- Machado-matos, M.; Miguel, P. Impact of a workplace exercise program on neck and shoulder segments in office workers Impacto de un programa de ejercicio en el trabajo en los segmentos de cuello y hombros en los trabajadores de oficina. DYNA 2016, 83, 63–68. [Google Scholar] [CrossRef]
- Marangoni, A.H. Effects of intermittent stretching exercises at work on musculoskeletal pain associated with the use of a personal computer and the influence of media on outcomes. Work 2010, 36, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Tunwattanapong, P.; Kongkasuwan, R. The effectiveness of a neck and shoulder stretching exercise program among office workers with neck pain: A randomized controlled trial. Clin. Rehabil. 2016, 30, 64–72. [Google Scholar] [CrossRef]
- Andersen, L.L.; Saervoll, C.A.; Mortensen, O.S.; Poulsen, O.M.; Hannerz, H.; Zebis, M.K. Effectiveness of small daily amounts of progressive resistance training for frequent neck/shoulder pain: Randomised controlled trial. Pain 2011, 152, 440–446. [Google Scholar] [CrossRef]
- Andersen, C.H.; Andersen, L.L.; Gram, B.; Pedersen, M.T.; Mortensen, O.S.; Zebis, M.K.; Sjøgaard, G. Influence of frequency and duration of strength training for effective management of neck and shoulder pain: A randomised controlled trial. Br. J. Sports Med. 2012, 46, 1004–1010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bispo, L.G.M.; da Silva, J.M.N.; Bolis, I.; dos Santos Leite, W.K.; de Araujo Vieira, E.M.; Colaço, G.A.; de Souza, E.L.; Gontijo, L.A.; da Silva, L.B. Effects of a worksite physical activities program among men and women: An interventional study in a footwear industry. Appl. Ergon. 2020, 84, 103005. [Google Scholar] [CrossRef] [PubMed]
- De Lacaze, D.H.C.; de Sacco, I.C.N.; Rocha, L.E.; de Bragança Pereira, C.A.; Casarotto, R.A. Stretching and Joint Mobilization Exercises Reduce Call-Center Operators ’Musculoskeletal Discomfort and Fatigue clinical science stretching and joint mobilization exercises reduce call-center operators’ musculoskeletal discomfort and fatigue. Clin. Sci. 2010, 7, 657–662. [Google Scholar]
- Andersen, L.L.; Bang, K.; Holtermann, A.; Poulsen, O.M.; Sjøgaard, G.; Pedersen, M.T.; Hansen, E.A. Effect of physical exercise interventions on musculoskeletal pain in all body regions among office workers: A one-year randomized controlled trial. Man. Ther. 2010, 15, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, A.; Rabal-pelay, J.; Berzosa, C. Effect of a Long Exercise Program in the Reduction of Musculoskeletal Discomfort in Office Workers. Int. J. Environ. Res. Public. Health 2020, 17, 9042. [Google Scholar] [CrossRef] [PubMed]
- Shariat, A.; Lam, E.T.C.; Kargarfard, M.; Tamrin, S.B.M. The application of a feasible exercise training program in the office setting. Work 2017, 56, 421–428. [Google Scholar] [CrossRef]
- Sihawong, R.; Janwantanakul, P.; Sitthipornvorakul, E.; Pensri, P. Exercise Therapy for Office Workers With Nonspecific Neck Pain: A Systematic Review. J. Manip. Physiol. Ther. 2010, 34, 62–71. [Google Scholar] [CrossRef]
- Louw, S.; Makwela, S.; Manas, L.; Terblanche, D.; Brink, Y. Effectiveness of exercise in office workers with neck pain: A systematic review and meta-analysis. S. Afr. J. Pshysiother. 2016, 73, 329. [Google Scholar] [CrossRef] [PubMed]
- Effendy, E.; Prasanty, N.; Utami, N. The effects of brain gym on quality of sleep, anxiety in elderly at nursing home care case Medan. Open Access Maced. J. Med. Sci. 2019, 7, 2595–2598. [Google Scholar] [CrossRef] [Green Version]
- Dennison, P. Brain Gym Teacher’s Edition The Companion Guide to Brain Gym: Simple Activities for Whole-Brain Learning; Edu-Kinestetics, Inc: Ventura, CA, USA, 2010; ISBN 0-942143-02-7. [Google Scholar]
- Doewes, M. Exercise and Brain Health in Elderly. Angew. Chem. Int. Ed. 1967, 6, 951–952. [Google Scholar]
- Sifft, J.M.; Khalsa, G.C. Effect of educational kinesiology upon simple response times and choice response times. Percept. Mot. Skills 1991, 73, 1011–1015. [Google Scholar] [CrossRef]
- Andrea, W.; Ginger, L. The Effect of Brain Gym® on Academic Engagement for Children With Developmental Disabilities. J. Chem. Inf. Model. 2019, 29, 1–9. [Google Scholar]
- Tschernitschek, H.; Fink, M. “Angewandte Kinesiologie” in medizin und zahnmedizin-Eine kritische übersicht. Wien. Med. Wochenschr. 2005, 155, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Thie, J.; Thie, M. Touch for Health: A Practical Guide to Natural Health with Acupressure Touch; Rehker, A., Prince, A., Eds.; First, Sec.; DeVorss & Company: Camarillo, CA, USA, 2006; ISBN 13:9780875368128. [Google Scholar]
- Pulat, B.M. Fundamentals of Industrial Ergonomics; Atkin, L.C., Ed.; Prentic-Hall, Inc.: Englewood Cliffs, NJ, USA, 1992; ISBN 0-13-345364-2. [Google Scholar]
- Lee, J.-H.; Gak, H.B. Effects of Self Stretching on Pain and Musculoskeletal Symptom of Bus Drivers. Soc. Phys. Ther. Sci. 2014, 26, 1911–1914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, B.; Anderson, J. Stretching; Shelter Publications Inc.: Bolinas, CA, USA, 2000; ISBN 9780936070223. [Google Scholar]
- Demuth, E. Touch for Health Express; Amini, A., Ed.; First Prin; YAKINDO: Tomohon, Indonesia, 2018; ISBN 978-602-520-140-0. [Google Scholar]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Crawford, J.O. The Nordic Musculoskeletal Questionnaire. Occup. Med. 2007, 57, 300–301. [Google Scholar] [CrossRef] [Green Version]





| Variable | IG (n = 27) | CG (n = 26) | P | |
|---|---|---|---|---|
| Age (year) | 31.33 ± 10.52 | 32.12 ± 9.04 | 0.315 | |
| Working period (year) | 7.37 ± 7.23 | 5.09 ± 6.06 | 0.270 | |
| Pulse (bpm) | 97.37 ± 14.80 | 91.08 ± 13.71 | 0.706 | |
| Weight (kg) | 55.78 ± 11.25 | 53.12 ± 12.80 | 0.259 | |
| Height (cm) | 152.31 ± 4.62 | 152.42 ± 5.16 | 0.540 | |
| Body mass index (BMI) (kg/m2) | 24.05 ± 4.94 | 22.91 ± 5.53 | 0.176 | |
| Variable | n | Frequency | Percentage (%) | |
| Education | Elementary School | 53 | 3 | 5.6 |
| Middle School | 20 | 37.7 | ||
| High School | 30 | 56.7 | ||
| Smoke | Yes | 53 | 0 | 0 |
| No | 53 | 100 | ||
| Fatigue | ||||
|---|---|---|---|---|
| Pre | Post | p0 | p1 | |
| IG | 319.16 ± 197 | 279.79 ± 155 | <0.001 | 0.046 |
| CG | 257.7 ± 121 | 260.57 ± 89 | 0.200 | |
| MSCs | ||||
|---|---|---|---|---|
| Pre | Post | p0 | p1 | |
| IG | 15 ± 15 | 9 ± 12 | <0.001 | <0.001 |
| CG | 16.5 ± 11 | 20 ± 16 | 0.106 | |
| Intervention Group | p | Mean Diff | Control Group | p | Mean Diff | |||
|---|---|---|---|---|---|---|---|---|
| Pre Mean ± SD (Min − Max) | Post Mean ± SD (Min − Max) | Pre Mean ± SD (Min − Max) | Post Mean ± SD (Min − Max) | |||||
| Upper Neck | 0.63 ± 0.9 (0.0–4.0) | 0.41 ± 0.6 (0.0–2.0) | 0.317 | −0.22 | 0.62 ± 0.6 (0.0–2.0) | 0.77 ± 0.6 (0.0–2.0) | 0.248 | +0.15 |
| Lower Neck | 0.74 ± 0.8 (0.0–3.0) | 0.67 ± 0.6 (0.0–2.0) | 0.635 | −0.07 | 0.92 ± 0.6 (0.0–2.0) | 0.69 ± 0.5 (0.0–2.0) | 0.153 | −0.23 |
| Left Shoulder | 0.52 ± 0.7 (0.0–2.0) | 0.37 ± 0.6 (0.0–2.0) | 0.206 | −0.15 | 1.04 ± 0.7 (0.0–2.0) | 1.04 ± 0.8 (0.0–2.0) | 0.971 | 0 |
| Right Shoulder | 0.59 ± 0.7 (0.0–2.0) | 0.59 ± 0.6 (0.0–2.0) | 1.000 | 0 | 0.96 ± 0.7 (0.0–2.0) | 0.96 ± 0.7 (0.0–2.0) | 1.000 | 0 |
| Left Lower Arm | 0.30 ± 0.7 (0.0–2.0) | 0.19 ± 0.4 (0.0–1.0) | 0.380 | −0.11 | 0.35 ± 0.6 (0.0–2.0) | 0.58 ± 0.6 (0.0–2.0) | 0.109 | +0.23 |
| Back | 0.78 ± 0.7 (0.0–2.0) | 0.59 ± 0.6 (0.0–2.0) | 0.215 | −0.19 | 0.92 ± 0.8 (0.0–2.0) | 0.85 ± 0.7 (0.0–2.0) | 0.617 | −0.07 |
| Right Lower Arm | 0.30 ± 0.6 (0.0–2.0) | 0.30 ± 0.4 (0.0–1.0) | 1.000 | 0 | 0.58 ± 0.6 (0.0–3.0) | 0.73 ± 0.6 (0.0–2.0) | 0.206 | +0.15 |
| Waist | 0.70 ± 0.8 (0.0–2.0) | 0.63 ± 0.6 (0.0–2.0) | 0.635 | −0.07 | 1.20 ± 0.7(0.0–3.0) | 1.20 ± 0.7 (0.0–2.0) | 0.976 | 0 |
| Buttock | 0.63 ± 0.7 (0.0–2.0) | 0.41 ± 0.6 (0.0–2.0) | 0.175 | −0.22 | 1.00 ± 0.8 (0.0–2.0) | 0.96 ± 0.7 (0.0–2.0) | 0.771 | −0.04 |
| Bottom | 0.59 ± 0.8 (0.0–3.0) | 0.37 ± 0.6 (0.0–2.0) | 0.109 | −0.22 | 0.58 ± 0.7 (0.0–1.0) | 0.96 ± 0.9 (0.0–2.0) | 0.032 * | +0.38 |
| Left Elbow | 0.15 ± 0.6(0.0–3.0) | 0.15 ± 0.5 (0.0–2.0) | 1.000 | 0 | 0.12 ± 0.3 (0.0–2.0) | 0.42 ± 0.6 (0.0–2.0) | 0.011 * | +0.30 |
| Right Elbow | 0.22 ± 0.6(0.0–3.0) | 0.15 ± 0.5 (0.0–2.0) | 0.680 | −0.07 | 0.19 ± 0.6 (0.0–2.0) | 0.54 ± 0.7 (0.0–2.0) | 0.021 * | +0.35 |
| Left Upper Arm | 0.44 ± 0.8 (0.0–3.0) | 0.26 ± 0.6 (0.0–2.0) | 0.059 | −0.18 | 0.39 ± 0.6 (0.0–2.0) | 0.77 ± 0.9 (0.0–3.0) | 0.032 * | +0.38 |
| Right Upper Arm | 0.44 ± 0.7 (0.0–2.0) | 0.33 ± 0.6 (0.0–2.0) | 0.257 | −0.11 | 0.50 ± 0.6 (0.0–2.0) | 0.96 ± 0.8 (0.0–2.0) | 0.005 * | +0.46 |
| Left Wrist | 0.59 ± 0.8 (0.0–3.0) | 0.22 ± 0.5 (0.0–2.0) | 0.008 * | −0.37 | 0.62 ± 0.8(0.0–2.0) | 0.65 ± 0.7 (0.0–2.0) | 0.184 | 0 |
| Right Wrist | 0.67 ± 0.8 (0.0–3.0) | 0.41 ± 0.5 (0.0–1.0) | 0.106 | −0.16 | 0.65 ± 0.8 (0.0–2.0) | 0.85 ± 0.9 (0.0–3.0) | 0.190 | +0.20 |
| Left Hand | 0.56 ± 0.8 (0.0–2.0) | 0.26 ± 0.5 (0.0–2.0) | 0.046 * | −0.30 | 0.50 ± 0.7 (0.0–2.0) | 0.65 ± 0.7 (0.0–2.0) | 0.331 | +0.15 |
| Right Hand | 0.74 ± 0.8 (0.0–2.0) | 0.44 ± 0.5 (0.0–1.0) | 0.073 | −0.30 | 0.69 ± 0.7 (0.0–2.0) | 0.81 ± 0.7 (0.0–2.0) | 0.366 | +0.12 |
| Left Thigh | 0.33 ± 0.7 (0.0–2.0) | 0.30 ± 0.5 (0.0–2.0) | 0.705 | −0.03 | 0.62 ± 0.6 (0.0–2.0) | 0.58 ± 0.8 (0.0–3.0) | 0.763 | −0.04 |
| Right Thigh | 0.41 ± 0.6 (0.0–2.0) | 0.52 ± 0.5 (0.0–2.0) | 0.257 | +0.11 | 0.69 ± 0.6 (0.0–2.0) | 0.65 ± 0.7 (0.0–2.0) | 0.763 | −0.04 |
| Left Knee | 0.44 ± 0.8 (0.0–3.0) | 0.19 ± 0.4 (0.0–1.0) | 0.035 * | −0.25 | 0.54 ± 0.7 (0.0–2.0) | 0.62 ± 0.7(0.0–2.0) | 0.564 | +0.08 |
| Right Knee | 0.56 ± 0.8 (0.0–3.0 | 0.33 ± 0.6 (0.0–2.0) | 0.130 | −0.23 | 0.73 ± 0.8 (0.0–1.0) | 0.89 ± 0.9 (0.0–3.0) | 0.372 | +0.01 |
| Left Calf | 0.44 ± 0.7 (0.0–2.0) | 0.26 ± 0.4 (0.0–1.0) | 0.059 | −0.18 | 0.58 ± 0.5 (0.0–2.0) | 0.85 ± 0.8(0.0–2.0) | 0.151 | +0.27 |
| Right Calf | 0.56 ± 0.8 (0.0–3.0) | 0.33 ± 0.5 (0.0–1.0) | 0.109 | −0.23 | 0.73 ± 0.5 (0.0–2.0) | 0.92 ± 0.8 (0.0–2.0) | 0.272 | +0.19 |
| Left Ankle | 0.37 ± 0.7 (0.0–2.0) | 0.30 ± 0.6 (0.0–2.0) | 0.414 | −0.07 | 0.35 ± 0.6 (0.0–2.0) | 0.73 ± 0.7 (0.0–2.0) | 0.013 * | +0.38 |
| Right Ankle | 0.59 ± 0.8 (0.0–3.0) | 0.37 ± 0.6 (0.0–2.0) | 0.058 | −0.22 | 0.50 ± 0.6 (0.0–2.0) | 0.77 ± 0.8 (0.0–3.0) | 0.124 | +0.22 |
| Left Foot | 0.48 ± 0.9 (0.0–4.0) | 0.26 ± 0.5 (0.0–2.0) | 0.132 | −0.22 | 0.46 ± 0.7 (0.0–2.0) | 0.62 ± 0.7 (0.0–2.0) | 0.206 | +0.16 |
| Right Foot | 0.70 ± 1.0 (0.0–4.0) | 0.44 ± 0.6 (0.0–2.0) | 0.083 | −0.26 | 0.77 ± 0.7(0.0–2.0) | 0.81 ± 0.7 (0.0–2.0) | 0.803 | +0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ismayenti, L.; Suwandono, A.; Denny, H.M.; Widjanarko, B. Reduction of Fatigue and Musculoskeletal Complaints in Garment Sewing Operator through a Combination of Stretching Brain Gym® and Touch for Health. Int. J. Environ. Res. Public Health 2021, 18, 8931. https://doi.org/10.3390/ijerph18178931
Ismayenti L, Suwandono A, Denny HM, Widjanarko B. Reduction of Fatigue and Musculoskeletal Complaints in Garment Sewing Operator through a Combination of Stretching Brain Gym® and Touch for Health. International Journal of Environmental Research and Public Health. 2021; 18(17):8931. https://doi.org/10.3390/ijerph18178931
Chicago/Turabian StyleIsmayenti, Lusi, Agus Suwandono, Hanifa Maher Denny, and Bagoes Widjanarko. 2021. "Reduction of Fatigue and Musculoskeletal Complaints in Garment Sewing Operator through a Combination of Stretching Brain Gym® and Touch for Health" International Journal of Environmental Research and Public Health 18, no. 17: 8931. https://doi.org/10.3390/ijerph18178931
APA StyleIsmayenti, L., Suwandono, A., Denny, H. M., & Widjanarko, B. (2021). Reduction of Fatigue and Musculoskeletal Complaints in Garment Sewing Operator through a Combination of Stretching Brain Gym® and Touch for Health. International Journal of Environmental Research and Public Health, 18(17), 8931. https://doi.org/10.3390/ijerph18178931






