Work Organization Factors Associated with Health and Work Outcomes among Apprentice Construction Workers: Comparison between the Residential and Commercial Sectors
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
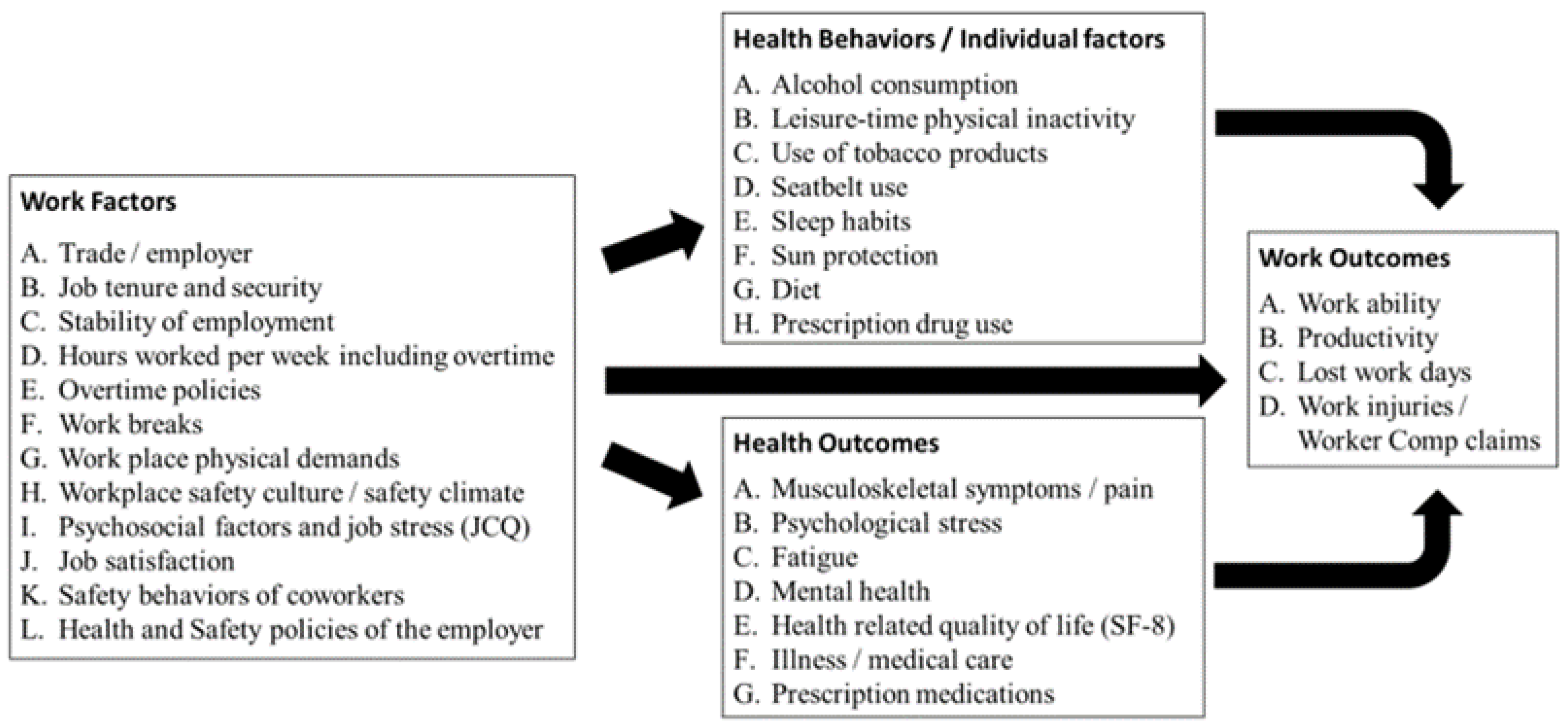
2.2. Survey
2.3. Analysis
3. Results
3.1. Study Population and Demographics
3.2. Work Organization and Environment Factors
3.3. Health Behaviors and Health Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wong, K.; Chan, A.H.S.; Ngan, S.C. The Effect of Long Working Hours and Overtime on Occupational Health: A Meta-Analysis of Evidence from 1998 to 2018. Int. J. Environ. Res. Public Health 2019, 16, 2102. [Google Scholar] [CrossRef] [PubMed]
- Ray, T.K.; Kenigsberg, T.A.; Pana-Cryan, R. Employment arrangement, job stress, and health-related quality of life. Saf. Sci. 2017, 100, 46–56. [Google Scholar] [CrossRef]
- Chang, Y.-H.; Yang, H.-H.; Hsu, W.-J. Effects of work shifts on fatigue levels of air traffic controllers. J. Air Transp. Manag. 2019, 76, 1–9. [Google Scholar] [CrossRef]
- Khamisa, N.; Peltzer, K.; Oldenburg, B. Burnout in relation to specific contributing factors and health outcomes among nurses: A systematic review. Int. J. Environ. Res. Public Health 2013, 10, 2214–2240. [Google Scholar] [CrossRef]
- Martinussen, M.; Richardsen, A.M.; Burke, R.J. Job demands, job resources, and burnout among police officers. J. Crim. Justice 2007, 35, 239–249. [Google Scholar] [CrossRef]
- Ângelo, R.P.; Chambel, M.J. The reciprocal relationship between work characteristics and employee burnout and engagement: A longitudinal study of firefighters. Stress Health 2015, 31, 106–114. [Google Scholar] [CrossRef]
- Ariza-Montes, A.; Arjona-Fuentes, J.M.; Han, H.; Law, R. Work environment and well-being of different occupational groups in hospitality: Job Deman„ ControŒ Support model. Int. J. Hosp. Manag. 2018, 73, 1–11. [Google Scholar] [CrossRef]
- Jung, H.S.; Jung, Y.S.; Yoon, H.H. COVID-19: The effects of job insecurity on the job engagement and turnover intent of deluxe hotel employees and the moderating role of generational characteristics. Int. J. Hosp. Manag. 2021, 92, 102703. [Google Scholar] [CrossRef]
- Evanoff, B.A.; Rohlman, D.S.; Strickland, J.R.; Dale, A.M. Influence of work organization and work environment on missed work, productivity, and use of pain medications among construction apprentices. Am. J. Ind. Med. 2020, 63, 269–276. [Google Scholar] [CrossRef]
- Acharya, P.; Boggess, B.; Zhang, K. Assessing Heat Stress and Health among Construction Workers in a Changing Climate: A Review. Int. J. Environ. Res. Public Health 2018, 15, 247. [Google Scholar] [CrossRef] [PubMed]
- Dale, A.M.; Ryan, D.; Welch, L.; Olsen, M.A.; Buchholz, B.; Evanoff, B. Comparison of musculoskeletal disorder health claims between construction floor layers and a general working population. Occup. Environ. Med. 2015, 72, 15–20. [Google Scholar] [CrossRef]
- Dong, X.W.S.; Wang, X.W.; Daw, C.; Ringen, K. Chronic Diseases and Functional Limitations Among Older Construction Workers in the United States: A 10-Year Follow-up Study. J. Occup. Environ. Med. 2011, 53, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Hung, Y.; Smith-Jackson, T.; Winchester, W. Use of attitude congruence to identify safety interventions for small residential builders. Constr. Manag. Econ. 2011, 29, 113–130. [Google Scholar] [CrossRef]
- Barnes, A.J.; Brown, E.R. Occupation as an Independent Risk Factor for Binge Drinking. Am. J. Drug Alcohol Abuse 2013, 39, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Boal, W.L.; Li, J.; Dong, X.S.; Sussell, A. Health Risk Behavior Profile of Construction Workers, 32 States, 2013–2016. J. Occup. Environ. Med. 2020, 62, 493502. [Google Scholar] [CrossRef] [PubMed]
- CPWR: The Center for Construction Research and Training. The Construction Chart Book: The United States Construction Industry and Its Workers, 6th ed.; CPWR: Silver Spring, MD, USA, 2018. [Google Scholar]
- Harley, A.E.; Devine, C.M.; Beard, B.; Stoddard, A.M.; Hunt, M.K.; Sorensen, G. Multiple health behavior changes in a cancer prevention intervention for construction workers, 2001–2003. Prev. Chronic Dis. 2010, 7, A55. [Google Scholar]
- Strickland, J.R.; Wagan, S.; Dale, A.M.; Evanoff, B.A. Prevalence and Perception of Risky Health Behaviors Among Construction Workers. J. Occup. Environ. Med. 2017, 59, 673–678. [Google Scholar] [CrossRef]
- Oude Hengel, K.M.; Blatter, B.M.; van der Molen, H.F.; Bongers, P.M.; van der Beek, A.J. The effectiveness of a construction worksite prevention program on work ability, health, and sick leave: Results from a cluster randomized controlled trial. Scand. J. Work Environ. Health 2013, 39, 456–467. [Google Scholar] [CrossRef]
- Lipscomb, H.J.; Dement, J.M.; Li, L.; Nolan, J.; Patterson, D. Work-related injuries in residential and drywall carpentry. Appl. Occup. Environ. Hyg. 2003, 18, 479–488. [Google Scholar] [CrossRef]
- Choi, S.D.; Carlson, K. Occupational Safety Issues in Residential Construction Surveyed in Wisconsin, United States. Ind. Health 2014, 52, 541–547. [Google Scholar] [CrossRef]
- Ringen, K.; Dong, X.S.; Goldenhar, L.M.; Cain, C.T. Construction Safety and Health in the USA: Lessons from a Decade of Turmoil. Ann. Work Expo. Health 2018, 62, S25–S33. [Google Scholar] [CrossRef]
- Stiehl, E.; Forst, L. Safety Climate Among Nontraditional Workers in Construction: Arguing for a Focus on Construed External Safety Image. N. Solut. 2018, 28, 33–54. [Google Scholar] [CrossRef]
- Solovieva, S.; Lallukka, T.; Virtanen, M.; Viikari-Juntura, E. Psychosocial factors at work, long work hours, and obesity: A systematic review. Scand. J. Work Environ. Health 2013, 39, 241–258. [Google Scholar] [CrossRef]
- Strickland, J.R.; Eyler, A.A.; Purnell, J.Q.; Kinghorn, A.M.; Herrick, C.; Evanoff, B.A. Enhancing workplace wellness efforts to reduce obesity: A qualitative study of low-wage workers in St Louis, Missouri, 2013–2014. Prev. Chronic Dis. 2015, 12, E67. [Google Scholar] [CrossRef]
- Lee, D.; Fleming, L.; Arheart, K.; LeBlanc, W.; Caban, A.; Chung-Bridges, K.; Christ, S.; McCollister, K.; Pitman, T. Smoking rate trends in U.S. occupational groups: The 1987 to 2004 National Health Interview Survey. J. Occup. Environ. Med. 2007, 49, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Kosinski, M.; Dewey, J.E.; Gandek, B. How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8 Health Survey; QualityMetric Incorporated: Lincoln, RI, USA, 2001. [Google Scholar]
- Baecke, J.A.; Burema, J.; Frijters, J.E. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am. J. Clin. Nutr. 1982, 36, 936–942. [Google Scholar] [CrossRef]
- Karasek, R.; Brisson, C.; Kawakami, N.; Houtman, I.; Bongers, P.; Amick, B. The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. J. Occup. Health Psychol. 1998, 3, 322–355. [Google Scholar] [CrossRef]
- Zohar, D.; Luria, G. A multilevel model of safety climate: Cross-level relationships between organization and group-level climates. J. Appl. Psychol. 2005, 90, 616–628. [Google Scholar] [CrossRef]
- Franzblau, A.; Salerno, D.F.; Armstrong, T.J.; Werner, R.A. Test-retest reliability of an upper-extremity discomfort questionnaire in an industrial population. Scand. J. Work Environ. Health 1997, 23, 299–307. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Questionnaire. 2015. Available online: https://www.cdc.gov/brfss/questionnaires/pdf-ques/2016_BRFSS_Questionnaire_FINAL.pdf (accessed on 12 December 2019).
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Ilmarinen, J. The Work Ability Index (WAI). Occup. Med. 2007, 57, 160. [Google Scholar] [CrossRef]
- Reilly, M.C.; Zbrozek, A.S.; Dukes, E.M. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 1993, 4, 353–365. [Google Scholar] [CrossRef]
- Zou, G. A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 2004, 159, 702–706. [Google Scholar] [CrossRef]
- Neal, A.; Griffin, M. A study of the lagged relationships among safety climate, safety motivation, safety behavior, and accidents at the individual and group levels. J. Appl. Psychol. 2006, 91, 946–953. [Google Scholar] [CrossRef]
- Bureau of Labor Statistics. Industry Injury and Illness Data. 2018. Table SNR05. Available online: https://www.bls.gov/iif/oshsum.htm#18Summary_Tables (accessed on 17 December 2019).
- Silverstein, B.; Viikari-Juntura, E.; Kalat, J. Use of a prevention index to identify industries at high risk for work-related musculoskeletal disorders of the neck, back, and upper extremity in Washington state, 1990–1998. Am. J. Ind. Med. 2002, 41, 149–169. [Google Scholar] [CrossRef]
- Lipscomb, H.J.; Nolan, J.; Patterson, D.; Sticca, V.; Myers, D.J. Safety, incentives, and the reporting of work-related injuries among union carpenters: “You’re pretty much screwed if you get hurt at work”. Am. J. Ind. Med. 2013, 56, 389–399. [Google Scholar] [CrossRef]
- Dale, A.M.; Evanoff, B.; Macomber, M.; O’Reilly, M.; Rosen, R.; Schneider, S. Can Ergonomics Programs Help Solve the Opioid Crisis? Available online: https://synergist.aiha.org/201905-ergonomics-opioid-crisis (accessed on 15 July 2021).
- Massachusetts Department of Public Health Occupational Health Surveillance Program. Opioid-Related Overdose Deaths in Massachusetts by Industry and Occupation, 2011–2015. Available online: https://www.mass.gov/doc/opioid-related-overdose-deaths-in-massachusetts-by-industry-and-occupation-2011-2015/download (accessed on 30 April 2021).
- McCoy, A.; Kucera, K.; Schoenfisch, A.; Silverstein, B.; Lipscomb, H. Twenty years of work-related injury and illness among union carpenters in Washington State. Am. J. Ind. Med. 2013, 56, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Albers, J.T.; Estill, C.F. Simple Solutions: Ergonomics for Construction Workers. Available online: http://www.cdc.gov/niosh/docs/2007-122/pdfs/2007-122.pdf (accessed on 15 July 2021).
- Choi, S.D. A study of trade-specific occupational ergonomics considerations in the U.S. construction industry. Work 2012, 42, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Gerlach, K.K.; Shopland, D.R.; Hartman, A.M.; Gibson, J.T.; Pechacek, T.F. Workplace smoking policies in the United States: Results from a national survey of more than 100,000 workers. Tob. Control 1997, 6, 199–206. [Google Scholar] [CrossRef]
- Syamlal, G.; King, B.A.; Mazurek, J.M. Tobacco product use among workers in the construction industry, United States, 2014–2016. Am. J. Ind. Med. 2018, 61, 939–951. [Google Scholar] [CrossRef] [PubMed]
- Bauer, J.E.; Hyland, A.; Li, Q.; Steger, C.; Cummings, K.M. A longitudinal assessment of the impact of smoke-free worksite policies on tobacco use. Am. J. Public Health 2005, 95, 1024–1029. [Google Scholar] [CrossRef] [PubMed]
- Shields, M. Smoking bans: Influence on smoking prevalence. Health Rep. 2007, 18, 9–24. [Google Scholar] [PubMed]
- Dutra, L.M.; Kim, S.S.; Williams, D.R.; Kawachi, I.; Okechukwu, C.A. Worksite safety climate, smoking, and the use of protective equipment by blue-collar building workers enrolled in the MassBUILT smoking cessation trial. J. Occup. Environ. Med. 2014, 56, 1082–1087. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gillen, M.; Baltz, D.; Gassel, M.; Kirsch, L.; Vaccaro, D. Perceived safety climate, job demands, and coworker support among union and nonunion injured construction workers. J. Safety Res. 2002, 33, 33–51. [Google Scholar] [CrossRef]
- Weil, D. The Fissured Workplace: Why Work Became So Bad for So Many and What Can Be Done to Improve It; Harvard University Press: Cambridge, MA, USA, 2017; p. 424. [Google Scholar]
| Variable | Definition/Source |
|---|---|
| Work organization and environment | |
| Residential construction work | Yes/No—versus commercial construction work |
| Policies for (a) hearing protection, (b) gloves, (c) water access, or (d) seasonal temps | Yes/No |
| Frequent heavy load lifting | Lift heavy loads “often” or “always” [28] |
| High job strain | Strain ratio > 1 [29] |
| Low (a) supervisor and (b) coworker support | Below median [29] |
| Safety Climate scale score (a) Supervisor and (b) coworker support | Range 0–100 [30] |
| Low job satisfaction | Response other than “very satisfied” on 4-point scale [31] |
| Commute time (minutes) | Duration of commute, minutes each way |
| Precarious work | Disagree with “my job security is good” OR work not “regular and steady” [29] |
| Poor job security | Disagree with “my job security is good” [29] |
| Job instability | Report work not “regular and steady” [29] |
| (a) Mandatory overtime, (b) smoking restriction policy, (c) access to food, or (d) designated eating area | Yes/No |
| Health behaviors | |
| Alcohol consumption days/month | Days had at least 1 drink, past month [32] |
| Binge drinking days/month | Days had 5 or more drinks on one occasion, past month [32] |
| Current cigarette smoker | Smoke cigarettes “everyday” [32] |
| Current e-cigarette user | Use electronic cigarettes “everyday” or “some days [32] |
| Health outcomes | |
| Pain/discomfort of (a) neck/shoulder, (b) hand/wrist, (c) lower back, and (d) knee | Any, past 12 months [33] |
| Doctor visit due to musculoskeletal symptoms | For neck/hands/lower back/knees, past 12 months [33] |
| Prescribed medication for pain | Any, past 12 months |
| Poor (a) physical and (b) mental health | Physical or mental SF-8 scale score below 1st quartile [27] |
| Low energy (past 4 weeks) | “Some”, “a little” or “none” [27] |
| Tired after work | Tired “often” or “very often” after work [28] |
| Work outcomes | |
| Missed days due to (a) work-related injury, (b) any injury or pain, or (c) any illness | 1 or more missed days, past 12 months |
| Poor work ability | Score below 9 on 10 point scale [34] |
| Poor work ability for (a) physical demands and (b) mental demands | “Poor” or “rather poor” on 5 point scale [34] |
| Poor health related productivity | Score above 1 on 10 point scale [35] |
| Variable | Total n = 929 | Commercial n = 520 a | Residential n = 408 a | p-Value b |
|---|---|---|---|---|
| Work organization and environment | % | |||
| Residential construction work | 44.0 | - | - | - |
| Hearing protection policy | 51.0 | 63.8 | 34.6 | <0.001 |
| Glove requirement policy | 46.2 | 65.0 | 22.3 | <0.001 |
| Water access | 49.9 | 62.7 | 33.6 | <0.001 |
| Seasonal warmth and cooling | 33.3 | 50.0 | 12.0 | <0.001 |
| Frequent heavy load lifting | 76.3 | 69.8 | 84.6 | <0.001 |
| High job strain | 65.2 | 58.4 | 73.9 | <0.001 |
| Low supervisor support | 19.8 | 16.7 | 23.5 | 0.01 |
| Low coworker support | 22.8 | 18.5 | 28.4 | 0.001 |
| Low job satisfaction | 40.2 | 35.8 | 45.6 | 0.003 |
| Mandatory overtime | 8.5 | 11.4 | 4.8 | 0.001 |
| Precarious work | 22.7 | 21.5 | 24.3 | 0.4 |
| Poor job security | 17.4 | 16.9 | 18.1 | 0.7 |
| Job instability | 8.7 | 8.5 | 9.1 | 0.8 |
| Smoking restriction policy | 54.8 | 66.2 | 40.4 | <0.001 |
| Food access near workplace | 53.0 | 60.8 | 42.9 | <0.001 |
| Designated eating areas | 27.2 | 42.7 | 7.6 | <0.001 |
| mean (SD) | ||||
| Supervisor support for safety | 70.22 (±19.84) | 71.74 (±19.04) | 68.38 (±20.63) | 0.01 |
| Coworker support for safety | 67.85 (±20.26) | 70.03 (±18.51) | 65.05 (±22.02) | <0.001 |
| Commute time (minutes) | 44.61 (±33.08) | 46.54 (±39.31) | 42.14 (±22.60) | 0.03 |
| Health behaviors | % | |||
| Current cigarette smoker | 27.3 | 24.9 | 30.5 | 0.07 |
| Current e-cigarette user | 10.7 | 10.0 | 11.5 | 0.5 |
| mean (SD) | ||||
| Alcohol consumption days/month | 8.49 (±9.13) | 7.96 (±8.61) | 9.17 (±9.73) | 0.05 |
| Binge drinking days/month | 4.28 (±6.11) | 3.97 (±5.75) | 4.67 (±6.52) | 0.08 |
| Health outcomes | % | |||
| Neck/shoulder pain/discomfort | 48.5 | 43.4 | 55.0 | 0.001 |
| Hand/wrist pain/discomfort | 53.5 | 46.4 | 62.6 | <0.001 |
| Lower back pain/discomfort | 62.9 | 56.4 | 71.1 | <0.001 |
| Knee pain/discomfort | 49.2 | 45.3 | 54.4 | 0.009 |
| Doctor visit due to MS symptoms | 22.0 | 19.3 | 25.6 | 0.03 |
| Prescribed medication for pain | 12.1 | 9.8 | 15.1 | 0.02 |
| Poor physical health | 25.0 | 21.7 | 29.0 | 0.01 |
| Poor mental health | 25.0 | 21.7 | 29.3 | 0.01 |
| Low energy | 39.7 | 36.3 | 44.1 | 0.02 |
| Tired after work | 55.1 | 49.9 | 61.5 | 0.001 |
| Work outcomes | % | |||
| Missed days—work-related injury | 9.5 | 6.4 | 13.5 | <0.001 |
| Missed days—any injury or pain | 20.5 | 16.6 | 25.4 | 0.002 |
| Missed days due to any illness | 41.3 | 42.0 | 40.6 | 0.7 |
| Poor work ability | 24.1 | 21.7 | 27.1 | 0.08 |
| Poor health related productivity | 14.8 | 11.8 | 18.5 | 0.007 |
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| Variable | n | Cases (%) | PR | 95% CI | PR | 95% CI |
| Missed days due to work-related injury | ||||||
| Residential construction work | 408 | 5.92 | 2.12 | (1.39–3.21) | 1.89 | (1.10–3.26) |
| Mandatory overtime | 73 | 0.49 | 0.61 | (0.23–1.62) | 0.41 | (0.11–1.56) |
| Smoking restriction policy | 509 | 4.69 | 0.81 | (0.54–1.21) | 0.97 | (0.59–1.57) |
| Glove requirement policy | 429 | 3.35 | 0.64 | (0.42–0.98) | 0.98 | (0.54–1.76) |
| Frequent heavy load lifting | 709 | 8.26 | 2.09 | (1.13–3.85) | 1.72 | (0.86–3.44) |
| High job strain | 563 | 7.56 | 2.26 | (1.31–3.89) | 1.83 | (1.03–3.26) |
| Low coworker support | 208 | 2.16 | 1.08 | (0.66–1.76) | 0.70 | (0.39–1.24) |
| Low supervisor support | 182 | 2.59 | 1.57 | (1.00–2.46) | 1.60 | (0.94–2.74) |
| Poor health related productivity | ||||||
| Residential construction work | 408 | 8.16 | 1.57 | (1.14–2.15) | 1.52 | (1.01–2.30) |
| Mandatory overtime | 73 | 2.06 | 1.91 | (1.22–2.99) | 1.67 | (1.00–2.79) |
| Smoking restriction policy | 509 | 8.82 | 1.23 | (0.89–1.69) | 1.34 | (0.93–1.94) |
| Glove requirement policy | 429 | 6.14 | 0.83 | (0.60–1.14) | 0.82 | (0.54–1.26) |
| Frequent heavy load lifting | 709 | 12.39 | 1.55 | (1.01–2.39) | 1.60 | (0.95–2.69) |
| High job strain | 563 | 11.03 | 1.81 | (1.21–2.71) | 1.37 | (0.88–2.14) |
| Low coworker support | 208 | 5.22 | 1.81 | (1.31–2.50) | 1.49 | (1.02–2.19) |
| Low supervisor support | 182 | 4.74 | 1.85 | (1.34–2.57) | 1.19 | (0.80–1.78) |
| Lower back pain/discomfort | ||||||
| Residential construction work | 408 | 31.09 | 1.26 | (1.14–1.39) | 1.15 | (1.02–1.30) |
| Mandatory overtime | 73 | 5.84 | 1.09 | (0.93–1.29) | 1.10 | (0.92–1.32) |
| Smoking restriction policy | 509 | 32.49 | 0.88 | (0.80–0.97) | 0.92 | (0.82–1.03) |
| Glove requirement policy | 429 | 26.78 | 0.85 | (0.77–0.94) | 0.98 | (0.85–1.11) |
| Frequent heavy load lifting | 709 | 51.70 | 1.45 | (1.25–1.69) | 1.39 | (1.18–1.64) |
| High job strain | 563 | 43.21 | 1.21 | (1.08–1.37) | 1.09 | (0.96–1.24) |
| Low coworker support | 208 | 16.01 | 1.15 | (1.03–1.28) | 1.08 | (0.95–1.23) |
| Low supervisor support | 182 | 14.20 | 1.17 | (1.05–1.31) | 1.07 | (0.93–1.22) |
| Tired after work | ||||||
| Residential construction work | 408 | 27.08 | 1.23 | (1.10–1.38) | 1.15 | (1.00–1.33) |
| Mandatory overtime | 73 | 4.92 | 1.08 | (0.88–1.32) | 1.08 | (0.89–1.33) |
| Smoking restriction policy | 509 | 30.39 | 1.02 | (0.91–1.14) | 1.09 | (0.96–1.25) |
| Glove requirement policy | 429 | 24.14 | 0.91 | (0.81–1.03) | 1.02 | (0.88–1.18) |
| Frequent heavy load lifting | 709 | 46.55 | 1.70 | (1.41–2.05) | 1.71 | (1.38–2.11) |
| High job strain | 563 | 39.56 | 1.35 | (1.17–1.55) | 1.23 | (1.05–1.43) |
| Low coworker support | 208 | 14.29 | 1.19 | (1.05–1.35) | 1.11 | (0.95–1.28) |
| Low supervisor support | 182 | 12.75 | 1.22 | (1.08–1.39) | 1.12 | (0.97–1.30) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dale, A.M.; Rohlman, D.S.; Hayibor, L.; Evanoff, B.A. Work Organization Factors Associated with Health and Work Outcomes among Apprentice Construction Workers: Comparison between the Residential and Commercial Sectors. Int. J. Environ. Res. Public Health 2021, 18, 8899. https://doi.org/10.3390/ijerph18178899
Dale AM, Rohlman DS, Hayibor L, Evanoff BA. Work Organization Factors Associated with Health and Work Outcomes among Apprentice Construction Workers: Comparison between the Residential and Commercial Sectors. International Journal of Environmental Research and Public Health. 2021; 18(17):8899. https://doi.org/10.3390/ijerph18178899
Chicago/Turabian StyleDale, Ann Marie, Diane S. Rohlman, Lisa Hayibor, and Bradley A. Evanoff. 2021. "Work Organization Factors Associated with Health and Work Outcomes among Apprentice Construction Workers: Comparison between the Residential and Commercial Sectors" International Journal of Environmental Research and Public Health 18, no. 17: 8899. https://doi.org/10.3390/ijerph18178899
APA StyleDale, A. M., Rohlman, D. S., Hayibor, L., & Evanoff, B. A. (2021). Work Organization Factors Associated with Health and Work Outcomes among Apprentice Construction Workers: Comparison between the Residential and Commercial Sectors. International Journal of Environmental Research and Public Health, 18(17), 8899. https://doi.org/10.3390/ijerph18178899






