Associations of Maternal-Infant Bonding with Maternal Mental Health, Infant’s Characteristics and Socio-Demographical Variables in the Early Postpartum Period: A Cross-Sectional Study
Abstract
:1. Introduction
1.1. Medical Aspects of Preterm Birth
1.2. Psychological Aspects of Preterm Birth
1.3. Objectives
- What is the maternal postpartum bonding score among mothers after a preterm birth?
- What are scores of stress, anxiety, and depressive symptoms among mothers after a preterm birth?
- Is postpartum bonding associated with maternal mental health (depressive symptoms, anxiety, and stress)?
- Is postpartum bonding associated with a child’s characteristics (gestational age, birth weight, and final APGAR score)?
- Is postpartum bonding associated with socio-demographical variables (age, education level, and number of children in the household)?
2. Materials and Methods
2.1. Study Design and Procedures
- Woman in the reproductive age between 18 and 49 years and 11 months. The motivation for the cut-off age limit was due to the role of age in reproductive health (e.g., mothers higher in age are vulnerable to infertility, fetal anomalies, pregnancy loss, obstetric complications, and stillbirth) and mental health (e.g., lower age is related to depression, substance abuse, and posttraumatic stress disorder) [42,43,44,45].
- Parents of children born below the 37th week of pregnancy (clinical group) or above the 37th week of pregnancy (control group),
- Those that agreed to participate in the study after having completed information disclosures assessments and gave consent.
2.2. Variables and Measurement Tools
2.2.1. Maternal Postpartum Bonding
2.2.2. Maternal Postpartum Depressive Symptoms
2.2.3. Maternal Anxiety
2.2.4. Maternal Stress
2.2.5. Infant’s Characteristics
2.2.6. Socio-Demographic Information
- age (years);
- marital status (single, married, living together, not married, divorced, separated, widowed, and other);
- education level (primary/elementary or less; secondary school but not completed; secondary school graduate; university/college but not completed; and university degree (bachelor, master, PhD, or equivalent));
- work situation (employed full-time; employed part-time; self-employed; student full-time or part-time; stay-at-home parent; and unemployed and/or seeking work); and
- number of children in the household including the newborn participating in this study.
2.3. Statistical Analysis
- In the first step, we calculated the Pearson correlation coefficient in order to verify the relationship between PBQ and the maternal variables (postnatal depressive symptoms, anxiety, and stress), and Spearman’s correlation coefficient for socio-demographic characteristics and the child’s characteristics variables.
- The second set of analyses included examining the predictors of maternal postpartum bonding; thus, we calculated the linear regression between postpartum bonding and those variables, which were statistically significant in the first phase of the correlation analysis.
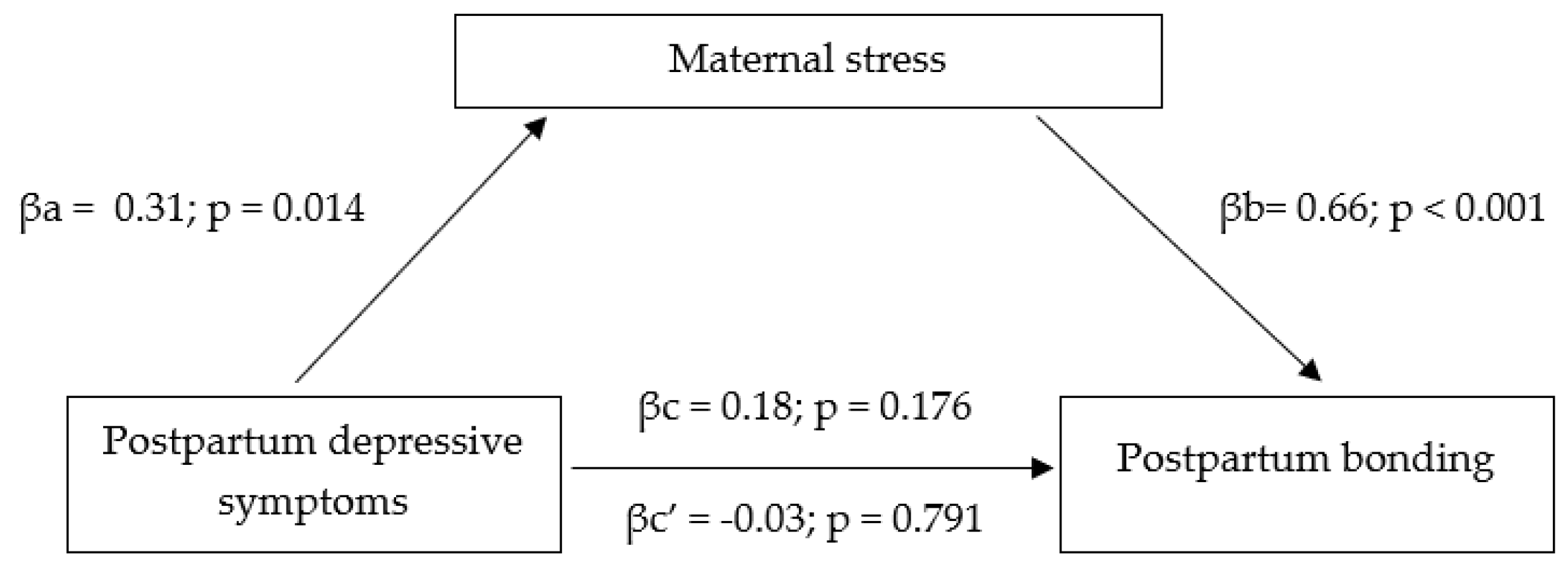
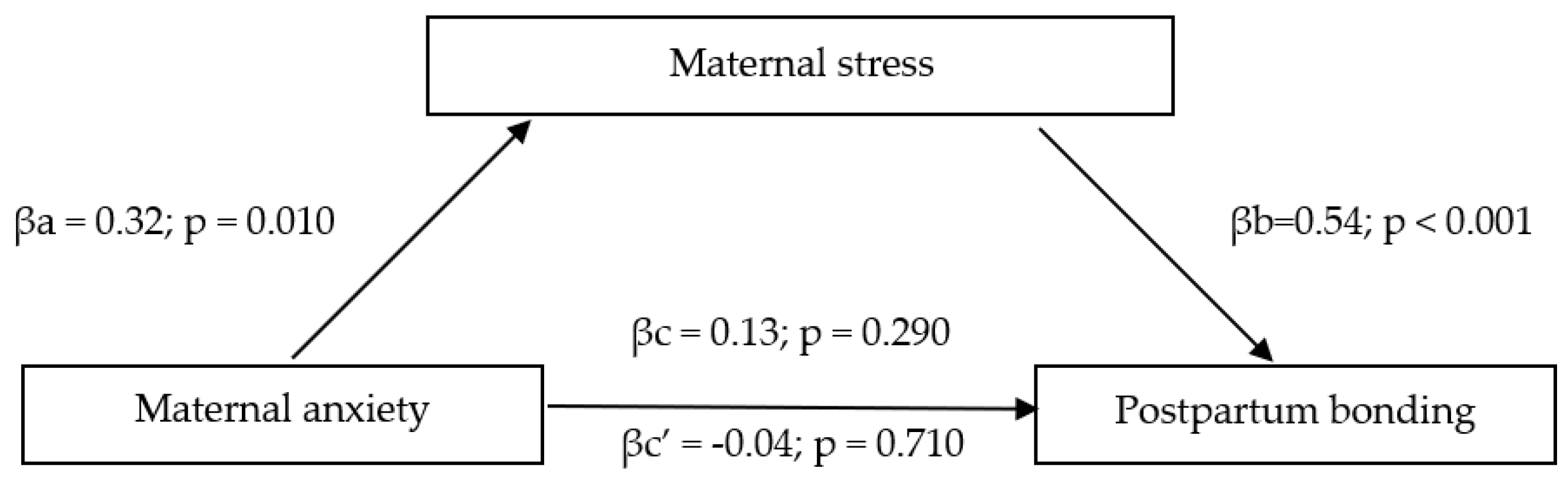
- To test the mediating models, we followed Model 4 of the PROCESS macro for SPSS [61]. We used 5000 bootstrap resamples to generate CIs for the indirect effect of maternal postpartum depression on maternal postpartum bonding via maternal stress and for the indirect effect of maternal anxiety on maternal postpartum bonding via maternal stress.
- Finally, we undertook a moderator analysis following Model 1 of the PROCESS macro for SPSS [61]. This analysis included maternal postpartum bonding and those variables that were statistically significant were also statistically significant in the first phase.
3. Results
3.1. The Characteristics of the Study Group
3.2. Maternal Postpartum Bonding Scores after Preterm Birth
3.3. Maternal Stress, Anxiety, and Depressive Symptoms Scores
3.4. Correlations between Maternal Postpartum Bonding and Study Variables
3.5. Predictors of Maternal Postpartum Bonding
3.6. Mediating Models
3.7. Moderators of the Relationship between Maternal Postpartum Bonding and Maternal Stress
4. Discussion
4.1. What Is the Maternal Postpartum Bonding Score among Mothers after Preterm Birth?
4.2. What Are the Mothers’ Scores in Relation to Maternal Stress, Anxiety, and Depression Symptoms?
4.3. Is Postpartum Bonding Associated with Maternal Mental Health (Depression Symptoms, Anxiety, and Stress)?
4.4. Is Postpartum Bonding Associated with a Child’s Characteristics (Gestational Age, Birth Weight, and Final Apgar Score)?
4.5. Is Maternal Postpartum Bonding Associated with Socio-Demographical Variables (Education Level, Age, and Number of Children in the Household)?
4.6. Implication for Clinical Practice
4.7. Implication for Further Research
4.8. Strengths
4.9. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended 14 October 1976. Acta Obstet. Gynecol. Scand. 1977, 56, 247–253. [Google Scholar]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Blencowe, H.; Cousens, S.; Chou, D.; Oestergaard, M.; Say, L.; Moller, A.-B.; Kinney, M.; Lawn, J. The born too soon preterm birth action group. The global epidemiology of 15 million preterm births. Reprod. Health 2013, 10, S2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chawanpaiboon, S.; Vogel, J.P.; Moller, A.-B.; Lumbiganon, P.; Petzold, M.; Hogan, D.; Landoulsi, S.; Jampathong, N.; Kongwattanakul, K.; Laopaiboon, M.; et al. Global, regional, and national estimates of levels of preterm birth in 2014: A systematic review and modelling analysis. Lancet Glob. Health 2018, 7, e37–e46. [Google Scholar] [CrossRef] [Green Version]
- Chang, H.H.; Larson, J.; Blencowe, H.; Spong, C.Y.; Howson, C.P.; Cairns-Smith, S.; Lackritz, E.M.; Lee, S.K.; Mason, E.; Serazin, A.C.; et al. Preventing preterm births: Analysis of trends and potential reductions with interventions in 39 countries with very high human development index. Lancet 2012, 381, 223–234. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Johnson, H.L.; Cousens, S.; Perin, J.; Scott, S.; Lawn, J.; Rudan, I.; Campbell, H.; Cibulskis, R.; Li, M.; et al. Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet 2012, 379, 2151–2161. [Google Scholar] [CrossRef]
- Saigal, S.; Doyle, L. Preterm birth 3. An overview of mortality and sequelae of preterm birth form infancy to adulthood. Lancet 2008, 371, 261–269. [Google Scholar] [CrossRef]
- Underwood, M.; Danielsen, B.; Gilbert, W.M. Cost, causes and rates of rehospitalization of preterm infants. J. Perinatol. 2007, 27, 614–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manuck, T.A.; Rice, M.M.; Bailit, J.L.; Grobman, W.A.; Reddy, U.M.; Wapner, R.; Thorp, J.M.; Caritis, S.N.; Prasad, M.; Tita, A.; et al. Preterm neonatal morbidity and mortality by gestational age: A contemporary cohort. Am. J. Obstet. Gynecol. 2016, 215, 103.e1–103.e14. [Google Scholar] [CrossRef] [Green Version]
- Synnes, A.; Hicks, M. Neurodevelopmental outcomes of preterm children at school age and beyond. Clin. Perinatol. 2018, 45, 393–408. [Google Scholar] [CrossRef] [PubMed]
- Vohr, B.R. Neurodevelopmental outcomes of extremely preterm infants. Clin. Perinatol. 2014, 41, 241–255. [Google Scholar] [CrossRef] [PubMed]
- Vogel, J.P.; Chawanpaiboon, S.; Moller, A.-B.; Watananirun, K.; Bonet, M.; Lumbiganon, P. The global epidemiology of preterm birth. Best Pr. Res. Clin. Obstet. Gynaecol. 2018, 52, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.D.; Mulder, R.T.; Darlow, B.A. Parental stress in the NICU: The influence of personality, psychological, pregnancy and family factors. Pers. Ment. Health 2007, 1, 40–50. [Google Scholar] [CrossRef]
- Ionio, C.; Colombo, C.; Brazzoduro, V.; Mascheroni, E.; Confalonieri, E.; Castoldi, F.; Lista, G. Mothers and fathers in NICU: The impact of preterm birth on parental distress. Eur. J. Psychol. 2016, 12, 604–621. [Google Scholar] [CrossRef] [Green Version]
- Jotzo, M.; Poets, C.F. Helping parents cope with the trauma of premature birth: An evaluation of a trauma-preventive psychological intervention. Pediatrics 2005, 115, 915–919. [Google Scholar] [CrossRef] [PubMed]
- Cook, N.; Ayers, S.; Horsch, A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: A systematic review. J. Affect. Disord. 2018, 225, 18–31. [Google Scholar] [CrossRef]
- Brunson, E.; Thierry, A.; Ligier, F.; Vulliez-Coady, L.; Novo, A.; Rolland, A.-C.; Eutrope, J. Prevalences and predictive factors of maternal trauma through 18 months after premature birth: A longitudinal, observational and descriptive study. PLoS ONE 2021, 16, e0246758. [Google Scholar] [CrossRef]
- Holditch-Davis, D.; Bartlett, T.R.; Blickman, A.L.; Miles, M.S. Posttraumatic stress symptoms in mothers of premature infants. J. Obstet. Gynecol. Neonatal Nurs. 2003, 32, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Eduardo, J.A.F.D.P.; de Rezende, M.G.; Menezes, P.; Del-Ben, C.M. Preterm birth as a risk factor for postpartum depression: A systematic review and meta-analysis. J. Affect. Disord. 2019, 259, 392–403. [Google Scholar] [CrossRef]
- Grekin, R.; O’Hara, M.W. Prevalence and risk factors of postpartum posttraumatic stress disorder: A meta-analysis. Clin. Psychol. Rev. 2014, 34, 389–401. [Google Scholar] [CrossRef]
- Vigod, S.N.; Villegas, L.; Dennis, C.-L.; E Ross, L. Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: A systematic review. BJOG Int. J. Obstet. Gynaecol. 2010, 117, 540–550. [Google Scholar] [CrossRef] [PubMed]
- Singer, L.T.; Salvator, A.; Guo, S.; Collin, M.; Lilien, L.; Baley, J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA 1999, 281, 799–805. [Google Scholar] [CrossRef] [Green Version]
- Alkozei, A.; McMahon, E.; Lahav, A. Stress levels and depressive symptoms in NICU mothers in the early postpartum period. J. Matern. Neonatal Med. 2014, 27, 1738–1743. [Google Scholar] [CrossRef] [PubMed]
- Abidin, R.R. The determinants of parenting behavior. J. Clin. Child Psychol. 1992, 21, 407–412. [Google Scholar] [CrossRef]
- Flacking, R.; Lehtonen, L.; Thomson, G.; Axelin, A.; Ahlqvist, S.; Moran, V.H.; Ewald, U.; Dykes, F. The SCENE group closeness and separation in neonatal intensive care. Acta Paediatr. 2012, 101, 1032–1037. [Google Scholar] [CrossRef] [Green Version]
- Bieleninik, Ł. Dzieci Urodzone Przedwcześnie w Percepcji Matek (Mothers’ Perception of Prematurely Born Children in the Period of the Early Childhood); Harmionia Universalis: Gdańsk, Poland, 2012. [Google Scholar]
- Gondwe, K.W.; Brandon, D.; Yang, Q.; Malcom, W.F.; Small, M.J.; Holditch-Davis, D. Emotional distress in mothers of early-preterm infants, late-preterm infants, and full-term infants in Malawi. Nurs. Outlook 2019, 68, 94–103. [Google Scholar] [CrossRef]
- Demier, R.L.; Hynan, M.T.; Hatfield, R.F.; Varner, M.; Harris, H.B.; Manniello, R.L. A measurement model of perinatal stressors: Identifying risk for postnatal emotional distress in mothers of high-risk infants. J. Clin. Psychol. 1999, 56, 89–100. [Google Scholar] [CrossRef]
- Kinsey, C.B.; Hupcey, J.E. State of the science of Maternal-Infant bonding: A principle-based concept analysis. Midwifery 2013, 29, 1314–1320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakano, M.; Upadhyaya, S.; Chudal, R.; Skokauskas, N.; Luntamo, T.; Sourander, A.; Kaneko, H. Risk factors for impaired maternal bonding when infants are 3 months old: A longitudinal population based study from Japan. BMC Psychiatry 2019, 19, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chandra, P.S.; Desai, G.; Reddy, D.; Thippeswamy, H.; Saraf, G. The establishment of a mother-baby inpatient psychiatry unit in India: Adaptation of a Western model to meet local cultural and resource needs. Indian J. Psychiatry 2015, 57, 290–294. [Google Scholar] [CrossRef]
- Kantrowitz-Gordon, I. Expanded care for women and families after preterm birth. J. Midwifery Women’s Health 2013, 58, 158–166. [Google Scholar] [CrossRef]
- Aagaard, H.; Hall, E.O. Mothers’ experiences of having a preterm infant in the neonatal care unit: A meta-synthesis. J. Pediatric Nurs. 2008, 23, e26–e36. [Google Scholar] [CrossRef] [PubMed]
- Trumello, C.; Candelori, C.; Cofini, M.; Cimino, S.; Cerniglia, L.; Paciello, M.; Babore, A. Mothers’ depression, anxiety, and mental representations after preterm birth: A study during the infant’s hospitalization in a Neonatal Intensive Care Unit. Front. Public Health 2018, 6, 359. [Google Scholar] [CrossRef] [PubMed]
- Khemakhem, R.; Bourgou, S.; Selmi, I.; Azzabi, O.; Belhadj, A.; Siala, N. Preterm birth, mother psychological state and mother infant bonding. Tunis. Med. 2020, 98, 992–997. [Google Scholar]
- Hall, R.A.S.; Hoffenkamp, H.N.; Tooten, A.; Braeken, J.; Vingerhoets, A.J.J.M.; Van Bakel, H.J.A. Child-rearing history and emotional bonding in parents of preterm and full-term infants. J. Child Fam. Stud. 2014, 24, 1715–1726. [Google Scholar] [CrossRef]
- Soltis, J. The signal functions of early infant crying. Behav. Brain Sci. 2004, 27, 443–490. [Google Scholar] [CrossRef]
- Müller-Nix, C.; Ansermet, F. Prematurity, risk and protective factors. In Handbook of Infant Mental Health; Zeanah, C.H., Ed.; The Guilford Press: New York, NY, USA, 2009; pp. 180–196. [Google Scholar]
- Hoffenkamp, H.N.; Tooten, A.; Hall, R.A.; Croon, M.A.; Braeken, J.; Winkel, F.W.; Vingerhoets, A.J.; van Bakel, H.J. The impact of premature childbirth on parental bonding. Evol. Psychol. 2012, 10, 542–561. [Google Scholar] [CrossRef]
- Goldberg, S.; DiVitto, B. Parenting children born preterm. In Handbook of Parenting: Children and Parenting, 2nd ed.; Bornstein, M.H., Ed.; Lawrence Erlbaum Associate: Mahwah, NJ, USA, 2002; pp. 329–354. [Google Scholar]
- Duley, L.; Uhm, S.; Oliver, S. Top 15 UK research priorities for preterm birth. Lancet 2014, 383, 2041–2042. [Google Scholar] [CrossRef]
- Agnafors, S.; Bladh, M.; Svedin, C.G.; Sydsjö, G. Mental health in young mothers, single mothers and their children. BMC Psychiatry 2019, 19, 112. [Google Scholar] [CrossRef] [Green Version]
- Sauer, M.V. Reproduction at an advanced maternal age and maternal health. Fertil. Steril. 2015, 103, 1136–1143. [Google Scholar] [CrossRef]
- Heath, D.T.; Mckenry, P.C.; Leigh, G.K. The consequences of adolescent parenthood on men’s depression, parental satisfaction, and fertility in adulthood. J. Soc. Serv. Res. 1995, 20, 127–148. [Google Scholar] [CrossRef]
- Hodgkinson, S.; Beers, L.; Southammakosane, C.; Lewin, A. Addressing the mental health needs of pregnant and parenting adolescents. Pediatrics 2013, 133, 114–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bieleninik, Ł.; Lutkiewicz, K.; Jurek, P.; Bidzan, M. Paternal postpartum bonding and its predictors in the early postpartum period: Cross-sectional study in a polish cohort. Front. Psychol. 2021, 12, 1112. [Google Scholar] [CrossRef]
- Lutkiewicz, K.; Bieleninik, Ł.; Cieślak, M.; Bidzan, M. Maternal-infant bonding and its relationships with maternal depressive symptoms, stress and anxiety in the early postpartum period in a Polish sample. Int. J. Environ. Res. Public Health 2020, 17, 5427. [Google Scholar] [CrossRef]
- Brockington, I.F.; Oates, J.; George, S.; Turner, D.; Vostanis, P.; Sullivan, M.; Loh, C.; Murdoch, C. A screening questionnaire for mother-infant bonding disorders. Arch. Women’s Ment. Health 2001, 3, 133–140. [Google Scholar] [CrossRef]
- Brockington, I.F.; Aucamp, H.M.; Fraser, C. Severe disorders of the mother-infant relationship: Definitions and frequency. Arch. Women’s Ment. Health 2006, 9, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Wittkowski, A.; Wieck, A.; Mann, S. An evaluation of two bonding questionnaires: A comparison of the mother-to-infant bonding scale with the postpartum bonding questionnaire in a sample of primiparous mothers. Arch. Women’s Ment. Health 2007, 10, 171–175. [Google Scholar] [CrossRef]
- Wittkowski, A.; Williams, J.; Wieck, A. An examination of the psychometric properties and factor structure of the post-partum bonding questionnaire in a clinical inpatient sample. Br. J. Clin. Psychol. 2010, 49, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [Green Version]
- Bielawska-Batorowicz, E. Determinanty Spostrzegania Dziecka Przez Rodziców w Okresie Poporodowym; Wydawnictwo Uniwersytetu Łódzkiego: Łódź, Poland, 1995. [Google Scholar]
- Marshall, J.; Bethell, K. Edinburgh Postnatal Depression Scale (EPDS): Translated Versions; State Perinatal Mental Health Reference Group: Perth, Australia, 2006.
- Kossakowska, K. Edynburska Skala Depresji Poporodowej Właściwości Psychometryczne i Charakterystyka. Folia Psychol. 2013, 17, 39–50. [Google Scholar]
- Chrzan-Dętkoś, M.; Walczak-Kozłowska, T. How do new mothers perceive screening for perinatal depression? Health Psychol. Rep. 2021, 9, 207–216. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [Green Version]
- Johnson, S.U.; Ulvenes, P.G.; Øktedalen, T.; Hoffart, A. Psychometric properties of the general anxiety disorder 7-item (GAD-7) scale in a heterogeneous psychiatric sample. Front. Psychol. 2019, 10, 1713. [Google Scholar] [CrossRef] [Green Version]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef]
- Berry, J.O.; Jones, W.H. The parental stress scale: Initial psychometric evidence. J. Soc. Pers. Relatsh. 1995, 12, 463–472. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Nima, A.A.; Rosenberg, P.; Archer, T.; Garcia, D. Anxiety, affect, self-esteem, and stress: Mediation and moderation effects on depression. PLoS ONE 2013, 8, e73265. [Google Scholar] [CrossRef]
- Borghini, A.; Pierrehumbert, B.; Miljkovitch, R.; Muller-Nix, C.; Forcada-Guex, M.; Ansermet, F. Mother’s attachment representations of their premature infant at 6 and 18 months after birth. Infant Ment. Health J. 2006, 27, 494–508. [Google Scholar] [CrossRef] [PubMed]
- Korja, R.; Latva, R.; Lehtonen, L. The effects of preterm birth on mother-infant interaction and attachment during the infant’s first two years. Acta Obstet. Gynecol. Scand. 2012, 91, 164–173. [Google Scholar] [CrossRef]
- Medina, I.M.F.; Granero-Molina, J.; Fernández-Sola, C.; Hernández-Padilla, J.M.; Avila, M.C.; Rodríguez, M.D.M.L. Bonding in neonatal intensive care units: Experiences of extremely preterm infants’ mothers. Women Birth 2018, 31, 325–330. [Google Scholar] [CrossRef]
- De Cock, E.S.; Henrichs, J.; Klimstra, T.A.; Maas, A.B.; Vreeswijk, C.M.; Meeus, W.H.; van Bakel, H.J. Longitudinal associations between parental bonding, parenting stress, and executive functioning in toddlerhood. J. Child Fam. Stud. 2017, 26, 1723–1733. [Google Scholar] [CrossRef] [Green Version]
- Bailhache, M.; Doyle, O.; Salmi, L.; McDonnell, T. Does maternal attachment to her infant mediate the link between perceptions of infant crying at 6 months and parenting stress at 24 months? A structural equation modelling approach. Child Care Health Dev. 2019, 45, 540–550. [Google Scholar] [CrossRef]
- Tichelman, E.; Westerneng, M.; Witteveen, A.B.; Van Baar, A.L.; Van Der Horst, H.E.; De Jonge, A.; Berger, M.Y.; Schellevis, F.G.; Burger, H.; Peters, L.L. Correlates of prenatal and postnatal mother-to-infant bonding quality: A systematic review. PLoS ONE 2019, 14, e0222998. [Google Scholar] [CrossRef] [Green Version]
- Nordahl, D.; Rognmo, K.; Bohne, A.; Landsem, I.P.; Moe, V.; Wang, C.E.A.; Høifødt, R.S. Adult attachment style and maternal-infant bonding: The indirect path of parenting stress. BMC Psychol. 2020, 8, 58. [Google Scholar] [CrossRef] [PubMed]
- Lehnig, F.; Nagl, M.; Stepan, H.; Wagner, B.; Kersting, A. Associations of postpartum mother-infant bonding with maternal childhood maltreatment and postpartum mental health: A cross-sectional study. BMC Pregnancy Childbirth 2019, 19, 278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Çalışır, H.; Karaçam, Z. Factors associated with parenting behavior of mothers in the early postpartum period in Turkey. Nurs. Health Sci. 2011, 13, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Korucku, O. Identification of factors affecting mother-infant bonding in advanced maternal age. Lupine Online J. Nurs. Health Care 2018, 1, 102. [Google Scholar]
- Feldman, R. Sensitive periods in human social development: New insights from research on oxytocin, synchrony, and high-risk parenting. Dev. Psychopathol. 2015, 27, 369–395. [Google Scholar] [CrossRef]
- Statistics Poland. Demographic Year Book of Poland; Statistics Poland: Warszawa, Poland, 2020.
- Statistics Poland. D.S.D. Demographic Situation of Poland up to 2017. Births and Fertility, 2018; Statistics Poland: Warszawa, Poland, 2018.
- Trombetta, T.; Giordano, M.; Santoniccolo, F.; Vismara, L.; Della Vedova, A.M.; Rollè, L. Pre-natal attachment and parent-to-infant attachment: A systematic review. Front. Psychol. 2021, 12, 664. [Google Scholar] [CrossRef] [PubMed]
- Wittkowski, A.; Vatter, S.; Muhinyi, A.; Garrett, C.; Henderson, M. Measuring bonding or attachment in the parent-infant-relationship: A systematic review of parent-report assessment measures, their psychometric properties and clinical utility. Clin. Psychol. Rev. 2020, 82, 101906. [Google Scholar] [CrossRef] [PubMed]
- Perrelli, J.G.A.; Zambaldi, C.F.; Cantilino, A.; Sougey, E.B. Instrumentos de Avaliação do Vínculo Entre Mãe e bebê; Revista Paulista de Pediatria; Orgao Oficial da Sociedade de Pediatria de Sao Paulo: Sao Paulo, Brazil, 2014; pp. 257–265. [Google Scholar]
| Demographic Variable | Mothers | |
|---|---|---|
| n | % | |
| Marital status | ||
| Single | 0 | 0 |
| Married | 58 | 80.6 |
| Partnership | 12 | 16.7 |
| Divorced | 1 | 1.4 |
| Separated | 0 | 0 |
| Widowed | 0 | 0 |
| Other | 0 | 0 |
| Missing | 1 | 1.4 |
| Work situation | ||
| Employed full-time | 51 | 70.8 |
| Employed part-time | 2 | 2.8 |
| Self-employed | 7 | 9.7 |
| Student full-time | 0 | 0 |
| Student part-time | 1 | 1.4 |
| Stay-at-home parent | 5 | 6.9 |
| Unemployed and seeking work | 0 | 0 |
| Missing | 6 | 8.2 |
| Education level | ||
| Primary/elementary or less | 1 | 1.4 |
| Secondary school but not completed | 2 | 2.8 |
| Secondary school graduate | 13 | 18.1 |
| University/college but not completed | 0 | 0 |
| University degree (Bachelors or equivalent) | 12 | 16.7 |
| University degree (Masters or equivalent) | 41 | 56.9 |
| University degree (PhD or equivalent) | 2 | 2.8 |
| Missing | 1 | 1.4 |
| Number of children in the family | ||
| One | 21 | 29.2 |
| Two | 31 | 43.1 |
| Three | 13 | 18.1 |
| Four | 3 | 4.2 |
| Five | 2 | 2.8 |
| Six | 1 | 1.4 |
| Missing | 1 | 1.4 |
| Type of birth | ||
| Vaginal birth | 26 | 36.1 |
| Caesaren birth | 46 | 63.9 |
| Sex of the child | ||
| Boy | 32 | 44.4 |
| Girl | 40 | 55.6 |
| APGAR | ||
| 5 | 3 | 4.2 |
| 6 | 4 | 5.6 |
| 7 | 6 | 8.3 |
| 8 | 15 | 20.8 |
| 9 | 14 | 19.4 |
| 10 | 17 | 23.6 |
| Missing | 13 | 18.1 |
| PBQ | N | M | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Extremely preterm (<28 weeks) | 3 | 7.33 | 3.21 | 5 | 11 |
| Very preterm (28 to 31 weeks and 6 days) | 7 | 9.00 | 8.26 | 1 | 26 |
| Moderate preterm (32 to 33 weeks and 6 days) | 15 | 8.00 | 6.52 | 1 | 21 |
| Late preterm (34 to 36 weeks and 6 days) | 47 | 7.70 | 7.55 | 0 | 41 |
| Variable | N | M | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Postpartum Bonding (PBQ) | 72 | 7.87 | 7.18 | 0 | 41 |
| Depressive Symptoms (EPDS) | 67 | 8.83 | 4.73 | 1 | 21 |
| Anxiety (GAD-7) | 66 | 13.60 | 5.35 | 7 | 28 |
| Parental Stress (PSS) | 66 | 32.81 | 7.80 | 19 | 58 |
| EPDS | GAD | PSS | |
|---|---|---|---|
| PBQ average scores | 0.227 | 0.168 | 0.696 ** |
| Variable | PBQ |
|---|---|
| Gestational age | −0.043 |
| Birth weight | −0.055 |
| APGAR scale | 0.052 |
| Maternal age | 0.244 * |
| Educational level | 0.386 ** |
| Number of children | 0.317 ** |
| Predictor | β | B | SE | p | t |
|---|---|---|---|---|---|
| Parental Stress (PSS) | 0.667 | 0.633 | 0.086 | 0.001 | 7.402 |
| Maternal age | 0.096 | 0.147 | 0.140 | 0.298 | 1.050 |
| Constant value | −17.493 | 4.782 | 0.001 | −3.658 |
| Predictor × Moderator | Dependent Variable | β | SE | t | p | LL | UL |
|---|---|---|---|---|---|---|---|
| Maternal stress × maternal age | 0.032 | 0.022 | 1.47 | 0.14 | −0.011 | 0.077 | |
| Maternal stress × educational level | postpartum bonding | 0.068 | 0.077 | 0.89 | 0.37 | −0.085 | 0.222 |
| Maternal stress × number of children | −0.014 | 0.062 | −0.202 | 0.84 | −0.152 | 0.124 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bieleninik, Ł.; Lutkiewicz, K.; Cieślak, M.; Preis-Orlikowska, J.; Bidzan, M. Associations of Maternal-Infant Bonding with Maternal Mental Health, Infant’s Characteristics and Socio-Demographical Variables in the Early Postpartum Period: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 8517. https://doi.org/10.3390/ijerph18168517
Bieleninik Ł, Lutkiewicz K, Cieślak M, Preis-Orlikowska J, Bidzan M. Associations of Maternal-Infant Bonding with Maternal Mental Health, Infant’s Characteristics and Socio-Demographical Variables in the Early Postpartum Period: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(16):8517. https://doi.org/10.3390/ijerph18168517
Chicago/Turabian StyleBieleninik, Łucja, Karolina Lutkiewicz, Mariusz Cieślak, Joanna Preis-Orlikowska, and Mariola Bidzan. 2021. "Associations of Maternal-Infant Bonding with Maternal Mental Health, Infant’s Characteristics and Socio-Demographical Variables in the Early Postpartum Period: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 16: 8517. https://doi.org/10.3390/ijerph18168517
APA StyleBieleninik, Ł., Lutkiewicz, K., Cieślak, M., Preis-Orlikowska, J., & Bidzan, M. (2021). Associations of Maternal-Infant Bonding with Maternal Mental Health, Infant’s Characteristics and Socio-Demographical Variables in the Early Postpartum Period: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(16), 8517. https://doi.org/10.3390/ijerph18168517







