Sagittal Integral Morphotype of Competitive Amateur Athletes and Its Potential Relation with Recurrent Low Back Pain
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Self-Administered Questionnaire
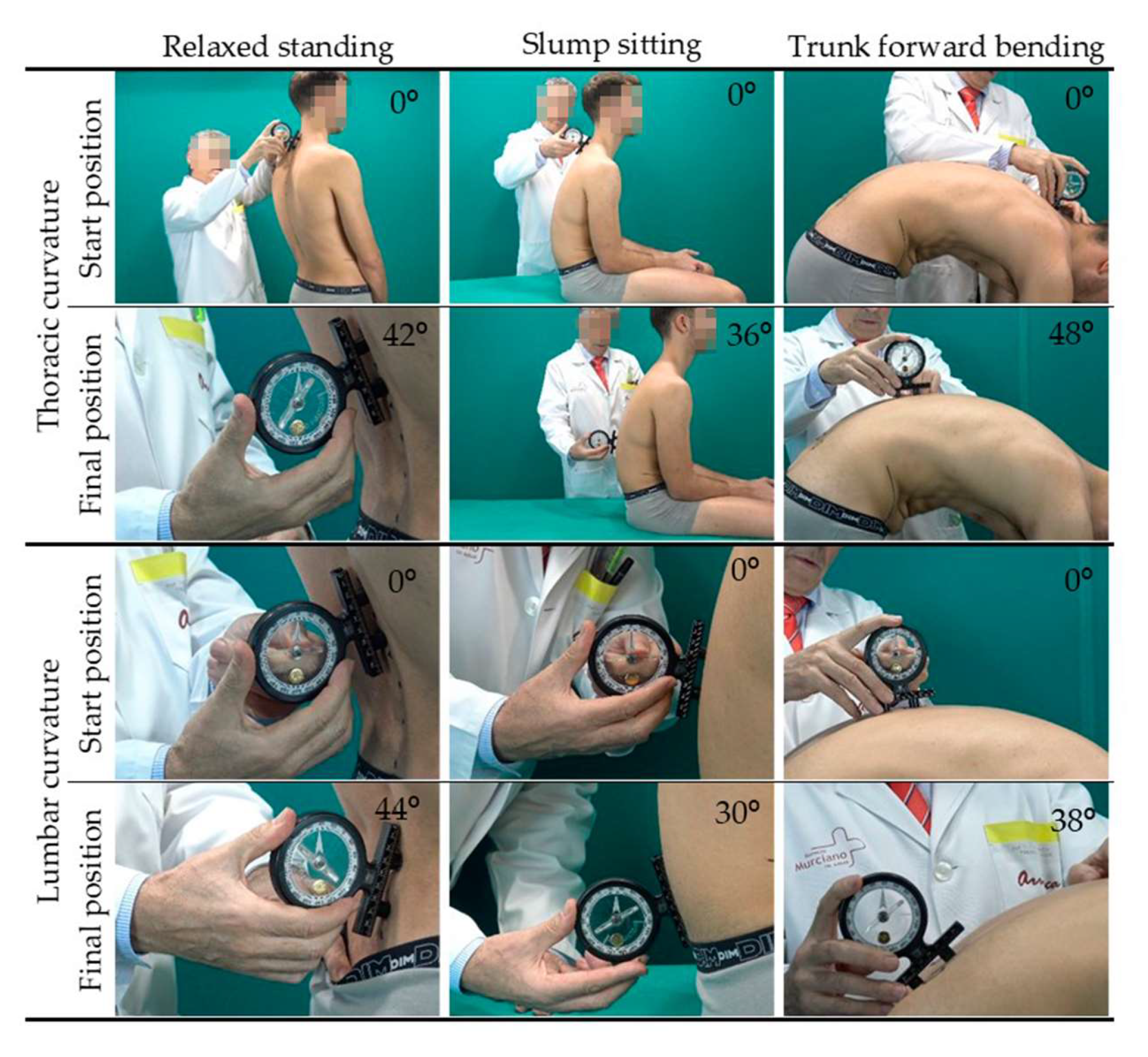
2.4. Sagittal Integrative Morphotype Assessment Procedure
2.5. Sagittal Pelvic Position Assessment Procedure
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kapandji, A. Fisiología Articular III: Miembro Inferior; Medica Panamericana: Madrid, Spain, 2007; ISBN 9788498350470. [Google Scholar]
- McGill, S. Low Back Disorders: Evidence-Based Prevention and Rehabilitation, 3rd ed.; Human Kinetics Australia: Lower Mitcham, Australia, 2015; ISBN 9781492585565. [Google Scholar]
- Kendall, F.; McCreary, E.; Provance, P.; Rodgers, M.; Romani, W. Muscles: Testing and Function with Posture and Pain; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2005; ISBN 0781747805. [Google Scholar]
- Chromik, K.; Burdukiewicz, A.; Pietraszewska, J.; Stachoń, A.; Wolański, P.; Goliński, D. Characteristics of anteroposterior curvatures of the spine in soccer and futsal players. Hum. Mov. 2017, 18, 49–54. [Google Scholar] [CrossRef]
- Wodecki, P.; Guigui, P.; Hanotel, M.; Cardinne, L.; Deburge, A. Sagittal alignment of the spine: Comparison between soccer players and subjects without sports activities. Rev. Chir. Orthop. Reparatrice L’appareil Mot. 2002, 88, 328–336. [Google Scholar]
- Ginés-Díaz, A.; Martinez-Romero, M.; Cejudo, A.; Aparicio-Sarmiento, A.; Sainz de Baranda, P. Sagittal Spinal Morphotype Assessment in Dressage and Show Jumping Riders Physical. J. Sport Rehabil. 2019, 29, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Grabara, M. Comparison of posture among adolescent male volleyball players and non-athletes. Biol. Sport 2015, 32, 79–85. [Google Scholar] [CrossRef]
- Rajabi, R.; Doherty, P.; Goodarzi, M.; Hemayattalab, R. Comparison of thoracic kyphosis in two groups of elite Greco-Roman and freestyle wrestlers and a group of non-athletic participants. Br. J. Sports Med. 2008, 42, 229–232. [Google Scholar] [CrossRef]
- Rajabi, R.; Mobarakabadi, L.; Alizadhen, H.; Hendrick, P. Thoracic kyphosis comparisons in adolescent female competitive field hockey players and untrained controls. J. Sports Med. Phys. Fit. 2012, 52, 545–550. [Google Scholar]
- Sainz de Baranda, P.; Cejudo, A.; Moreno-Alcaraz, V.; Martinez-Romero, M.; Aparicio-Sarmiento, A.; Santonja, F. Sagittal spinal morphotype assessment in 8 to 15 years old Inline Hockey players. PeerJ 2020, 8, e8229. [Google Scholar] [CrossRef] [PubMed]
- Grabara, M. Sagittal spinal curvatures in adolescent male basketball players and non-training individuals–a two-year study. Sci. Sports 2016, 31, e147–e153. [Google Scholar] [CrossRef]
- Lichota, M.; Plandowska, M.; Mil, P. The Shape of Anterior-Posterior Curvatures of the Spine in Athletes Practising Selected Sports. Pol. J. Sport Tour. 2011, 2, 112–121. [Google Scholar] [CrossRef]
- Boldori, L.; Da Soldá, M.; Marelli, A. Anomalies of the trunk. An analysis of their prevalence in young athletes. Minerva Pediatrica 1999, 51, 259–264. [Google Scholar]
- Kums, T.; Ereline, J.; Gapeyeva, H.; Pääsuke, M. Spinal curvature and trunk muscle tone in rhytmic gymnasts and untrained girls. J. Back Musculoskelet. Rehabil. 2007, 20, 87–95. [Google Scholar] [CrossRef]
- Sanz-Mengibar, J.; Sainz de Baranda, P.; Santonja-Medina, F. Training intensity and sagittal curvature of the spine in male and female artistic gymnasts. J. Sports Med. Phys. Fit. 2018, 58, 465–471. [Google Scholar] [CrossRef]
- Wojtys, E.; Ashton-Miller, J.; Huston, L.; Moga, P. The association between athletic training time and the sagittal curvature of the immature spine. Am. J. Sports Med. 2000, 28, 490–498. [Google Scholar] [CrossRef]
- Sainz de Baranda, P.; Santonja-Medina, F.; Rodríguez-Iniesta, M. Training Time and Sagittal Curvature of the Spine in Trampolin Gymnasts. Rev. Int. Med. Cienc. Act. Física Deporte 2010, 10, 521–536. Available online: http://cdeporte.rediris.es/revista/revista40/artentrenamiento169.htm (accessed on 11 June 2021).
- Hobbs, S.J.; Baxter, J.; Broom, L.; Rossell, L.-A.; Sinclair, J.; Clayton, H.M. Posture, Flexibility and Grip Strength in Horse Riders. J. Hum. Kinet. 2014, 42, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Alricsson, M.; Björklund, G.; Cronholm, M.; Olsson, O.; Viklund, P.; Svantesson, U. Spinal alignment, mobility of the hip and thoracic spine and prevalence of low back pain in young elite cross-country skiers. J. Exerc. Rehabil. 2016, 12, 21. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dionne, C.; Dunn, K.; Croft, P.; Nachemson, A.; Buchbinder, R.; Walker, B.; Wyatt, M.; Cassidy, J.; Rossignol, M.; Leboeuf-Yde, C.; et al. A Consensus Approach Toward the Standardization of Back Pain Definitions for Use in Prevalence Studies. Spine 2008, 33, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Foss, I.; Holme, I.; Bahr, R. The Prevalence of Low Back Pain Among Former Elite Cross-Country Skiers, Rowers, Orienteerers, and Nonathletes A 10-Year Cohort Study. Am. J. Sports Med. 2012, 40, 2610–2616. [Google Scholar] [CrossRef]
- Christie, H.; Kumar, S.; Warren, S. Postural Aberrations in Low Back Pain. Arch. Phys. Med. Rehabil. 1995, 76, 218–224. [Google Scholar] [CrossRef]
- Salminen, J.; Oksanen, A.; Mäki, P.; Pentti, J.; Kujala, U. Leisure time physical activity in the young. Correlation with low-back pain, spinal mobility and trunk muscle strength in 15-year-old school children. Int. J. Sports Med. 1993, 14, 406–410. [Google Scholar] [CrossRef]
- Roncarati, A.; McMullen, W. Correlates of low back pain in a general population sample: A multidisciplinary perspective. J. Manip. Physiol. Ther. 1988, 11, 158–164. [Google Scholar]
- Norton, B.; Sahrmann, S.; Van Dillen, L. Differences in measurements of lumbar curvature related to gender and low back pain. J. Orthop. Sports Phys. Ther. 2004, 34, 524–534. [Google Scholar] [CrossRef] [PubMed]
- Ohlén, G.; Wredmark, T.; Spangfort, E. Spinal sagittal configuration and mobility related to low-back pain in the female gymnast. Spine 1989, 14, 847–850. [Google Scholar] [CrossRef] [PubMed]
- Cejudo, A.; Gómez-Lozano, S.; Sainz de Baranda, P.; Vargas-Macías, A.; Santonja-Medina, F. Sagittal integral morphotype of female classical ballet dancers and predictors of sciatica and low back pain. Int. J. Environ. Res. Public Health 2021, 18, 5039. [Google Scholar] [CrossRef] [PubMed]
- Sivanich, A.; Shultz, J.; Raja, A. Chronic Lumbar Spondylolysis in an Adolescent Hockey Player. JBJS J. Orthop. Physician Assist. 2018, 6, e39. [Google Scholar] [CrossRef]
- Lawrence, K.; Elser, T.; Stromberg, R. Lumbar spondylolysis in the adolescent athlete. Phys. Ther. Sport 2016, 20, 56–60. [Google Scholar] [CrossRef]
- Congeni, J.; McCulloch, J.; Swanson, K. Lumbar spondylolysis. A study of natural progression in athletes. Am. J. Sports Med. 1997, 25, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Standaert, C.; Herring, S. Expert Opinion and Controversies in Sports and Musculoskeletal Medicine: The Diagnosis and Treatment of Spondylolysis in Adolescent Athletes. Arch. Phys. Med. Rehabil. 2007, 88, 537–540. [Google Scholar] [CrossRef]
- Been, E.; Kalichman, L. Lumbar lordosis. Spine J. 2014, 14, 87–97. [Google Scholar] [CrossRef]
- Katz, D.; Scerpella, T. Anterior and middle column thoracolumbar spine injuries in young female gymnasts: Report of seven cases and review of the literature. Am. J. Sports Med. 2003, 31, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Purcell, L.; Micheli, L. Low back pain in young athletes. Sports Health 2009, 1, 212–222. [Google Scholar] [CrossRef]
- Kruse, D.; Lemmen, B. Spine injuries in the sport of gymnastics. Curr. Sports Med. Rep. 2009, 8, 20–28. [Google Scholar] [CrossRef]
- Ambegaonkar, J.; Caswell, A.; Kenworthy, K.; Cortes, N.; Caswell, S. Lumbar lordosis in female collegiate dancers and gymnasts. Med. Probl. Perform. Artist. 2014, 29, 189–192. [Google Scholar] [CrossRef]
- Kobayashi, A.; Kobayashi, T.; Kato, K.; Higuchi, H.; Takagishi, K. Diagnosis of Radiographically Occult Lumbar Spondylolysis in Young Athletes by Magnetic Resonance Imaging. Am. J. Sports Med. 2013, 41, 169–176. [Google Scholar] [CrossRef]
- Bezuglov, E.; Lazarev, A.; Petrov, A.; Brodskaia, A.; Lyubushkina, A.; Kubacheva, K.; Achkasov, E.; Nikolenko, V. Asymptomatic Degenerative Changes in the Lumbar Spine Among Professional Soccer Players. Spine 2021, 46, 122–128. [Google Scholar] [CrossRef]
- Ball, J.; Harris, C.; Lee, J.; Vives, M. Lumbar Spine Injuries in Sports: Review of the Literature and Current Treatment Recommendations. Sports Med. Open 2019, 5, 26. [Google Scholar] [CrossRef]
- Santonja-Medina, F.; Collazo-Diéguez, M.; Martínez-Romero, M.; Rodríguez-Ferrán, O.; Aparicio-Sarmiento, A.; Cejudo, A.; Andújar, P.; Sainz De Baranda, P. Classification System of the Sagittal Integral Morphotype in Children from the ISQUIOS Programme (Spain). Int. J. Environ. Res. Public Health 2020, 17, 2467. [Google Scholar] [CrossRef]
- Korff, M. Studying the Natural History of Back Pain. Spine 1994, 19, 2041S–2046S. [Google Scholar] [CrossRef] [PubMed]
- Van Dillen, L.; Bloom, N.; Gombatto, S.; Susco, T. Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys. Ther. Sport 2008, 9, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Sainz de Baranda, P.; Rodríguez-Iniesta, M.; Ayala, F.; Santonja, F.; Cejudo, A. Determination of the criterion-related validity of hip joint angle test for estimating hamstring flexibility using a contemporary statistical approach. Clin. Sports Med. 2014, 24, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Santonja-Medina, F.; Santonja-Renedo, S.; Cejudo, A.; Ayala, F.; Ferrer, V.; Pastor, A.; Collazo-Diéguez, M.; Rodríguez-Ferrán, O.; Andújar, P.; Sainz de Baranda, P. Straight Leg Raise Test: Influence of Lumbosant© and Assistant Examiner in Hip, Pelvis Tilt and Lumbar Lordosis. Symmetry 2020, 12, 927. [Google Scholar] [CrossRef]
- Hopkins, W. Spreadsheets for Analysis of Validity and Reliability. Sportscience 2015, 19, 36–42. [Google Scholar]
- Sainz de Baranda, P.; Santonja-Medina, F.; Rodríguez-Iniesta, M. Valoración de la disposición sagital del raquis en gimnastas especialistas en trampolín. RICYDE Rev. Int. Cienc. Deporte 2009, 5, 21–33. [Google Scholar] [CrossRef]
- Lang-Tapia, M.; España-Romero, V.; Anelo, J.; Castillo, M. Differences on spinal curvature in standing position by gender, age and weight status using a noninvasive method. J. Appl. Biomech. 2011, 27, 143–150. [Google Scholar] [CrossRef]
- Sainz De Baranda, P.; Cejudo, A.; Martínez-Romero, M.; Aparicio-Sarmiento, A.; Rodríguez-Ferrán, O.; Collazo-Diéguez, M.; Hurtado-Avilés, J.; Andújar, P.; Santonja-Medina, F. Sitting Posture, Sagittal Spinal Curvatures and Back Pain in 8 to 12-Year-Old Children from the Region of Murcia (Spain): ISQUIOS Programme. Int. J. Environ. Res. Public Health Artic. 2020, 17, 2578. [Google Scholar] [CrossRef]
- Santonja-Medina, F.; Andújar, P.; Collazo, M.; Pastor, A.; Santonja-Renedo, F.; Martinez-Romero, M.T.; Aparicio-Sarmiento, A.; Cejudo, A.; de Baranda, P.S. Sagittal standing spinal alignment and back pain in 8 to 12-year-old children from the Region of Murcia, Spain: The ISQUIOS Program. J. Back Musculoskelet. Rehabil. 2020, 1–12. [Google Scholar] [CrossRef]
- Janda, V. Muscle Function Testing; Butterworth-Heinemann, Ed.; Elsevier: London, UK, 2013. [Google Scholar]
- Jang, H.; Hughes, L.; Oh, D.; Kim, S. Effects of corrective exercise for thoracic hyperkyphosis on posture, balance, and well-being in older women: A double-blind, group-matched design. J. Geriatr. Phys. Ther. 2019, 42, E17–E27. [Google Scholar] [CrossRef] [PubMed]
- Seidi, F.; Bayattork, M.; Minoonejad, H.; Andersen, L.; Page, P. Comprehensive corrective exercise program improves alignment, muscle activation and movement pattern of men with upper crossed syndrome: Randomized controlled trial. Sci. Rep. 2020, 10, 20688. [Google Scholar] [CrossRef] [PubMed]
- Chaléat-Valayer, E.; Mac-Thiong, J.; Paquet, J.; Berthonnaud, E.; Siani, F.; Roussouly, P. Sagittal spino-pelvic alignment in chronic low back pain. Eur. Spine J. 2011, 20, 634–640. [Google Scholar] [CrossRef] [PubMed]
- Janda, V. Evaluation of muscular imbalance. Rehabilitation of the spine: A practitioner’s manual. In Rehabillitation of the Spine: A Practitioner’s Manual; Liebenson, C.E., Ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 1996; pp. 97–112. [Google Scholar]
- Patel, K. Corrective Exercise: A Practical Approach: A Practical Approach; Routledge: London, UK, 2014; ISBN 0340889322. [Google Scholar]
- Wilke, H.; Neef, P.; Caimi, M.; Hoogland, T.; Claes, L. New In Vivo Measurements of Pressures in the Intervertebral Disc in Daily Life. Spine 1999, 24, 755–762. [Google Scholar] [CrossRef]
- Nachemson, A. Disc pressure measurements. Spine 1981, 6, 93–97. [Google Scholar] [CrossRef]
- Nixon, J. Intervertebral disc mechanics: A review. J. R. Soc. Med. 1986, 79, 100–104. [Google Scholar] [CrossRef]
- Moreno-Alcaraz, V.; Cejudo, A.; Sainz de Baranda, P. Injury types and frequency in Spanish inline hockey players. Phys. Ther. Sport 2020, 42, 91–99. [Google Scholar] [CrossRef]
- Krabak, B.; Kennedy, D. Functional rehabilitation of lumbar spine injuries in the athlete. Sports Med. Arthrosc. Rev. 2008, 16, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.; Cholewicki, J.; Van Dieën, J. Spinal Control: The Rehabilitation of Back Pain. State of the Art and Science; Elsevier/Churchill Livingstone: Edinburgh, UK, 2013. [Google Scholar]
- Fédération Équestre Internationale Dressage Tests|FEI. Available online: https://inside.fei.org/fei/your-role/organisers/dressage/tests (accessed on 11 June 2021).
- Grabara, M. Anteroposterior curvatures of the spine in adolescent athletes. J. Back Musculoskelet. Rehabil. 2014, 27, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Wand, B.; O’Connell, N. Chronic non-specific low back pain—Sub-groups or a single mechanism? BMC Musculoskelet. Disord. 2008, 9, 11. [Google Scholar] [CrossRef] [PubMed]
- Roffey, D.; Wai, E.; Bishop, P.; Kwon, B.; Dagenais, S. Causal assessment of awkward occupational postures and low back pain: Results of a systematic review. Spine J. 2010, 10, 89–99. [Google Scholar] [CrossRef]
- Nachemson, A.; Morris, J. In vivo measurements of intradiscal pressure: Discometry, a method for the determination of pressure in the lower lumbar discs. J. Bone Jt. Surg. 1964, 46, 1077–1092. [Google Scholar] [CrossRef]
| Variables | Male (N = 61) | Female (N = 33) | ES Hedges’ g 1 | Total 2 (N = 94) | |
|---|---|---|---|---|---|
| Years of training | 9.86 ± 7.69 | 5.77 ± 6.47 | Moderate (g = 0.56) | 8.34 ± 7.51 | |
| Training hours per week | 6.52 ± 2.74 | 6.50 ± 3.18 | Trivial (g = 0.00) | 6.52 ± 2.84 | |
| LH-SSP (degrees) | 103.43 ± 7.89 | 95.45 ± 9.17 | Large (g = 0.94) | 100.63 ± 9.15 | |
| LH-MTFP (degrees) | 100.26 ± 13.44 | 86.64 ± 15.70 | Large (g = 0.94) | 95.48 ± 15.62 | |
| Thoracic curvature (degrees) | RSP | 49.23 ± 8.15 | 44.94 ± 10.09 | Moderate (g = 0.47) | 47.72 ± 9.07 |
| SSP | 51.92 ± 9.48 | 44.55 ± 9.76 | Large (g = 0.76) | 49.33 ± 10.16 | |
| MTFP | 73.25 ± 9.87 | 68.97 ± 9.90 | Moderate (g = 0.42) | 71.74 ± 10.04 | |
| Lumbar curvature (degrees) | RSP | 32.51 ± 7.27 | 43.33 ± 8.24 | Large (g = −1.40) | 36.30 ± 9.20 |
| SSP | 9.79 ± 8.09 | 1.55 ± 11.01 | Large (g = 0.88) | 6.89 ± 9.98 | |
| MTFP | 17.49 ± 6.62 | 12.94 ± 9.43 | Moderate (g = 0.58) | 15.89 ± 7.98 | |
| Variable | Position | Category | Male (N = 61) | Female (N = 33) | ||
|---|---|---|---|---|---|---|
| Total (Degrees) | N (%) | Total (Degrees) | N (%) | |||
| Thoracic curvature | RSP | Hypokyphosis (<20°) | − | − | − | − |
| Normal (20 to 40°) | 37.50 ± 3.42 | 12 (19.67%) | 34.67 ± 6.98 | 12 (36.36%) | ||
| Hyperkyphosis (>40°) | 52.10 ± 6.13 | 49 (80.33%) | 50.81 ± 6.05 | 21 (63.64%) | ||
| SSP | Hypokyphosis (<20°) | − | − | − | − | |
| Normal (20 to 40°) | 37.55 ± 4.68 | 11 (18.03%) | 36.67 ± 5.97 | 15 (45.45%) * | ||
| Hyperkyphosis (>40°) | 55.08 ± 7.00 | 50 (81.97%) | 51.11 ± 7.03 | 18 (54.55%) | ||
| MTFP | Hypokyphosis (<40°) | − | − | − | − | |
| Normal (40 to 65°) | 60.88 ± 4.11 | 16 (26.23%) | 59.38 ± 5.24 | 13 (39.39%) | ||
| Hyperkyphosis (>65°) | 77.64 ± 7.18 | 45 (73.77%) | 75.20 ± 6.63 | 20 (60.61%) | ||
| Lumbar curvature | RSP | Hypolordosis (<−20°) | −18.50 ± −0.71 | 2 (3.28%) | − | − |
| Normal (−20 to −40°) | −31.73 ± −5.13 | 55 (90.16%) | −36.50 ± −3.03 | 16 * (48.48%) | ||
| Hyperlordotic (>−40°) | −50.00 ± −5.89 | 4 (5.89%) | −49.76 ± −6.05 | 17 (51.52%) | ||
| SSP | Hypokyphosis (<−15°) | −18.00 ± 0.0 | 1 (1.64%) | −24.00 ± 5.70 | 2 (6.06%) | |
| Normal (−15 to 15°) | 7.40 ± 4.43 | 48 (78.67%) | 1.70 ± 7.08 | 29 (87.88%) | ||
| Hyperkyphosis (>15°) | 21.60 ± 5.40 | 12 (19.67%) | 25.00 ± 7.09 | 2 (6.06%) | ||
| MTFP | Hypokyphosis (<10°) | 4.00 ± 5.89 | 4 (6.56%) | −0.29 ± 9.8 | 7 (21.2%) | |
| Normal (10 to 30°) | 18.14 ± 5.16 | 56 (91.80%) | 16.5 ± 5.4 | 26 (78.8%) | ||
| Hyperkyphosis (>30°) | 35.0 ± 0.0 | 1 (1.64%) | − | − | ||
| Thoracic SIM Classification | Position | Male (N = 61) | Female (N = 33) | |||
|---|---|---|---|---|---|---|
| Category | Subcategory | RSP | SSP | MFTP | N (%) | N (%) |
| Hypokyphotic attitude | Standing | Hypokyphosis (<20°) | Normal (20–40°) | Normal (40–65°) | − | 1 (1.06) |
| Functional hyperkyphosis | Static | Normal (20–40°) | Hyperkyphosis (>40°) | Normal (40–65°) | 2 (3.28) | − |
| Dynamic | Normal (20–40°) | Normal (20–40°) | Hyperkyphosis (>65) | − | 2 (6.06) | |
| Total | Normal (20–40°) | Hyperkyphosis (>40°) | Hyperkyphosis (>65°) | 5 (8.20) | 2 (6.06) | |
| Hyperkyphosis | Static | Hyperkyphosis (>40°) | Hyperkyphosis (>40°) | Normal (40–65°) | 7 (11.48) | 2 (6.06) |
| Standing | Hyperkyphosis (>40°) | Normal (20–40°) | Normal (40–65°) | 2 (3.28) | 3 (9.09) | |
| Dynamic | Hyperkyphosis (>40°) | Normal (20–40°) | Hyperkyphosis (>65°) | 4 (6.56) | 2 (6.06) | |
| Total | Hyperkyphosis (>40°) | Hyperkyphosis (>40°) | Hyperkyphosis (>65°) | 36 (59.02) | 14 (42.42) | |
| Lumbar SIM Classification | Position | Male (N = 61) | Female (N = 33) | |||
|---|---|---|---|---|---|---|
| Category | Subcategory | RSP | SSP | MFT | N (%) | N (%) |
| Hyperlordotic attitude | − | Hyperlordosis (>−40°) | Normal (−15 to −15°) | Normal (10 to 30°) | 3 (4.92) | 10 (30.30) * |
| Functional lumbarhyperkyphosis | Static | Normal (−20 to −40°) | Hyperkyphosis (>15°) | Normal (10–30°) | 10 (16.39) | 1 (3.03) |
| Lumbar spine with reduced mobility | Functional lumbar lordotic or Hypomobile lordosis | Normal (−20 to −40°) | Normal (0 ± 15°) | Hypokyphosis or lordosis (<10°) | 2 (3.28) | − |
| Hypolordosis | Hypolordotic attitude | Hypolordotic (<−20°) | Normal (0 ± 15°) | Normal (10–30°) | 2 (3.28) | − |
| Lumbar hypermobility | − | Hyperlordotic (>−40°) | Hyperkyphosis (>15°) | Hyperkyphosis (>30°) | 1 (1.64) | − |
| Structured hyperlordosis | − | Hyperlordotic (>−40°) | Hyperlordotic (<−15°) or normal (0 ± 15°) | Hypokyphosis (<10°) | 1 (1.64) | 7 (21.21) * |
| Variables | LBP-Free (N = 58) | LBP (N = 36) | p-Value | ES Hedges’ g 1 | |
|---|---|---|---|---|---|
| Years of training | 12.44 ± 5.72 | 12.62 ± 5.75 | 0.964 | Small (g = −0.25) | |
| Training hours per week | 6.56 ± 3.12 | 6.46 ± 2.49 | 0.554 | Small (g = −0.26) | |
| LH-SSP (degrees) | 100.50 ± 8.33 | 100.83 ± 10.46 | 0.433 | No effect (g = −0.03) | |
| LH-MTFP (degrees) | 94.95 ± 15.47 | 96.33 ± 16.04 | 0.753 | No effect (g = −0.09) | |
| Thoracic curvature (degrees) | RSP | 47.60 ± 9.36 | 47.92 ± 8.70 | 0.916 | No effect (g = −0.03) |
| SSP | 48.67 ± 10.92 | 50.39 ± 8.85 | 0.587 | Small (g = −0.17) | |
| MFTP | 71.69 ± 9.03 | 71.83 ± 11.61 | 0.773 | No effect (g = −0.01) | |
| Lumbar curvature (degrees) | RSP | 35.41 ± 8.04 | 37.72 ± 10.77 | 0.341 | Small (g = −0.25) |
| SSP | 5.97 ± 8.22 | 8.39 ± 12.28 | 0.303 | Small (g = −0.24) | |
| MFTP | 16.14 ± 6.17 | 15.50 ± 10.34 | 0.848 | No effect (g = 0.08) | |
| Classification SIM for Thoracic Curvature | Position | Low Back Pain | ||||
| Category | Subcategory | SP | SSP | MFT | Male (N = 61) | Female (N = 33) |
| Hyperkyphosis | Standing | Hyperkyphosis (>40°) | Normal (20–40°) | Normal (40–65°) | 0 | 1 |
| Functional hyperkyphosis | Dynamic | Normal (20–40°) | Normal (20–40°) | Hyperkyphosis (>65) | 0 | 2 |
| Total | Normal (20–40°) | Hyperkyphosis (>40°) | Hyperkyphosis (>65°) | 3 | 0 | |
| Hyperkyphosis | Dynamic | Hyperkyphosis (>40°) | Normal (20–40°) | Hyperkyphosis (>65°) | 0 | 2 |
| Total | Hyperkyphosis (>40°) | Hyperkyphosis (>40°) | Hyperkyphosis (>65°) | 12 | 8 | |
| Classification SIM for Lumbar Curvature | Position | Low Back Pain | ||||
| Category | Subcategory | RSP | SSP | MFTP | Male (N = 61) | Female (N = 33) |
| Hyperlordotic attitude | − | Hyperlordosis (>−40) | Normal (−15 to −15°) | Normal (10 to 30°) | 1 | 7 |
| Functional lumbar hyperkyphosis | Static | Normal (−20 to −40°) | Hyperkyphosis (>15°) | Normal (10–30°) | 7 | 1 |
| Structured hyperlordotic | − | Hyperlordosis (>−40°) | Hyperlordosis (<−15°) or normal (0 ± 15°) | Lordosis or Hypokyphosis (<10°) | 1 | 4 |
| Hypolordotic attitude | − | Hypolordosis (>−20°) | Normal (−15 to −15°) | Normal (10 to 30°) | 2 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cejudo, A.; Centenera-Centenera, J.M.; Santonja-Medina, F. Sagittal Integral Morphotype of Competitive Amateur Athletes and Its Potential Relation with Recurrent Low Back Pain. Int. J. Environ. Res. Public Health 2021, 18, 8262. https://doi.org/10.3390/ijerph18168262
Cejudo A, Centenera-Centenera JM, Santonja-Medina F. Sagittal Integral Morphotype of Competitive Amateur Athletes and Its Potential Relation with Recurrent Low Back Pain. International Journal of Environmental Research and Public Health. 2021; 18(16):8262. https://doi.org/10.3390/ijerph18168262
Chicago/Turabian StyleCejudo, Antonio, Josep María Centenera-Centenera, and Fernando Santonja-Medina. 2021. "Sagittal Integral Morphotype of Competitive Amateur Athletes and Its Potential Relation with Recurrent Low Back Pain" International Journal of Environmental Research and Public Health 18, no. 16: 8262. https://doi.org/10.3390/ijerph18168262
APA StyleCejudo, A., Centenera-Centenera, J. M., & Santonja-Medina, F. (2021). Sagittal Integral Morphotype of Competitive Amateur Athletes and Its Potential Relation with Recurrent Low Back Pain. International Journal of Environmental Research and Public Health, 18(16), 8262. https://doi.org/10.3390/ijerph18168262






