The Humanoid Robot Sil-Bot in a Cognitive Training Program for Community-Dwelling Elderly People with Mild Cognitive Impairment during the COVID-19 Pandemic: A Randomized Controlled Trial
Abstract
1. Introduction
Demographic Changes and Mild Cognitive Impairment
2. Materials and Methods
2.1. Design
2.2. Participants
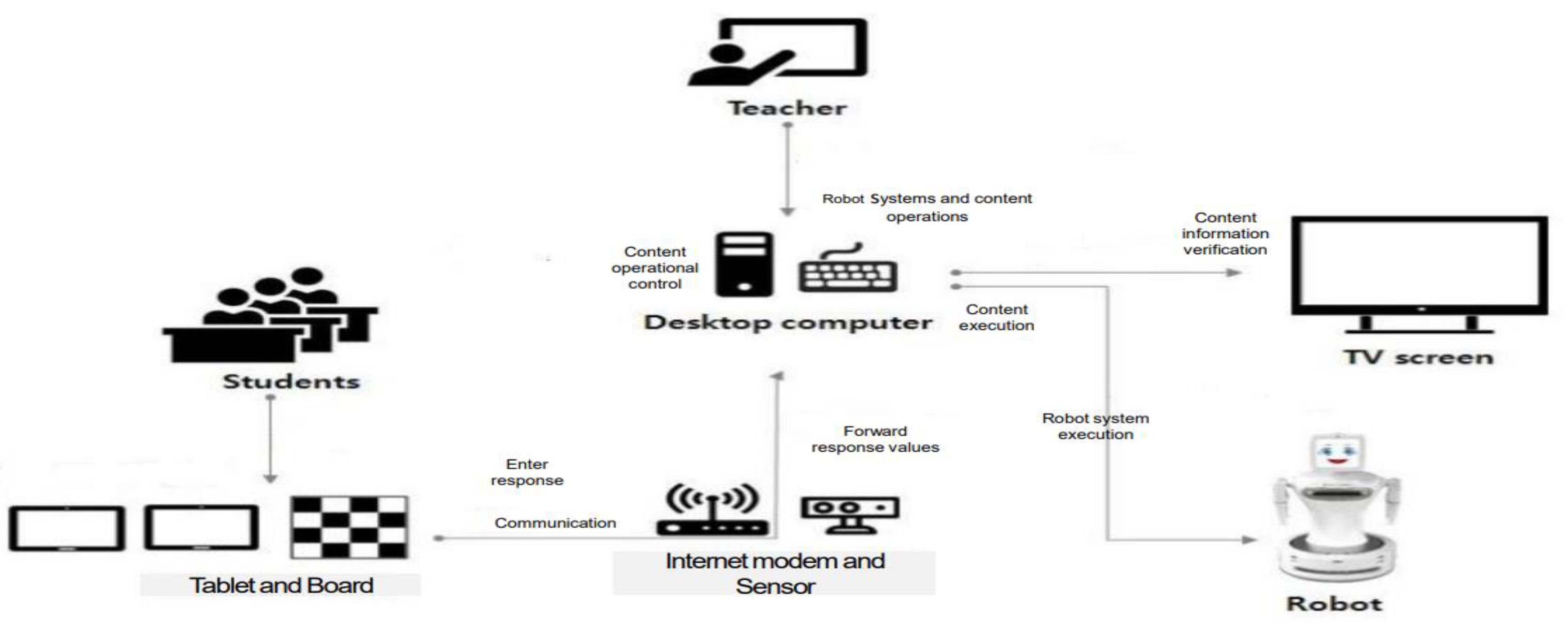
2.3. Materials
2.3.1. Main Software
2.3.2. Variables and Measuring Instruments
Cognition
Subjective Memory Complaints
Neuropsychological Assessment
Depression
2.3.3. Data Analysis
2.4. Procedure
2.4.1. RACT Groups
2.4.2. TCT Groups
2.4.3. NI Groups
2.5. Ethical Considerations
3. Results
3.1. Sample Description
3.2. Effect of Humanoid Robot Sil-Bot in a Cognitive Training Program on Cognition and Depression
3.3. Differences in the Pre- and Post-Intervention Effects
3.3.1. Cognition
3.3.2. Subjective Memory Complaints
3.3.3. Neuropsychological Assessment
3.3.4. Depression
3.4. Differences in the Pre- and Post-Intervention Effects According to General Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Petersen, R.C. Mild cognitive impairment. N. Engl. J. Med. 2011, 364, 2227–2234. [Google Scholar] [CrossRef] [PubMed]
- Overton, M.; Pihlsgård, M.; Elmståhl, S. Prevalence and incidence of mild cognitive impairment across subtypes, age, and sex. Dement. Geriatr. Cogn. Disord. 2019, 47, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Hussin, N.M.; Shahar, S.; Yahya, H.M.; Din, N.C.; Singh, D.K.A.; Omar, M.A. Incidence and predictors of mild cognitive impairment (MCI) within a multi-ethnic Asian populace: A community-based longitudinal study. BMC Public Health 2019, 19, 1159. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare & National Institute of Dementia. Korean Dementia Observatory. 2019. Available online: https://www.nid.or.kr/info/dataroom_view.aspx?bid=209 (accessed on 16 March 2021).
- Health Insurance Review and Assessment Service. Treatment Analysis of Dementia and Mild Cognitive Impairment. Available online: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020 (accessed on 16 March 2021).
- Tsoy, R.T.; Turuspekova, S.T.; Klipitskaya, N.K.; Mereke, A.; Cumming, R.G. Prevalence of Mild Cognitive Impairment Among Older People in Kazakhstan and Potential Risk Factors. Alzheimer Dis. Assoc. Disord. 2019, 33, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Ryu, S.H. The Clinical Significance of Cognitive Interventions for the Patients with Mild Cognitive Impairment. J. Korean Neuropsychiatr. Assoc. 2018, 57, 23–29. [Google Scholar] [CrossRef]
- Ginó, S.; Mendes, T.; Maroco, J.; Ribeiro, F.; Schmand, B.A.; De Mendonça, A.; Guerreiro, M. Memory complaints are frequent but qualitatively different in young and elderly healthy people. Gerontology 2010, 56, 272–277. [Google Scholar] [CrossRef]
- Buckley, R.; Saling, M.M.; Ames, D.; Rowe, C.C.; Lautenschlager, N.T.; Macaulay, S.L.; Martins, R.N.; Masters, C.L.; O’Meara, T.; Savage, G. Factors affecting subjective memory complaints in the AIBL aging study: Biomarkers, memory, affect, and age. Int. Psychogeriatr. 2013, 25, 1307–1315. [Google Scholar] [CrossRef]
- Jessen, F.; Wolfsgruber, S.; Wiese, B.; Bickel, H.; Mösch, E.; Kaduszkiewicz, H.; Pentzek, M.; Riedel-Heller, S.G.; Luck, T.; Fuchs, A. AD dementia risk in late MCI, in early MCI, and in subjective memory impairment. Alzheimers Dement. 2014, 10, 76–83. [Google Scholar] [CrossRef]
- Park, Y.; Oh, H. Development and evaluation of a community based multifaceted cognitive training program for the elderly with mild cognitive impairment. J. Korean Acad. Community Health Nurs. 2019, 30, 119–129. [Google Scholar] [CrossRef]
- Lin, J.S.; O’Connor, E.; Rossom, R.C.; Perdue, L.A.; Eckstrom, E. Screening for cognitive impairment in older adults: A systematic review for the US Preventive Services Task Force. Ann. Intern. Med. 2013, 159, 601–612. [Google Scholar] [CrossRef]
- Kim, C.; Park, M.; Kim, S. Analysis of trends in non-pharmacological studies for elders with dementia in Korea. J. Korean Gerontol. Nurs. 2012, 14, 129–141. [Google Scholar]
- Engvig, A.; Fjell, A.M.; Westlye, L.T.; Moberget, T.; Sundseth, Ø.; Larsen, V.A.; Walhovd, K.B. Effects of memory training on cortical thickness in the elderly. NeuroImage 2010, 52, 1667–1676. [Google Scholar] [CrossRef]
- Wenger, E.; Schaefer, S.; Noack, H.; Kühn, S.; Mårtensson, J.; Heinze, H.-J.; Düzel, E.; Bäckman, L.; Lindenberger, U.; Lövdén, M. Cortical thickness changes following spatial navigation training in adulthood and aging. NeuroImage 2012, 59, 3389–3397. [Google Scholar] [CrossRef]
- Eckroth-Bucher, M.; Siberski, J. Preserving cognition through an integrated cognitive stimulation and training program. Am. J. Alzheimers Dis. Other Demen. 2009, 24, 234–245. [Google Scholar] [CrossRef]
- Cheng, Y.; Wu, W.; Feng, W.; Wang, J.; Chen, Y.; Shen, Y.; Li, Q.; Zhang, X.; Li, C. The effects of multi-domain versus single-domain cognitive training in non-demented older people: A randomized controlled trial. BMC Med. 2012, 10, 30. [Google Scholar] [CrossRef]
- Kueider, A.M.; Parisi, J.M.; Gross, A.L.; Rebok, G.W. Computerized cognitive training with older adults: A systematic review. PLoS ONE 2012, 7, e40588. [Google Scholar] [CrossRef] [PubMed]
- Gates, N.J.; Sachdev, P. Is cognitive training an effective treatment for preclinical and early Alzheimer’s disease? J. Alzheimers Dis. 2014, 42, S551–S559. [Google Scholar] [CrossRef]
- Gavelin, H.M.; Lampit, A.; Hallock, H.; Sabatés, J.; Bahar-Fuchs, A. Cognition-oriented treatments for older adults: A systematic overview of systematic reviews. Neuropsychol. Rev. 2020, 30, 167–193. [Google Scholar] [CrossRef] [PubMed]
- Rebok, G.W.; Carlson, M.C.; Langbaum, J.B. Training and maintaining memory abilities in healthy older adults: Traditional and novel approaches. J. Gerontol. B Psychol. Sci. Soc. Sci. 2007, 62, 53–61. [Google Scholar] [CrossRef]
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.G.; Fu, H. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020, 20, 669–677. [Google Scholar] [CrossRef]
- Guan, W.J.; Liang, W.H.; Zhao, Y.; Liang, H.R.; Chen, Z.S.; Li, Y.M.; Liu, X.Q.; Chen, R.C.; Tang, C.L.; Wang, T. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur. Respir. J. 2020, 55. [Google Scholar] [CrossRef]
- Livingston, G.; Weidner, W. COVID-19 and Dementia: Difficult Decisions about Hospital Admission and Triage. 2020. Available online: https://www.alz.co.uk/news/adi-releases-position-paper-on-covid-19-anddementia (accessed on 22 April 2020).
- Kim, G.H.; Jeon, S.; Im, K.; Kwon, H.; Lee, B.H.; Kim, G.Y.; Jeong, H.; Han, N.E.; Seo, S.W.; Cho, H. Structural brain changes after traditional and robot-assisted multi-domain cognitive training in community-dwelling healthy elderly. PLoS ONE 2015, 10, e0123251. [Google Scholar] [CrossRef]
- Pino, O.; Palestra, G.; Trevino, R.; De Carolis, B. The humanoid robot NAO as trainer in a memory program for elderly people with mild cognitive impairment. Int. J. Soc. Robot. 2020, 12, 21–33. [Google Scholar] [CrossRef]
- Manca, M.; Paternò, F.; Santoro, C.; Zedda, E.; Braschi, C.; Franco, R.; Sale, A. The impact of serious games with humanoid robots on mild cognitive impairment older adults. Int. J. Hum. Comput. Stud. 2021, 145, 102509. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.H. Sample size calculations with dropouts in clinical trials. Comm. Stat. Appl. Methods 2008, 15, 353–365. [Google Scholar] [CrossRef][Green Version]
- Folstein, M. A practical method for grading the cognitive state of patients for the children. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Kim, T.H.; Jhoo, J.H.; Park, J.H.; Kim, J.L.; Ryu, S.H.; Moon, S.W.; Choo, I.H.; Lee, D.W.; Yoon, J.C.; Do, Y.J. Korean version of mini mental status examination for dementia screening and its’ short form. Psychiatry Investig. 2010, 7, 102. [Google Scholar] [CrossRef]
- Youn, J.C.; Kim, K.W.; Lee, D.Y.; Jhoo, J.H.; Lee, S.B.; Park, J.H.; Choi, E.A.; Choe, J.Y.; Jeong, J.W.; Choo, I.H. Development of the subjective memory complaints questionnaire. Dement. Geriatr. Cogn. Disord. 2009, 27, 310–317. [Google Scholar] [CrossRef]
- Lee, D.Y. A normative study of the Korean version of CERAD neuropsychological test battery CERAD-K in elderly. Ph.D. Thesis, Seoul National University, Seoul, Korea, 2001. [Google Scholar]
- Yesavage, J.A.; Sheikh, J.I. 9/Geriatric depression scale (GDS) recent evidence and development of a shorter version. Clin. Gerontol. 1986, 5, 165–173. [Google Scholar] [CrossRef]
- Kee, B.S. A preliminary study for the standardization of geriatric depression scale short form-Korea version. J. Korean Neuropsychiatr. Assoc. 1996, 35, 298–307. [Google Scholar]
- Oh, J.H.; Yi, Y.J.; Shin, C.J.; Park, C.S.; Kang, S.S.; Kim, J.H.; Kim, I.S. Effects of silver-care-robot program on cognitive function, depression, and activities of daily living for institutionalized elderly people. J. Korean Acad. Nurs. 2015, 45, 388–396. [Google Scholar] [CrossRef]
- Coyle, H.; Traynor, V.; Solowij, N. Computerized and virtual reality cognitive training for individuals at high risk of cognitive decline: Systematic review of the literature. Am. J. Geriatr. Psychiatry 2015, 23, 335–359. [Google Scholar] [CrossRef]
- Gates, N.J.; Sachdev, P.S.; Singh, M.A.F.; Valenzuela, M. Cognitive and memory training in adults at risk of dementia: A systematic review. BMC Geriatr. 2011, 11, 55. [Google Scholar] [CrossRef] [PubMed]
- Demarin, V.; Morović, S. Neuroplasticity. Period. Biol. 2014, 116, 209–211. [Google Scholar]
- Park, Y.R.J.; Sohng, K.Y. Effects of a customized health promotion program on depression, cognitive functioning, and physical health of elderly women living slone in community: A cluster randomized controlled trial. J. Korean Acad. Nurs. 2019, 49, 515–525. [Google Scholar] [CrossRef]
- Hill, N.T.; Mowszowski, L.; Naismith, S.L.; Chadwick, V.L.; Valenzuela, M.; Lampit, A. Computerized cognitive training in older adults with mild cognitive impairment or dementia: A systematic review and meta-analysis. Am. J. Psychiatry 2017, 174, 329–340. [Google Scholar] [CrossRef]
- Reddy, R. Robotics and intelligent systems in support of society. IEEE Intell. Syst. 2006, 21, 24–31. [Google Scholar] [CrossRef]
- Kim, K.; Kim, O. The effects of exercise-cognitive combined dual-task program on cognitive function and depression in elderly with mild cognitive impairment. Korean J. Adult Nurs. 2015, 27, 707–717. [Google Scholar] [CrossRef]
- Bemelmans, R.; Gelderblom, G.J.; Jonker, P.; De Witte, L. Socially assistive robots in elderly care: A systematic review into effects and effectiveness. J. Am. Med. Dir. Assoc. 2012, 13, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Cotten, S.R.; Ford, G.; Ford, S.; Hale, T.M. Internet use and depression among older adults. Comput. Hum. Behav. 2012, 28, 496–499. [Google Scholar] [CrossRef]
- Han, A.; Park, Y.H. Attitude Toward and Intention to Use Care Robot Technology in Older Adults and Family Members. Korean J. Adult Nurs. 2019, 31. [Google Scholar] [CrossRef]
- Stice, E.; Ragan, J.; Randall, P. Prospective relations between social support and depression: Differential direction of effects for parent and peer support? J. Abnorm. Psychol. 2004, 113, 155. [Google Scholar] [CrossRef] [PubMed]
- Ernst, R.L.; Hay, J.W.; Fenn, C.; Tinklenberg, J.; Yesavage, J.A. Cognitive function and the costs of Alzheimer disease. An exploratory study. Arch. Neurol. 1997, 54, 687–693. [Google Scholar] [CrossRef]
- Choi, J.; Medalia, A. Factors associated with a positive response to cognitive remediation in a community psychiatric sample. Psychiatr. Serv. 2005, 56, 602–604. [Google Scholar] [CrossRef]
- Sokolov, A.A.; Collignon, A.; Bieler-Aeschlimann, M. Serious video games and virtual reality for prevention and neurorehabilitation of cognitive decline because of aging and neurodegeneration. Curr. Opin. Neurol. 2020, 33, 239–248. [Google Scholar] [CrossRef]

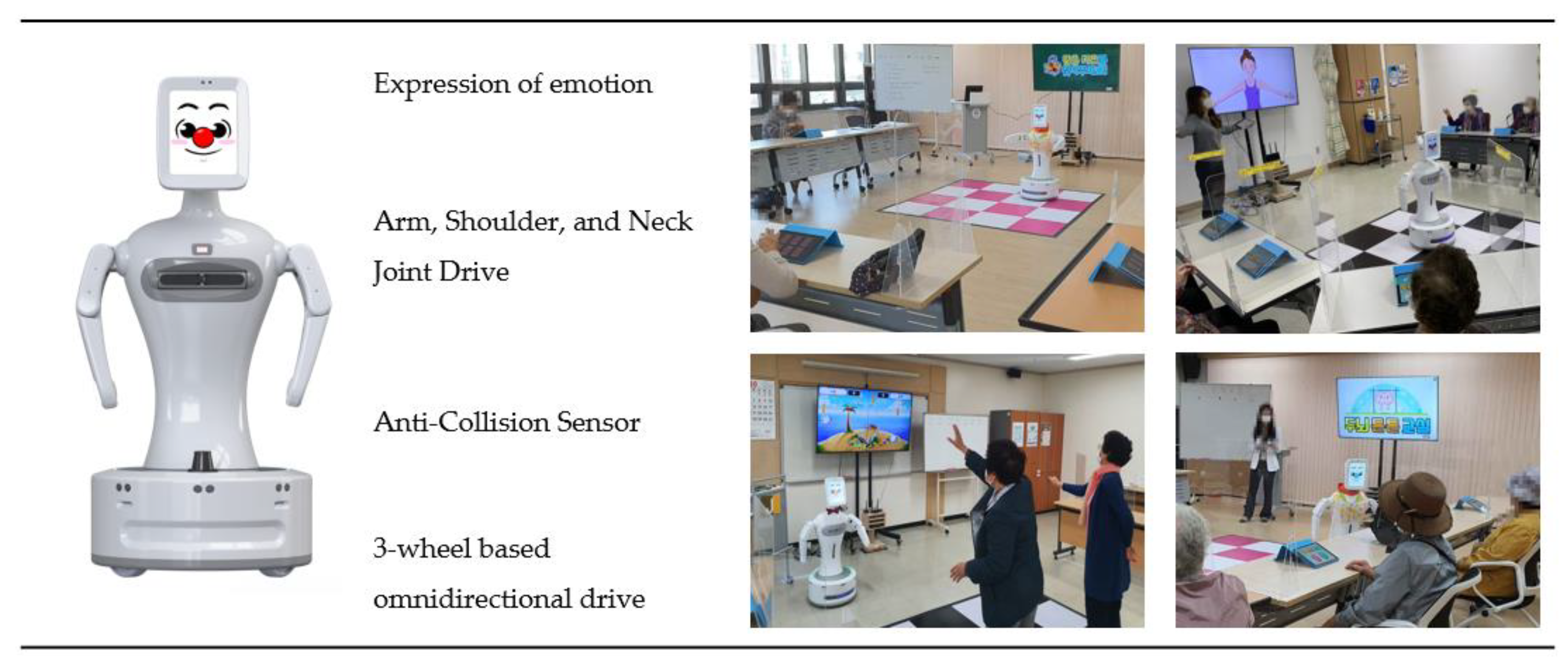
| Category | Detailed Specifics | Category | Detailed Specifics |
|---|---|---|---|
| Size | 480 × 520 × 1150 (mm) | System | Intel i3 CPU |
| 8G DDR4 RAM | |||
| 2 × USB 3.0 | |||
| Wireless Ethernet | |||
| Gigabit Ethernet | |||
| Weight | 25 kg | OS | Linux Ubuntu |
| Battery usage time | 4–6 h | Display | 9.7 inch IPS decompression formula |
| Display (1024 × 768 Resolution) | |||
| Battery charging time | 90 min (220 Vcharger) | Sensor, etc. | Gyro sensor, LED |
| Battery | 24 V Lithium ion | Camera | HD 720 P (1280 × 720) (mm) |
| Degree of freedom | 11 (arms, head, mobile) | Software | ROS Kinetic |
| Voice and language | Korean (adult female 3 types, adult male 3 types, child 3 types) | Smart pad | Galaxytab10.1 (Samsung Electronics, Seoul, Korea) |
| English (adult female 3 types, adult male 2 types) |
| Variables | Categories | Total (N = 135) | Robot-Assisted (N = 45) | Traditional (N = 45) | No Intervention (N = 45) | p |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |||
| Cognitive impairment status | MCI | 57 (42.2) | 17 (37.8) | 22 (48.9) | 18 (40.0) | 0.529 |
| SMC | 78 (57.8) | 28 (62.2) | 23 (51.1) | 27 (60.0) | ||
| Age (years), Mean ± SD | 75.9 ± 6.1 | 75.5 ± 5.9 | 76.7 ± 5.9 | 75.6 ± 6.6 | 0.959 | |
| Gender | Male | 37 (27.4) | 13 (28.9) | 12 (26.7) | 12 (26.7) | 0.963 |
| Female | 98 (72.6) | 32 (71.1) | 33 (73.3) | 33 (73.3) | ||
| Living status (duplicate selection) | Alone | 45 (33.3) | 21 (46.7) | 13 (28.9) | 11 (24.4) | 0.061 |
| Spouse | 66 (48.9) | 18 (40.0) | 25 (55.6) | 23 (51.1) | 0.315 | |
| Children | 30 (22.2) | 10 (22.2) | 8 (17.8) | 12 (26.7) | 0.598 | |
| Offspring | 8 (5.9) | 2 (4.4) | 2 (4.4) | 4 (8.9) | 0.588 | |
| Etc. | 2 (1.5) | 0 (0.0) | 0 (0.0) | 2 (4.4) | 0.131 | |
| Number of children | None | 6 (4.4) | 5 (11.1) | 1 (2.2) | 0 (0.0) | 0.189 |
| 1 | 19 (14.1) | 8 (17.8) | 6 (13.3) | 5 (11.1) | ||
| 2 | 39 (28.9) | 11 (24.4) | 14 (31.1) | 14 (31.1) | ||
| ≥3 | 71 (52.6) | 21 (46.7) | 24 (53.3) | 26 (57.8) | ||
| Level of education | Mean ± SD | 8.8 ± 4.3 | 9.3 ± 4.2 | 8.4 ± 4.6 | 8.8 ± 4.2 | 0.645 |
| None | 12 (8.9) | 3 (6.7) | 5 (11.1) | 4 (8.9) | 0.749 | |
| Elementary school | 43 (31.9) | 14 (31.1) | 17 (37.8) | 12 (26.7) | ||
| Middle school | 32 (23.7) | 9 (20.0) | 9 (20.0) | 14 (31.1) | ||
| High school | 30 (22.2) | 13 (28.9) | 7 (15.6) | 10 (22.2) | ||
| College and higher | 18 (13.3) | 6 (13.3) | 7 (15.6) | 5 (11.1) | ||
| Health status | Average | 3.1 ± 0.9 | 3.2 ± 0.9 | 3.0 ± 0.9 | 3.2 ± 0.9 | 0.906 |
| Very good | 2 (1.5) | 1 (2.2) | 0 (0.0) | 1 (2.2) | 0.899 | |
| good | 30 (22.2) | 10 (22.2) | 12 (26.7) | 8 (17.8) | ||
| Moderate | 61 (45.2) | 18 (40.0) | 22 (48.9) | 21 (46.7) | ||
| Bad | 33 (24.4) | 13 (28.9) | 8 (17.8) | 12 (26.7) | ||
| Very bad | 9 (6.7) | 3 (6.7) | 3 (6.7) | 3 (6.7) | ||
| Comorbidity status (duplicate selection) | None | 17 (12.6) | 3 (6.7) | 5 (11.1) | 9 (20.0) | 0.152 |
| Hypertension | 70 (51.9) | 27 (60.0) | 25 (55.6) | 18 (40.0) | 0.137 | |
| Diabetes | 32 (23.7) | 12 (26.7) | 8 (17.8) | 12 (26.7) | 0.519 | |
| Stroke | 9 (6.7) | 4 (8.9) | 2 (4.4) | 3 (6.7) | 0.700 | |
| Arthritis | 42 (31.1) | 17 (37.8) | 9 (20.0) | 16 (35.6) | 0.139 | |
| Incontinence | 15 (11.1) | 5 (11.1) | 4 (8.9) | 6 (13.3) | 0.799 | |
| Cancer | 7 (5.2) | 4 (8.9) | 0 (0.0) | 3 (6.7) | 0.141 | |
| Heart disease | 17 (12.6) | 6 (13.3) | 4 (8.9) | 7 (15.6) | 0.624 | |
| Hyperlipidemia | 20 (14.8) | 3 (6.7) | 9 (20.0) | 8 (17.8) | 0.162 | |
| Etc. | 41 (30.4) | 17 (37.8) | 12 (26.7) | 12 (26.7) | 0.417 | |
| Variables | Robot-Assisted a (N = 45) | Traditional b (N = 45) | No Intervention c (N = 45) | p | Source | F | p | |
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | ||||||||
| MMSE-DS | Pre | 25.3 ± 4.1 | 26.6 ± 3.0 | 25.8 ± 3.9 | 0.516 | Time | 3.939 | 0.049 |
| Post | 26.6 ± 3.3 | 26.3 ± 3.1 | 26.0 ± 4.1 | 0.387 | Time × group | 6.172 | 0.003 | |
| Group | 0.335 | 0.716 | ||||||
| SMCQ | Pre | 5.9 ± 3.3 | 7.6 ± 2.0 | 6.3 ± 2.4 | 0.46 | Time | 31.744 | <0.001 |
| Post | 4.7 ± 3.5 | 5.0 ± 3.2 | 6.6 ± 3.0 | 0.008 | Time × group | 14.635 | <0.001 | |
| a < c | Group | 2.328 | 0.102 | |||||
| CERAD-K | Pre | 67.8 ± 15.1 | 64.5 ± 16.0 | 64.9 ± 13.7 | 0.368 | Time | 46.558 | <0.001 |
| Post | 71.6 ± 14.6 | 69.0 ± 17.4 | 66.0 ± 15.2 | 0.091 | Time × group | 5.274 | 0.006 | |
| Group | 0.925 | 0.399 | ||||||
| GDSSF-K | Pre | 4.3 ± 4.8 | 3.8 ± 3.8 | 4.9 ± 3.9 | 0.481 | Time | 0.949 | 0.332 |
| Post | 3.0 ± 3.6 | 4.7 ± 4.9 | 4.7 ± 4.1 | 0.048 | Time × group | 6.284 | 0.002 | |
| a < bc | Group | 1.045 | 0.355 | |||||
| Variables | Robot-Assisted (N = 45) | Traditional (N = 45) | No Intervention (N = 45) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | t (p) | Pre | Post | t (p) | Pre | Post | t (p) | ||
| MMSE-DS | 25.3 ± 4.1 | 26.6 ± 3.3 | 4.707 (<0.001) | 26.6 ± 3.0 | 26.3 ± 3.1 | −1.180 (0.224) | 25.8 ± 3.9 | 26.0 ± 4.1 | 0.355 (0.724) | |
| SMCQ | 5.9 ± 3.3 | 4.7 ± 3.5 | −2.282 (0.007) | 7.6 ± 2.0 | 5.0 ± 3.2 | −6.671 (<0.001) | 6.3 ± 2.4 | 6.6 ± 3.0 | 0.842 (0.404) | |
| GDSSF-K | 4.3 ± 4.8 | 3.0 ± 3.6 | −3.307 (0.004) | 3.8 ± 3.8 | 4.7 ± 4.9 | 1.971 (0.055) | 4.9 ± 3.9 | 4.7 ± 4.1 | −0.450 (0.655) | |
| CERAD-K | Total | 67.8 ± 15.1 | 71.6 ± 14.6 | 4.610 (<0.001) | 64.5 ± 16.0 | 69.0 ± 17.4 | 5.393 (<0.001) | 64.9 ± 13.7 | 66.0 ± 15.2 | 1.487 (0.144) |
| Verbal Fluency | 13.4 ± 4.2 | 14.0 ± 5.0 | 1.210 (0.233) | 12.4 ± 3.9 | 12.9 ± 5.0 | 1.068 (0.292) | 11.7 ± 3.7 | 11.7 ± 3.9 | 0.000 (0.999) | |
| Boston Naming | 10.9 ± 3.2 | 11.4 ± 2.9 | 2.395 (0.021) | 10.2 ± 2.8 | 10.5 ± 2.9 | 1.108 (0.274) | 10.6 ± 2.6 | 10.6 ± 2.8 | 0.0119 (0.906) | |
| MMSE-KC | 25.9 ± 3.6 | 26.6 ± 3.3 | 2.378 (0.022) | 26.6 ± 3.0 | 26.3 ± 3.1 | −1.074 (0.289) | 25.8 ± 3.6 | 26.0 ± 4.1 | 0.555 (0.582) | |
| Word List Memory | 16.0 ± 4.2 | 17.1 ± 4.3 | 2.711 (0.010) | 15.7 ± 5.0 | 17.2 ± 5.6 | 2.955 (0.005) | 15.5 ± 3.7 | 16.4 ± 4.4 | 1.932 (0.060) | |
| Constructional Praxis | 9.8 ± 1.7 | 9.6 ± 1.9 | −0.831 (0.410) | 9.7 ± 1.7 | 9.6 ± 1.7 | −0.304 (0.763) | 9.4 ± 2.0 | 8.9 ± 2.0 | −2.296 (0.027) | |
| Word List Recall | 4.7 ± 2.3 | 5.4 ± 2.0 | 3.387 (0.001) | 4.5 ± 2.7 | 5.3 ± 2.7 | 4.038 (<0.001) | 4.6 ± 2.2 | 5.0 ± 2.7 | 1.633 (0.110) | |
| Word List Recognition | 8.2 ± 2.2 | 8.7 ± 2.0 | 2.383 (0.002) | 7.6 ± 2.8 | 7.8 ± 2.4 | 0.946 (0.350) | 8.2 ± 2.1 | 8.4 ± 2.2 | 0.759 (0.452) | |
| Constructional Recall | 4.7 ± 3.4 | 5.4 ± 3.1 | 1.907 (0.063) | 4.7 ± 3.2 | 5.7 ± 3.4 | 3.100 (0.003) | 4.9 ± 2.8 | 5.0 ± 2.8 | 0.232 (0.817) | |
| Variables | Robot-Assisted | Traditional | No Intervention | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Pre | Post | t (p) | N | Pre | Post | t (p) | N | Pre | Post | t (p) | |||
| MMSE-DS | Gender | Male | 13 | 25.6 ± 3.7 | 26.6 ± 2.8 | −1.927 (0.078) | 12 | 26.2 ± 2.8 | 25.6 ± 3.3 | 1.023 (0.328) | 12 | 24.6 ± 4.8 | 25.4 ± 4.6 | −0.940 (0.367) |
| Female | 32 | 25.2 ± 4.3 | 26.6 ± 3.5 | −4.319 (< 0.001) | 33 | 26.8 ± 3.1 | 26.5 ± 3.1 | 0.713 (0.481) | 33 | 26.3 ± 3.5 | 26.2 ± 4.0 | 0.180 (0.858) | ||
| Age | <75 years | 20 | 25.2 ± 3.9 | 27.1 ± 3.0 | −4.498 (< 0.001) | 16 | 27.2 ± 2.7 | 26.6 ± 2.9 | 1.098 (0.289) | 19 | 25.4 ± 4.3 | 26.0 ± 4.8 | −1.207 (0.243) | |
| ≥75 years | 25 | 25.4 ± 4.3 | 26.3 ± 3.6 | −2.402 (0.024) | 29 | 26.3 ± 3.2 | 26.1 ± 3.2 | 0.519 (0.608) | 26 | 26.1 ± 3.7 | 26.0 ± 3.6 | 0.228 (0.821) | ||
| Years of Education | ≤9 years | 26 | 24.3 ± 4.8 | 25.8 ± 3.8 | −3.545 (0.002) | 31 | 26.4 ± 3.2 | 26.3 ± 3.3 | 0.456 (0.651) | 30 | 25.6 ± 3.7 | 25.6 ± 4.1 | −0.11 (0.911) | |
| >9 years | 19 | 26.7 ± 2.3 | 27.8 ± 1.9 | −3.162 (0.005) | 14 | 27.0 ± 2.5 | 26.4 ± 2.6 | 1.979 (0.069) | 15 | 26.3 ± 4.4 | 26.7 ± 4.3 | −0.56 (0.587) | ||
| SMCQ | Gender | Male | 13 | 6.1 ± 3.2 | 4.3 ± 3.2 | 1.998 (0.069) | 12 | 6.4 ± 2.2 | 3.7 ± 3.1 | 4.371 (0.001) | 12 | 5.4 ± 2.2 | 5.8 ± 2.6 | −0.731 (0.480) |
| Female | 32 | 5.8 ± 3.4 | 4.8 ± 3.7 | 2.025 (0.052) | 33 | 8.0 ± 1.7 | 5.4 ± 3.2 | 5.251 (< 0.001) | 33 | 6.7 ± 2.4 | 6.8 ± 3.2 | −0.507 (0.616) | ||
| Age | <75 years | 20 | 5.8 ± 3.0 | 4.6 ± 3.3 | 1.842 (0.081) | 16 | 8.1 ± 1.9 | 5.3 ± 3.3 | 3.873 (0.002) | 19 | 5.9 ± 2.4 | 6.3 ± 2.8 | −0.812 (0.427) | |
| ≥75 years | 25 | 6.0 ± 3.6 | 4.8 ± 3.7 | 2.103 (0.046) | 29 | 7.3 ± 2.0 | 4.8 ± 3.2 | 5.358 (< 0.001) | 26 | 6.6 ± 2.4 | 6.7 ± 3.2 | −0.36 (0.722) | ||
| Years of Education | ≤9 years | 26 | 6.3 ± 3.5 | 4.8 ± 3.7 | 2.562 (0.017) | 31 | 7.4 ± 1.5 | 4.4 ± 2.9 | 6.059 (< 0.001) | 30 | 6.4 ± 2.4 | 6.4 ± 3.1 | 0.126 (0.901) | |
| >9 years | 19 | 5.3 ± 3.0 | 4.5 ± 3.4 | 1.285 (0.215) | 14 | 8.0 ± 2.8 | 6.3 ± 3.7 | 3.067 (0.009) | 15 | 6.1 ± 2.6 | 6.9 ± 3.0 | −1.26 (0.228) | ||
| CERAD-K | Gender | Male | 13 | 66.5 ± 17.7 | 70.0 ± 19.2 | −1.963 (0.073) | 12 | 57.7 ± 15.7 | 63.8 ± 19.8 | −3.163 (0.009) | 12 | 62.8 ± 15.3 | 64.6 ± 16.4 | −1.325 (0.212) |
| Female | 32 | 68.3 ± 14.2 | 72.3 ± 12.6 | −4.221 (< 0.001) | 33 | 67.0 ± 15.6 | 70.9 ± 16.4 | −4.381 (< 0.001) | 33 | 65.7 ± 13.3 | 66.5 ± 15.0 | −0.951 (0.349) | ||
| Age | <75 years | 20 | 72.1 ± 15.0 | 74.8 ± 14.2 | −2.950 (0.008) | 16 | 65.9 ± 13.3 | 70.3 ± 13.5 | −4.040 (0.001) | 19 | 67.5 ± 15.1 | 69.0 ± 16.0 | −1.661 (0.114) | |
| ≥75 years | 25 | 64.3 ± 14.6 | 69.1 ± 14.7 | −3.688 (0.001) | 29 | 63.7 ± 17.4 | 68.3 ± 19.5 | −3.956 (< 0.001) | 26 | 63.0 ± 12.6 | 63.8 ± 14.5 | −0.69 (0.495) | ||
| Years of Education | ≤9 years | 26 | 64.0 ± 14.8 | 68.8 ± 14.6 | −4.206 (< 0.001) | 31 | 65.6 ± 15.7 | 69.6 ± 17.7 | −4.009 (< 0.001) | 30 | 63.5 ± 13.0 | 64.7 ± 14.9 | −1.29 (0.206) | |
| >9 years | 19 | 72.9 ± 14.2 | 75.4 ± 14.0 | −2.150 (0.045) | 14 | 62.0 ± 17.0 | 67.6 ± 17.5 | −3.657 (0.003) | 15 | 67.7 ± 15.2 | 68.6 ± 16.1 | −0.71 (0.487) | ||
| GDSSF-K | Gender | Male | 13 | 3.7 ± 4.3 | 1.9 ± 2.7 | 2.599 (0.023) | 12 | 3.0 ± 4.0 | 3.5 ± 4.8 | −0.944 (0.365) | 12 | 4.9 ± 3.6 | 5.9 ± 4.3 | −1.436 (0.179) |
| Female | 32 | 4.6 ± 5.0 | 3.4 ± 3.9 | 2.121 (0.042) | 33 | 4.2 ± 3.7 | 5.1 ± 4.9 | −1.745 (0.091) | 33 | 4.9 ± 4.1 | 4.3 ± 4.0 | 1.187 (0.244) | ||
| Age | <75 years | 20 | 3.8 ± 4.8 | 3.1 ± 3.0 | 0.928 (0.365) | 16 | 4.6 ± 4.1 | 4.4 ± 4.8 | 0.332 (0.744) | 19 | 6.0 ± 4.6 | 5.8 ± 4.7 | 0.203 (0.841) | |
| ≥75 years | 25 | 4.8 ± 4.8 | 2.8 ± 4.0 | 3.488 (0.002) | 29 | 3.4 ± 3.5 | 4.8 ± 5.0 | −2.522 (0.018) | 26 | 4.2 ± 3.2 | 3.9 ± 3.5 | 0.433 (0.669) | ||
| Years of Education | ≤9 years | 26 | 4.7 ± 5.3 | 2.8 ± 3.7 | 2.794 (0.010) | 31 | 3.7 ± 3.7 | 4.5 ± 4.8 | −1.511 (0.141) | 30 | 4.9 ± 4.0 | 4.7 ± 4.3 | 0.261 (0.796) | |
| >9 years | 19 | 3.8 ± 4.1 | 3.1 ± 3.5 | 1.351 (0.193) | 14 | 4.1 ± 4.1 | 4.9 ± 5.1 | −1.295 (0.218) | 15 | 5.1 ± 3.9 | 4.7 ± 3.9 | 0.378 (0.711) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, E.-A.; Jung, A.-R.; Lee, K.-A. The Humanoid Robot Sil-Bot in a Cognitive Training Program for Community-Dwelling Elderly People with Mild Cognitive Impairment during the COVID-19 Pandemic: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 8198. https://doi.org/10.3390/ijerph18158198
Park E-A, Jung A-R, Lee K-A. The Humanoid Robot Sil-Bot in a Cognitive Training Program for Community-Dwelling Elderly People with Mild Cognitive Impairment during the COVID-19 Pandemic: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(15):8198. https://doi.org/10.3390/ijerph18158198
Chicago/Turabian StylePark, Eun-A, Ae-Ri Jung, and Kyoung-A Lee. 2021. "The Humanoid Robot Sil-Bot in a Cognitive Training Program for Community-Dwelling Elderly People with Mild Cognitive Impairment during the COVID-19 Pandemic: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 15: 8198. https://doi.org/10.3390/ijerph18158198
APA StylePark, E.-A., Jung, A.-R., & Lee, K.-A. (2021). The Humanoid Robot Sil-Bot in a Cognitive Training Program for Community-Dwelling Elderly People with Mild Cognitive Impairment during the COVID-19 Pandemic: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(15), 8198. https://doi.org/10.3390/ijerph18158198






