‘Improving Health through Reducing Stress’: Parents’ Priorities in the Participatory Development of a Multilevel Family Health Programme in a Low-Income Neighbourhood in The Netherlands
Abstract
:1. Introduction
2. Methods
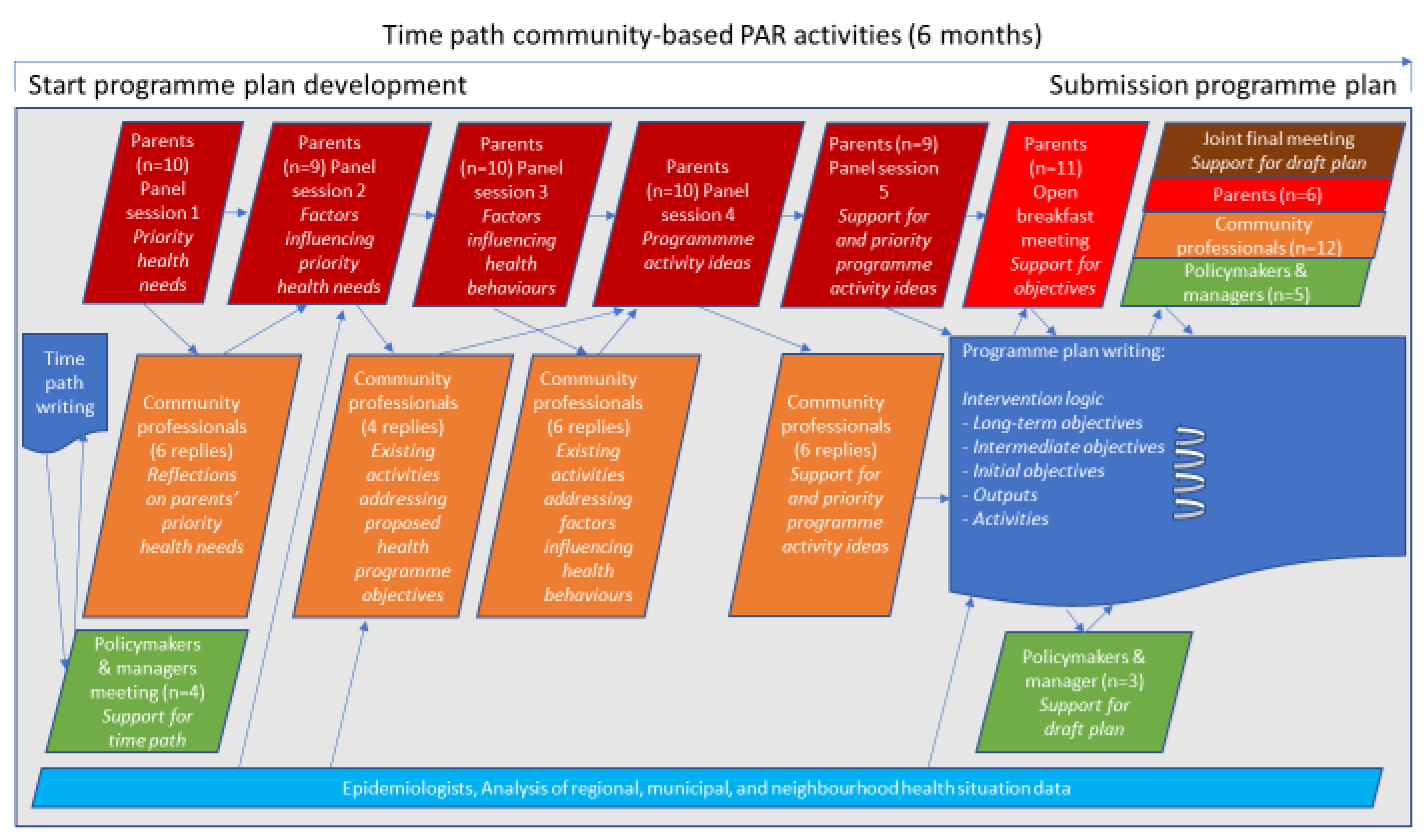
2.1. Study Design
2.2. Study Context and Setting
2.3. Study Population
2.4. Data Collection by Panel Sessions with Parents
2.5. Data Analysis
3. Results
3.1. Panel Participants’ Characteristics
3.2. Parents’ Views on What Family Health Entails in Their Neighbourhood
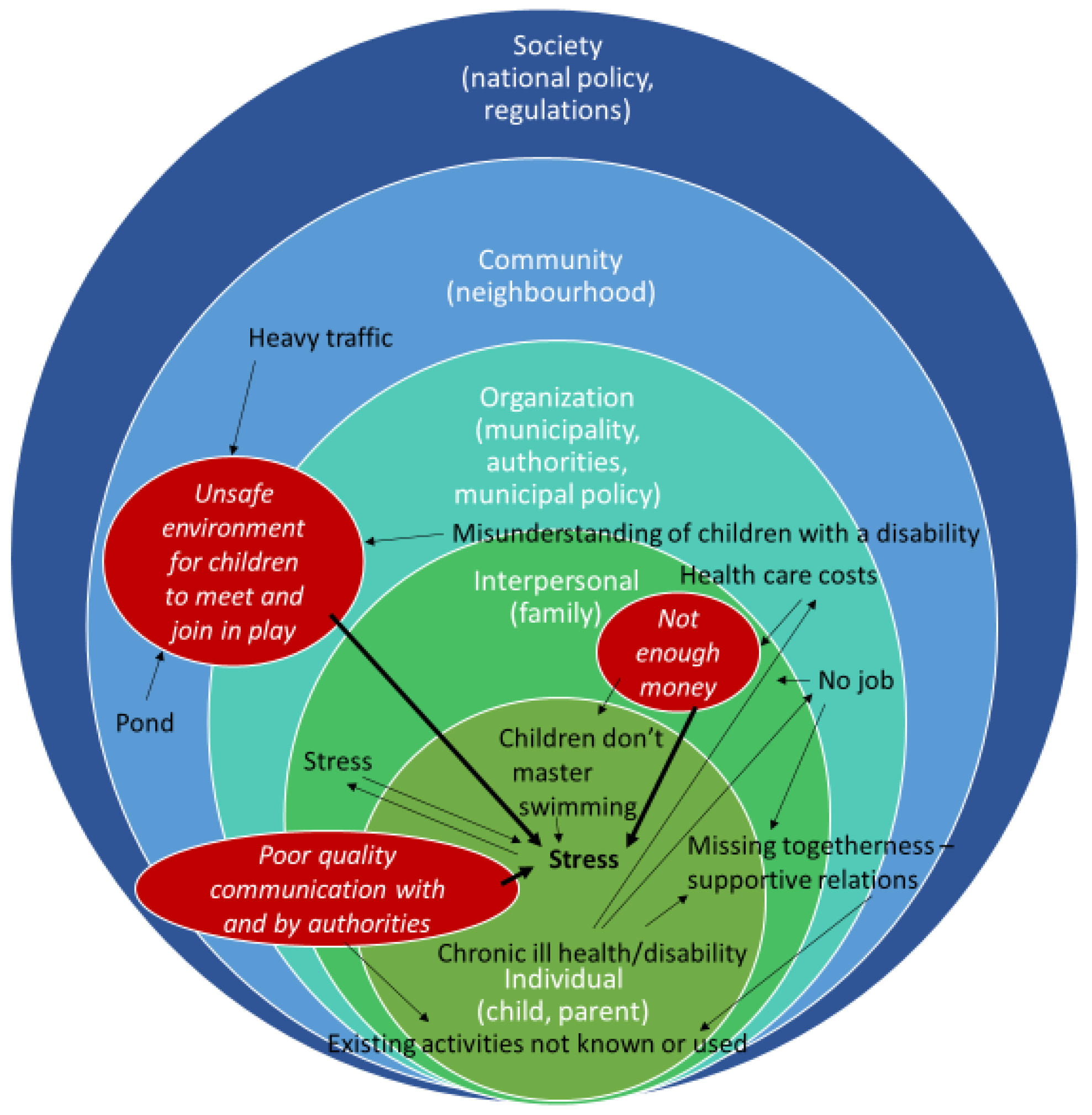
3.3. Parents’ Priorities for Improving Family Health
3.3.1. Parents’ Priority: Enough Money
3.3.2. Parents’ Priority: Happy Children with a Safe Place to Meet and Play
3.3.3. Parents’ Priority: Good Communication with Authorities
3.4. Parents’ Ideas for Programme Activities
- Information on, and easy referral to, organisations that could help to reduce financial stress, for instance by paying for swimming lessons for children. Parents indicated that many people did not make use of existing possibilities as people did not know of their existence, or did not know where or whom to ask about them, or the people that they asked did not know. Parents suggested that the authorities or the general practitioner should refer people to specific information on websites or inform them on who does what.
- Adjustment of forms from authorities to make them easier to understand, to reduce stress related to communication. Parents suggested that the municipality should accompany verbal information with written information that they could read at home at leisure. They suggested that professionals working at authorities should empathise with their situation, think along with their ideas and keep their word.
- Regular low-cost group activities for children to meet friends, differentiated by children’s age and disability, for instance, ‘playing games, playing soccer, craft making’.
- Low cost, social activities for parents to increase togetherness, for example, a healthy-cooking workshop or creative activities. However, many parents expected the participation threshold to be (too) high; for example, people would be afraid to participate alone, fearing that people going there already would all be friends. To overcome this threshold, they suggested an accompanying buddy or a high financial reward, for example, a bingo night with high value prizes for all, though this was not considered realistic.
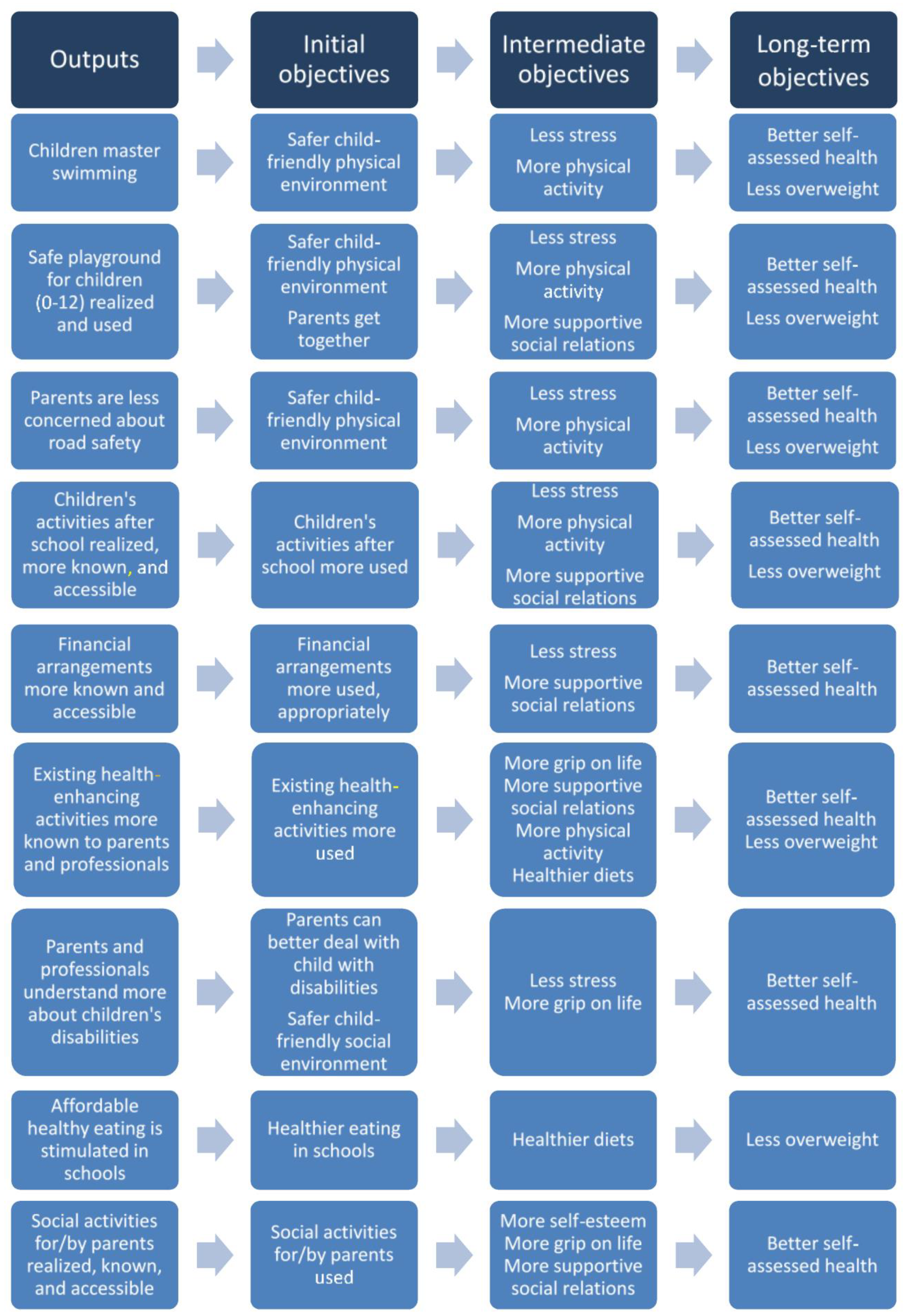
3.5. Integrating Parents’ Perceptions in Programme Plan Development
4. Discussion
4.1. Our Main Results
4.2. Comparisons with Existing Literature
4.3. Methodological Reflections
4.4. Strengths and Limitations
4.5. Recommendations
4.5.1. For Health Policymakers
4.5.2. For Further Research and Research Funding
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marmot, M.; Allen, J.; Bell, R.; Goldblatt, P. Building of the global movement for health equity: From Santiago to Rio and beyond. Lancet 2012, 379, 181–188. [Google Scholar] [CrossRef] [Green Version]
- Mackenbach, J.P.; Valverde, J.R.; Artnik, B.; Bopp, M.; Brønnum-Hansen, H.; Deboosere, P.; Kalediene, R.; Kovács, K.; Leinsalu, M.; Martikainen, P.; et al. Trends in health inequalities in 27 European countries. Proc. Natl. Acad. Sci. USA 2018, 115, 6440–6445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- RIVM. National Institute for Public Health and the Environment. Public Health Foresight Study 2018. Health Inequalities. Available online: https://www.vtv2018.nl/gezondheidsverschillen (accessed on 20 January 2021).
- Ball, K. Traversing myths and mountains: Addressing socioeconomic inequities in the promotion of nutrition and physical activity behaviours. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marmot, M.; Goldblatt, P.; Allen, J. Fair Society Healthy Lives (The Marmot Review). Available online: http://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review (accessed on 20 January 2021).
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.; Taylor, S. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Fransen, G.; Molleman, G. Hoe Kan Preventief Gezondheidsbeleid Voor Volwassenen in de Leeftijd 30 Tot 65 in Wijchen Eruit Zien? [How Can Preventive Health Policy for Adults Aged 30–65 in Wijchen Look Like?]. 2013. Available online: https://academischewerkplaatsamphi.nl/wp-content/uploads/2016/06/rapport-preventief-gezondheidsbeleid-voor-volwassenen-in-Wijchen-definitief.pdf (accessed on 28 January 2021).
- Bartholomew, L.K.; Parcel, G.S.; Kok, G.; Gottlieb, N.H.; Fernández, M.E. Planning Health Promotion Programs an Intervention Mapping Approach, 3rd ed.; Jossey-Bass a Wiley Imprint: San Francisco, CA, USA, 2011. [Google Scholar]
- O’Mara-Eves, A.; Brunton, G.; McDaid, D.; Oliver, S.; Kavanagh, J.; Jamal, F.; Matosevic, T.; Hardenberg, A.; Thomas, J. Community engagement to reduce inequalities in health: A systematic review, meta-analysis and economic analysis. Public Health Res. 2013, 1, 1–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bronfenbrenner, U. The Ecology of Human Development: Experiments by Design and Nature; Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An Ecological Approach to Creating Active Living Communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef] [Green Version]
- Richard, L.; Potvin, L.; Kishchuk, N.; Prlic, H.; Green, L.W. Assessment of the Integration of the Ecological Approach in Health Promotion Programs. Am. J. Health Promot. 1996, 10, 318–328. [Google Scholar] [CrossRef]
- Novilla, M.L.B.; Barnes, M.D.; De La Cruz, N.G.; Williams, P.N.; Rogers, J. Public Health Perspectives on the Family. Fam. Community Health 2006, 29, 28–42. [Google Scholar] [CrossRef]
- Agurs-Collins, T.; Persky, S.; Paskett, E.D.; Barkin, S.L.; Meissner, H.I.; Nansel, T.; Arteaga, S.S.; Zhang, X.; Das, R.; Farhat, T. Designing and Assessing Multilevel Interventions to Improve Minority Health and Reduce Health Disparities. Am. J. Public Health 2019, 109, S86–S93. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.E.; Ruiter, R.A.C.; Markham, C.M.; Kok, G. Intervention Mapping: Theory and Evidence-Based Health Promotion Program Planning: Perspective and Examples. Front. Public Health 2019, 7, 209. [Google Scholar] [CrossRef] [Green Version]
- Green, L.W.; Kreuter, M.W. Health Program Planning: An Educational and Ecological Approach, 4th ed.; McGraw-Hill: New York, NY, USA, 2005. [Google Scholar]
- Brún, M.O.-D.; De Brún, T.; Okonkwo, E.; Bonsenge-Bokanga, J.-S.; Silva, M.M.D.A.; Ogbebor, F.; Mierzejewska, A.; Nnadi, L.; Van Weel-Baumgarten, E.; Van Weel, C.; et al. Using Participatory Learning & Action research to access and engage with ‘hard to reach’ migrants in primary healthcare research. BMC Health Serv. Res. 2015, 16, 25. [Google Scholar] [CrossRef] [Green Version]
- Vermeer, A.J.; Van Assema, P.; Janse, M.; Hesdahl, B.; De Vries, N.K. Duurzame wijkgerichte gezondheidsbevordering: Wat is het en welke factoren spelen een rol? Tijdschr. Gezondh. 2012, 90, 97–104. [Google Scholar] [CrossRef]
- Wagemakers, A.; Corstjens, R.; Koelen, M.; Vaandrager, L.; Riet, H.V.; Dijkshoorn, H. Participatory approaches to promote healthy lifestyles among Turkish and Moroccan women in Amsterdam. Promot. Educ. 2008, 15, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Naaldenberg, J. Healthy Aging in Complex Environments Exploring the Benefits of Systems Thinking for Health Promotion Practice. Ph.D. Thesis, Wageningen University and Research, Wageningen, The Netherlands, 2011. [Google Scholar]
- De Jong, M.A.J.G.; Wagemakers, A.; Koelen, M.A. We Don’t Assume that Everyone Has the Same Idea about Health, Do We? Explorative Study of Citizens’ Perceptions of Health and Participation to Improve Their Health in a Low Socioeconomic City District. Int. J. Environ. Res. Public Health 2020, 17, 4958. [Google Scholar] [CrossRef]
- Flinterman, F.; Bisscheroux, P.; Dijkema, P.; Hertog, F.D.; de Jong, M.; Vermeer, A.; Vosjan, M. Positieve Gezondheid en gezondheidspercepties van mensen met een lage SES. Tijdschr. Gezondh. 2019, 97, 96–105. [Google Scholar] [CrossRef] [Green Version]
- Wagemakers, A.; Koelen, M.; Van Nierop, P.; Meertens, Y.; Weijters, J.; Kloek, G. Actiebegeleidend onderzoek ter bevordering van intersectorale samenwerking en bewonersparticipatie. Tijdschr. Gezondh. 2007, 85, 23–31. [Google Scholar] [CrossRef]
- Municipal Health Service GGD Gelderland-Zuid. Neighbourhood monitor. Personal communication, 2012. [Google Scholar]
- Fonds NutsOhra. Programma Gezonde Toekomst Dichterbij. [Program Healthy Future Nearby]. 2014. Available online: https://www.fnozorgvoorkansen.nl/programma-gezonde-toekomst-dichterbij/ (accessed on 28 April 2021).
- Wink, G.; Broekhuisen, N.; Fransen, G. Handboek De Ronde van Samen met Inwoners Werken aan Gezondheid in de Wijk. [Handbook De Ronde van. Collaborating with Residents on Health in the Neighbourhood]. Available online: https://onderzoek.ggdgelderlandzuid.nl/handboek-de-ronde-van/de-ronde-van/ (accessed on 28 April 2021).
- De Vlaming, R. Construct a logic model. In Epidemiology in Public Health Practice, 1st ed.; Haveman-Nies, A., Jansen, S., van Oers, H., van’t Veer, P., Eds.; Academic Publishers: Wageningen, The Netherlands, 2010; pp. 159–183. [Google Scholar]
- Fransen, G.; Hiddink, G.; Koelen, M.; Van Dis, S.; Drenthen, A.; Van Binsbergen, J.; Van Woerkum, C. The development of a minimal intervention strategy to address overweight and obesity in adult primary care patients in The Netherlands. Fam. Pract. 2008, 25, i112–i115. [Google Scholar] [CrossRef] [Green Version]
- Vasileiou, K.; Barnett, J.; Thorpe, S.; Young, T. Characterising and justifying sample size sufficiency in interview-based studies: Systematic analysis of qualitative health research over a 15-year period. BMC Med. Res. Methodol. 2018, 18, 148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wewerinke, D.; Boersma, S.; Wolf, J. Gezondheid: Basis Voor Jouw Toekomst! Ontwikkeling van Een Een Gezondheidsbevorderende Interventie Voor en Door Dakloze Jongeren. [Health: Basis for Your Future! Development of a Health Promotion Intervention for and by Homeless Young People.]; Impuls—Onderzoekscentrum maatschappelijke zorg, Radboudumc: Nijmegen, The Netherlands, 2014. [Google Scholar]
- Brún, M.O.; De Brún, T.; O’Donnell, K.; Papadakaki, M.; Saridaki, A.; Lionis, C.; Burns, N.; Dowrick, C.; Gravenhorst, K.; Spiegel, W.; et al. Material practices for meaningful engagement: An analysis of participatory learning and action research techniques for data generation and analysis in a health research partnership. Health Expect. 2017, 21, 159–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leerlooijer, J.; Vet, E. Health promotion. In Epidemiology in Public Health Practice, 2nd ed.; Haveman-Nies, A., Jansen, M., van Oers, J., van ’t Veer, P., Eds.; Academic Publishers: Wageningen, The Netherlands, 2017. [Google Scholar]
- Nagelhout, G.E.; Hogeling, L.; Spruijt, R.; Postma, N.; De Vries, H. Barriers and Facilitators for Health Behavior Change among Adults from Multi-Problem Households: A Qualitative Study. Int. J. Environ. Res. Public Health 2017, 14, 1229. [Google Scholar] [CrossRef] [Green Version]
- De Brún, T.; De Brún, M.O.; Van Weel-Baumgarten, E.; Burns, N.; Dowrick, C.; Lionis, C.; O’Donnell, C.; Mair, F.; Papadakaki, M.; Saridaki, A.; et al. Using Participatory Learning & Action (PLA) research techniques for inter-stakeholder dialogue in primary healthcare: An analysis of stakeholders’ experiences. Res. Involv. Engag. 2017, 3, 28. [Google Scholar] [CrossRef] [Green Version]
- Muijsenbergh, M.E.T.C.V.D.; LeMaster, J.W.; Shahiri, P.; Brouwer, M.; Hussain, M.; Dowrick, C.; Papadakaki, M.; Lionis, C.; MacFarlane, A. Participatory implementation research in the field of migrant health: Sustainable changes and ripple effects over time. Health Expect. 2020, 23, 306–317. [Google Scholar] [CrossRef] [Green Version]
- Huber, M.; Van Vliet, M.; Giezenberg, M.; Winkens, B.; Heerkens, Y.; Dagnelie, P.C.; Knottnerus, J.A. Towards a ‘patient-centred’ operationalisation of the new dynamic concept of health: A mixed methods study. BMJ Open 2016, 6, e010091. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Huisman, M.; Wink, G.; Fransen, G.A.J.; Boersma, S.; van den Muijsenbergh, M.E.T.C. Startfoto Project Gezond Leven Wijchen Noord [Start Situation Program Northern Wijchen]; GGD Gelderland-Zuid: Nijmegen, The Netherlands, 2016. [Google Scholar]
- Ministry of Public Health, Wellbeing and Sports. Nationaal Preventieakkoord [Dutch National Prevention Agreement]. November 2018. Available online: https://www.rijksoverheid.nl/binaries/rijksoverheid/documenten/convenanten/2018/11/23/nationaal-preventieakkoord/nationaal-preventieakkoord.pdf (accessed on 28 April 2021).
- McEwen, C.A.; McEwen, B.S. Social Structure, Adversity, Toxic Stress, and Intergenerational Poverty: An Early Childhood Model. Annu. Rev. Sociol. 2017, 43, 445–472. [Google Scholar] [CrossRef]
- Ziol-Guest, K.M.; Duncan, G.J.; Kalil, A.; Boyce, W.T. Early childhood poverty, immune-mediated disease processes, and adult productivity. Proc. Natl. Acad. Sci. USA 2012, 109, 17289–17293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marmot, M.; Wilkinson, R.G. Social organization, stress, and health. In Social Determinants of Health; Oxford University Press: Oxford, UK, 2005. [Google Scholar] [CrossRef]
- Oxford Learner’s Dictionaries. Available online: https://www.oxfordlearnersdictionaries.com/definition/english/ (accessed on 26 January 2021).
- Mullainathan, S.; Shafir, E. Scarcity: Why Having too Little Means so Much; Time Books, Henry Holt & Company LLC: New York, NY, USA, 2013. [Google Scholar]
- Kate, J.T.; De Koster, W.; van der Waal, J. Why are Depressive Symptoms More Prevalent among the Less Educated? The Relevance of Low Cultural Capital and Cultural Entitlement. Sociol. Spectr. 2017, 37, 63–76. [Google Scholar] [CrossRef] [Green Version]
- Vissenberg, C.; Nierkens, V.; Uitewaal, P.J.M.; Middelkoop, B.J.C.; Nijpels, G.; Stronks, K. Development of the Social Network-Based Intervention Powerful Together with Diabetes Using Intervention Mapping. Front. Public Health 2017, 5, 334. [Google Scholar] [CrossRef] [Green Version]
- Renes, R.J.; Ronteltap, A.; Bukman, A.J. Leefstijladvies voor mensen met een lage SES. Bijblijven 2018, 34, 237–246. [Google Scholar] [CrossRef]
- Cleland, V.; Granados, A.; Crawford, D.; Winzenberg, T.; Ball, K. Effectiveness of interventions to promote physical activity among socioeconomically disadvantaged women: A systematic review and meta-analysis. Obes. Rev. 2012, 14, 197–212. [Google Scholar] [CrossRef] [Green Version]
- Stevens, J.; Pratt, C.; Boyington, J.; Nelson, C.; Truesdale, K.P.; Ward, D.S.; Lytle, L.; Sherwood, N.E.; Robinson, T.N.; Moore, S.M.; et al. Multilevel Interventions Targeting Obesity: Research Recommendations for Vulnerable Populations. Am. J. Prev. Med. 2017, 52, 115–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Den Broeder, L. Citizen Science for Health in All Policies. Engaging Communities in Knowledge Development. Ph.D. Thesis, Free University Amsterdam, Amsterdam, The Netherlands, 2017. Available online: https://www.publicatie-online.nl/files/2414/9969/2929/14659_-_Broeder_BNW_ONL.pdf (accessed on 27 January 2021).
- Trentacosta, C.J.; Irwin, J.L.; Crespo, L.M.; Beeghly, M. Financial hardship and parenting stress in families with young children with autism: Opportunities for preventive intervention. In Handbook of Parent-Implemented Interventions for Very Young Children with Autism; Siller, M., Morgan, L., Eds.; Springer: Cham, Switzerland, 2018; pp. 79–91. [Google Scholar] [CrossRef]
- Conger, R.D.; Donnellan, M.B. An Interactionist Perspective on the Socioeconomic Context of Human Development. Annu. Rev. Psychol. 2007, 58, 175–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baker, D.L.; Drapela, L.A. Mostly the mother: Concentration of adverse employment effects on mothers of children with autism. Soc. Sci. J. 2010, 47, 578–592. [Google Scholar] [CrossRef]
- Cidav, Z.; Marcus, S.C.; Mandell, D.S. Implications of Childhood Autism for Parental Employment and Earnings. Pediatrics 2012, 129, 617–623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaandrager, L.; Hogeling, L.; Crijns, C.; van Lonkhuijzen, R.; de Meere, F.; Hermens, N.; Snoek, H.; Raaijmakers, I.; Oosterkamp, E.; Koelen, M. Overkoepelend Evaluatieonderzoek Gezonde Toekomst Dichterbij. Eindrapportage. [Overarching Evaluation Study Healthy Future Nearby. Final Report]. 2020. Available online: https://edepot.wur.nl/538608 (accessed on 27 January 2021).
| Panel Session | Topic | Questions to Parents | Techniques |
|---|---|---|---|
| 1 | Family health needs that parents prioritised to be addressed in the programme | 1. What does being healthy in your neighbourhood mean for you and your family? 2a. What aspect of your own or your family’s health would you like to see improved? 2b. What is the most relevant need for (i) your own family and (ii) families in the neighbourhood? | |
| 2 | Factors influencing three priority health needs emerging in session 1 Lifestyle themes prioritised by parents | 1. What are the factors that facilitate or obstruct the improvement of family health for priority needs? 2. Which of the healthy lifestyle themes that the health organisations think are important (smoking, alcohol use, or healthy eating and physical activity) do you consider most relevant for families in the neighbourhood to address? |
|
| 3 | Factors influencing health behaviours | 1. What does healthy eating mean for you, and what do you need to eat more healthily, a. for you as parent? b. for your child(ren)? 2. What do you and your children need to be more physically active? 3. What helps you to relax in stressful periods? |
|
| 4 | Ideas for programme activities for health behaviours | 1. What are your ideas for solutions/programme activities for a. healthy eating, b. physical activity, c. relaxation? |
|
| 5 | Programme activity ideas prioritised by parents | 1. What activity will contribute most to family health in your neighbourhood? 2. In what activity do you see your family participating? 3. To which activities would you contribute? |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wink, G.; Fransen, G.; Huisman, M.; Boersma, S.; van Disseldorp, L.; van der Velden, K.; Wagemakers, A.; van den Muijsenbergh, M. ‘Improving Health through Reducing Stress’: Parents’ Priorities in the Participatory Development of a Multilevel Family Health Programme in a Low-Income Neighbourhood in The Netherlands. Int. J. Environ. Res. Public Health 2021, 18, 8145. https://doi.org/10.3390/ijerph18158145
Wink G, Fransen G, Huisman M, Boersma S, van Disseldorp L, van der Velden K, Wagemakers A, van den Muijsenbergh M. ‘Improving Health through Reducing Stress’: Parents’ Priorities in the Participatory Development of a Multilevel Family Health Programme in a Low-Income Neighbourhood in The Netherlands. International Journal of Environmental Research and Public Health. 2021; 18(15):8145. https://doi.org/10.3390/ijerph18158145
Chicago/Turabian StyleWink, Gerda, Gerdine Fransen, Merel Huisman, Sandra Boersma, Lieke van Disseldorp, Koos van der Velden, Annemarie Wagemakers, and Maria van den Muijsenbergh. 2021. "‘Improving Health through Reducing Stress’: Parents’ Priorities in the Participatory Development of a Multilevel Family Health Programme in a Low-Income Neighbourhood in The Netherlands" International Journal of Environmental Research and Public Health 18, no. 15: 8145. https://doi.org/10.3390/ijerph18158145
APA StyleWink, G., Fransen, G., Huisman, M., Boersma, S., van Disseldorp, L., van der Velden, K., Wagemakers, A., & van den Muijsenbergh, M. (2021). ‘Improving Health through Reducing Stress’: Parents’ Priorities in the Participatory Development of a Multilevel Family Health Programme in a Low-Income Neighbourhood in The Netherlands. International Journal of Environmental Research and Public Health, 18(15), 8145. https://doi.org/10.3390/ijerph18158145







