Reject Rates of Radiographic Images in Dentomaxillofacial Radiology: A Literature Review
Abstract
:1. Introduction
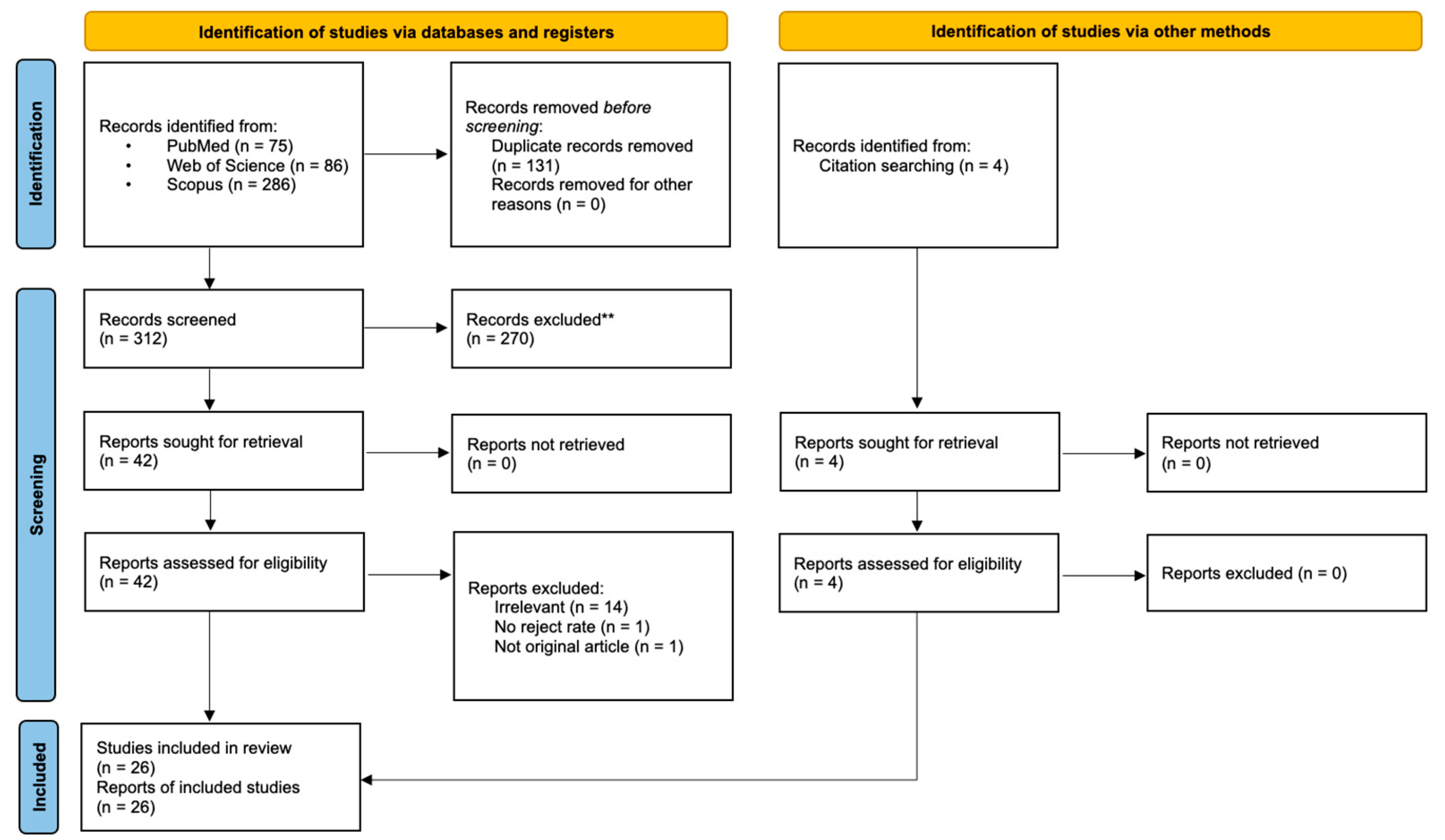
2. Materials and Methods
3. Results
3.1. Intra-Oral Radiography
3.2. Extra-Oral Radiography
3.3. CBCT
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Boeddinghaus, R.; Whyte, A. Trends in maxillofacial imaging. Clin. Radiol. 2018, 73, 4–18. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Wong, N.S.M. Medial Sigmoid Depression of the Mandibular Ramus as a Lesion-Mimicking Anatomical Variation: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4271. [Google Scholar] [CrossRef]
- Jaju, P.P.; Jaju, S.P. Cone-beam computed tomography: Time to move from ALARA to ALADA. Imaging Sci. Dent. 2015, 45, 263–265. [Google Scholar] [CrossRef] [Green Version]
- International Commission on Radiological Protection. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann. Icrp 2007, 37, 1–332. [Google Scholar]
- Oenning, A.C.; Jacobs, R.; Pauwels, R.; Stratis, A.; Hedesiu, M.; Salmon, B.; Group, D.R. Cone-beam CT in paediatric dentistry: DIMITRA project position statement. Pediatr. Radiol. 2018, 48, 308–316. [Google Scholar] [CrossRef]
- Yeung, A.W.K. The “As Low As Reasonably Achievable” (ALARA) principle: A brief historical overview and a bibliometric analysis of the most cited publications. Radioprotection 2019, 54, 103–109. [Google Scholar] [CrossRef]
- Shetty, A.; Almeida, F.T.; Ganatra, S.; Senior, A.; Pacheco-Pereira, C. Evidence on radiation dose reduction using rectangular collimation: A systematic review. Int. Dent. J. 2019, 69, 84–97. [Google Scholar] [CrossRef] [PubMed]
- Yeung, A.W.K.; Jacobs, R.; Bornstein, M.M. Novel low-dose protocols using cone beam computed tomography in dental medicine: A review focusing on indications, limitations, and future possibilities. Clin. Oral Investig. 2019, 23, 2573–2581. [Google Scholar] [CrossRef] [PubMed]
- American Dental Association Council on Scientific Affairs. The use of dental radiographs: Update and recommendations. J. Am. Dent. Assoc. 2006, 137, 1304–1312. [Google Scholar] [CrossRef] [PubMed]
- Bissoon, A.; QWhaites, E.; Moze, K.; Naidu, R. Evaluation of common operator errors in panoramic radiography in Trinidad and Tobago: A comparison of formally vs informally trained operators. West. Indian Med. J. 2012, 61, 733–738. [Google Scholar] [PubMed]
- Macleod, I.; Heath, N. Cone-beam computed tomography (CBCT) in dental practice. Dent. Update 2008, 35, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Acharya, S.; Pai, K.M.; Acharya, S. Repeat film analysis and its implications for quality assurance in dental radiology: An institutional case study. Contemp. Clin. Dent. 2015, 6, 392–395. [Google Scholar] [CrossRef]
- Behroozi, H.; Afkandeh, R. Causes of Repeating Digital Panoramic Radiographs in Maxillofacial Imaging Centers. J. Maz. Univ. Med. Sci. 2015, 25, 209–212. [Google Scholar]
- Benediktsdottir, I.; Hintze, H.; Petersen, J.; Wenzel, A. Image quality of two solid-state and three photostimulable phosphor plate digital panoramic systems, and treatment planning of mandibular third molar removal. Dentomaxillofac. Radiol. 2003, 32, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Chau, A.; Li, T.; Wong, J. A randomized double blinded study to assess the efficacy of a laser-guided collimator on dental radiography training. Dentomaxillofac. Radiol. 2006, 35, 200–204. [Google Scholar] [CrossRef]
- Ekstromer, K.; Hjalmarsson, L. Positioning errors in panoramic images in general dentistry in Sörmland County, Sweden. Swed. Dent. J. 2014, 38, 31–38. [Google Scholar]
- Gound, T.G.; DuBois, L.; Biggs, S.G. Factors that affect the rate of retakes for endodontic treatment radiographs. Oral Surg. Oral Med. Oral Pathol. 1994, 77, 514–518. [Google Scholar] [CrossRef]
- Gratt, B.M.; Sickles, E.A.; Littman, R.I. Comparison of dental xeroradiography and conventional film techniques for the frequency and significance of image artifacts. Oral Surg. Oral Med. Oral Pathol. 1985, 60, 546–552. [Google Scholar] [CrossRef]
- Greenall, C.; Thomas, B.; Drage, N.; Brown, J. An audit of image quality of three dental cone beam computed tomography units. Radiography 2016, 22, 56–59. [Google Scholar] [CrossRef]
- Habibi, Y.; Habibi, E.; Al-Nawas, B. Re-exposure in cone beam CT of the dentomaxillofacial region: A retrospective study. Dentomaxillofac. Radiol. 2019, 48, 20180184. [Google Scholar] [CrossRef]
- Hellén-Halme, K.; Johansson, P.-M.; Håkansson, J.; Petersson, A. Image quality of digital and film radiographs in applications sent to the Dental Insurance Office in Sweden for treatment approval. Swed. Dent. J. 2004, 28, 77–84. [Google Scholar]
- Hung, K.; Hui, L.; Yeung, A.W.K.; Scarfe, W.C.; Bornstein, M.M. Image retake rates of cone beam computed tomography in a dental institution. Clin. Oral Investig. 2020, 24, 4501–4510. [Google Scholar] [CrossRef]
- Jensen, T.W. Improved reliability of dental radiography by application of X-ray beam-guiding instruments: A two-year report. J. Dent. Educ. 1978, 42, 481–485. [Google Scholar] [CrossRef]
- Matzen, L.H.; Christensen, J.; Wenzel, A. Patient discomfort and retakes in periapical examination of mandibular third molars using digital receptors and film. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 107, 566–572. [Google Scholar] [CrossRef]
- Mupparapu, M.; Jariwala, S.; Singer, S.; Kim, I.; Janal, M. Comparison of re-exposure rates of intraoral radiographs between dental students and trained dental assistants in an oral and maxillofacial radiology clinic. Dentomaxillofac. Radiol. 2007, 36, 224–228. [Google Scholar] [CrossRef]
- Nenad, M.W.; Halupa, C.; Spolarich, A.E.; Gurenlian, J.R. A dental radiography checklist as a tool for quality improvement. J. Dent. Hyg. 2016, 90, 386–393. [Google Scholar]
- Nixon, P.; Thorogood, J.; Holloway, J.; Smith, N. An audit of film reject and repeat rates in a department of dental radiology. Br. J. Radiol. 1995, 68, 1304–1307. [Google Scholar] [CrossRef] [PubMed]
- Örtendahl, T.; Borrman, H.; Gröndahl, H. Quality assessment of lateral cephalograms amongst radiologists and orthodontists. Br. J. Orthod. 1994, 21, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Pachêco-Pereira, C.; Brandelli, J.; Senior, A. Re-exposure rates of digital intraoral images taken by undergraduate dental hygiene students. Can. J. Dent. Hyg. 2017, 51, 16–22. [Google Scholar]
- Parrott, L.; Ng, S. A comparison between bitewing radiographs taken with rectangular and circular collimators in UK military dental practices: A retrospective study. Dentomaxillofac. Radiol. 2011, 40, 102–109. [Google Scholar] [CrossRef] [Green Version]
- Senior, A.; Winand, C.; Ganatra, S.; Lai, H.; Alsulfyani, N.; Pachêco-Pereira, C. Digital Intraoral Imaging Re-Exposure Rates of Dental Students. J. Dent. Educ. 2018, 82, 61–68. [Google Scholar] [CrossRef]
- Sommers, T.M.; Mauriello, S.M.; Ludlow, J.B.; Platin, E.; Tyndall, D.A. Pre-clinical performance comparing intraoral film and CCD-based systems. J. Dent. Hyg. 2002, 76, 26–33. [Google Scholar]
- Spin-Neto, R.; Matzen, L.H.; Schropp, L.; Gotfredsen, E.; Wenzel, A. Factors affecting patient movement and re-exposure in cone beam computed tomography examination. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 119, 572–578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szymkowiak, L.; Sarll, D.; Horner, K. Some factors affecting the standards of radiography in general dental practice. Br. Dent. J. 1995, 179, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Van Acker, J.W.; Jacquet, W.; Dierens, M.; Martens, L.C. A reject analysis of cone-beam CTs in under-aged patients. Dentomaxillofac. Radiol. 2019, 48, 20180138. [Google Scholar] [CrossRef]
- Versteeg, C.; Sanderink, G.; Van Ginkel, F.; Van der Stelt, P. An evaluation of periapical radiography with a charge-coupled device. Dentomaxillofac. Radiol. 1998, 27, 97–101. [Google Scholar] [CrossRef]
- Yusof, M.Y.P.M.; Rahman, N.L.A.; Asri, A.A.A.; Othman, N.I.; Mokhtar, I.W. Repeat analysis of intraoral digital imaging performed by undergraduate students using a complementary metal oxide semiconductor sensor: An institutional case study. Imaging Sci. Dent. 2017, 47, 233–239. [Google Scholar] [CrossRef] [Green Version]
- Arai, Y.; Tammisalo, E.; Iwai, K.; Hashimoto, K.; Shinoda, K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac. Radiol. 1999, 28, 245–248. [Google Scholar] [CrossRef]
- Mozzo, P.; Procacci, C.; Tacconi, A.; Martini, P.T.; Andreis, I.B. A new volumetric CT machine for dental imaging based on the cone-beam technique: Preliminary results. Eur. Radiol. 1998, 8, 1558–1564. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.; Packota, G.; Major, P.; Flores-Mir, C. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: A systematic review. Dentomaxillofac. Radiol. 2008, 37, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Horner, K. Quality assurance: 1. Reject analysis, operator technique and the X-ray set. Dent. Update 1992, 19, 75–80. [Google Scholar] [PubMed]
- White, S.; Pharaoh, M. Oral Radiology Principles and Interpretation, 5th ed.; Mosby: St. Louis, MO, USA, 2004. [Google Scholar]
- Spin-Neto, R.; Wenzel, A. Patient movement and motion artefacts in cone beam computed tomography of the dentomaxillofacial region: A systematic literature review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 121, 425–433. [Google Scholar] [CrossRef]
- Bontempi, M.; Bettuzzi, M.; Casali, F.; Pasini, A.; Rossi, A.; Ariu, M. Relevance of head motion in dental cone-beam CT scanner images depending on patient positioning. Int. J. Comput. Assist. Radiol. Surg. 2008, 3, 249–255. [Google Scholar] [CrossRef]
- Yildizer Keris, E.; Demirel, O.; Ozdede, M. Evaluation of motion artifacts in cone-beam computed tomography with three different patient positioning. Oral Radiol. 2020, 37, 276–281. [Google Scholar] [CrossRef]
- Spin-Neto, R.; Hauge Matzen, L.; Hermann, L.; Fuglsig, J.M.d.C.e.S.; Wenzel, A. Head motion and perception of discomfort by young children during simulated CBCT examinations. Dentomaxillofac. Radiol. 2021, 50, 20200445. [Google Scholar] [CrossRef]
| Study | Modality | Reject N | Total N | Reject % | Receptor Type | FFD (cm) | Collimator | Operator | Patient Age | Factors Associated with Reject Rate (A < B Means B Had Higher Reject Rate) | Common Errors Leading to Reject (Account for >5%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Jensen (1978) [24] | FMX (14 Peri + 4 BW) | 300 | 5076 | 5.91 | Film | 40 | Circular | Dental undergrads | Adults | Additional teaching; Ant < Post; work experience | Positioning |
| Gratt (1985) [19] | FMX (21) | 130 | 1220 | 10.66 | Film; xeroradiography | 43 | N.A. | N.A. | >21 y | Film < xeroradiography | N.A. |
| Gound (1994) [18] | Peri (for endo) | 92 | 402 | 22.89 | Film | N.A. | N.A. | Dental undergrads | Adults | Md < Mx; EndoRay < hemostat | N.A. |
| Nixon (1995) [28] | BW | 39 | 1999 | 1.95 | Film | N.A. | N.A. | Multiple levels | All age | Radiographer < undergrad & dentist < radiographer student & postgrad | Positioning |
| Peri | 163 | 6313 | 2.58 | ||||||||
| Szymkowiak (1995) [35] | Peri + BW | 119 | 305 | 39.02 | Film | N.A. | N.A. | Dentists | N.A. | N.A. | Positioning; horizontal angulation; cone cut; vertical angulation; density and contrast |
| Versteeg (1998) [37] | Peri | 34 | 100 | 34.00 | Film; IO sensor | N.A. | Rectangular | Radiographers | N.A. | Film < IO sensor | N.A. |
| Sommers (2002) [33] | FMX (14 Peri + 4 BW) | 371 | 1008 | 36.81 | Film; IO sensor | N.A. | N.A. | DH students | Manikin | Film < IO sensor | N.A. |
| Hellen-Halme (2004) [22] | Peri + BW | 878 | 4657 | 18.85 | Film (mainly); digital | N.A. | N.A. | Dentists | >65 y | Film < digital | Positioning |
| Chau (2006) [16] | Peri + BW | 418 | 2334 | 17.91 | Film | N.A. | Rectangular | DH students | >8 y | Laser guided collimator < standard; work experience | N.A. |
| Mupparapu (2007) [26] | Peri + BW | 1017 | 34312 | 2.96 | Film | N.A. | Rectangular | Dental undergrads; dental surgery assistants | N.A. | Staff < student | N.A. |
| Matzen (2009) [25] | Peri (of lower 8 s) | 98 | 298 | 32.89 | IO sensor; PSP | N.A. | Rectangular | N.A. | >18 y | Women < men; discomfort; X-ray system | Positioning |
| Parrott (2011) [31] | BW | 374 | 3000 | 12.47 | Film | N.A. | Both | N.A. | Adult | N.A. | Vertical distortion; horizontal angulation |
| Acharya (2015) [13] | Peri + BW | 677 | 9495 | 7.13 | Film | N.A. | Rectangular | Multiple levels | N.A. | Md < Mx | N.A. |
| Nenad (2016) [27] | BW | 183 | 660 | 27.73 | N.A. | N.A. | N.A. | DH students | N.A. | Work experience | N.A. |
| Pacheco-Pereira (2017) [30] | BW | 90 | 1296 | 6.94 | IO sensor; PSP | N.A. | Rectangular | DH students | All age | PSP < IO sensor | Positioning; cone cut; patient not biting |
| Peri | 33 | 590 | 5.59 | ||||||||
| Yusof (2017) [38] | BW | 345 | 2284 | 15.11 | IO sensor | N.A. | N.A. | Dental undergrads | N.A. | N.A. | Positioning |
| Peri | 1978 | 5746 | 34.42 | ||||||||
| Senior (2018) [32] | BW | 632 | 5540 | 11.41 | IO sensor; PSP | 40 | Rectangular | Dental undergrads | All age | PSP < IO sensor | Positioning; cone cut; horizontal angulation |
| Peri | 429 | 3814 | 11.25 |
| Study | Modality | Reject N | Total N | Reject % | Receptor Type | Operator | Patient Age | Factors Associated with Reject Rate (A < B Means B Had Higher Reject Rate) | Common Errors Leading to Reject (Account for >5%) |
|---|---|---|---|---|---|---|---|---|---|
| Ortendahl (1994) [29] | Lat ceph (for orthodontics) | 33 | 240 | 13.75 | Film | N.A. | N.A. | N.A. | N.A. |
| Nixon (1995) [28] | Pan | 212 | 6395 | 3.32 | Film | Multiple levels | All age | N.A. | Positioning; patient movement |
| Lat ceph | 41 | 978 | 4.19 | ||||||
| Benediktsdottir (2003) [15] | Pan (for lower 8 s) | 38 | 497 | 7.65 | Digital | Radiographers | 18–44 y | X-ray system | N.A. |
| Hellen-Halme (2004) [22] | Pan | 24 | 206 | 11.65 | Film; digital | Dentists | >65 y | N.A. | Unsharpness; contrast too low |
| Ekstromer (2014) [17] | Pan | 55 | 1904 | 2.89 | Film; digital | N.A. | All age | N.A. | N.A. |
| Acharya (2015) [13] | All EO | 137 | 2339 | 5.86 | Film | Multiple levels | N.A. | Radiographers < Dental postgrads | Positioning; improper exposure; patient movement; improper bite; film fog |
| Behroozi (2015) [14] | Pan | 153 | 2751 | 5.56 | Digital | N.A. | N.A. | N.A. | Positioning; not sticking the tongue to the hard palate |
| Study | Reject N | Total N | Reject % | Patient Posture | Stabilizer | Scan Time | Operator | Patient Age | Factors Associated with Reject Rate (A < B Means B Had Higher Reject Rate) | Common Errors Leading to Reject (Account for >5%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Spin-Neto (2015) [34] | 16 | 248 | 6.45 | Seated | Chin rest; head clamp | 17–22 s | N.A. | All age | Small FOV < large FOV | Inadequate FOV |
| Greenall (2016) [20] | 29 | 1010 | 2.87 | N.A. | Chin rest; head strap | 18–40 s | Radiographers | 5–80 y | X-ray system; Md < Mx | Patient movement; inadequate FOV |
| Habibi (2019) [21] | 82 | 4986 | 1.64 | N.A. | N.A. | N.A. | N.A. | All age | Large FOV < small FOV | Patient movement |
| Van Acker (2019) [36] | 16 | 79 | 20.25 | N.A. | N.A. | N.A. | N.A. | <12 y | N.A. | N.A. |
| Hung (2020) [23] | 80 | 1737 | 4.61 | N.A. | N.A. | N.A. | Dentists | All age | X-ray system; Adult < under 12 y | Patient movement; inadequate FOV |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeung, A.W.K.; Wong, N.S.M. Reject Rates of Radiographic Images in Dentomaxillofacial Radiology: A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 8076. https://doi.org/10.3390/ijerph18158076
Yeung AWK, Wong NSM. Reject Rates of Radiographic Images in Dentomaxillofacial Radiology: A Literature Review. International Journal of Environmental Research and Public Health. 2021; 18(15):8076. https://doi.org/10.3390/ijerph18158076
Chicago/Turabian StyleYeung, Andy Wai Kan, and Natalie Sui Miu Wong. 2021. "Reject Rates of Radiographic Images in Dentomaxillofacial Radiology: A Literature Review" International Journal of Environmental Research and Public Health 18, no. 15: 8076. https://doi.org/10.3390/ijerph18158076
APA StyleYeung, A. W. K., & Wong, N. S. M. (2021). Reject Rates of Radiographic Images in Dentomaxillofacial Radiology: A Literature Review. International Journal of Environmental Research and Public Health, 18(15), 8076. https://doi.org/10.3390/ijerph18158076






