Short and Long-Term Innovations on Dietary Behavior Assessment and Coaching: Present Efforts and Vision of the Pride and Prejudice Consortium
Abstract
:1. Introduction
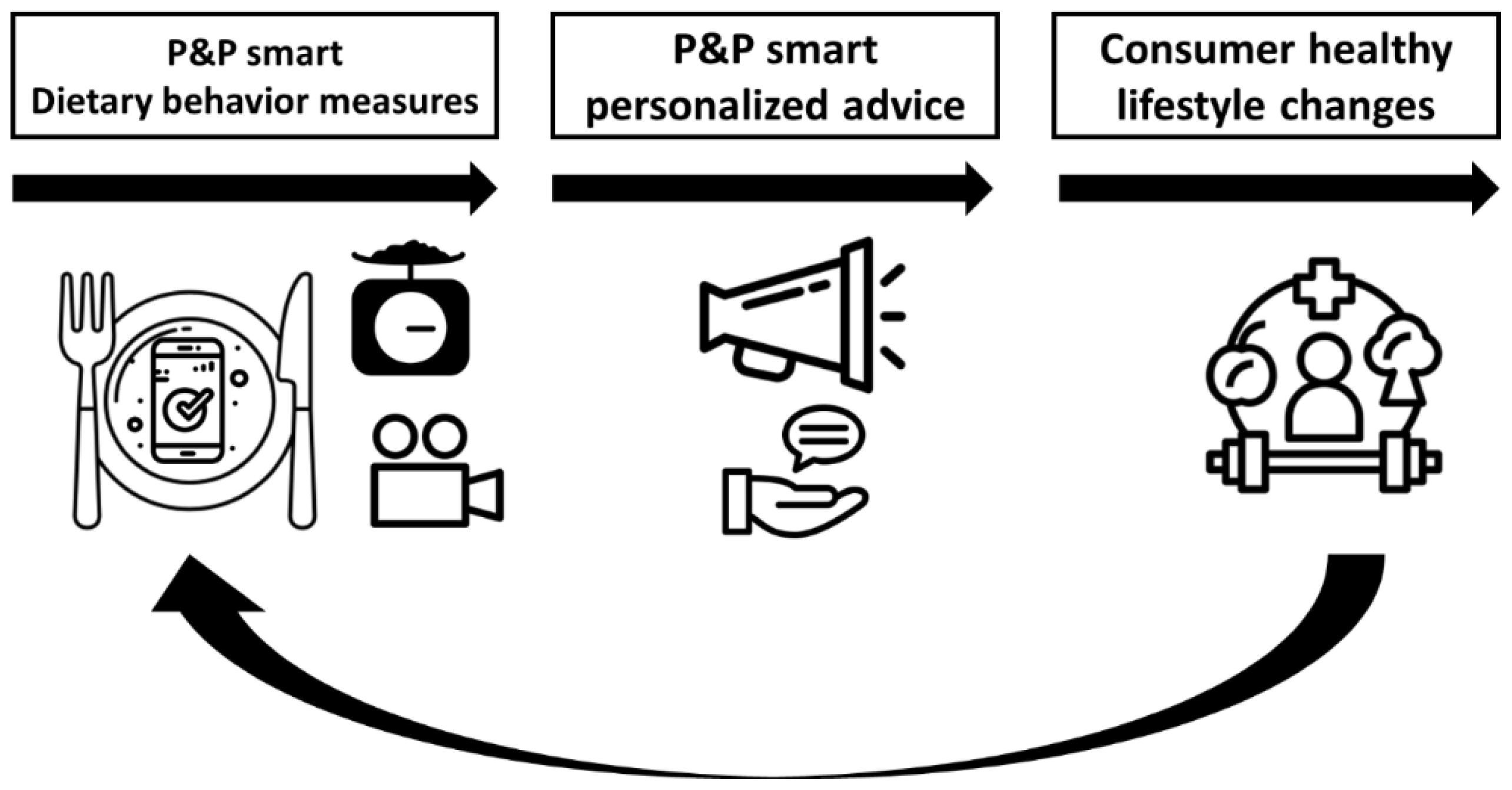
2. The Pride & Prejudice Consortium
3. Current Tools to Assess Dietary Intake
4. Current tools to Assess Eating Behavior
4.1. Individual Eating Behavior
4.2. Social Eating Behavior
5. Technology to Improve Measures of Dietary Behavior
5.1. Image and Spectroscopy to Improve Dietary Intake Measures
5.2. Conversational Agents to Improve Dietary Intake Measures
5.3. Video Image Analysis and Sensors to Improve Eating Behavior Measures
6. Technology to Improve Personalized Dietary Behavior Interventions
6.1. Conversational Agents for Stimulating Dietary Behavior Change
6.2. Game-Elements to Improve Dietary Behavior Interventions
6.3. Targeted Dietary Interventions during Food Shopping
6.4. Tailored Dietary Behavior Interventions
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blakely, T. Major strides in forecasting future health. Lancet 2018, 392, e14–e15. [Google Scholar] [CrossRef] [Green Version]
- Gezondheidsraad. Richtlijnen Goede Voeding 2015; Gezondheidsraad: Den Haag, The Netherlands, 2015. [Google Scholar]
- van Rossum, C.T.M.; Buurma-Rethans, E.J.M.; Dinnissen, C.S.; Beukers, M.H.; Brants, H.A.M.; Dekkers, A.L.M.; Ocke, M.C. The Diet of the Dutch. Results of the Dutch National Food Consumption Survey 2012–2016; National Institute for Public Health and the Environment: Bilthoven, The Netherlands, 2020. [Google Scholar]
- Berthoud, H.R. The neurobiology of food intake in an obesogenic environment. Proc. Nutr. Soc. 2012, 71, 478–487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- French, S.A.; Epstein, L.H.; Jeffery, R.W.; Blundell, J.E.; Wardle, J. Eating behavior dimensions. Associations with energy intake and body weight. A review. Appetite 2012, 59, 541–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viskaal-van Dongen, M.; Kok, F.J.; de Graaf, C. Eating rate of commonly consumed foods promotes food and energy intake. Appetite 2011, 56, 25–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohkuma, T.; Hirakawa, Y.; Nakamura, U.; Kiyohara, Y.; Kitazono, T.; Ninomiya, T. Association between eating rate and obesity: A systematic review and meta-analysis. Int. J. Obes. 2015, 39, 1589–1596. [Google Scholar] [CrossRef]
- Robinson, E.; Almiron-Roig, E.; Rutters, F.; de Graaf, C.; Forde, C.G.; Smith, C.T.; Nolan, S.J.; Jebb, S.A. A systematic review and meta-analysis examining the effect of eating rate on energy intake and hunger. Am. J. Clin. Nutr. 2014, 100, 123–151. [Google Scholar] [CrossRef] [Green Version]
- Hill, J.O.; Wyatt, H.R.; Reed, G.W.; Peters, J.C. Obesity and the environment: Where do we go from here? Science 2003, 299, 853–855. [Google Scholar] [CrossRef] [Green Version]
- Rolls, B.J. The relationship between dietary energy density and energy intake. Physiol. Behav. 2009, 97, 609–615. [Google Scholar] [CrossRef] [Green Version]
- De Graaf, C.; Kok, F.J. Slow food, fast food and the control of food intake. Nat. Rev. Endocrinol. 2010, 6, 290. [Google Scholar] [CrossRef]
- Eaton, S.B.; Konner, M. A consideration of its nature and current implications. N. Engl. J. Med. 1985, 312, 283–289. [Google Scholar] [CrossRef]
- Cordain, L.; Eaton, S.B.; Sebastian, A.; Mann, N.; Lindeberg, S.; Watkins, B.A.; O’Keefe, J.H.; Brand-Miller, J. Origins and evolution of the Western diet: Health implications for the 21st century. Am. J. Clin. Nutr. 2005, 81, 341–354. [Google Scholar] [CrossRef] [PubMed]
- Krop, E.M.; Hetherington, M.M.; Nekitsing, C.; Miquel, S.; Postelnicu, L.; Sarkar, A. Influence of oral processing on appetite and food intake-A systematic review and meta-analysis. Appetite 2018, 125, 253–269. [Google Scholar] [CrossRef] [PubMed]
- Lasschuijt, M.P.; Mars, M.; Stieger, M.; Miquel-Kergoat, S.; de Graaf, C.; Smeets, P. Comparison of oro-sensory exposure duration and intensity manipulations on satiation. Physiol. Behav. 2017, 176, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Zijlstra, N.; Mars, M.; de Wijk, R.A.; Westerterp-Plantenga, M.S.; de Graaf, C. The effect of viscosity on ad libitum food intake. Int. J. Obes. 2008, 32, 676–683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bolhuis, D.P.; Forde, C.G. Application of food texture to moderate oral processing behaviors and energy intake. Trends Food Sci. Technol. 2020, 106, 445–456. [Google Scholar] [CrossRef]
- Kelly, M.P.; Barker, M. Why is changing health-related behaviour so difficult? Public Health 2016, 136, 109–116. [Google Scholar] [CrossRef] [Green Version]
- Al-Awadhi, B.; Fallaize, R.; Zenun Franco, R.; Hwang, F.; Lovegrove, J.A. Insights into the Delivery of Personalized Nutrition: Evidence from Face-to-Face and Web-Based Dietary Interventions. Front. Nutr. 2020, 7, 570531. [Google Scholar] [CrossRef] [PubMed]
- Payne, H.E.; Lister, C.; West, J.H.; Bernhardt, J.M. Behavioral functionality of mobile apps in health interventions: A systematic review of the literature. JMIR Mhealth Uhealth 2015, 3, e20. [Google Scholar] [CrossRef]
- Eldridge, A.L.; Piernas, C.; Illner, A.-K.; Gibney, M.J.; Gurinović, M.A.; De Vries, J.H.M.; Cade, J.E. Evaluation of New Technology-Based Tools for Dietary Intake Assessment—An ILSI Europe Dietary Intake and Exposure Task Force Evaluation. Nutrients 2019, 11, 55. [Google Scholar] [CrossRef] [Green Version]
- Maringer, M.; van’t Veer, P.; Klepacz, N.; Verain, M.C.D.; Normann, A.; Ekman, S.; Timotijevic, L.; Raats, M.M.; Geelen, A. User-documented food consumption data from publicly available apps: An analysis of opportunities and challenges for nutrition research. Nutr. J. 2018, 17, 59. [Google Scholar] [CrossRef]
- Brouwer-Brolsma, E.M.; Lucassen, D.; de Rijk, M.G.; Slotegraaf, A.; Perenboom, C.; Borgonjen, K.; Siebelink, E.; Feskens, E.J.M.; de Vries, J.H.M. Dietary Intake Assessment: From Traditional Paper-Pencil Questionnaires to Technology-Based Tools. In International Symposium on Environmental Software Systems; Springer: Berlin/Heidelberg, Germany, 2020; pp. 7–23. [Google Scholar]
- Bardus, M.; van Beurden, S.B.; Smith, J.R.; Abraham, C. A review and content analysis of engagement, functionality, aesthetics, information quality, and change techniques in the most popular commercial apps for weight management. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 1–9. [Google Scholar] [CrossRef] [Green Version]
- DiFilippo, K.N.; Huang, W.-H.; Andrade, J.E.; Chapman-Novakofski, K.M. The use of mobile apps to improve nutrition outcomes: A systematic literature review. J. Telemed. Telecare 2015, 21, 243–253. [Google Scholar] [CrossRef]
- Ferrara, G.; Kim, J.; Lin, S.; Hua, J.; Seto, E. A focused review of smartphone diet-tracking apps: Usability, functionality, coherence with behavior change theory, and comparative validity of nutrient intake and energy estimates. JMIR Mhealth Uhealth 2019, 7, e9232. [Google Scholar] [CrossRef]
- König, L.M.; Attig, C.; Franke, T.; Renner, B. Barriers to and Facilitators for Using Nutrition Apps: Systematic Review and Conceptual Framework. JMIR Mhealth Uhealth 2021, 9, e20037. [Google Scholar]
- Chang, T.-R.; Kaasinen, E.; Kaipainen, K. What influences users’ decisions to take apps into use? A framework for evaluating persuasive and engaging design in mobile apps for well-being. In Proceedings of the Proceedings of the 11th International Conference on Mobile and Ubiquitous Multimedia, Ulm, Germany, 4–6 December 2012; pp. 1–10. [Google Scholar]
- Peng, W.; Kanthawala, S.; Yuan, S.; Hussain, S.A. A qualitative study of user perceptions of mobile health apps. BioMed Cent. 2016, 16, 1158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Preece, J.; Sharp, H.; Rogers, Y. Interaction Design: Beyond Human-Computer Interaction; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Chen, J.; Lieffers, J.; Bauman, A.; Hanning, R.; Allman-Farinelli, M. Designing Health Apps to Support Dietetic Professional Practice and Their Patients: Qualitative Results From an International Survey. JMIR Mhealth Uhealth 2017, 5, e40. [Google Scholar] [CrossRef] [PubMed]
- Cambon, L. Health smart devices and applications…towards a new model of prevention? Eur. J. Public Health 2017, 27, 390–391. [Google Scholar] [CrossRef]
- McClung, H.L.; Ptomey, L.T.; Shook, R.P.; Aggarwal, A.; Gorczyca, A.M.; Sazonov, E.S.; Becofsky, K.; Weiss, R.; Das, S.K. Dietary Intake and Physical Activity Assessment: Current Tools, Techniques, and Technologies for Use in Adult Populations. Am. J. Prev. Med. 2018, 55, e93–e104. [Google Scholar] [CrossRef] [Green Version]
- Vu, T.; Lin, F.; Alshurafa, N.; Xu, W. Wearable Food Intake Monitoring Technologies: A Comprehensive Review. Computers 2017, 6, 4. [Google Scholar] [CrossRef]
- Forster, H.; Walsh, M.C.; Gibney, M.J.; Brennan, L.; Gibney, E.R. Personalised nutrition: The role of new dietary assessment methods. Proc. Nutr. Soc. 2016, 75, 96–105. [Google Scholar] [CrossRef] [Green Version]
- Lucassen, D.A.; Brouwer-Brolsma, E.M.; van de Wiel, A.M.; Siebelink, E.; Feskens, E.J. Iterative Development of an Innovative Smartphone-Based Dietary Assessment Tool: Traqq. J. Vis. Exp. 2021, 169, e62032. [Google Scholar]
- Oinas-Kukkonen, H.; Harjumaa, M. Persuasive systems design: Key issues, process model, and system features. Commun. Assoc. Inf. Syst. 2009, 24, 28. [Google Scholar] [CrossRef]
- Subar, A.F.; Freedman, L.S.; Tooze, J.A.; Kirkpatrick, S.I.; Boushey, C.; Neuhouser, M.L.; Thompson, F.E.; Potischman, N.; Guenther, P.M.; Tarasuk, V.; et al. Addressing Current Criticism Regarding the Value of Self-Report Dietary Data. J. Nutr. 2015, 145, 2639–2645. [Google Scholar] [CrossRef] [Green Version]
- Thompson, F.E.; Subar, A.F. Dietary Assessment Methodology. In Nutrition in the Prevention and Treatment of Disease; Elsevier Inc.: Amsterdam, The Netherlands, 2017; pp. 5–48. [Google Scholar]
- Ioakimidis, I.; Zandian, M.; Eriksson-Marklund, L.; Bergh, C.; Grigoriadis, A.; Sodersten, P. Description of chewing and food intake over the course of a meal. Physiol. Behav. 2011, 104, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Papapanagiotou, V.; Diou, C.; Zhou, L.; van den Boer, J.; Mars, M.; Delopoulos, A. A Novel Chewing Detection System Based on PPG, Audio, and Accelerometry. IEEE J. Biomed. Health Inform. 2017, 21, 607–618. [Google Scholar] [CrossRef] [PubMed]
- Lausberg, H.; Sloetjes, H. Coding gestural behavior with the NEUROGES-ELAN system. Behav. Res. Methods 2009, 41, 841–849. [Google Scholar] [CrossRef]
- Noldus Information Technology. Observer XT. Available online: https://www.noldus.com/observer-xt?gclid=Cj0KCQjwsqmEBhDiARIsANV8H3ZF1xKvZD3hx2eYpPV-rw75WQDKl1FCT7DTWeL6TZHFywrMdnXrY5AaAva9EALw_wcB (accessed on 29 April 2021).
- McCrickerd, K.; Lim, C.M.H.; Leong, C.; Chia, E.M.; Forde, C.G. Texture-Based Differences in Eating Rate Reduce the Impact of Increased Energy Density and Large Portions on Meal Size in Adults. J. Nutr. 2017, 147, 1208–1217. [Google Scholar] [CrossRef]
- Sazonov, E.; Schuckers, S.; Lopez-Meyer, P.; Makeyev, O.; Sazonova, N.; Melanson, E.L.; Neuman, M. Non-invasive monitoring of chewing and swallowing for objective quantification of ingestive behavior. Physiol. Meas. 2008, 29, 525–541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puig-Divi, A.; Escalona-Marfil, C.; Padulles-Riu, J.M.; Busquets, A.; Padulles-Chando, X.; Marcos-Ruiz, D. Validity and reliability of the Kinovea program in obtaining angles and distances using coordinates in 4 perspectives. PLoS ONE 2019, 14, e0216448. [Google Scholar] [CrossRef]
- Aguayo-Mendoza, M.G.; Ketel, E.C.; van der Linden, E.; Forde, C.G.; Piqueras-Fiszman, B.; Stieger, M. Oral processing behavior of drinkable, spoonable and chewable foods is primarily determined by rheological and mechanical food properties. Food Qual. Prefer. 2019, 71, 87–95. [Google Scholar] [CrossRef]
- Kohyama, K.; Hayakawa, F.; Gao, Z.; Ishihara, S.; Funami, T.; Nishinari, K. Natural eating behavior of two types of hydrocolloid gels as measured by electromyography: Quantitative analysis of mouthful size effects. Food Hydrocolloid 2016, 52, 243–252. [Google Scholar] [CrossRef]
- Fuentes, R.; Arias, A.; Lezcano, M.F.; Saravia, D.; Kuramochi, G.; Dias, F.J. Systematic Standardized and Individualized Assessment of Masticatory Cycles Using Electromagnetic 3D Articulography and Computer Scripts. Biomed. Res. Int. 2017, 2017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okada, A.; Honma, A.; Nomura, S.; Yamada, Y. Oral behavior from food intake until terminal swallow. Physiol. Behav. 2007, 90, 172–179. [Google Scholar] [CrossRef]
- Lee, J.; Woo, J.; Xing, F.X.; Murano, E.Z.; Stone, M.; Prince, J.L. Semi-automatic segmentation for 3D motion analysis of the tongue with dynamic MRI. Comput. Med. Imag. Grap. 2014, 38, 714–724. [Google Scholar] [CrossRef] [Green Version]
- de Lavergne, M.D.; van de Velde, F.; Stieger, M. Bolus matters: The influence of food oral breakdown on dynamic texture perception. Food Funct. 2017, 8, 464–480. [Google Scholar] [CrossRef] [Green Version]
- Lewinski, P.; den Uyl, T.M.; Butler, C. Automated Facial Coding: Validation of Basic Emotions and FACS AUs in FaceReader. J. Neurosci. Psychol. Econ. 2014, 7, 227–236. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Cao, Y.; Luo, Y.; Chen, G.L.; Vokkarane, V.; Ma, Y.S.; Chen, S.Q.; Hou, P. A New Deep Learning-Based Food Recognition System for Dietary Assessment on An Edge Computing Service Infrastructure. IEEE Trans. Serv. Comput. 2018, 11, 249–261. [Google Scholar] [CrossRef]
- Mezgec, S.; Seljak, B.K. NutriNet: A Deep Learning Food and Drink Image Recognition System for Dietary Assessment. Nutrients 2017, 9, 657. [Google Scholar] [CrossRef] [PubMed]
- de Vries, R.A.; Haarman, J.A.; Harmsen, E.C.; Heylen, D.K.; Hermens, H.J. The Sensory Interactive Table: Exploring the Social Space of Eating. In Proceedings of the 2020 International Conference on Multimodal Interaction, Amsterdam, The Netherlands, 25–29 October 2020; pp. 689–693. [Google Scholar]
- Pesch, M.H.; Lumeng, J.C. Methodological considerations for observational coding of eating and feeding behaviors in children and their families. Int. J. Behav. Nutr. Phys. Act. 2017, 14. [Google Scholar] [CrossRef] [Green Version]
- Haarman, J.A.M.; de Vries, R.A.J.; Harmsen, E.C.; Hermens, H.J.; Heylen, D.K.J. Sensory Interactive Table (SIT)-Development of a Measurement Instrument to Support Healthy Eating in a Social Dining Setting. Sensors 2020, 20, 2636. [Google Scholar] [CrossRef]
- Kim, Y.; Singh, M.; Kays, S.E. Near-infrared spectroscopic analysis of macronutrients and energy in homogenized meals. Food Chem. 2007, 105, 1248–1255. [Google Scholar] [CrossRef]
- Boushey, C.J.; Spoden, M.; Zhu, F.M.; Delp, E.J.; Kerr, D.A. New mobile methods for dietary assessment: Review of image-assisted and image-based dietary assessment methods. Proc. Nutr. Soc. 2017, 76, 283–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ptomey, L.T.; Willis, E.A.; Honas, J.J.; Mayo, M.S.; Washburn, R.A.; Herrmann, S.D.; Sullivan, D.K.; Donnelly, J.E. Validity of energy intake estimated by digital photography plus recall in overweight and obese young adults. J. Acad. Nutr. Diet. 2015, 115, 1392–1399. [Google Scholar] [CrossRef] [Green Version]
- Elinder, L.; Brunosson, A.; Bergström, H.; Hagströmer, M.; Patterson, E. Validation of personal digital photography to assess dietary quality among people with intellectual disabilities. J. Intellect. Disabil. Res. 2012, 56, 221–226. [Google Scholar] [CrossRef]
- Ptomey, L.T.; Herrmann, S.D.; Lee, J.; Sullivan, D.K.; Rondon, M.F.; Donnelly, J.E. Photo-assisted recall increases estimates of energy and macronutrient intake in adults with intellectual and developmental disabilities. J. Acad. Nutr. Diet. 2013, 113, 1704–1709. [Google Scholar] [CrossRef] [Green Version]
- Ahmad, Z.; Kerr, D.A.; Bosch, M.; Boushey, C.J.; Delp, E.J.; Khanna, N.; Zhu, F. A Mobile Food Record for Integrated Dietary Assessment. MADiMa16 2016, 2016, 53–62. [Google Scholar] [CrossRef] [Green Version]
- Lo, F.P.W.; Sun, Y.; Qiu, J.; Lo, B. Image-Based Food Classification and Volume Estimation for Dietary Assessment: A Review. IEEE J. Biomed. Health Inform. 2020, 24, 1926–1939. [Google Scholar] [CrossRef]
- Chang, X.; Ye, H.; Albert, P.; Edward, D.; Nitin, K.; Carol, B. Image-Based Food Volume Estimation. CEA13 2013, 2013, 75–80. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.; Paliwal, J. Near-infrared spectroscopy and imaging in food quality and safety. Sens. Instrum. Food Qual. Saf. 2007, 1, 193–207. [Google Scholar] [CrossRef]
- Pallav, P.; Diamond, G.G.; Hutchins, D.A.; Green, R.J.; Gan, T.H. A Near-Infrared (NIR) Technique for Imaging Food Materials. J. Food Sci. 2009, 74, E23–E33. [Google Scholar] [CrossRef]
- Bickmore, T.; Kimani, E.; Trinh, H.; Pusateri, A.; Paasche-Orlow, M.; Magnani, J. Managing Chronic Conditions with a Smartphone-based Conversational Virtual Agent. In Proceedings of the 18th International Conference on Intelligent Virtual Agents, Sydney, Australia, 5–8 November 2018; pp. 119–124. [Google Scholar] [CrossRef]
- Bol, N.; Helberger, N.; Weert, J.C.M. Differences in mobile health app use: A source of new digital inequalities? Inf. Soc. 2018, 34, 183–193. [Google Scholar] [CrossRef] [Green Version]
- Fadhil, A. Can a Chatbot System Determine My Diet?: Addressing Challenges of Chatbot Application for Meal Recommendation. arXiv 2018, arXiv:1802.09100. [Google Scholar]
- Franco, R.Z.; Fallaize, R.; Lovegrove, J.A.; Hwang, F. Popular Nutrition-Related Mobile Apps: A Feature Assessment. JMIR Mhealth Uhealth 2016, 4, e85. [Google Scholar] [CrossRef] [PubMed]
- Graf, B.; Krüger, M.; Müller, F.; Ruhland, A.; Zech, A. Nombot: Simplify food tracking. In Proceedings of the 14th International Conference on Mobile and Ubiquitous Multimedia, Linz, Austria, 30 November–2 December 2015; pp. 360–363. [Google Scholar]
- Casas, J.; Mugellini, E.; Khaled, O.A. Food diary coaching chatbot. In Proceedings of the 2018 ACM International Joint Conference and 2018 International Symposium on Pervasive and Ubiquitous Computing and Wearable Computers, Singapore, 8–12 October 2018; pp. 1676–1680. [Google Scholar]
- Rusu, A.; Randriambelonoro, M.; Perrin, C.; Valk, C.; Alvarez, B.; Schwarze, A.K. Aspects Influencing Food Intake and Approaches towards Personalising Nutrition in the Elderly. J. Popul. Ageing 2020, 13, 239–256. [Google Scholar] [CrossRef] [Green Version]
- Forksy Website. Available online: https://getforksy.com/ (accessed on 26 February 2021).
- Farooq, M.; Doulah, A.; Parton, J.; McCrory, M.A.; Higgins, J.A.; Sazonov, E. Validation of Sensor-Based Food Intake Detection by Multicamera Video Observation in an Unconstrained Environment. Nutrients 2019, 11, 609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bell, B.M.; Alam, R.; Alshurafa, N.; Thomaz, E.; Mondol, A.S.; de la Haye, K.; Stankovic, J.A.; Lach, J.; Spruijt-Metz, D. Automatic, wearable-based, in-field eating detection approaches for public health research: A scoping review. NPJ Digit. Med. 2020, 3, 38. [Google Scholar] [CrossRef] [Green Version]
- Hossain, D.; Ghosh, T.; Sazonov, E. Automatic Count of Bites and Chews from Videos of Eating Episodes. IEEE Access 2020, 8, 101934–101945. [Google Scholar] [CrossRef]
- Kyritsis, K.; Tatli, C.L.; Diou, C.; Delopoulos, A. Automated analysis of in meal eating behavior using a commercial wristband IMU sensor. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju, Korea, 11–15 July 2017; pp. 2843–2846. [Google Scholar]
- Lin, B.; Hoover, A. A Comparison of Finger and Wrist Motion Tracking to Detect Bites during Food Consumption. In Proceedings of the 2019 IEEE 16th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Chicago, IL, USA, 19–22 May 2019; pp. 1–4. [Google Scholar]
- Kramer, L.L.; Ter Stal, S.; Mulder, B.C.; de Vet, E.; van Velsen, L. Developing Embodied Conversational Agents for Coaching People in a Healthy Lifestyle: Scoping Review. J. Med. Internet Res. 2020, 22, e14058. [Google Scholar] [CrossRef]
- Ruttkay, Z.; Pelachaud, C. From Brows to Trust: Evaluating Embodied Conversational Agents; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2006; Volume 7. [Google Scholar]
- Fadhil, A.; Gabrielli, S. Addressing challenges in promoting healthy lifestyles: The al-chatbot approach. In Proceedings of the 11th EAI International Conference on Pervasive Computing Technologies for Healthcare, Barcelona, Spain, 23–26 May 2017; pp. 261–265. [Google Scholar] [CrossRef]
- Fox, J.; Bailenson, J.; Binney, J. Virtual Experiences, Physical Behaviors: The Effect of Presence on Imitation of an Eating Avatar. Presence-Teleop Virt 2009, 18, 294–303. [Google Scholar] [CrossRef]
- ter Stal, S.; Kramer, L.L.; Tabak, M.; op den Akker, H.; Hermens, H. Design Features of Embodied Conversational Agents in eHealth: A Literature Review. Int. J. Hum.-Comput. Stud. 2020, 138, 102409. [Google Scholar] [CrossRef]
- Kramer, L.L.; Blok, M.; van Velsen, L.; Mulder, B.C.; de Vet, E. Supporting eating behaviour of community-dwelling older adults: Co-design of an embodied conversational agent. Des. Health 2021, 1–20. [Google Scholar] [CrossRef]
- Kramer, L.L.; Mulder, B.C.; van Velsen, L.; de Vet, E. Use and Effect of Web-Based Embodied Conversational Agents for Improving Eating Behavior and Decreasing Loneliness Among Community-Dwelling Older Adults: Protocol for a Randomized Controlled Trial. JMIR Res. Protoc. 2021, 10, e22186. [Google Scholar] [CrossRef]
- Schoeppe, S.; Alley, S.; Rebar, A.L.; Hayman, M.; Bray, N.A.; Van Lippevelde, W.; Gnam, J.-P.; Bachert, P.; Direito, A.; Vandelanotte, C. Apps to improve diet, physical activity and sedentary behaviour in children and adolescents: A review of quality, features and behaviour change techniques. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, T.; Ryan, C.; Hoyos-Cespedes, A.; Lu, A.S. Nutrition education and dietary behavior change games: A scoping review. Games Health J. 2019, 8, 153–176. [Google Scholar] [CrossRef] [PubMed]
- Sardi, L.; Idri, A.; Fernández-Alemán, J.L. A systematic review of gamification in e-Health. J. Biomed. Inform. 2017, 71, 31–48. [Google Scholar] [CrossRef]
- Alahäivälä, T.; Oinas-Kukkonen, H. Understanding persuasion contexts in health gamification: A systematic analysis of gamified health behavior change support systems literature. Int. J. Med Inform. 2016, 96, 62–70. [Google Scholar] [CrossRef]
- Johnson, D.; Deterding, S.; Kuhn, K.-A.; Staneva, A.; Stoyanov, S.; Hides, L. Gamification for health and wellbeing: A systematic review of the literature. Internet Interv. 2016, 6, 89–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nour, M.; Yeung, S.H.; Partridge, S.; Allman-Farinelli, M. A narrative review of social media and game-based nutrition interventions targeted at young adults. J. Acad. Nutr. Diet. 2017, 117, 735–752. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.; Bhatt, R.; Lazarus, M.; Cullen, K.; Baranowski, J.; Baranowski, T. A serious video game to increase fruit and vegetable consumption among elementary aged youth (Squire’s Quest! II): Rationale, design, and methods. JMIR Res. Protoc. 2012, 1, e2348. [Google Scholar] [CrossRef]
- Thompson, D. Incorporating behavioral techniques into a serious videogame for children. Games Health J. 2017, 6, 75–86. [Google Scholar] [CrossRef] [Green Version]
- Schnall, R.; Rojas, M.; Bakken, S.; Brown, W.; Carballo-Dieguez, A.; Carry, M.; Gelaude, D.; Mosley, J.P.; Travers, J. A user-centered model for designing consumer mobile health (mHealth) applications (apps). J. Biomed. Inform. 2016, 60, 243–251. [Google Scholar] [CrossRef]
- McCurdie, T.; Taneva, S.; Casselman, M.; Yeung, M.; McDaniel, C.; Ho, W.; Cafazzo, J. mHealth consumer apps: The case for user-centered design. Biomed. Instrum. Technol. 2012, 46, 49–56. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, M.; Oh, A.; Vanderlee, L.; Franco-Arellano, B.; Schermel, A.; Lou, W.; L’Abbé, M.R. A randomized controlled trial examining consumers’ perceptions and opinions on using different versions of a FoodFlip© smartphone application for delivery of nutrition information. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 22. [Google Scholar] [CrossRef] [PubMed]
- López, D.; Torres, M.; Vélez, J.; Grullon, J.; Negrón, E.; Pérez, C.M.; Palacios, C. Development and evaluation of a nutritional smartphone application for making smart and healthy choices in grocery shopping. Healthc. Inform. Res. 2017, 23, 16. [Google Scholar] [CrossRef] [PubMed]
- Samoggia, A.; Riedel, B. Assessment of nutrition-focused mobile apps’ influence on consumers’ healthy food behaviour and nutrition knowledge. Food Res. Int. 2020, 128, 108766. [Google Scholar] [CrossRef]
- Voedingscentrum. Voedingscentrum-app ‘Kies Ik Gezond?’. Available online: https://www.voedingscentrum.nl/nl/thema/apps-en-tools-voedingscentrum/kies-ik-gezond-.aspx (accessed on 24 June 2021).
- Flaherty, S.-J.; McCarthy, M.; Collins, A.; McAuliffe, F. Can existing mobile apps support healthier food purchasing behaviour? Content analysis of nutrition content, behaviour change theory and user quality integration. Public Health Nutr. 2018, 21, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Flaherty, S.J.; McCarthy, M.B.; Collins, A.M.; McAuliffe, F.M. A different perspective on consumer engagement: Exploring the experience of using health apps to support healthier food purchasing. J. Mark. Manag. 2019, 35, 310–337. [Google Scholar] [CrossRef]
- Gilliland, J.; Sadler, R.; Clark, A.; O’Connor, C.; Milczarek, M.; Doherty, S. Using a smartphone application to promote healthy dietary behaviours and local food consumption. Biomed. Res. Int. 2015, 2015. [Google Scholar] [CrossRef] [Green Version]
- Palacios, C.; Torres, M.; López, D.; Trak-Fellermeier, M.A.; Coccia, C.; Pérez, C.M. Effectiveness of the nutritional app “mynutricart” on food choices related to purchase and dietary behavior: A pilot randomized controlled trial. Nutrients 2018, 10, 1967. [Google Scholar] [CrossRef] [Green Version]
- Adams, S.H.; Anthony, J.C.; Carvajal, R.; Chae, L.; Khoo, C.S.H.; Latulippe, M.E.; Matusheski, N.V.; McClung, H.L.; Rozga, M.; Schmid, C.H. Perspective: Guiding principles for the implementation of personalized nutrition approaches that benefit health and function. Adv. Nutr. 2020, 11, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Celis-Morales, C.; Livingstone, K.M.; Marsaux, C.F.; Macready, A.L.; Fallaize, R.; O’Donovan, C.B.; Woolhead, C.; Forster, H.; Walsh, M.C.; Navas-Carretero, S. Effect of personalized nutrition on health-related behaviour change: Evidence from the Food4me European randomized controlled trial. Int. J. Epidemiol. 2017, 46, 578–588. [Google Scholar] [CrossRef] [Green Version]
- Spruijt-Metz, D.; Wen, C.K.; O’Reilly, G.; Li, M.; Lee, S.; Emken, B.; Mitra, U.; Annavaram, M.; Ragusa, G.; Narayanan, S. Innovations in the use of interactive technology to support weight management. Curr. Obes. Rep. 2015, 4, 510–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terzimehić, N.; Schneegass, C.; Hußmann, H. Exploring Challenges in Automated Just-In-Time Adaptive Food Choice Interventions. In Proceedings of the 2nd International Workshop on Multimedia for Personal Health and Health Care, Mountain View, CA, USA, 23 October 2017; pp. 81–84. [Google Scholar]
- Nahum-Shani, I.; Hekler, E.B.; Spruijt-Metz, D. Building health behavior models to guide the development of just-in-time adaptive interventions: A pragmatic framework. Health Psychol. 2015, 34, 1209. [Google Scholar] [CrossRef]
- Wang, L.; Miller, L.C. Just-in-the-moment adaptive interventions (JITAI): A meta-analytical review. Health Commun. 2020, 35, 1531–1544. [Google Scholar] [CrossRef]
- Lyzwinski, L.N. A systematic review and meta-analysis of mobile devices and weight loss with an intervention content analysis. J. Pers. Med. 2014, 4, 311–385. [Google Scholar] [CrossRef] [Green Version]
- Hartmann-Boyce, J.; Johns, D.J.; Jebb, S.A.; Aveyard, P.; Behavioural Weight Management Review Group. Effect of behavioural techniques and delivery mode on effectiveness of weight management: Systematic review, meta-analysis and meta-regression. Obes. Rev. 2014, 15, 598–609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dombrowski, S.U.; Sniehotta, F.F.; Avenell, A.; Johnston, M.; MacLennan, G.; Araújo-Soares, V. Identifying active ingredients in complex behavioural interventions for obese adults with obesity-related co-morbidities or additional risk factors for co-morbidities: A systematic review. Health Psychol. Rev. 2012, 6, 7–32. [Google Scholar] [CrossRef] [Green Version]
- Ter Borg, S.; Koopman, N.; Verkaik-Kloosterman, J. Food consumption, nutrient intake and status during the first 1000 days of life in the netherlands: A systematic review. Nutrients 2019, 11, 860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sporrel, K.; Nibbeling, N.; Wang, S.; Ettema, D.; Simons, M. Unraveling Mobile Health Exercise Interventions for Adults: Scoping Review on the Implementations and Designs of Persuasive Strategies. JMIR Mhealth Uhealth 2021, 9, e16282. [Google Scholar] [CrossRef]
- Lippke, S.; Ziegelmann, J.P. Theory-based health behavior change: Developing, testing, and applying theories for evidence-based interventions. Appl. Psychol. 2008, 57, 698–716. [Google Scholar] [CrossRef]
- Looman, M.; Van den Berg, C.; Geelen, A.; Samlal, R.A.; Heijligenberg, R.; Klein Gunnewiek, J.M.; Balvers, M.G.; Leendertz-Eggen, C.L.; Wijnberger, L.D.; Feskens, E.J. Supplement use and dietary sources of folate, vitamin D, and n-3 fatty acids during preconception: The GLIMP2 study. Nutrients 2018, 10, 962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kind, K.L.; Moore, V.M.; Davies, M.J. Diet around conception and during pregnancy–effects on fetal and neonatal outcomes. Reprod. Biomed. Online 2006, 12, 532–541. [Google Scholar] [CrossRef]
- Clohessy, S.; Walasek, L.; Meyer, C. Factors influencing employees’ eating behaviours in the office-based workplace: A systematic review. Obes. Rev. 2019, 20, 1771–1780. [Google Scholar] [CrossRef]
- Jastran, M.M.; Bisogni, C.A.; Sobal, J.; Blake, C.; Devine, C.M. Eating routines. Embedded, value based, modifiable, and reflective. Appetite 2009, 52, 127–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lassen, A.D.; Fagt, S.; Lennernäs, M.; Nyberg, M.; Haapalar, I.; Thorsen, A.V.; Møbjerg, A.C.; Beck, A.M. The impact of worksite interventions promoting healthier food and/or physical activity habits among employees working ‘around the clock’hours: A systematic review. Food Nutr. Res. 2018, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bos-de Vos, M. A framework for designing for divergent values. In Proceedings of the DRS2020 International Conference, Brisbane, Australia, 11–14 August 2020; pp. 39–53. [Google Scholar]
- Berezowska, A.; Fischer, A.R.; Ronteltap, A.; Kuznesof, S.; Macready, A.; Fallaize, R.; Van Trijp, H.C. Understanding consumer evaluations of personalised nutrition services in terms of the privacy calculus: A qualitative study. Public Health Genom. 2014, 17, 127–140. [Google Scholar] [CrossRef] [Green Version]
- Berezowska, A.; Fischer, A.R.; Ronteltap, A.; van der Lans, I.A.; van Trijp, H.C. Consumer adoption of personalised nutrition services from the perspective of a risk–benefit trade-off. Genes Nutr. 2015, 10, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ronteltap, A.; van Trijp, H.; Berezowska, A.; Goossens, J. Nutrigenomics-based personalised nutritional advice: In search of a business model? Genes Nutr. 2013, 8, 153–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucassen, D.A.; Lasschuijt, M.P.; Camps, G.; Van Loo, E.J.; Fischer, A.R.H.; de Vries, R.A.J.; Haarman, J.A.M.; Simons, M.; de Vet, E.; Bos-de Vos, M.; et al. Short and Long-Term Innovations on Dietary Behavior Assessment and Coaching: Present Efforts and Vision of the Pride and Prejudice Consortium. Int. J. Environ. Res. Public Health 2021, 18, 7877. https://doi.org/10.3390/ijerph18157877
Lucassen DA, Lasschuijt MP, Camps G, Van Loo EJ, Fischer ARH, de Vries RAJ, Haarman JAM, Simons M, de Vet E, Bos-de Vos M, et al. Short and Long-Term Innovations on Dietary Behavior Assessment and Coaching: Present Efforts and Vision of the Pride and Prejudice Consortium. International Journal of Environmental Research and Public Health. 2021; 18(15):7877. https://doi.org/10.3390/ijerph18157877
Chicago/Turabian StyleLucassen, Desiree A., Marlou P. Lasschuijt, Guido Camps, Ellen J. Van Loo, Arnout R. H. Fischer, Roelof A. J. de Vries, Juliet A. M. Haarman, Monique Simons, Emely de Vet, Marina Bos-de Vos, and et al. 2021. "Short and Long-Term Innovations on Dietary Behavior Assessment and Coaching: Present Efforts and Vision of the Pride and Prejudice Consortium" International Journal of Environmental Research and Public Health 18, no. 15: 7877. https://doi.org/10.3390/ijerph18157877
APA StyleLucassen, D. A., Lasschuijt, M. P., Camps, G., Van Loo, E. J., Fischer, A. R. H., de Vries, R. A. J., Haarman, J. A. M., Simons, M., de Vet, E., Bos-de Vos, M., Pan, S., Ren, X., de Graaf, K., Lu, Y., Feskens, E. J. M., & Brouwer-Brolsma, E. M. (2021). Short and Long-Term Innovations on Dietary Behavior Assessment and Coaching: Present Efforts and Vision of the Pride and Prejudice Consortium. International Journal of Environmental Research and Public Health, 18(15), 7877. https://doi.org/10.3390/ijerph18157877






