Development and Validation of a Self-Efficacy Scale for Nursing Educators’ Role in Sri Lanka
Abstract
:1. Introduction
2. Methods
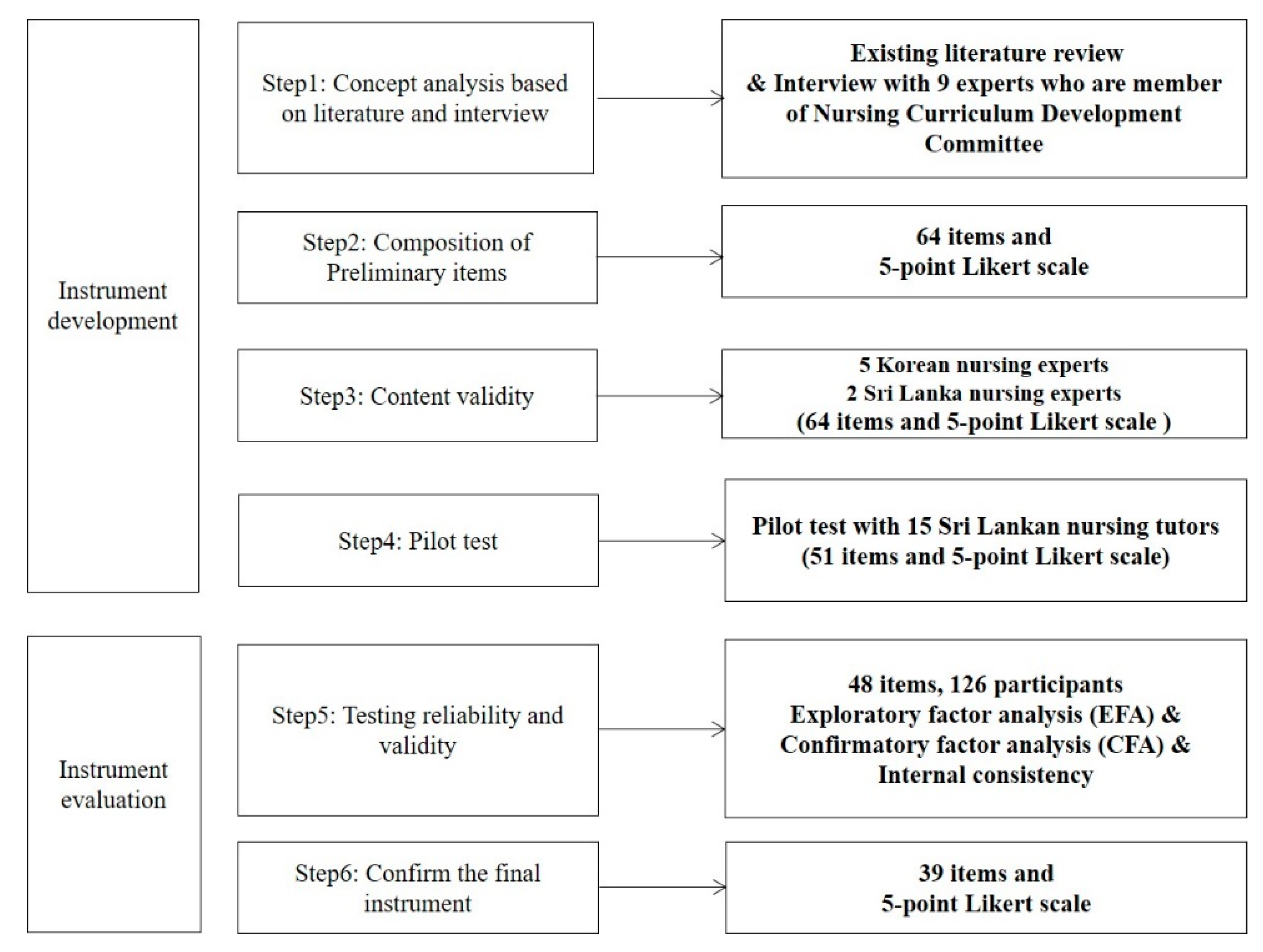
2.1. Study Design
2.2. Concept Analysis of the Nursing Educator’s Role
2.3. Composition of Preliminary Items
2.4. Content Validity and Pilot Testing
2.5. Validity and Reliability Testing
2.5.1. Sample and Setting
2.5.2. Data Collection
2.5.3. Validity Testing
2.5.4. Reliability Testing
2.6. Data Analysis
2.6.1. Qualitative Data
2.6.2. Quantitative Data
2.7. Ethical Consideration
3. Results
3.1. Concept Analysis of Nursing Educators’ Role
3.2. Categorization of Preliminary Items
3.3. Content Validity and Pilot Testing
3.4. Validity and Reliability Testing
3.4.1. Identification of Participants’ General Characteristics
3.4.2. Item Analysis
3.4.3. Exploratory Factor Analysis
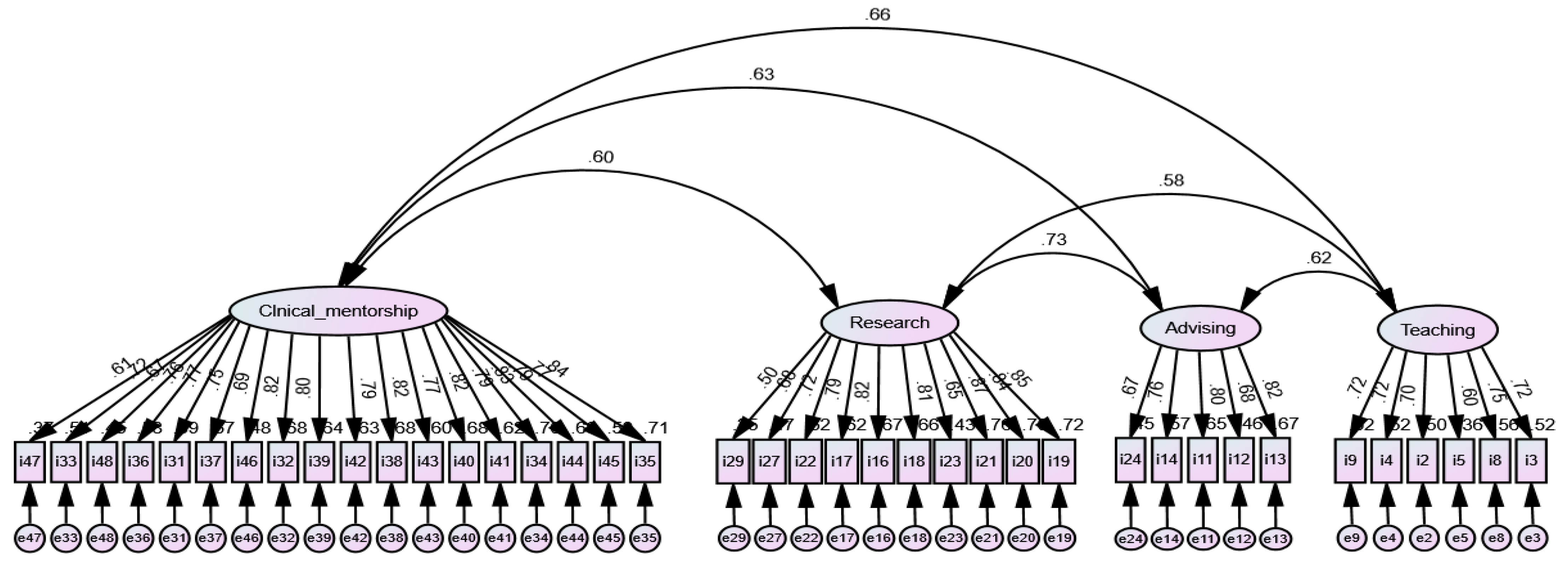
3.4.4. Confirmatory Factor Analysis
3.4.5. Reliability Testing
3.5. Confirmation of the Final Instrument
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Satoh, M.; Fujima, A.; Satao, N. Competency of academic nurse educators. SAGE Open Nurs. 2020, 6, 1–11. [Google Scholar] [CrossRef]
- Brown, T.; Sorrell, J.M. Challenges of novice nurse educator’s transition from practice to classroom. Teach. Learn. Nurs. 2017, 12, 207–211. [Google Scholar] [CrossRef] [Green Version]
- Jayasekara, R.; Amarasekara, T. Nursing education in Sri Lanka: Challenges and vision for the future. In Proceedings of the 3rd Annual Worldwide Nursing Conference, Singapore, 29–30 June 2015; Global Science & Technology Forum: Singapore, 2015; pp. 14–20. [Google Scholar]
- Rathnayake, S.; Ekanayaka, J. Depression, anxiety and stress among undergraduate nursing students in a public university in Sri Lanka. Int. J. Caring Sci. 2016, 9, 1020–1032. [Google Scholar]
- Aluwihare-samaranayake, D.; Ogilvie, L.; Cummings, G.G.; Gellatly, I.R. The nursing profession in Sri Lanka: Time for policy changes. Int. Nurs. Rev. 2017, 64, 363–370. [Google Scholar] [CrossRef] [PubMed]
- David, D.; Stullenbarger, E.; Dearman, C.; Kelly, J.A. Proposed nurse educator competencies: Development and validation of a model. Nurs. Outlook 2005, 53, 206–211. [Google Scholar] [CrossRef]
- Meretoja, R.; Numminen, O.; Isoaho, H.; Leino-Kilpi, H. Nurse competence between three generational nurse cohorts: A cross sectional study. Int. J. Nurs. Pract. 2015, 21, 350–358. [Google Scholar] [CrossRef]
- Nazari, R.; Mohammadi, E. Characteristics of competent clinical instructors: A review of the experiences of nursing students and instructors. J. Nurs. Midwifery Sci. 2015, 2, 11–22. [Google Scholar] [CrossRef]
- Park, I.; Suh, Y.O. Development of teaching efficacy scale to evaluate clinical nursing instructors. Korean J. Adult Nurs. 2018, 31, 18–29. [Google Scholar] [CrossRef] [Green Version]
- Fukada, M. Nursing competency: Definition, structure and development. Yonago Acta Med. 2018, 61, 1–7. [Google Scholar] [CrossRef] [Green Version]
- DeVellis, R.F. Scale Development: Theory and Application, 4th ed.; Sage Publications: Thousand Oaks, CA, USA, 2017; pp. 1–297. [Google Scholar]
- Hou, X.; Zhu, D.; Zheng, M. Clinical nursing faculty competence inventory—Development and psychometric testing. J. Adv. Nurs. 2010, 67, 1109–1117. [Google Scholar] [CrossRef]
- Kwak, E.; Oh, H. Development and psychometric testing of the clinical nursing competency scale for clinical preceptor use (CNCS-SP). J. Korean Acad. Nurs. 2018, 48, 419–431. [Google Scholar] [CrossRef]
- Ahn, S.; Lee, N.; Jang, H. Patient safety teaching competency of nursing faculty. J. Korean Acad. Nurs. 2018, 48, 720–730. [Google Scholar] [CrossRef] [PubMed]
- Abou, S.H.; McGrath, J.M.; Estes, T. Developing and testing the nurse educator scale: A robust measure of students’ intentions to pursue an educator role. J. Nurs. Educ. 2013, 52, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Hinkin, T.R. A brief tutorial on the development of measures for use in survey questionnaires. Organ. Res. Methods 1998, 2, 104–121. [Google Scholar] [CrossRef]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Kang, H.C. A guide on the use of factor analysis in the assessment of construct validity. J. Korean Acad. Nurs. 2013, 43, 587–594. [Google Scholar] [CrossRef] [Green Version]
- Vaismoradi, M.; Jones, J.; Turunen, H.; Snelgrove, S. Theme development in qualitative content analysis and thematic analysis. J. Nurs. Educ. Pract. 2016, 6, 100–110. [Google Scholar] [CrossRef] [Green Version]
- Lynn, M.R. Determination and quantification of content validity. Nurs. Res. 1986, 35, 382–385. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef] [Green Version]
- Field, A.P. Discovering Statistics Using IBM SPSS Statistics, 4th ed.; Sage Publications: London, UK, 2013; pp. 685–686. [Google Scholar]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Prentice Hall: Upper Saddle River, NJ, USA, 2009; pp. 1–784. [Google Scholar]
- Heo, J. Structural Equation Modeling with AMOS; Hannarae Publishing Co.: Seoul, Korea, 2013; pp. 70–89. [Google Scholar]
- Brown, T.A. Confirmatory Factor Analysis For Applied Research, 2nd ed.; Guilford Press: New York, NY, USA, 2015; pp. 1–462. [Google Scholar]
- Gutteling, J.J.; de Man, R.A.; Busschbach, J.J.; Darlington, A.E. Quality of health care and patient satisfaction in liver disease: The development and preliminary results of the QUOTE-Liver questionnaire. BMC Gastroenterol. 2008, 8, 25. [Google Scholar] [CrossRef] [Green Version]
- Oh, J.; Cho, H.; Kim, Y.Y.; Park, H.J.; Kim, H.K. An Integrative Review on Development of “QUality Of care Through the patients’ Eyes” (QUOTE) Instruments. J. Nurs. Care Qual. 2015, 30, E26–E31. [Google Scholar] [CrossRef]
- Pett, M.A.; Lackey, N.R.; Sullivan, J.J. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Research; Sage Publications: Thousand Oaks, CA, USA, 2003; pp. 232–233. [Google Scholar]
- Samarasooriya, R.C.; Park, J.; Yoon, S.H.; Oh, J.; Baek, S. Self-directed learning among nurse learners in Sri Lanka. J. Contin. Educ. Nurs. 2019, 50, 41–48. [Google Scholar] [CrossRef]
- Chen, Y.; Roger, W.; Hilton, A. An exploration of the structure of mentors’ behavior in nursing education using exploratory factor analysis and Mokken scale analysis. Nurse Educ. Today 2016, 40, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Horntvedt, M.E.T.; Nordsteien, A.; Fermann, T.; Severinsson, E. Strategies for teaching evidence-based practice in nursing education: A thematic literature review. BMC Med. Educ. 2018, 18, 172. [Google Scholar] [CrossRef]
- The Role of Research in Teacher Education: Reviewing the Evidence. Available online: https://www.thersa.org/globalassets/pdfs/reports/bera-rsa-interim-report.pdf (accessed on 31 December 2020).
- Dreifuerst, K.T.; McNelis, A.M.; Weaver, M.T.; Broome, M.E.; Draucker, C.B.; Fedko, A.S. Exploring the Pursuit of Doctoral Education by Nurses Seeking or Intending to Stay in Faculty Roles. J. Prof. Nurs. 2016, 32, 202–212. [Google Scholar] [CrossRef] [PubMed]
- Booth, T.L.; Emerson, C.J.; Hackney, M.G.; Souter, S. Preparation of academic nurse educators. Nurse Educ. Pract. 2016, 19, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Chapman, H.; Lewis, P.; Osborne, Y.; Gray, G. An action research approach for the professional development of Vietnamese nurse educators. Nurse Educ. Today 2013, 33, 129–132. [Google Scholar] [CrossRef] [Green Version]
- Snyder, B.; Griffin, M. Nursing student perceptions of faculty and advising. Nurs. Educ. Perspect. 2020, 41, 163–167. [Google Scholar] [CrossRef]
- Read, A.; Hicks, J.; Christenbery, T. Appreciative advising in nursing education. Nurse Educ. 2017, 42, 81–84. [Google Scholar] [CrossRef]
- Park, H.; Cho, H. Effects of nursing education using films on perception of nursing, satisfaction with major, and professional nursing values. J. Nurs. Res. 2021, 29, e150. [Google Scholar] [CrossRef]
- Morris, A.H.; Faulk, D.R. Transformative Learning in Nursing; Springer: New York, NY, USA, 2012; p. 20. [Google Scholar]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994; pp. 1–752. [Google Scholar]
- Lee, H.J.; Song, R.Y.; Lee, E.H.; Ahn, S.H. Research Methods and Critical Appraisal; Koonja Pub: Paju, Korea, 2017; pp. 300–301. [Google Scholar]
- Gray, J.R.; Grove, S.K. Burns and Grove’s the Practice of Nursing Research: Appraisal, Synthesis, and Generation of Evidence, 9th ed.; Elsevier: Maryland Heights, MO, USA, 2020; pp. 458–463. [Google Scholar]
- Oh, J.; Cho, H.; Kim, Y.Y.; Yoo, S.Y. Validation of the Korean version of the nursing profession self-efficacy scale: A methodological study. Int. J. Environ. Res. Public Health 2021, 18, 1080. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.Y.; Lee, H.; Lee, I.; Lee, M.; Cho, H. Validation of the nurses’ involvement in dying patients and family care-Korean version. J. Hosp. Palliat Care 2020, 23, 228–240. [Google Scholar] [CrossRef]
| Theme | Category | Contents |
|---|---|---|
| Teaching | Student assessment | ⬥ Development of an objective assessment tool ⬥ Development of a practical examination |
| Curriculum development | ⬥ Designing course work ⬥ Delivering curriculum contents | |
| Student support | ⬥ Motivating students ⬥ Guiding students to overcome problems | |
| Classroom lecture | ⬥ Planning teaching methodologies ⬥ Guiding students to perform self-learning | |
| Research | Engagement in research activities | ⬥ Creating a national research problem ⬥ Publishing research results |
| Generation of new knowledge | ⬥ Dissemination of research findings ⬥ Utilization of current literature | |
| Perform life-long learning | ⬥ Nurturing intrinsic motivation | |
| Clinical mentorship | Practice in the real word | ⬥ Delivering care ⬥ Facing emerging challenges in clinic |
| Training nursing skills | ⬥ Preparing students ⬥ Demonstrating nursing skills ⬥ Evaluating nursing students | |
| Applying new knowledge in clinical practice | ⬥ Facilitating evidence-based practice | |
| Advising | Relationship with other members | ⬥ Maintaining relationships with members |
| Communication | ⬥ Applying communication skills | |
| Developing leadership | ⬥ Remaining alert to latest global trends and issues |
| Characteristics | n | % | Mean ± SD | Min–Max. | |
|---|---|---|---|---|---|
| Sex | Female | 102 | 81.0 | ||
| Male | 24 | 19.0 | |||
| Age (year) | 46.36 ± 5.21 | 37–59 | |||
| Institution | Basic nursing school | 117 | 92.9 | ||
| PBCN | 9 | 7.1 | |||
| Maximum qualification | Post-graduation | 19 | 15.1 | ||
| Bachelor’s degree | 71 | 56.3 | |||
| Diploma | 36 | 28.6 | |||
| Teaching experience (year) | 10.50 ± 3.16 | 4–18 | |||
| Clinical nursing experience (year) | 9.87 ± 4.52 | 4–36 | |||
| Types of clinical settings 1 | National hospital | 22 | 17.5 | ||
| Teaching hospital | 86 | 48.9 | |||
| General hospital | 43 | 24.4 | |||
| District general hospital | 25 | 14.2 | |||
| Items 1 | Communality | Factor 1 | Factor 2 | Factor 3 | Factor 4 | |
|---|---|---|---|---|---|---|
| I Have the Ability to … | Clinical Mentorship | Research | Advising | Teaching | ||
| 35 | Build relationships based on mutual trust and respect with clinical staff. | 0.74 | 0.80 | 0.12 | 0.25 | 0.14 |
| 45 | Provide constructive feedback to students on their clinical performance. | 0.42 | 0.80 | 0.06 | 0.07 | 0.16 |
| 44 | Monitor the improvement of studies, clinical learning, and activities. | 0.68 | 0.80 | 0.15 | 0.09 | 0.13 |
| 34 | Encourage students to adapt themselves to their clinical nursing career. | 0.74 | 0.77 | 0.13 | 0.32 | 0.18 |
| 41 | Utilize appropriate clinical learning opportunities according to students’ stage of learning. | 0.66 | 0.77 | 0.18 | 0.14 | 0.12 |
| 40 | Provide support to students to facilitate their transition from one clinical learning environment to another. | 0.69 | 0.76 | 0.18 | 0.21 | 0.19 |
| 43 | Encourage students to combine theory and practice during clinical placement. | 0.62 | 0.74 | 0.10 | 0.26 | 0.15 |
| 38 | Contribute to the organization of a learner-friendly clinical environment. | 0.70 | 0.73 | 0.31 | 0.07 | 0.27 |
| 42 | Guide students to reflect on their clinical experiences. | 0.64 | 0.72 | 0.24 | 0.21 | 0.14 |
| 39 | Orient students to understand the legal framework of patient care management. | 0.66 | 0.72 | 0.19 | 0.16 | 0.28 |
| 32 | Maintain new knowledge of clinical practice. | 0.69 | 0.72 | 0.33 | 0.20 | 0.20 |
| 46 | Evaluate students’ clinical learning by using various clinical assessment strategies. | 0.61 | 0.70 | 0.26 | −0.12 | 0.18 |
| 37 | Prioritize patient-centered care to support students’ clinical learning. | 0.61 | 0.69 | 0.18 | 0.33 | 0.09 |
| 31 | Cooperate in academic management functions. | 0.64 | 0.68 | 0.31 | 0.09 | 0.26 |
| 36 | Create opportunities for students to build relationships with clinical staff. | 0.60 | 0.68 | 0.27 | 0.25 | 0.10 |
| 48 | Be attentive to the emotional stress faced by students in clinical situations. | 0.50 | 0.66 | 0.05 | 0.24 | 0.15 |
| 33 | Develop professional relationships with the members of other academic communities. | 0.57 | 0.64 | 0.37 | 0.03 | 0.17 |
| 47 | Direct students to search the literature that is relevant to their nursing interventions. | 0.42 | 0.58 | 0.18 | 0.09 | 0.21 |
| 19 | Engage in research activities in one’s interest areas. | 0.77 | 0.11 | 0.86 | 0.17 | 0.12 |
| 20 | Create rational research problems/arguments. | 0.76 | 0.15 | 0.85 | 0.13 | 0.14 |
| 21 | Utilize evidence based on knowledge or research findings. | 0.78 | 0.18 | 0.83 | 0.24 | 0.08 |
| 23 | Build relationships with national and international professional organizations. | 0.53 | 0.14 | 0.71 | 0.08 | 0.11 |
| 18 | Remain alert to latest global trends and issues. | 0.65 | 0.34 | 0.69 | 0.21 | 0.19 |
| 16 | Perform life-long learning to increase professional competency as a nurse educator. | 0.71 | 0.30 | 0.66 | 0.42 | 0.10 |
| 17 | Utilize relevant and current literature in all academic activities. | 0.66 | 0.24 | 0.63 | 0.40 | 0.21 |
| 22 | Safely, responsibly, and ethically handle the information obtained over the Internet. | 0.60 | 0.27 | 0.58 | 0.44 | 0.05 |
| 27 | Analyze policy guidelines or circulars relevant to nursing education. | 0.57 | 0.30 | 0.58 | 0.24 | 0.28 |
| 29 | Participate in interdisciplinary actions to address healthcare and educational issues and needs. | 0.40 | 0.31 | 0.50 | 0.02 | 0.22 |
| 13 | Act as a role model for students’ professional socialization. | 0.65 | 0.27 | 0.25 | 0.75 | 0.15 |
| 12 | Use linguistic skills (English) in reading, writing, listening, and speaking for academic purposes. | 0.62 | 0.13 | 0.19 | 0.73 | 0.18 |
| 11 | Provide effective counseling and help to students to solve their needs and problems. | 0.66 | 0.24 | 0.26 | 0.72 | 0.22 |
| 14 | Use feedback gained from oneself, peers, students, and administrators to improve role effectiveness. | 0.55 | 0.26 | 0.35 | 0.59 | 0.20 |
| 24 | Be accountable for one’s own professional judgments, actions, and outcomes. | 0.59 | 0.25 | 0.43 | 0.55 | 0.11 |
| 3 | Implement various teaching strategies, such as active learning, problem-based learning, and team-based learning, in the classroom. | 0.70 | 0.21 | 0.28 | −0.06 | 0.78 |
| 8 | Design objective assessment tools, such as checklists, test papers, assignments, portfolios, and clinical diaries. | 0.60 | 0.23 | 0.17 | 0.24 | 0.71 |
| 5 | Guide students to perform self- and peer evaluations of academic activities. | 0.54 | 0.15 | 0.00 | 0.26 | 0.67 |
| 2 | Plan teaching methodologies suited to students’ learning needs and styles. | 0.60 | 0.35 | 0.19 | 0.01 | 0.67 |
| 4 | Motivate students to use various learning sources, such as print materials, audio visual materials, the Internet, and smartphones. | 0.59 | 0.26 | 0.25 | 0.26 | 0.61 |
| 9 | Use students’ assessment and evaluation data to improve the teaching–learning process. | 0.52 | 0.32 | 0.17 | 0.29 | 0.59 |
| Explained variance | 10.65 | 6.45 | 3.95 | 3.74 | ||
| Explained percentage | 27.31 | 16.55 | 10.12 | 9.60 | ||
| Cumulative percentage | 27.31 | 43.86 | 53.98 | 63.58 | ||
| Goodness of Fit | χ2(p) | χ2/df | RMR | RMSEA | GFI | NFI | TLI | CFI |
|---|---|---|---|---|---|---|---|---|
| Baseline | p > 0.05 | ≤3 | ≤0.05 | ≤0.10 | ≥0.90 | ≥0.80 | ≥0.80 | ≥0.80 |
| Results | 1321.2 (p < 0.001) | 1.90 | 0.07 | 0.09 | 0.66 | 0.71 | 0.82 | 0.84 |
| Factor | Item | Standardized Factor Loading | Critical Ratio | p | CR | AVE | Cronbach’s Alpha |
|---|---|---|---|---|---|---|---|
| Clinical mentorship | 31 | 0.77 | 0.97 | 0.64 | 0.96 | ||
| 32 | 0.83 | 10.20 | <0.001 | ||||
| 33 | 0.72 | 8.57 | <0.001 | ||||
| 34 | 0.83 | 10.34 | <0.001 | ||||
| 35 | 0.84 | 10.43 | <0.001 | ||||
| 36 | 0.76 | 9.23 | <0.001 | ||||
| 37 | 0.75 | 9.12 | <0.001 | ||||
| 38 | 0.82 | 10.16 | <0.001 | ||||
| 39 | 0.80 | 9.86 | <0.001 | ||||
| 40 | 0.82 | 10.16 | <0.001 | ||||
| 41 | 0.79 | 9.59 | <0.001 | ||||
| 42 | 0.79 | 9.71 | <0.001 | ||||
| 43 | 0.77 | 9.40 | <0.001 | ||||
| 44 | 0.79 | 9.70 | <0.001 | ||||
| 45 | 0.77 | 9.34 | <0.001 | ||||
| 46 | 0.69 | 8.21 | <0.001 | ||||
| 47 | 0.61 | 7.14 | <0.001 | ||||
| 48 | 0.67 | 7.95 | <0.001 | ||||
| Research | 16 | 0.82 | 0.93 | 0.56 | 0.88 | ||
| 17 | 0.79 | 10.34 | <0.001 | ||||
| 18 | 0.81 | 10.75 | <0.001 | ||||
| 19 | 0.85 | 11.55 | <0.001 | ||||
| 20 | 0.84 | 11.26 | <0.001 | ||||
| 21 | 0.87 | 11.98 | <0.001 | ||||
| 22 | 0.72 | 9.14 | <0.001 | ||||
| 23 | 0.65 | 8.01 | <0.001 | ||||
| 27 | 0.68 | 8.48 | <0.001 | ||||
| 29 | 0.50 | 5.86 | <0.001 | ||||
| Advising | 11 | 0.80 | 0.88 | 0.61 | 0.88 | ||
| 12 | 0.68 | 7.84 | <0.001 | ||||
| 13 | 0.82 | 9.92 | <0.001 | ||||
| 14 | 0.76 | 9.02 | <0.001 | ||||
| 24 | 0.67 | 7.80 | <0.001 | ||||
| Teaching | 2 | 0.70 | 0.89 | 0.57 | 0.97 | ||
| 3 | 0.72 | 7.354 | <0.001 | ||||
| 4 | 0.72 | 7.345 | <0.001 | ||||
| 5 | 0.60 | 6.186 | <0.001 | ||||
| 8 | 0.75 | 7.612 | <0.001 | ||||
| 9 | 0.72 | 7.363 | <0.001 |
| Sub-Factors of the SSNER-SL | Factor 1 | Factor 2 | Factor 3 | Factor 4 |
|---|---|---|---|---|
| Factor 1: Clinical mentorship | 0.80 1 | |||
| Factor 2: Research | 0.63 (<0.001) | 0.75 1 | ||
| Factor 3: Advising | 0.76 (<0.001) | 0.71 (<0.001) | 0.78 1 | |
| Factor 4: Teaching | 0.69 (<0.001) | 0.73 (<0.001) | 0.67 (<0.001) | 0.75 1 |
| Factor (Number of Items) | Mean ± SD | Min-Max | Rank |
|---|---|---|---|
| SSNER-SL (39) | 3.20 ± 0.61 | 2.10–4.83 | — |
| - Clinical mentorship (18) | 3.41 ± 0.71 | 1.89–5.0 | 1 |
| - Research (10) | 2.79 ± 0.81 | 1.40–4.90 | 4 |
| - Advising (5) | 3.35 ± 0.73 | 1.60–5.0 | 2 |
| - Teaching (6) | 3.24 ± 0.66 | 1.83–4.67 | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weerasekara, S.S.; Oh, J.; Cho, H.; Im, M. Development and Validation of a Self-Efficacy Scale for Nursing Educators’ Role in Sri Lanka. Int. J. Environ. Res. Public Health 2021, 18, 7773. https://doi.org/10.3390/ijerph18157773
Weerasekara SS, Oh J, Cho H, Im M. Development and Validation of a Self-Efficacy Scale for Nursing Educators’ Role in Sri Lanka. International Journal of Environmental Research and Public Health. 2021; 18(15):7773. https://doi.org/10.3390/ijerph18157773
Chicago/Turabian StyleWeerasekara, Shyamamala S., Jina Oh, Haeryun Cho, and Mihae Im. 2021. "Development and Validation of a Self-Efficacy Scale for Nursing Educators’ Role in Sri Lanka" International Journal of Environmental Research and Public Health 18, no. 15: 7773. https://doi.org/10.3390/ijerph18157773
APA StyleWeerasekara, S. S., Oh, J., Cho, H., & Im, M. (2021). Development and Validation of a Self-Efficacy Scale for Nursing Educators’ Role in Sri Lanka. International Journal of Environmental Research and Public Health, 18(15), 7773. https://doi.org/10.3390/ijerph18157773






