Socioeconomic Health Inequalities in Adolescent Metabolic Syndrome and Depression: No Mediation by Parental Depression and Parenting Style
Abstract
:1. Introduction
2. Methods
2.1. Setting and Population
2.2. Procedures
2.3. Measures
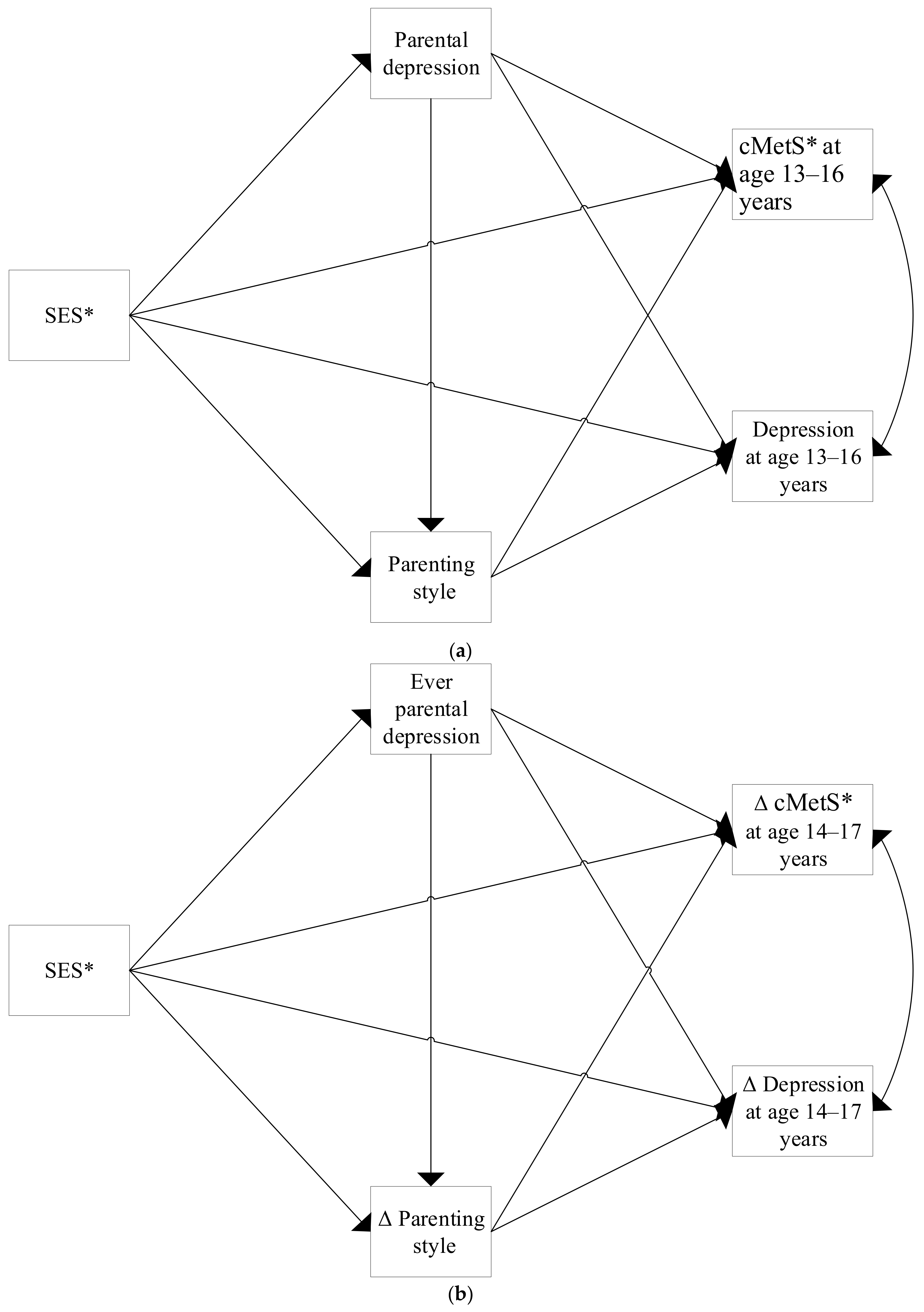
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. SES and Baseline Depression and cMetS: Mediation by Baseline Parental Depression and Parenting Style
3.3. SES and Changes in Depression and cMetS: Mediation by Changes in Both Parental Depression and Parenting Style
4. Discussion
4.1. Strengths and Limitations
4.2. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Elgar, F.J.; Pförtner, T.-K.; Moor, I.; De Clercq, B.; Stevens, G.W.J.M.; Currie, C. Socioeconomic inequalities in adolescent health 2002–2010: A time-series analysis of 34 countries participating in the Health Behaviour in School-aged Children study. Lancet 2015, 385, 2088–2095. [Google Scholar] [CrossRef] [Green Version]
- WHO. Healthy, Prosperous Lives for All: The European Health Equity Status Report; Licence: CC BY-NC-SA 3.0 IGO; WHO Regional Office for Europe: Copenhagen, Denmark, 2019. [Google Scholar]
- Devenish, B.; Hooley, M.; Mellor, D. The Pathways Between Socioeconomic Status and Adolescent Outcomes: A Systematic Review. Am. J. Community Psychol. 2017, 59, 219–238. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, M.; de Groh, M.; Loukine, L.; Prud’homme, D.; Dubois, L. Prevalence of metabolic syndrome and its risk factors in Canadian children and adolescents: Canadian Health Measures Survey Cycle 1 (2007–2009) and Cycle 2 (2009–2011). Health Promot. Chronic. Dis. Prev. Can. 2016, 36, 32–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burcusa, S.L.; Iacono, W.G. Risk for recurrence in depression. Clin. Psychol. Rev. 2007, 27, 959–985. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hadjiyannakis, S. The metabolic syndrome in children and adolescents. Paediatr. Child Health 2005, 10, 41–47. [Google Scholar] [CrossRef] [Green Version]
- Magnussen, C.G.; Cheriyan, S.; Sabin, M.A.; Juonala, M.; Koskinen, J.; Thomson, R.; Skilton, M.R.; Kahonen, M.; Laitinen, T.; Taittonen, L.; et al. Continuous and Dichotomous Metabolic Syndrome Definitions in Youth Predict Adult Type 2 Diabetes and Carotid Artery Intimsa Media Thickness: The Cardiovascular Risk in Young Finns Study. J. Pediatr. 2016, 171, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Van Der Kooy, K.; Van Hout, H.; Marwijk, H.; Marten, H.; Stehouwer, C.; Beekman, A. Depression and the risk for cardiovascular diseases: Systematic review and meta analysis. Int. J. Geriatr. Psychiatry 2007, 22, 613–626. [Google Scholar] [CrossRef]
- IHME. GBD Compare Data Visualization. Available online: http://vizhub.healthdata.org/gbd-compare (accessed on 16 December 2020).
- Pan, A.; Keum, N.; Okereke, O.I.; Sun, Q.; Kivimaki, M.; Rubin, R.R.; Hu, F.B. Bidirectional Association Between Depression and Metabolic Syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care 2012, 35, 1171–1180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masarik, A.S.; Conger, R.D. Stress and child development: A review of the Family Stress Model. Curr. Opin. Psychol. 2017, 13, 85–90. [Google Scholar] [CrossRef] [Green Version]
- Marco, P.L.; Valério, I.D.; Zanatti, C.L.D.M.; Gonçalves, H. Systematic review: Symptoms of parental depression and anxiety and offspring overweight. Rev. Saude Publica 2020, 54, 49. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.P.; Bluestone, C.; Burke, C.T. Trajectories of BMI from early childhood through early adolescence: SES and psychosocial predictors. Br. J. Health Psychol. 2013, 18, 66–82. [Google Scholar] [CrossRef] [PubMed]
- Conger, R.D.; Conger, K.J.; Martin, M.J. Socioeconomic Status, Family Processes, and Individual Development. J. Marriage Fam. 2010, 72, 685–704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morrison Gutman, L.; McLoyd, V.C.; Tokoyawa, T. Financial Strain, Neighborhood Stress, Parenting Behaviors, and Adolescent Adjustment in Urban African American Families. J. Res. Adolesc. 2005, 15, 425–449. [Google Scholar] [CrossRef]
- Walper, S. Links of perceived economic deprivation toadolescents’ well-being six years later. J. Fam. Res. 2009, 21. [Google Scholar] [CrossRef]
- Scholtens, S.; Smidt, N.; Swertz, M.A.; Bakker, S.J.; Dotinga, A.; Vonk, J.M.; van Dijk, F.; van Zon, S.K.; Wijmenga, C.; Wolffenbuttel, B.H.; et al. Cohort Profile: LifeLines, a three-generation cohort study and biobank. Int. J. Epidemiol. 2015, 44, 1172–1180. [Google Scholar] [CrossRef] [Green Version]
- Stolk, R.P.; Rosmalen, J.G.; Postma, D.S.; de Boer, R.A.; Navis, G.; Slaets, J.P.; Ormel, J.; Wolffenbuttel, B.H. Universal risk factors for multifactorial diseases: LifeLines: A three-generation population-based study. Eur. J. Epidemiol. 2008, 23, 67–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Achenbach, T.M.; Rescorla, L. Manual for the ASEBA School-Age Forms & Profiles: An Integrated System of Multi-Informant Assessment; University of Vermont, Research Center for Children, Youth, & Families: Burlington, VT, USA, 2001. [Google Scholar]
- Eisenmann, J.C.; Laurson, K.R.; DuBose, K.D.; Smith, B.K.; Donnelly, J.E. Construct validity of a continuous metabolic syndrome score in children. Diabetol. Metab. Syndr. 2010, 2, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Growth Analyser. Growth Analyser RCT; 4.1.5; Growth Analyser: Rotterdam, The Netherlands, 2018. [Google Scholar]
- Talma, H.; Schonbeck, Y.; Bakker, B.; Hirasing, R.A.; Buuren, S.v. Groeidiagrammen 2010: Handleiding Bij het Meten en Wegen van Kinderen en het Invullen van Groeidiagrammen; TNO: Leiden, The Netherlands, 2010. [Google Scholar]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59 (Suppl. 20), 22–33. [Google Scholar]
- Muris, P.; Bosma, H.; Meesters, C.; Schouten, E. Perceived parental rearing behaviours: A confirmatory factor analytic study of the Dutch EMBU for children. J. Sch. Violence 1998, 24, 439–442. [Google Scholar] [CrossRef]
- Janssen, D.F. State of the World’s Fathers Country Report: Netherlands 2015; Rutgers: Utrecht, The Netherlands, 2015. [Google Scholar]
- De Graaf, N.D.; De Graaf, P.M.; Kraaykamp, G. Parental Cultural Capital and Educational Attainment in the Netherlands: A Refinement of the Cultural Capital Perspective. Sociol. Educ. 2000, 73, 92–111. [Google Scholar] [CrossRef]
- International Labour Office. International Standard Classification of Occupations. ISCO-08: Structure, Group Definitions and Correspondence Tables; International Labour Office: Geneva, Switzerland, 2012; Volume 1. [Google Scholar]
- Ganzeboom, H.B.G.; Treiman, D.J. International Stratification and Mobility File: Conversion Tools. Available online: http://www.harryganzeboom.nl/ismf/index.htm (accessed on 7 July 2020).
- Treiman, D.J. Occupational Prestige in Comparative Perspective, 1st ed.; Rossi, P.H., Ed.; Academic Press: New York, NY, USA, 1977; p. 536. [Google Scholar]
- OECD. Compare Your Income—Methodology and Conceptual Issues; OECD: Paris, France, 2018. [Google Scholar]
- Muthen, L.K.; Muthen, B. Mplus User’s Guide: Statistical Analysis with Latent Variables; Muthen & Muthen: Los Angeles, LA, USA, 2017. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing, 3.5.2; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Heeger-Hertter, S. Social assistance benefits in the Netherlands. Studia Zakr. Prawa Pr. Polityki Społecznej 2019, 26, 75–93. [Google Scholar] [CrossRef]
- Goosby, B.J. Poverty Duration, Maternal Psychological Resources, and Adolescent Socioemotional Outcomes. J. Fam. Issues 2007, 28, 1113–1134. [Google Scholar] [CrossRef] [Green Version]
- Klijs, B.; Scholtens, S.; Mandemakers, J.J.; Snieder, H.; Stolk, R.P.; Smidt, N. Representativeness of the LifeLines Cohort Study. PLoS ONE 2015, 10, e0137203. [Google Scholar] [CrossRef] [PubMed]
- Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics 2011, 128 (Suppl. 5), S213–S256. [CrossRef] [Green Version]
- Berenbaum, S.A.; Beltz, A.M.; Corley, R. The Importance of Puberty for Adolescent Development. Elsevier: Amsterdam, The Netherlands, 2015; pp. 53–92. [Google Scholar]
- Morrison, A.K.; Glick, A.; Yin, H.S. Health Literacy: Implications for Child Health. Pediatr. Rev. 2019, 40, 263. [Google Scholar] [CrossRef] [PubMed]
- Stormacq, C.; Van den Broucke, S.; Wosinski, J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promot. Int. 2019, 34, e1–e17. [Google Scholar] [CrossRef] [PubMed]
| Males (n = 589) | Females (n = 628) | ||||
|---|---|---|---|---|---|
| Mean (sd), Median [IQR], or n (n%) | Missing n (n%) | Mean (sd), Median [IQR], or n (n%) | Missing n (n%) | p-Value e | |
| Baseline Age (years) | 13 [13–14] | 13 [13–14] | 0.192 | ||
| Health Outcomes | |||||
| Continuous MetS score | 0.03 (2.89) | 64 (10.9%) | 0.02 (2.79) | 75 (11.9%) | 0.956 |
| Δ a Continuous MetS score | 0.10 (2.49) | 117 (19.9%) | −0.76 (2.40) | 135 (21.5%) | <0.001 |
| Symptoms of depression | 1 [0–3] | 19 (3.2%) | 3 [1–5] | 24 (3.8%) | <0.001 |
| Δ a Symptoms of depression | 0.09 (2.76) | 157 (26.7%) | 0.00 (3.44) | 132 (21.0%) | 0.812 |
| Baseline Mediators | |||||
| Parental depression | 19 (3.2%) | 14 (2.4%) | 20 (3.2%) | 19 (3.0%) | 1.000 |
| Parenting style | 3 [1–5] | 21 (3.6%) | 3 [1–5] | 25 (4.0%) | 0.980 |
| Changes Mediators | |||||
| Ever parental depression b | 36 (6.1%) | 87 (14.8%) | 45 (7.2%) | 89 (14.2%) | 0.490 |
| Δ a Parenting style | −0.12 (3.66) | 147 (25.0%) | −0.39 (3.31) | 111 (17.7%) | 0.289 |
| SES | |||||
| Years of education | 12 [12–15] | 6 (1.0%) | 12 [12–15] | 0 (0%) | 0.367 |
| Equivalized household income c | 1375 [1125.0–1677.1] | 57 (9.7%) | 1375 [1010.4–1625.0] | 82 (13.1%) | 0.056 |
| Occupation d | 49.13 (12.11) | 1 (0.2%) | 48.16 (12.70) | 6 (1.0%) | 0.162 |
| Participated during 2A (n = 1217) | Lost to Follow-Up (n = 945) | |||||
|---|---|---|---|---|---|---|
| Mean (sd), Median [IQR], or n (n%) | Missing n (n%) | Mean (sd), Median [IQR], or n (n%) | Missing n (n%) | p-Value c | ||
| Sex | Male | 589 (48.4%) | 461 (48.8%) | 0.862 | ||
| Female | 628 (51.6%) | 484 (51.2%) | ||||
| Age (years) | 13 [13–14] | 14 [13–15] | <0.001 | |||
| MetS Components: | ||||||
| Fasting Glucose (mmol/L) | 4.73 (0.46) | 135 (11.1%) | 4.72 (0.48) | 162 (17.1%) | 0.793 | |
| HDL (mmol/L) | 1.52 (0.32) | 106 (8.7%) | 1.48 (0.30) | 121 (12.8%) | 0.001 | |
| Triglycerides (mmol/L) | 0.66 [0.51–0.88] | 106 (8.7%) | 0.68 [0.52–0.90] | 121 (12.8%) | 0.145 | |
| Mean Arterial Pressure (mmHg) | 80.02 (6.29) | 5 (0.4%) | 80.58 (6.34) | 12 (1.3%) | 0.050 | |
| Waist Circumference (cm) | 70.54 (8.07) | 3 (0.2%) | 72.28 (8.11) | 11 (1.2%) | <0.001 | |
| Health Outcomes | ||||||
| BMI SDS | 0.38 (1.07) | 3 (0.2%) | 0.50 (1.05) | 11 (1.2%) | 0.023 | |
| Symptoms of depression | 2 [1–4] | 43 (3.5%) | 2 [0–4] | 54 (5.7%) | 0.882 | |
| Baseline Mediators | ||||||
| Parental Depression | 39 (3.2%) | 33 (2.7%) | 33 (3.5%) | 26 (2.8%) | 0.718 | |
| Parenting Style | 3 [1–5] | 46 (3.8%) | 3 [1–6] | 57 (6.0%) | 0.015 | |
| SES | ||||||
| Years of education | 12 [12–15] | 6 (0.5%) | 12 [12–15] | 9 (1.4%) | 0.146 | |
| Equivalized household income a | 1375 [1125–1677.1] | 139 (11.4%) | 1375 [1039.4–1638.0] | 101 (10.7%) | 0.170 | |
| Occupation b | 48.63 (12.42) | 7 (0.6%) | 47.86 (12.73) | 14 (1.5%) | 0.227 | |
| Depression Coefficient [95% CI] | cMetS Coefficient [95% CI] | |
|---|---|---|
| Education b | ||
| Direct effect of parental depression | 0.185 [−0.284; 0.552] | −0.122 [−0.961; 0.755] |
| Direct effect of parenting style | 0.028 [0.008; 0.047] | 0.056 [0.003; 0.107] |
| Direct effect of education | 0.022 [−0.009; 0.052] | −0.098 [−0.184; −0.020] |
| Education via parental depression | −0.033 [−0.156; 0.039] | 0.021 [−0.123; 0.207] |
| Education via parenting style | −0.001 [−0.002; 0.000] | −0.002 [−0.004; 0.000] |
| Education via parental depression and parenting style | −0.001 [−0.004; 0.000] | −0.003 [−0.010; 0.001] |
| Total effect a of education | 0.018 [−0.013; 0.049] | −0.104 [−0.187; −0.026] |
| Income c | ||
| Direct effect of parental depression | 0.187 [−0.291; 0.541] | −0.045 [−0.924; 0.803] |
| Direct effect of parenting style | 0.028 [0.008; 0.048] | 0.060 [0.007; 0.111] |
| Direct effect of income | 0.007 [−0.008; 0.023] | −0.004 [−0.044; 0.040] |
| Income via parental depression | −0.026 [−0.083; 0.038] | 0.006 [−0.124; 0.127] |
| Income via parenting style | 0.000 [−0.001; 0.000] | −0.001 [−0.003; 0.000] |
| Income via parental depression and parenting style | −0.001 [−0.003; 0.000] | −0.002 [−0.007; 0.001] |
| Total effect a of income | 0.006 [−0.011; 0.020] | −0.008 [−0.051; 0.032] |
| Occupation d | ||
| Direct effect of parental depression | 0.172 [−0.299; 0.523] | −0.049 [−0.931; 0.783] |
| Direct effect of parenting style | 0.028 [0.007; 0.047] | 0.059 [0.007; 0.110] |
| Direct effect of occupation | 0.023 [−0.025; 0.071] | −0.057 [−0.188; 0.075] |
| Occupation via parental depression | −0.033 [−0.135; 0.069] | 0.009 [−0.156; 0.222] |
| Occupation via parenting style | −0.002 [−0.004; 0.000] | −0.003 [−0.009; 0.000] |
| Occupation via parental depression and parenting style | −0.002 [−0.006; 0.000] | −0.003 [−0.012; 0.001] |
| Total effect a of occupation | 0.018 [−0.031; 0.065] | −0.066 [−0.201; 0.067] |
| Δ Depression Coefficient [95% CI] | Δ cMetS Coefficient [95% CI] | |
|---|---|---|
| Education b | ||
| Direct effect of parental depression | −0.390 [−1.046; 0.293] | 0.034 [−0.609; 0.738] |
| Direct effect of parenting style | 0.120 [0.058; 0.179] | −0.002 [−0.046; 0.042] |
| Direct effect of education | 0.072 [−0.013; 0.149] | −0.079 [−0.158; −0.004] |
| Education via ever parental depression | 0.078 [−0.051; 0.261] | −0.007 [−0.156; 0.127] |
| Education via Δ parenting style | −0.002 [−0.014; 0.010] | 0.000 [−0.002; 0.002] |
| Education via ever parental depression and Δ parenting style | 0.016 [−0.002; 0.043] | 0.000 [−0.009; 0.008] |
| Total effect a of education | 0.079 [−0.008; 0.159] | −0.080 [−0.161; −0.005] |
| Income c | ||
| Direct effect of parental depression | −0.369 [−1.049; 0.345] | 0.069 [−0.591; 0.755] |
| Direct effect of parenting style | 0.121 [0.059; 0.180] | −0.003 [−0.047; 0.041] |
| Direct effect of income | 0.016 [−0.030; 0.061] | −0.016 [−0.057; 0.022] |
| Income via ever parental depression | 0.041 [−0.037; 0.139] | −0.008 [−0.091; 0.069] |
| Income via Δ parenting style | −0.003 [−0.010; 0.004] | 0.000 [−0.002; 0.002] |
| Income via ever parental depression and Δ parenting style | 0.009 [−0.001; 0.025] | 0.000 [−0.005; 0.004] |
| Total effect a of income | 0.018 [−0.029; 0.064] | −0.016 [−0.055; 0.022] |
| Occupation d | ||
| Direct effect of parental depression | −0.372 [−1.043; 0.348] | 0.093 [−0.559; 0.779] |
| Direct effect of parenting style | 0.120 [0.058; 0.181] | −0.002 [−0.046; 0.041] |
| Direct effect of occupation | 0.028 [−0.114; 0.159] | −0.073 [−0.187; 0.039] |
| Occupation via ever parental depression | 0.114 [−0.095; 0.362] | −0.028 [−0.248; 0.184] |
| Occupation via Δ parenting style | −0.002 [−0.022; 0.018] | 0.000 [−0.004; 0.004] |
| Occupation via ever parental depression and Δ parenting style | 0.025 [−0.002; 0.069] | 0.000 [−0.013; 0.011] |
| Total effect a of occupation | 0.048 [−0.095; 0.181] | −0.076 [−0.190; 0.040] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lepe, A.; Reijneveld, S.A.; Almansa, J.; de Winter, A.F.; de Kroon, M.L.A. Socioeconomic Health Inequalities in Adolescent Metabolic Syndrome and Depression: No Mediation by Parental Depression and Parenting Style. Int. J. Environ. Res. Public Health 2021, 18, 7716. https://doi.org/10.3390/ijerph18147716
Lepe A, Reijneveld SA, Almansa J, de Winter AF, de Kroon MLA. Socioeconomic Health Inequalities in Adolescent Metabolic Syndrome and Depression: No Mediation by Parental Depression and Parenting Style. International Journal of Environmental Research and Public Health. 2021; 18(14):7716. https://doi.org/10.3390/ijerph18147716
Chicago/Turabian StyleLepe, Alexander, Sijmen A. Reijneveld, Josué Almansa, Andrea F. de Winter, and Marlou L. A. de Kroon. 2021. "Socioeconomic Health Inequalities in Adolescent Metabolic Syndrome and Depression: No Mediation by Parental Depression and Parenting Style" International Journal of Environmental Research and Public Health 18, no. 14: 7716. https://doi.org/10.3390/ijerph18147716
APA StyleLepe, A., Reijneveld, S. A., Almansa, J., de Winter, A. F., & de Kroon, M. L. A. (2021). Socioeconomic Health Inequalities in Adolescent Metabolic Syndrome and Depression: No Mediation by Parental Depression and Parenting Style. International Journal of Environmental Research and Public Health, 18(14), 7716. https://doi.org/10.3390/ijerph18147716






