Nutrition Education Programs Aimed at African Mothers of Infant Children: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
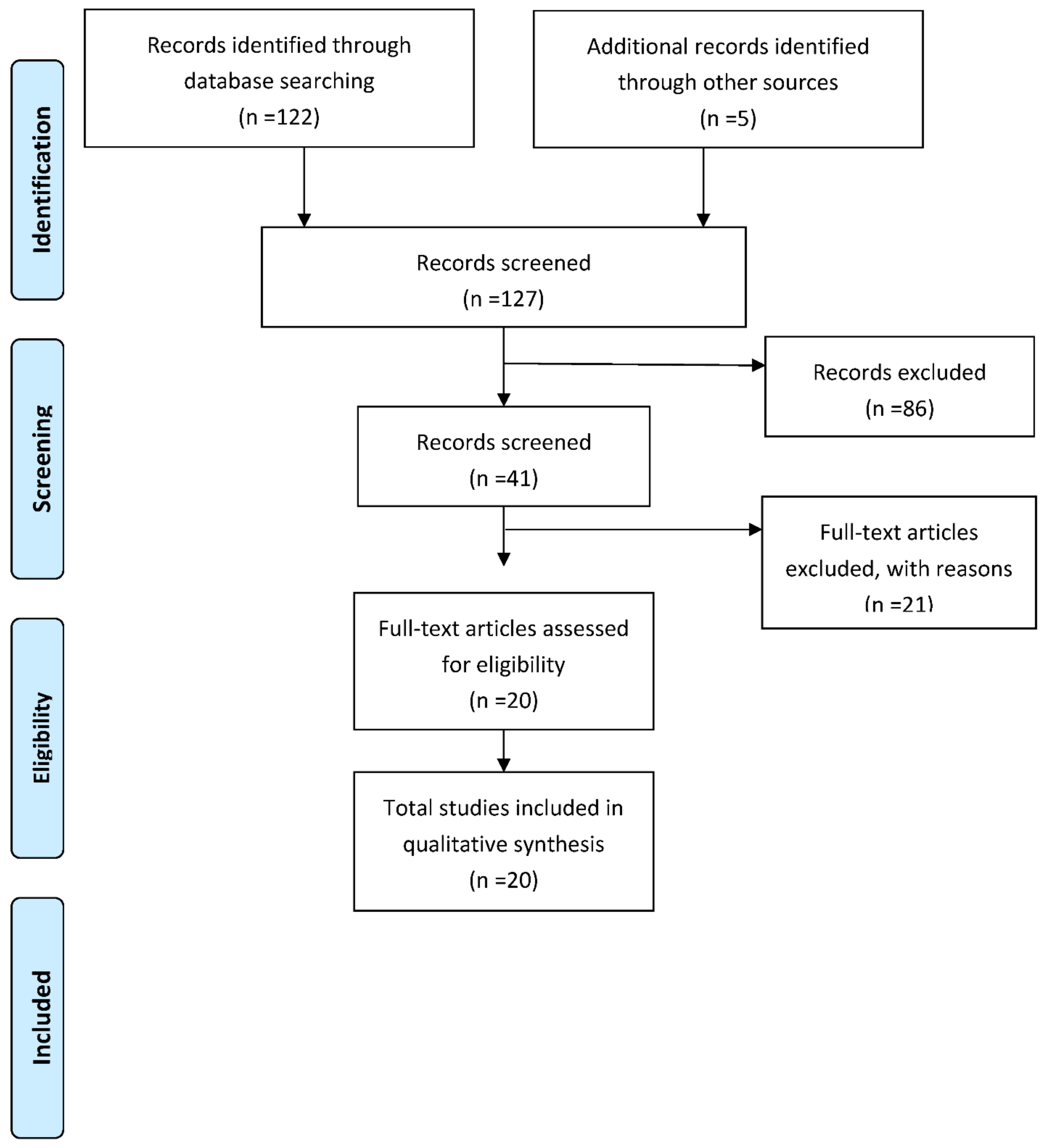
2.3. Selection of Articles
2.4. Data Abstraction
3. Results
4. Discussion
4.1. Effects of Educational Programs on Mother’s Knowledge and Feeding Practices, and Infant Nutritional Intake
4.2. Effects of Educational Programs on Anthropometric Development and Degree of Malnutrition
5. Strengths and Limitations
6. Policy and Future Research
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations Children’s Fund (UNICEF). The State of the World’s Children 2019. Children, Food and Nutrition. Growing Well in a Changing World. Available online: https://www.unicef.ch/sites/default/files/2019-10/SOWC_2019_Full-Report_EN.pdf (accessed on 28 May 2020).
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO); International Bank for Reconstruction and Development/The World Bank. Levels and Trends in Child Malnutrition: Key Findings of the 2019 Edition of the Joint Child Malnutrition Estimates; World Health Organization: Geneva, Switzerland, 2019; Licence: CC BY-NC-SA 3.0 IGO. Available online: https://www.unicef.org/media/60626/file/Joint-malnutrition-estimates-2019.pdf (accessed on 28 May 2020).
- Global Report on Food Crises. Food Security Information Network 2020. Available online: http://ebrary.ifpri.org/utils/getfile/collection/p15738coll2/id/133693/filename/133904.pdf (accessed on 3 October 2020).
- Bain, L.E.; Awah, P.K.; Geraldine, N.; Kindong, N.P.; Sigal, Y.; Bernard, N.; Tanjeko, A.T. Malnutrition in Sub-Saharan Africa: Burden, causes and prospects. Pan Afr. Med. J. 2013, 15, 120. [Google Scholar] [CrossRef] [PubMed]
- World Bank. Repositioning Nutrition as Central to Development: A Strategy for Large-Scale Action; World Bank: Washington, DC, USA, 2006; Available online: https://openknowledge.worldbank.org/handle/10986/7409 (accessed on 15 June 2021).
- Lartey, A. Maternal and child nutrition in Sub-Saharan Africa: Challenges and interventions. Proc. Nutr. Soc. 2008, 67, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Akombi, B.J.; Agho, K.E.; Hall, J.J.; Wali, N.; Renzaho, A.M.N.; Merom, D. Stunting, wasting and underweight in Sub-Saharan Africa: A systematic review. Int. J. Environ. Res. Public Health 2017, 14, 863. [Google Scholar] [CrossRef] [PubMed]
- Rice, A.I.; West, K.P.; Black, R.E. Vitamin A Deficiency. In Comparative Quantification of Health Risks; Available online: http://www.who.int/publications/cra/chapters/volume1/0211-0256.pdf (accessed on 28 May 2020).
- Dewey, K.G.; Adu-Afarwuah, S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Mater. Child Nutr. 2008, 4, 24–85. [Google Scholar] [CrossRef]
- Imdad, A.; Yakoob, M.Y.; Bhutta, Z.A. Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health 2011, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Negash, C.; Belachew, T.; Henry, C.J.; Kebebu, A.; Abegaz, K.; Whiting, S.J. Nutrition education and introduction of broad bean-based complementary food improves knowledge and dietary practices of caregivers and nutritional status of their young children in Hula, Ethiopia. Food Nutr. Bull. 2014, 35, 480–486. [Google Scholar] [CrossRef]
- Ministry of Health Federal Democratic Republic of Ethiopia. Alive and Thrive. Complementary Feeding of Children 6 up to Months Old. Federal Democratic Republic of Ethiopia Ministry of Health. Available online: https://www.aliveandthrive.org/wp-content/uploads/2018/07/CF-Training-Manual-Nov-2012_English.pdf (accessed on 28 May 2020).
- Desai, A.; Smith, L.E.; Mbuya, M.N.; Chigumira, A.; Fundira, D.; Tavengwa, N.V.; Malaba, T.R.; Majo, F.D.; Humphrey, J.H.; Stoltzfus, R.J.; et al. The SHINE Trial Infant Feeding Intervention: Pilot Study of Effects on Maternal Learning and Infant Diet Quality in Rural Zimbabwe. Clin. Infect. Dis. 2015, 61, S710–S715. [Google Scholar] [CrossRef]
- Waswa, L.M.; Jordan, I.; Herrmann, J.; Krawinkel, M.B.; Keding, G.B. Community-based educational intervention improved the diversity of complementary diets in western Kenya: Results from a randomized controlled trial. Public Health Nutr. 2015, 18, 3406–3419. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations (FAO). Family Nutrition Guide. 2004. Available online: http://www.fao.org/3/a-y5740e.pdf (accessed on 15 June 2020).
- United Nations Children’s Fund (UNICEF). Key Messages Booklet: The Community Infant and Young Child Feeding Counselling Package. 2012. Available online: https://www.unicef.org/nutrition/files/Key_Message_Booklet_2012_small.pdf (accessed on 15 June 2020).
- Tariku, B.; Whiting, S.J.; Mulualem, D.; Singh, P. Application of the Health Belief Model to Teach Complementary Feeding Messages in Ethiopia. Ecol. Food Nutr. 2015, 54, 572–582. [Google Scholar] [CrossRef]
- Food Science and Nutrition Program—Addis Ababa University. Complementary Feeding of Children of 6 to 24 Months Old. 2011. Available online: https://www.sdgfund.org/sites/default/files/Ethiopia_%20Complementary%20feeding.pdf (accessed on 18 June 2020).
- United States Agency for International Development Behavior Change Interventions and Child Nutritional Status: Evidence from the Promotion of Improved Complementary Feeding Practices. 2011. Available online: http://iycn.wpengine.netdnacdn.com/files/IYCN_comp_feeding_lit_review_062711.pdf (accessed on 18 June 2020).
- Olney, D.K.; Pedehombga, A.; Ruel, M.T.; Dillon, A. A 2-Year Integrated Agriculture and Nutrition and Health Behavior Change Communication Program Targeted to Women in Burkina Faso Reduces Anemia, Wasting, and Diarrhea in Children 3–12.9 Months of Age at Baseline: A Cluster-Randomized Controlled Trial. J. Nutr. 2015, 145, 1317–1324. [Google Scholar] [CrossRef]
- Guyon, A.B.; Quinn, V.J.; Hainsworth, M.; Ravonimanantsoa, P.; Ravelojoana, V.; Rambeloson, Z.; Martin, L. Implementing an integrated nutrition package at large scale in madagascar: The essential nutrition actions framework. Food Nutr. Bull. 2009, 30, 233–244. [Google Scholar] [CrossRef]
- Mulualem, D.; Henry, C.J.; Berhanu, G.; Whiting, S.J. The effectiveness of nutrition education: Applying the Health Belief Model in child-feeding practices to use pulses for complementary feeding in Southern Ethiopia. Ecol. Food Nutr. 2016, 55, 308–323. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J. Introduction to Health Behavior Theory; Jones and Bartlett: Sudbury, MA, USA, 2009; pp. 31–44. [Google Scholar]
- Fadnes, L.T.; Nankabirwa, V.; Engebretsen, I.M.; Sommerfelt, H.; Birungi, N.; Lombard, C.; Swanevelder, S.; Van den Broeck, J.; Tylleskär, T.; Tumwine, J.K.; et al. Effects of an exclusive breastfeeding intervention for six months on growth patterns of 4-5 year old children in Uganda: The cluster-randomised PROMISE EBF trial. BMC Public Health 2016, 16, 555. [Google Scholar] [CrossRef] [PubMed]
- United Nations Children’s Fund (UNICEF). Community Based Infant and Young Child Feeding. Counselling Cards for Community Workers. 2010. Available online: http://www.unicef.org/nutrition/index_58362.html (accessed on 15 June 2020).
- Food and Agriculture Organization of the United Nations (FAO). What Works at Home? Improving Complementary Feeding Based on Locally Available Foods—Learning from Caregivers through Trials of Improved Practices in Kasungu and Mzimba districts of Malawi. 2014. Available online: http://www.fao.org/3/a-bc795e.pdf (accessed on 15 June 2020).
- Kang, Y.; Kim, S.; Sinamo, S.; Christian, P. Effectiveness of a community-based nutrition programme to improve child growth in rural Ethiopia: A cluster randomized trial. Matern. Child Nutr. 2017, 13. [Google Scholar] [CrossRef] [PubMed]
- Positive Deviance/Hearth: A Resource Guide for Sustainably Rehabilitating Malnourished Children. Child Survival Collaborations and Resources Group Nutrition Working Group. 2003. Available online: https://coregroup.org/wp-content/uploads/2017/09/Positive-Deviance-Hearth-Resource-Guide.pdf (accessed on 15 June 2020).
- Ethiopia Public Health Training Initiative Trainer’s Guide. Using the Essential Nutrition Actions to Improve the Nutrition of Women and Children in Ethiopia, including under Situations of Emergencies and HIV & AIDS. 2004. Available online: https://www.ennonline.net/attachments/96/trainers-guide.pdf (accessed on 15 June 2020).
- United Nations University. Positive Deviance in Child Nutrition (With Emphasis on Psychosocial and Behavioral Aspects and Implications for Development). [Internet] Tokyo, Japan. 1990. Available online: https://archive.unu.edu/unupress/unupbooks/80697e/80697E00.htm (accessed on 15 June 2020).
- Kang, Y.; Suh, Y.K.; Debele, L.; Juon, H.S.; Christian, P. Effects of a community-based nutrition promotion programme on child feeding and hygiene practices among caregivers in rural Eastern Ethiopia. Public Health Nutr. 2017, 20, 1461–1472. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kuchenbecker, J.; Reinbott, A.; Mtimuni, B.; Krawinkel, M.B.; Jordan, I. Nutrition education improves dietary diversity of children 6-23 months at communitylevel: Results from a cluster randomized controlled trial in Malawi. PLoS ONE 2017, 12, e0175216. [Google Scholar] [CrossRef] [PubMed]
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO). Breastfeeding counselling: A Training Course. 1993. Available online: https://www.who.int/maternal_child_adolescent/documents/who_cdr_93_3/en/ (accessed on 18 June 2020).
- World Health Organization (WHO). HIV and Infant Feeding Counselling Tools: Reference Guide. 2005. Available online: https://apps.who.int/iris/handle/10665/43191 (accessed on 18 June 2020).
- Muhoozi, G.K.M.; Atukunda, P.; Diep, L.M.; Mwadime, R.; Kaaya, A.N.; Skaare, A.B.; Willumsen, T.; Westerberg, A.C.; Iversen, P.O. Nutrition, hygiene, and stimulation education to improve growth, cognitive, language, and motor development among infants in Uganda: A cluster randomized trial. Matern. Child Nutr. 2018, 14, e12527. [Google Scholar] [CrossRef]
- Pan American Health Organization (PAHO); World Health Organization (WHO). Guiding Principles for Complementary Feeding of the Breastfed Child; Division of Health Promotion and Protection: Washington, DC, USA, 2003; Available online: https://www.who.int/nutrition/publications/guiding_principles_compfeeding_breastfed.pdf (accessed on 28 May 2020).
- Seetha, A.; Tsusaka, T.W.; Munthali, T.W.; Musukwa, M.; Mwangwela, A.; Kalumikiza, Z.; Manani, T.; Kachulu, L.; Kumwenda, N.; Musoke, M.; et al. How immediate and significant is the outcome of training on diversified diets, hygiene and food safety? An effort to mitigate child undernutrition in rural Malawi. Public Health Nutr. 2018, 21, 1156–1166. [Google Scholar] [CrossRef]
- Nutrition Work Group; Child Survival Collaborations and Resources Goup. Positive Deviance/Hearth: A Resource Guide for Sustainably Rehabilitating Malnourished Children. 2003. Available online: https://coregroup.org/wp-content/uploads/2017/09/PositiveDeviance-Hearth-Resource-Guide.pdf (accessed on 18 June 2020).
- Gelli, A.; Margolies, A.; Santacroce, M.; Roschnik, N.; Twalibu, A.; Katundu, M.; Moestue, H.; Alderman, H.; Ruel, M. Using a Community-Based Early Childhood Development Center as a Platform to Promote Production and Consumption Diversity Increases Children’s Dietary Intake and Reduces Stunting in Malawi: A Cluster-Randomized Trial. J. Nutr. 2018, 148, 1587–1597. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middleincome countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- International Food Policy Research Institute. The Agriculture-Nutrition Disconnect in India, What Do We Know. 2012. Available online: https://researchonline.lshtm.ac.uk/id/eprint/1440425/1/The_AgricultureNutrition_Disconnect_in_India_What_Do_We_Know.pdf (accessed on 18 June 2020).
- Bundy, D.A.P.; Burbano, C.; Grosh, M.; Gelli, A.; Jukes, M.D.L. Rethinking School Feeding: Social Safety Nets, Child Development, and the Education Sector. 2009. Available online: https://documents.wfp.org/stellent/groups/public/documents/reports/wfp284 (accessed on 28 May 2020).
- Somassè, Y.E.; Dramaix, M.; Traoré, B.; Ngabonziza, I.; Touré, O.; Konaté, M.; Diallo, M.; Donnen, P. The WHO recommendation of home fortification of foods with multiple micronutrient powders in children under 2 years of age and its effectiveness on anaemia and weight: A pragmatic cluster-randomized controlled trial. Public Health Nutr. 2018, 21, 1350–1358. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Guideline: Use of Multiple Micronutrient Powders for Home Fortification of Foods Consumed by Infants and Children 6–23 Months of Age. 2011. Available online: https://www.ncbi.nlm.nih.gov/books/NBK180125/ (accessed on 15 June 2020).
- Mbogori, T.; Murimi, M. Effects of a nutrition education intervention on maternal nutrition knowledge, dietary intake and nutritional status among food insecure households in Kenya. Int. J. Community Med. Public Health 2019, 6, 1831. [Google Scholar] [CrossRef]
- The Republic of Malawi Office of the President and Cabinet (OPC) Department of Nutrition, Hiv and Aids. Malawi National Nutrition Policy and Strategic Plan (2007–2011). Available online: https://extranet.who.int/nutrition/gina/sites/default/filesstore/MWI%202009%20National%20Nutrition%20Policy%20Strategic%20Plan%202009.pdf (accessed on 28 May 2020).
- Kajjura, R.B.; Veldman, F.J.; Kassier, S.M. Effect of Nutrition Education on Knowledge, Complementary Feeding, and Hygiene Practices of Mothers With Moderate Acutely Malnourished Children in Uganda. Food Nutr. Bull. 2019, 40, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Ministry of Health. Guidelines for Integrated Management of Acute Malnutrition in Uganda. Available online: http://library.health.go.ug/sites/default/files/resources/IMAM_Guidelines-for-Uganda-Jan-2016-FINAL-LORES2-2.pdf (accessed on 28 May 2020).
- Atukunda, P.; Muhoozi, G.K.M.; Westerberg, A.C.; Iversen, P.O. Nutrition, hygiene and stimulation education for impoverished mothers in rural Uganda: Effect on maternal depression symptoms and their associations to child development outcomes. Nutrients 2019, 11, 1561. [Google Scholar] [CrossRef]
- Atukunda, P.; Muhoozi, G.K.M.; van den Broek, T.J.; Kort, R.; Diep, L.M.; Kaaya, A.N.; Iversen, P.O.; Westerberg, A.C. Child development, growth and microbiota: Follow-up of a randomized education trial in Uganda. J. Glob. Health 2019, 9, 010431. [Google Scholar] [CrossRef]
- Hitachi, M.; Wanjihia, V.; Nyandieka, L.; Francesca, C.; Wekesa, N.; Changoma, J.; Muniu, E.; Ndemwa, P.; Honda, S.; Hirayama, K.; et al. Improvement of Dietary Diversity and Attitude toward Recommended Feeding through Novel Community Based Nutritional Education Program in Coastal Kenya—An Intervention Study. Int. J. Environ. Res. Public Health 2020, 17, 7269. [Google Scholar] [CrossRef]
- World Health Organization. Indicators for Assessing Infant and Young Child Feeding Practices, Part I: Definition; WHO Press: Geneva, Switzerland, 2008. [Google Scholar]
- Leroy, J.L.; Olney, D.K.; Nduwabike, N.; Ruel, M.T. Tubaramure, a Food-Assisted Integrated Health and Nutrition Program, Reduces Child Wasting in Burundi: A Cluster-Randomized Controlled Intervention Trial. J. Nutr. 2021, 151, 197–2005. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Complementary Feeding of Young Children in Developing Countries: A Review of Current Scientific Knowledge. 1998. Available online: https://www.who.int/nutrition/publications/infantfeeding/WHO_NUT_98.1/en/ (accessed on 15 June 2020).
- Roche, M.L.; Marquis, G.S.; Gyorkos, T.W.; Blouin, B.; Sarsoza, J.; Kuhnlein, H.V. A Community-Based Positive Deviance/Hearth Infant and Young Child Nutrition Intervention in Ecuador Improved Diet and Reduced Underweight. J. Nutr. Educ. Behav. 2017, 49, 196–203. [Google Scholar] [CrossRef]
- Penny, M.E.; Creed-Kanashiro, H.M.; Robert, R.C.; Narro, M.R.; Caulfield, L.E.; Black, R.E. Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: A cluster-randomised controlled trial. Lancet 2005, 365, 1863–1872. [Google Scholar] [CrossRef]
- Hop, L.T. Programs to improve production and consumption of animal source foods and malnutrition in Vietnam. J. Nutr. 2003, 133, 4006S–4009S. [Google Scholar] [CrossRef] [PubMed]
- Beyene, M.; Worku, A.G.; Wassie, M.M. Dietary diversity, meal frequency and associated factors among infant and young children in Northwest Ethiopia: Across- sectional study. BMC Public Health 2015, 15, 1007. [Google Scholar] [CrossRef]
- Belew, A.K.; Ali, B.M.; Abebe, Z.; Dachew, B.A. Dietary diversity and meal frequency among infant and young children: A community based study. Ital. J. Pediatr. 2017, 43, 73. [Google Scholar] [CrossRef]
- Michaud-Létourneau, I.; Gayard, M.; Pelletier, D.L. Contribution of the Alive & Thrive-UNICEF advocacy efforts to improve infant and young child feeding policies in Southeast Asia. Matern. Child Nutr. 2019, 15, e12683. [Google Scholar]
- Carpenter, C.J. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. 2010, 25, 661–669. [Google Scholar] [CrossRef]
- Bisits, P.A. The positive deviance/hearth approach to reducing child malnutrition: Systematic review. Trop. Med. Int. Health 2011, 16, 1354–1366. [Google Scholar] [CrossRef]
- Vilella, E. The Effect of a Nutrition-Specific Intervention on Nutritional Status in Moderate Acute Malnourished Children under five Years of Age in a Rural Area of Mozambique. Ph.D. Thesis, Rovira i Virgili University, Department of Basic Medical Sciences, 2017. Available online: https://www.tdx.cat/handle/10803/442982#page=1 (accessed on 3 October 2020).
- Jeihooni, A.K.; Hidarnia, A.; Kaveh, M.H.; Hajizadeh, E.; Askari, A. The effect of an educational program based on health belief model on preventing osteoporosis in women. Int. J. Prev. Med. 2015, 6, 115. [Google Scholar]
- D’Alimonte, M.R.; Deshmukh, D.; Jayaraman, A.; Chanani, S.; Humphries, D.L. Using Positive Deviance to Understand the Uptake of Optimal Infant and Young Child Feeding Practices by Mothers in an Urban Slum of Mumbai. Matern. Child Health J. 2016, 20, 1133–1142. [Google Scholar] [CrossRef]
- Lassi, Z.S.; Das, J.K.; Zahid, G.; Imdad, A.; Bhutta, Z.A. Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries: A systematic review. BMC Public Health 2013, 13, S13. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, M.; Rubert, L.; Pani, P. Specially formulated foods for treating children with moderate acute malnutrition in low- and middle-income countries. Cochrane Database Syst. Rev. 2013, 6, CD009584. [Google Scholar] [CrossRef] [PubMed]
- Hutton, G.B.; Brugulat-Panés, A.; Bhagtani, D.; Mba Maadjhou, C.; Birch, J.M.; Shih, H.; Okop, K.; Muti, M.; Wadende, P.; Tatah, L.; et al. A Systematic Scoping Review of the Impacts of Community Food Production Initiatives in Kenya, Cameroon, and South Africa. J. Glob. Health Rep. 2021, 5, e2021010. [Google Scholar] [PubMed]
- FAO; ECA; AUC. Africa Regional Overview of Food Security and Nutrition; FAO: Accra, Ghana, 2020; Available online: https://doi.org/10.4060/ca7343en (accessed on 3 October 2020).
| Author Ref. Year, Country | Type of Intervention | Intervention Methodology | Nutrition Indicators | Results | Q |
|---|---|---|---|---|---|
| Negash et al. 2014. Ethiopia [11] | RCT, EP Educational model: Workshops on infant feeding, practical demonstrations of supplemented baby food recipes. Visual material Alive and Thrive [12] | Realized by nutrition educators. IG N = 80/CG N = 73 Directed to mothers of infants 6 to 23 months of age (N = 153) Format: Group 12 sessions (twice a month; 120 min) | At 6 months post-intervention Boy: MDD and MMF Anthropometry, food consumption Mother: nutritional knowledge. Complementary feeding practices | IG N = 80/CG N = 73 Knowledge: 5.8 to 7.11 **/6.3 to 6.3 Complementary Feeding: 9.1 to 9.6 */9.1 to 9.1 Minimum Diet Diversity: 33 to 54%/32 to 14% Minimum meal frequency: 28 to 52%/25 to 32% Energy: 854 to 1045 Kcal/717 to 885 Kcal Protein: 24 to 28.7 g/20.6 to 21.6 p ≤ 0.05 Iron: 28.9 to 30.6 mg/16.9 to 20.9 p ≤ 0.05 Non-significant changes in nutritional classification | Q4 |
| Desai et al. 2015. Zimbabwe [13] | Quasi-experimental, EP Educational model: home visits on maternal and infant feeding and nutrition, delivery tools and activities to illustrate key concepts, fortified recipes. | Realized by: Health workers Directed to mothers of infants 6 to 12 months of age (N = 19) Format: individual home visits 4 month | Infants: food consumption Mother: nutritional knowledge | PRE-TEST-FINAL TEST (%met requirement) Energy 1759 (63%)–2635 (79%) p < 0.05 Protein 9.9 g (84%)–15.8 g (95%) p < 0.05 Fat 9.3 g (89%)–20 g (100%) p < 0.05 Vit. A 58 µg (79%)–678 µg (100%) p < 0.05 Folate 26.4 µg (31%)–119 µg (68%) p < 0.05 Calcium 58 mg (10%)–352 mg (89%) p < 0.05 Iron 2.4 mg (0%)–8.9 (68%) p < 0.05 Zinc 2.3 mg (16%)–11 (89%) p < 0.05 | Q1 |
| Waswa et al. 2015. Kenya [14] | RCT, EP Educational model: Workshops in infant feeding, practical demonstrations of cooking and recipes, practice food hygiene. FAO and UNICEF [15,16] | Realized by: Health workers Directed to mothers of infants 6 to 17 months of age (N = 207). Format: group and individual 4 sessions 2–5 h | At 12 months post-intervention. Infants: Anthropometry. MDD and MMF. Mother: nutritional knowledge | IG N = 110/CG N = 97 H/A −1.61 to −1.85/−1.31 to −1.50 W/A −0.87 to −0.74/−0.57 to −0.39 p = 0.022 W/H −0.04 to 0.25/0.15 to 0.49 Chronic malnutrition 29.3 to 49%/29.3 to 34% Low weight 17.2 to 8.2%/10.1 to 7.2% Acute malnutrition 2 to 0%/2 to 3.1% Minimum dietary diversity: 55.6 to 87.3%/50.5 to 55.7% p ≤ 0.001 Minimum meal frequency: 80.6 to 98.8%/88.9 to 88.6% p = 0.01 Nutritional knowledge: 8.21/21/3.66/21 p ≤ 0.001 | Q3 |
| Tariku et al. 2015. Ethiopia [17] | RCT, EP Educational model: Workshops on infant food and nutrition health believe model [18,19] | Realized by: Health workers and community volunteers Directed to Women with infants 6 to 18 months of age (N = 166) Format: 2 sessions/month for 3 months Group and individual | At the end of the intervention Infants: MDD and MMF | HBM N = 56A/TRADITIONAL METHOD N = 54B/CG N = 56C Minimum dietary diversity: versus AB and AC. p ≤ 0.001 Minimum meal frequency: versus AB and AC *. p ≤ 0.005 | Q4 |
| Olney et al. 2015. Burkina Faso [20] | RCT, AEP Contents: Domestic agriculture. Workshops on maternal and infant feeding and nutrition. Helen Keller International [21] | Carried out by: Leader mothers (LM +), health committee (HC) Directed to mothers of infants 3–12.9 months of age (N= 1481) Format: individual. Home visits 2 times/month for 6 months. | At 2 years post-intervention Infants: MDD, anthropometry and haemoglobin Mother: Knowledge | LM + N= 443A/HC = 441B/GC N = 597C H/A −1.06 to −1.77/−1.35 to −1.96/−1.29 to −1.91 Chronic malnutrition 28.5 to 43.5%/33.5 to 47%/30.3 to 47.7% W/H −0.98 to −0.66/−1.16 to −0.73/−0.96 to −0.66 Acute malnutrition 25.7 to 8.4%/30.8 to 8.6%/24.3 to 10.2% W/A −1.41 to −1.44/−1.73 to −1.62/−1.63 to −1.53 Under weight 31.9 to 26.5%/41.5 to 31.3%/39.5 to 31.4% Knowledge 34 to 75%/38 to 79%/42 to 63% p ≤ 0.05 ABC MDD 3% to 15%/1.7% to 18.2%/2.6% to 6.3% Haemoglobin 9 to 9.4 g/dl/8.87 to 9.87 g/dl/9.3 to 9.5 g/dl p ≤ 0.05CB Adjusted at 3–5.9 months of age | Q1 |
| Mulualem et al. 2016. Ethiopia [22] | RCT, EP Educational model: Workshops on infant food and nutrition. Health believe model and Alive-Thrive manual [18,23] | Realized by: Health workers Directed to mothers of infants 6 to 18 months of age (N = 160) Format: group and individual 2 sessions/month for 6 months | At 2 weeks post-intervention Infants: Anthropometry MMF Mother: Complementary feeding practices, nutritional knowledge | IG N = 80/CG N = 80 Nutritional knowledge 1.09 to 9.46 */1.48 to 1.68 p ≤ 0.05 Complementary feeding 1.31 to 7.6 */1.15 to1.23 p ≤ 0.05 W/H 0.42 to 2.20 */0.37 to 0.89 *. p ≤ 0.05 H/A −1.34 to −2.78 */−1.43 to −2.82 * W/A −0.39 to 0.31 */−0.43 to −0.73 * p ≤ 0.05 MUAC 13.09 to 13.34/13.06 to 13.19 Minimum meal frequency 86.2 to 83.3%/81.2 to 52.5% | Q4 |
| For the PROMISE-EBF Study Group et al., 2016. Uganda [24] | RCT, EP Educational model: Support workshops on breastfeeding, infant feeding and HIV. WHO [25,26] | Directed to Pregnant women and mothers of infants <6 months of age (Base N = 886; final line N = 466) Format: Individual 5 home visits/month during pregnancy and 4 visits after birth. | 5 years post-birth age Infants: anthropometry. | IG/CG H/A −0.45 to −1.78/−0.32 to −1.53 W/A −0.40 to −1.28/−0.16 to −1.06 Chronic malnutrition 12 to 41%/7 to 33% Low weight 8 to 26%/5 to 16% | Q2 |
| Kang et al. 2017. Ethiopia [27] | RCT, ESP Educational model: Workshops on infant feeding, practical demonstrations of recipes. Positive Deviance (PD)/Hearth [28,29,30] | Realized by community volunteers or health workers. Directed to Mothers of children 6 to 24 months of age (N = 1790) Format: group and individual 12 sessions over 12 months. | 12 months after the intervention. Infants: Anthropometry | IG N = 876/CG N = 914 Monthly growth effect H/A −0.074/−0.095. p = 0.001 W/A −0.032/−0.060. p ≤ 0.001 W/H 0.011/0.030. p ≤ 0.001 | Q3 |
| Kang et al. 2017. Ethiopia [31] | RCT, ESP Educational model: Workshops in infant feeding, practical demonstrations of recipes. Positive Deviance/Hearth [28,29,30] | Realized by community volunteers or health workers. Directed to Mothers of infants 6 to 24 months of age (N = 1199) Format: group and individual 12 sessions over 12 months. | 12 months after the intervention. Infants: MDD and MMF Mother: Handwashing. | IG N= 570/CG N= 629 Minimum meal frequency: 7.95 of 15/6.8 of 15 p = 0.003 Minimum dietary diversity: 4.68 out of 10/4.40 out of 10 Handwashing: 3.07 out of 6/2.64 out of 6 | Q3 |
| Kuchenbecker et al. 2017. Malawi [32] | RCT, AEP Educational model: Workshops on infant feeding, agricultural and livestock supplies, food hygiene practices, practical cooking demonstrations and recipes. FAO and UNICEF [33,34] | Realized by community volunteers Directed to agricultural mothers of infants 6 to 23 months of age (Base N = 832; final line N = 959) Format: Group 10 sessions of 2–3 h during 5 months | At 36 months post-intervention Infants: Anthropometry. MDD and MMF | IG/CG W/A −0.93 to −0.69/−0.86 to −0.76 H/A −1.81 to −1.79/−1.71 to −1.85 W/H 0.01 to 0.32/0.03 to 0.27 Minimum dietary diversity 61.9 to 71.1%/59.9 to 55.5% p = 0.01 Minimum meal frequency: 88.6 to 90.3%/80.4 to 81.6% | Q2 |
| Muhoozi et al. 2018 Uganda [35] | RCT, EP Educational model: food hygiene practices, infant feeding workshops, practical cooking and recipe demonstrations. WHO [36] | Realized by leaders in health team Directed to mothers of infants 6 to 8 months of age (N = 511) Format: group and individual 3 sessions (6–8 h/session) | Approx. 20–24 months old participants. Infants: Anthropometry | IG N = 243/CG N = 224 H/A −1.07 to −2.15/−1.2 to −2.25 W/A −0.63 to −0.87/−0.72 to −0.88 W/H 0.12 to 0.31/0.16 to 0.36 HCZ: 0.68 to 0.39/0.57 to 0.33 | Q2 |
| Seetha et al. 2018. Malawi [37] | Quasi-experimental, ESP Educational model: Workshops on infant feeding, practice food hygiene, provision of flour mix, practical cooking demonstrations and recipes. Positive Deviance/Hearth [38] | Realized by: Health workers Directed to mothers of infants <24 months of age (N = 179). Format: group 21 sessions, 3 h | At the end of the intervention Infants: Anthropometry. | RANDOM EFFECT W/H −0.70 to 0.85 p = 0.002 W/A −0.25 to 0.73 p = 0.000 H/A 0.59 to 0.18 p = 0.458 | Q3 |
| Gelli et al. 2018b. Malawi [39] | RCT, AEP Educational model: Workshops in infant feeding, practical demonstrations of cooking and recipes, food hygiene practices, domestic agriculture [40,41,42] | Realized by: Government trainers. Directed to farmers, parents, teachers in nursery schools. Format: group and individual 2 weeks training + 3 days/month. Monthly follow-ups. | At 12 months post-intervention Infants: Anthropometry Infants: Food consumption | Infants 6–24 months of age IG N = 155/CG N = 149 H/A −1.70 to −1.87/−1.61 to −2.29 p ≤ 0.05 Chronic malnutrition 41 to 45%/41 to 63%. p ≤ 0.05 W/H 0.12 to 0.04/0.09 to 0.09 Acute malnutrition 1 to 2%/3 to 1% W/A −0.68 to −1.05/−0.73 to −1.18 Low weight 14 to 16%/13 to 22% Participant 36–72 months of age N = 631/N = 617 H/A −1.75 to −1.70/−1.74 to −1.70 Chronic malnutrition 40 to 36%/39 to 36% W/H 0.09 to −0.06/0.11 to 0.08 Acute malnutrition 1 to 1%/2 to 1% W/A −1.08 to −1.16/−1.05 to −1.15 Low weight 17 to 34%/17 to 32% Energy 1273 to 1627 kcal/1321 to 1376 p ≤ 0.001 Protein 40 to 54 g/42 to 48 g p ≤ 0.05 Vitamin A 449 to 930 µg/600 to 1000 µg Iron 11 to 13 mg/11 to 12 mg. p ≤ 0.05 | Q1 |
| Somassè et al. 2018. Mali [43] | RCT, ESP Contents: Micronutrient supplementation and workshops on infant food and nutrition. WHO [36,44] | Realized by: community volunteers Directed to mothers of children 6–23 months of age (N = 722) Format: micronutrient supplementation and nutritional education (2 sessions/month) for 3 months | 3 months after the intervention Child: Anthropometry, haemoglobin | IG N = 396/CG N = 326 Weight change 0.76 kg/0.74 kg MUAC 3.4 mm/3.8 mm Change length 3 cm/2 cm Hemoglobin change 0.50 g/dl/0.9 g/dl p = 0.023 | Q3 |
| Mbogori et al. 2019, Kenya [45] | Quasi-experimental, EP Educational model: Workshops on infant food and nutrition, practical cooking demonstrations, food hygiene practices and child care [46] | Realized by women leaders and researchers Directed to mothers of infants <5 years (Mothers N= 48; Infants N = 45) Format: Group 5 days (two sessions/day 120–180 min) | At 6 months post-intervention. Infants: food consumption Infants: anthropometry, nutrition knowledge | Pre-test–post-test Vitamin A: 28.6–116.8 µg retinol p = 0.001 Calcium: 74.6–173.6 mg p = 0.001 Knowledge: 68–91% p = 0.004 Energy: 755–636 kcal Protein: 19.7–14.7 g Acute malnutrition 21.7–26% Chronic malnutrition 29–19% Low weight 29–22% Non-significant changes: W/H, H/A and W/A | NIJ |
| Kajjura et al. 2019, Uganda [47] | RCT, EP Educational model: practical food hygiene and workshops on complementary feeding and infant nutrition, practical cooking and recipe demonstrations. Health believe model [48,49] | Realized by Health workers aimed at mothers of infants 6 to 18 months of age, moderate acute malnutrition (N = 204) Format: Group 12 sessions (weekly for 3 months, 60 min) | At the end of the intervention Infants: MDD and MMF practices. Mother: knowledge of MDD, MMF, food hygiene. | IG N = 104 (supplemented porridge: sorghum-based malted porridge)/CG N = 100 (porridge supplemented with: soy and corn mix) Practices: Minimum meal frequency: 41 to 83.7%/40 to 93%. p = 0.038 Minimum dietary diversity: 8.7 to 77.9% **/18 to 88% ** N = 204 Base/post-intervention: Practices: Minimum meal frequency: 40.7% to 88.2% p ≤ 0.001 Minimum dietary diversity: 13.2% to 82.8% p ≤ 0.001 Food hygiene: 36.7% to 90.2% p ≤ 0.001 Knowledge: Minimum meal frequency: 2.21 to 2.82 **/2.1 to 2.83 ** Minimum dietary diversity: 3.76 to 5.63 **/3.76 to 6.14 ** Food hygiene: 2.13 to 3.31 **/2.08 to 3.52 ** | Q4 |
| Atukunda et al. 2019a. Uganda [50] | RCT, EP Educational model: food hygiene practices, infant feeding workshops, practical cooking and recipe demonstrations. WHO [36] | Realized by leaders in health team Directed to mothers of infants 6 to 8 months of age (N = 511) Format: group and individual 3 sessions (6–8 h/session) | Approx. 20–24 months old participants. Infants: Anthropometry | Baseline IG N = 263/CG N = 248 at 20–24 months of age IG N = 77/CG N = 78 Chronic malnutrition 20.9 to 41.6%/28 to 59% Low weight 9.5 to 7.8%/14.5 to 10.3% Acute malnutrition 4.6 to 3.9%/4.8 to 2.6% | Q1 |
| Atukunda et al. 2019b. Uganda [51] | RCT, EP Educational model: food hygiene practices, infant feeding workshops, practical cooking and recipe demonstrations. WHO [36] | Realized by leaders in health team Directed to mothers of infants 6 to 8 months of age (N = ±150) Format: group and individual 3 sessions (6–8 h/session) | Approx. 20–24 to 36 months of age Infants: Anthropometry. | Baseline IG N = 263/CG N = 248 at 20–24 months age IG N = 74–77/CG N = 73–78 Chronic malnutrition 20.9 to 18.1%/28 to 36% Low weight 9.5 to 8.3%/14.5 to 11.3% Acute malnutrition 4.6 to 4.2%/4.8 to 2.8% Growth from 20–24 months to 36 months old IG N= 74–77/CG N= 73–78 H/A −1.96 to −2.15/−2.07 to −2.65 p = 0.0001 W/A −0.76 to −0.98/−0.85 to −1.18 p = 0.40 W/H 0.26 to 0.44/0.45 to 0.84 p = −0.054 HCZ 0.30 to −0.34/0.61 to 0.05 p = 0.055 | Q1 |
| Hitachi et al. 2020. Kenya [52] | Quasi-experimental, EP Educational model: educational sessions maternal and child nutrition and follow-up consultations. WHO [53] | Realized by: community health workers Directed to household and children aged 6–59 months Format: educational sessions on maternal nutrition during pregnancy and lactation, breastfeeding, complementary feeding, diverse diet and food groups, hygiene and sanitation practices, supplements health program and family planning. | At the end of the intervention Household: diet quality, food consumption Child: Anthropometry | CG: N = 181 household; N = 113 children/ IG: N = 181 household; N = 67 children Household DDS 4.18 to 6.15 p ≤ 0.01/4.97 to 6.91 p ≤ 0.01 Child anthropometry H/A −1.56 to −1.55/−1.30 to −1.51 W/A −1.14 to −1.04/−0.89 to −0.97 W/A −0.44 to −0.22 p = 0.06/−0.24 to −0.16 | Q2 |
| Leroy et al. 2020. Burundi [54] | RCT, ESP Contents: 3 treatment arms and 1 control arm: 1 treatment arm (from pregnancy to 18 months); 2 treatment arm (from pregnancy to 24 months); 3 treatment arm (from birth to 24 months). Food ration, health services and behaviour change communication. | Directed to child 0–24 months Format: 3 treatment arms received household and individual (mother or child in the first 1000 days) food rations (corn-soy blend and micronutrient-fortified vegetable oil), The control arm received no rations or behaviour change communication. | At the end of the intervention Child: Anthropometry. | 1 treatment arm: N = 866; 2 treatment arm: N = 425; 3 treatment arm: N = 420/CG: N = 855 W/L 1 treatment arm: −0.3 to −0.1 W/L 2 treatment arm: −0.3 to −0.2 W/L 3 treatment arm: −0.3 to −0.3 W/L CG: −0.3 to −0.3 | Q1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jardí, C.; Casanova, B.D.; Arija, V. Nutrition Education Programs Aimed at African Mothers of Infant Children: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 7709. https://doi.org/10.3390/ijerph18147709
Jardí C, Casanova BD, Arija V. Nutrition Education Programs Aimed at African Mothers of Infant Children: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(14):7709. https://doi.org/10.3390/ijerph18147709
Chicago/Turabian StyleJardí, Cristina, Byron David Casanova, and Victoria Arija. 2021. "Nutrition Education Programs Aimed at African Mothers of Infant Children: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 14: 7709. https://doi.org/10.3390/ijerph18147709
APA StyleJardí, C., Casanova, B. D., & Arija, V. (2021). Nutrition Education Programs Aimed at African Mothers of Infant Children: A Systematic Review. International Journal of Environmental Research and Public Health, 18(14), 7709. https://doi.org/10.3390/ijerph18147709







