Physical Activity Barriers and Assets in Rural Appalachian Kentucky: A Mixed-Methods Study
Abstract
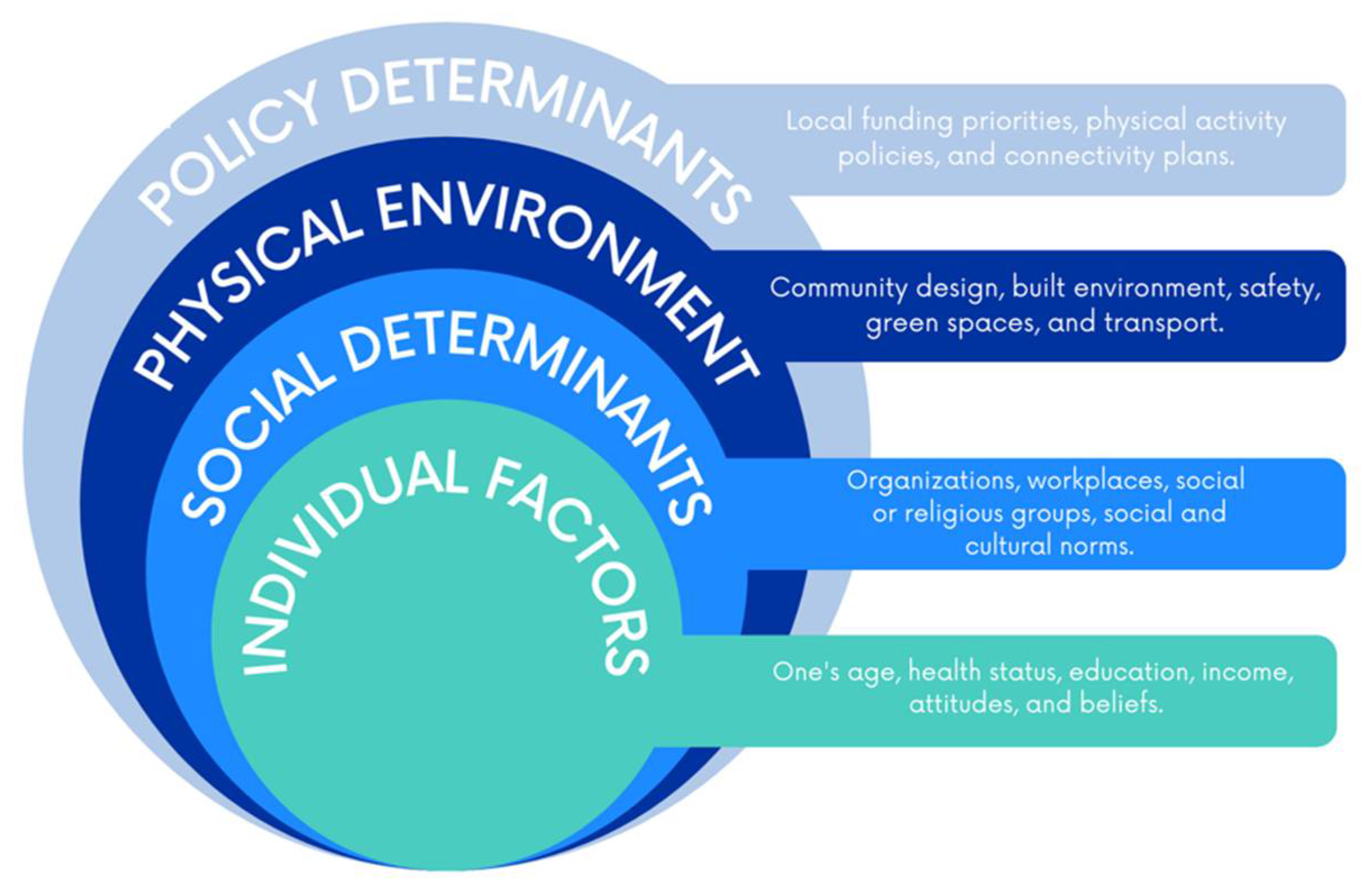
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Study Design
2.2.1. Cohort Survey Recruitment
2.2.2. Cohort Survey Measures
2.2.3. Cohort Survey Statistical Analysis
2.2.4. Focus Group Recruitment
2.2.5. Focus Group Analysis
3. Results
3.1. Individual Factors
“I think it just depends, I think some people live a very active lifestyle and then some I think it’s just completely a toss-up. You know, some people are never active, but you know I think there’s just a divide. I think that, I don’t think we have a fully active community.”
3.2. Social Determinants
“It’s never really been a part of our culture around here, it just isn’t. I mean we’re like the most unhealthy people in the country. This part, I mean that’s just honest, central Appalachia it is.”
“My mom and I for example, and mom’s like “I don’t really want to walk today” and I am like ok no big deal. But if Sarah called me and said, “Hey you are supposed to walk with us ` today at 6 o’clock”. I am like oh gosh, can’t let Sarah down. We got to get off your butt let’s go. You know what I am saying? It is that unknown person that would come in and motivate some people because like my mom won’t do anything, I ask her to do anyways.”
3.3. Physical Environment
“No, I wouldn’t drive over here to walk on a trail cause it’s 30 min for me to get here.”
“You have hollers everywhere that people can’t, they have no way to get here [to town with recreation facilities].”
“When I walk up there to the tower, I always have a gun, because there has been bears spotted up in there you know and all.”
“(Referring to a local park) They are finding a lot of needles over there. Cause the last birthday party we had over there, people was afraid to turn their kids loose.”
“We are a lot of back roads. You know, there’s not sidewalks everywhere.”
“I mean anyone with knee trouble, back trouble, disabilities would have trouble. You couldn’t do it with a wheelchair you would have to stay on the road.”
3.4. Policy Determinants
“We need more parks, the parks we have need updated equipment, that sort of thing. Or livability type issues, you need to be able to safely walk a stroller around town and have someplace to go.”
“There’s trails, I mean we have one of the most beautiful places in the world to get out and do stuff.”
“I think that there’s a lot more grassroots stuff happening here now like we’re taking our communities back and we’re fixing it ourselves instead of people coming in and trying to fix us like they’ve always done. And it’s a power of the people and I think that’s what it is.”
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- 2018 Physical Activity Guidelines Advisory Committee. In 2018 Physical Activity Guidelines Advisory Committee Scientific Report; Department of Health and Human Services: Washington, DC, USA, 2018; Available online: https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf (accessed on 12 April 2021).
- Centers for Disease Control and Prevention. Prevalence of Self-Reported Physical Inactivity among US Adults by State and Territory, BRFSS, 2015–2018. Available online: https://www.cdc.gov/physicalactivity/data/inactivity-prevalence-maps/index.html (accessed on 12 April 2021).
- Whitefield, G.P.; Carlson, S.A.; Ussery, E.N.; Fulton, J.E.; Galuska, D.A.; Peterson, R. Trends in Meeting Physical Activity Guidelines among Urban and Rural Dwelling Adults—United States, 2008–2017. Morb. Mortal. Wkly. Rep. 2019, 68, 513–518. Available online: https://www.cdc.gov/mmwr/volumes/68/wr/mm6823a1.htm (accessed on 12 April 2021). [CrossRef] [PubMed]
- Appalachian Regional Commission. Health Disparities Related to Obesity in Appalachia. 2019. Available online: https://www.arc.gov/wp-content/uploads/2020/06/HealthDisparitiesRelatedtoObesityinAppalachiaApr2019.pdf (accessed on 12 April 2021).
- Hales, C.M.; Fryar, C.D.; Carroll, M.D.; Freedman, D.S.; Ogden, C.L. Trends in Obesity and Severe Obesity Prevalence in US Youth and Adults by Sex and Age, 2007–2008 to 2015–2016. JAMA 2018, 319, 1723–1725. [Google Scholar] [CrossRef] [PubMed]
- Wen, M.; Fan, J.X.; Kowaleski-Jones, L.; Wan, N. Rural-Urban Disparities in Obesity Prevalence among Working Age Adults in the United States: Exploring the Mechanisms. Am. J. Health Promot. AJHP 2018, 32, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Trust for America’s Health. State of Obesity. 2019. Available online: https://www.tfah.org/wp-content/uploads/2019/09/2019ObesityReportFINAL-1.pdf (accessed on 12 April 2021).
- Appalachian Regional Commission. Health Disparities in Appalachia. 2017. Available online: https://www.arc.gov/wp-content/uploads/2020/06/Health_Disparities_in_Appalachia_August_2017.pdf (accessed on 12 April 2021).
- Richard, L.; Gauvin, L.; Raine, K. Ecological Models Revisited: Their Uses and Evolution in Health Promotion Over Two Decades. Annu. Rev. Public Health 2011, 32, 307–326. [Google Scholar] [CrossRef]
- Springer, A.E.; Evans, A.E.; Ortuño, J.; Salvo, D.; Varela Arévalo, M.T. Health by Design: Interweaving Health Promotion into Environments and Settings. Front. Public Health 2017, 5, 268. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.F.; Martin, B.W. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Schoenberg, N.E.; Howell, B.M.; Swanson, M.; Grosh, C.; Bardach, S. Perspectives on healthy eating among Appalachian residents. J. Rural Health 2013, 29, s25–s34. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Annu. Rrev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef] [PubMed]
- Chrisman, M.; Nothwehr, F.; Janz, K.; Yang, J.; Oleson, J. Perceived Resources and Environmental Correlates of Domain-Specific Physical Activity in Rural Midwestern Adults. J. Phys. Act. Health 2015, 12, 962–967. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gilbert, A.S.; Duncan, D.D.; Beck, A.M.; Eyler, A.A.; Brownson, R.C. A Qualitative Study Identifying Barriers and Facilitators of Physical Activity in Rural Communities. J. Environ. Public Health 2019, 2019, 7298692. [Google Scholar] [CrossRef] [PubMed]
- McGladrey, M.; Carman, A.; Nuetzman, C.; Peritore, N. Extension as a Backbone Support Organization for Physical Activity Promotion: A Collective Impact Case Study From Rural Kentucky. J. Phys. Act. Health 2020, 17, 62–67. [Google Scholar] [CrossRef] [PubMed]
- US Census Bureau. QuickFacts, Martin County, Kentucky. Available online: https://www.census.gov/quickfacts/martincountykentucky (accessed on 22 June 2021).
- US Census Bureau. Commuting Characteristics, Martin County, Kentucky. Available online: https://data.census.gov/cedsci/table?q=martin%20county%20kentucky&tid=ACSST5Y2019.S0801&hidePreview=false.Published2019 (accessed on 8 February 2021).
- DeWitt, E.; Gillespie, R.; Norman-Burgdolf, H.; Cardarelli, K.M.; Slone, S.; Gustafson, A. Rural SNAP Participants and Food Insecurity: How Can Communities Leverage Resources to Meet the Growing Food Insecurity Status of Rural and Low-Income Residents? Int. J. Environ. Res. Public Health 2020, 17, 6037. [Google Scholar] [CrossRef] [PubMed]
- Kristin, J.; Der Ananian, C.A.; Ainsworth, B.E. Validity and Reliability of the Global Physical Activity Questionnaire (GPAQ). Meas. Phys. Educ. Exerc. Sci. 2013, 17, 221–235. [Google Scholar]
- Donahue, K.E.; Mielenz, T.J.; Sloane, P.D.; Callahan, L.F.; Devellis, R.F. Identifying supports and barriers to physical activity in patients at risk for diabetes. Prev. Chronic Dis. 2006, 3, A119. [Google Scholar] [PubMed]
- Ibrahim, S.; Karim, N.A.; Oon, N.L.; Ngah, W.Z.W. Perceived physical activity barriers related to body weight status and sociodemographic factors among Malaysian men in Klang Valley. BMC Public Health 2013, 13, 275. [Google Scholar] [CrossRef] [PubMed]
- Cardarelli, K.; DeWitt, E.; Gillespie, R.; Norman-Burgdolf, H.; Jones, N.; Mullins, J.T. “We’re, Like, the Most Unhealthy People in the Country”: Using an Equity Lens to Reduce Barriers to Healthy Food Access in Rural Appalachia. Prev. Chronic. Dis. 2020, 17, 200340. [Google Scholar] [CrossRef] [PubMed]
- America's Health Rankings, United Health Foundation. Analysis of CDC, Behavioral Risk Factor Surveillance System. 2019. Available online: https://www.americashealthrankings.org/explore/annual/measure/Sedentary/state/KY (accessed on 12 April 2021).
- County Health Rankings & Roadmaps. Kentucky, Martin County Demographics. 2020. Available online: https://www.countyhealthrankings.org/app/kentucky/2020/rankings/martin/county/outcomes/overall/snapshot (accessed on 12 April 2021).
- Kruger, T.M.; Swanson, M.; Davis, R.E.; Wright, S.; Dollarhide, K.; Schoenberg, N.E. Formative research conducted in rural Appalachia to inform a community physical activity intervention. Am. J. Health Promot. AJHP 2012, 26, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Barnidge, E.K.; Radvanyi, C.; Duggan, K.; Motton, F.; Wiggs, I.; Baker, E.A.; Brownson, R.C. Understanding and addressing barriers to implementation of environmental and policy interventions to support physical activity and healthy eating in rural communities. J. Rural Health 2013, 29, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Umstattd Meyer, M.R.; Moore, J.B.; Abildso, C.; Edwards, M.B.; Gamble, A.; Baskin, M.L. Rural Active Living: A Call to Action. J. Public Health Manag. Pract. JPHMP 2016, 22, E11–E20. [Google Scholar] [CrossRef] [PubMed]
- Lyn, R.; Aytur, S.; Davis, T.A.; Eyler, A.A.; Evenson, K.R.; Chriqui, J.F.; Brownson, R.C. Policy, systems, and environmental approaches for obesity prevention: A framework to inform local and state action. J. Public Health Manag. Pract. JPHMP 2013, 19 (Suppl. 1), S23. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Cohort Study (N = 152) | Focus Group (N = 34) |
|---|---|---|
| Age, M (SD) | 54.7 (15.3) | 50.4 (13.1) years |
| Gender, n (%) | ||
| Female | 99 (65.1%) | 27 (79%) |
| Male | 53 (34.9%) | 7 (21%) |
| Race, n (%) | ||
| White | 150 (98.7%) | 34 (100%) |
| Education, n (%) | ||
| 11th grade or less | 66 (43.4%) | 1 (3%) |
| High school graduate | 55 (36.2%) | 4 (12%) |
| Some college | 17 (11.2%) | 12 (35%) |
| College graduate | 14 (9.2%) | 17 (50%) |
| Household Income, n (%) | ||
| Less than $20,000 | 90 (60.4%) | 8 (23%) |
| $21,000–59,999 | 44 (29.5%) | 13 (38%) |
| $60,000 and above | 15 (10.1%) | 13 (38%) |
| Inactive (n = 48) | Mod. Active (n = 67) | Active (n = 37) | All (n = 152) | p-Value | |
|---|---|---|---|---|---|
| Lack of time ** | 16 (34.8%) | 44 (66.7%) | 21 (56.8%) | 81 (54.4%) | 0.004 |
| Lack of energy or motivation | 36 (80.0%) | 58 (87.9%) | 26 (70.3%) | 120 (81.1%) | 0.089 |
| Lack of space * | 13 (28.3%) | 34 (51.5%) | 15 (41.7%) | 62 (41.9%) | 0.049 |
| Access to reliable childcare | 7 (15.2%) | 10 (15.2%) | 6 (16.7%) | 23 (15.5%) | 0.977 |
| Access to facilities or space to be active ** | 13 (28.3%) | 38 (57.6%) | 10 (27.8%) | 61 (41.2%) | 0.001 |
| Access to proper clothing or shoes for activity * | 13 (28.3%) | 30 (45.5%) | 8 (22.2%) | 51 (34.5%) | 0.035 |
| Access to safe places to walk *** | 14 (30.4%) | 41 (62.1%) | 8 (22.2%) | 63 (42.6%) | <0.001 |
| Cost | 11 (23.9%) | 27 (40.9%) | 8 (22.2%) | 46 (31.1%) | 0.067 |
| Weather * | 26 (56.5%) | 50 (75.8%) | 28 (77.8%) | 104 (70.3%) | 0.048 |
| Self-conscious | 17 (37.0%) | 34 (51.5%) | 15 (41.7%) | 66 (44.6%) | 0.288 |
| Health condition (such as asthma, COPD, or arthritis) * | 35 (76.1%) | 40 (60.6%) | 18 (50.0%) | 93 (62.8%) | 0.046 |
| Injury (such as a broken bone, recovery from surgery) | 22 (47.8%) | 27 (40.9%) | 15 (41.7%) | 64 (43.2%) | 0.750 |
| Lack of self-discipline | 23 (50.0%) | 41 (63.1%) | 20 (55.6%) | 84 (57.1%) | 0.381 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jones, N.; Dlugonski, D.; Gillespie, R.; DeWitt, E.; Lianekhammy, J.; Slone, S.; Cardarelli, K.M. Physical Activity Barriers and Assets in Rural Appalachian Kentucky: A Mixed-Methods Study. Int. J. Environ. Res. Public Health 2021, 18, 7646. https://doi.org/10.3390/ijerph18147646
Jones N, Dlugonski D, Gillespie R, DeWitt E, Lianekhammy J, Slone S, Cardarelli KM. Physical Activity Barriers and Assets in Rural Appalachian Kentucky: A Mixed-Methods Study. International Journal of Environmental Research and Public Health. 2021; 18(14):7646. https://doi.org/10.3390/ijerph18147646
Chicago/Turabian StyleJones, Natalie, Deirdre Dlugonski, Rachel Gillespie, Emily DeWitt, Joann Lianekhammy, Stacey Slone, and Kathryn M. Cardarelli. 2021. "Physical Activity Barriers and Assets in Rural Appalachian Kentucky: A Mixed-Methods Study" International Journal of Environmental Research and Public Health 18, no. 14: 7646. https://doi.org/10.3390/ijerph18147646
APA StyleJones, N., Dlugonski, D., Gillespie, R., DeWitt, E., Lianekhammy, J., Slone, S., & Cardarelli, K. M. (2021). Physical Activity Barriers and Assets in Rural Appalachian Kentucky: A Mixed-Methods Study. International Journal of Environmental Research and Public Health, 18(14), 7646. https://doi.org/10.3390/ijerph18147646






