Association of Tooth Scaling with Acute Myocardial Infarction and Analysis of the Corresponding Medical Expenditure: A Nationwide Population-Based Study
Abstract
1. Introduction
2. Materials and Methods
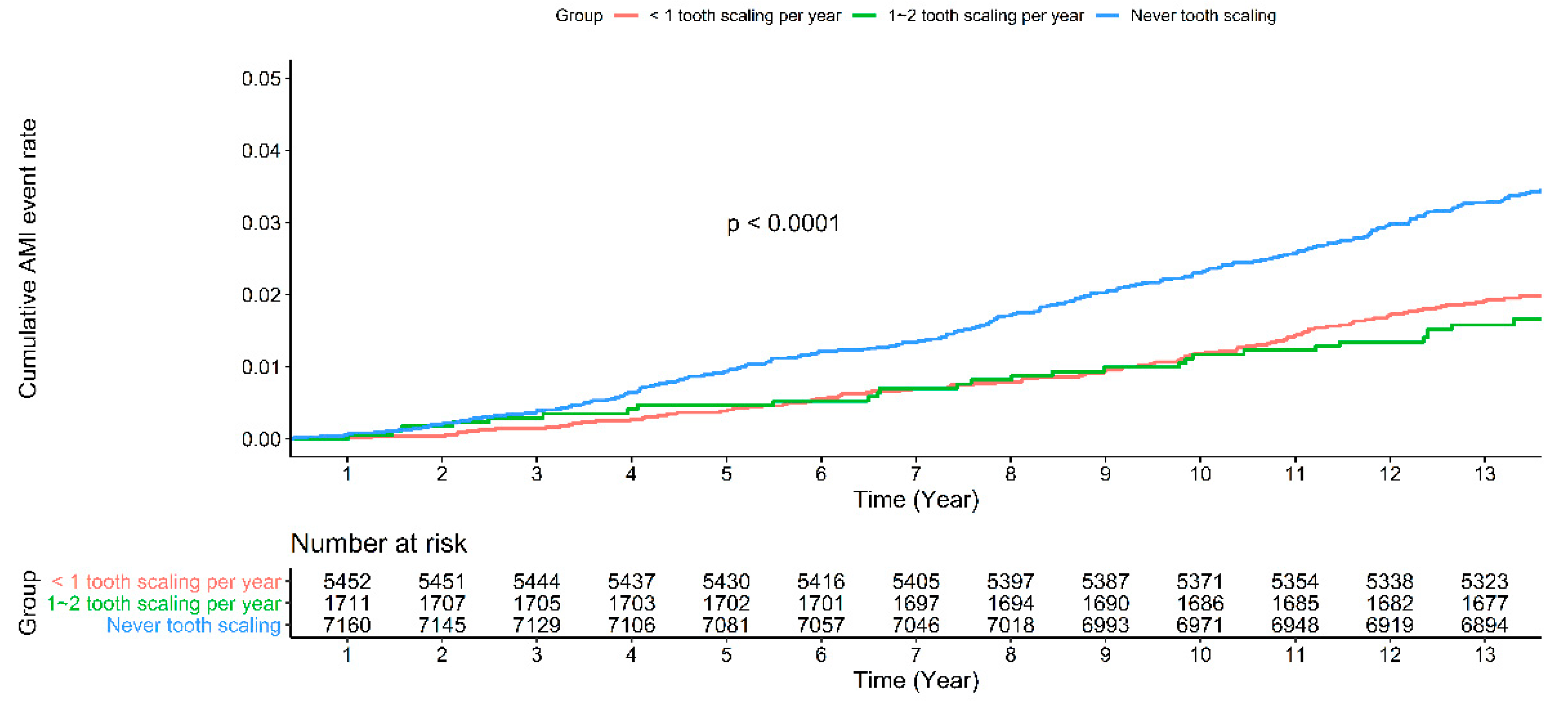
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Scannapieco, F. Role of Oral Bacteria in Respiratory Infection. J. Periodontol. 1999, 70, 793–802. [Google Scholar] [CrossRef]
- Petersen, P.E.; Yamamoto, T. Improving the oral health of older people: The approach of the WHO Global Oral Health Programme. Community Dent. Oral Epidemiol. 2005, 33, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.-Y.; Chiang, C.-H.; Huang, C.-C.; Chung, C.-M.; Chan, W.-L.; Huang, P.-H.; Lin, S.-J.; Chen, J.-W.; Leu, H.-B. The Association of Tooth Scaling and Decreased Cardiovascular Disease: A Nationwide Population-based Study. Am. J. Med. 2012, 125, 568–575. [Google Scholar] [CrossRef]
- Chen, S.-J.; Liu, C.-J.; Chao, T.-F.; Wang, K.-L.; Wang, F.-D.; Chen, T.-J.; Chiang, C.-E. Dental Scaling and Risk Reduction in Infective Endocarditis: A Nationwide Population-Based Case-Control Study. Can. J. Cardiol. 2013, 29, 429–433. [Google Scholar] [CrossRef]
- Yu, H.-C.; Su, N.-Y.; Huang, J.-Y.; Lee, S.-S.; Chang, Y.-C. Trends in the prevalence of periodontitis in Taiwan from 1997 to 2013: A nationwide population-based retrospective study. Medicine 2017, 96, e8585. [Google Scholar] [CrossRef]
- Madi, M.; Abuohashish, H.M.; Attia, D.; AlQahtani, N.; Alrayes, N.; Pavlic, V.; Bhat, S.G. Association between Periodontal Disease and Comorbidities in Saudi’s Eastern Province. BioMed Res. Int. 2021, 2021, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Zhen, Z.; Pelekos, G.; Yiu, K.H.; Jin, L. Periodontal disease increases the risk for onset of systemic comorbidities in dental hospital attendees: An 18-year retrospective cohort study. J. Periodontol. 2018, 90, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Holmstrup, P.; Damgaard, C.; Olsen, I.; Klinge, B.; Flyvbjerg, A.; Nielsen, C.H.; Hansen, P.R. Comorbidity of periodontal disease: Two sides of the same coin? An introduction for the clinician. J. Oral Microbiol. 2017, 9, 1332710. [Google Scholar] [CrossRef] [PubMed]
- Campus, G.; Salem, A.; Uzzau, S.; Baldoni, E.; Tonolo, G. Diabetes and Periodontal Disease: A Case-Control Study. J. Periodontol. 2005, 76, 418–425. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Tu, S.-T.; Sheu, W.H.-H. 2019 Diabetes Atlas: Achievements and challenges in diabetes care in Taiwan. J. Formos. Med. Assoc. 2019, 118, S130–S134. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.-C.; Suen, Y.-J.; Wang, Y.-H.; Lin, T.-C.; Yu, H.-C.; Chang, Y.-C. The Association of Periodontal Treatment and Decreased Pneumonia: A Nationwide Population-Based Cohort Study. Int. J. Environ. Res. Public Heal. 2020, 17, 356. [Google Scholar] [CrossRef]
- Tai, T.-W.; Lin, T.-C.; Ho, C.-J.; Yang, Y.-H.K.; Yang, C.-Y. Frequent Dental Scaling Is Associated with a Reduced Risk of Periprosthetic Infection following Total Knee Arthroplasty: A Nationwide Population-Based Nested Case-Control Study. PLoS ONE 2016, 11, e0158096. [Google Scholar] [CrossRef]
- Guo, S.; Fraser, M.W. Propensity Score Analysis: Statistical Methods and Applications; SAGE: St. Louis, MO, USA, 2014; Volume 11. [Google Scholar]
- Health Promotion Administration, M.o.H.a.W. National Health Interview Survey, NHIS. Available online: https://www.hpa.gov.tw/Pages/List.aspx?nodeid=236 (accessed on 27 December 2017).
- Worthington, H.V.; Clarkson, J.E.; Bryan, G.; Beirne, P.V. Routine scale and polish for periodontal health in adults. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef] [PubMed]
- Danesh, J.; Collins, R.; Peto, R. Chronic infections and coronary heart disease: Is there a link? Lancet 1997, 350, 430–436. [Google Scholar] [CrossRef]
- Qin, X.; Zhao, Y.; Guo, Y. Periodontal disease and myocardial infarction risk: A meta-analysis of cohort studies. Am. J. Emerg. Med. 2021, 48, 103–109. [Google Scholar] [CrossRef]
- Sanz, M.; Del Castillo, A.M.; Jepsen, S.; Juanatey, J.R.G.; D’Aiuto, F.; Bouchard, P.; Chapple, I.; Dietrich, T.; Gotsman, I.; Graziani, F.; et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 2020, 47, 268–288. [Google Scholar] [CrossRef]
- Moutsopoulos, N.M.; Madianos, P.N. Low-Grade Inflammation in Chronic Infectious Diseases: Paradigm of Periodontal Infections. Ann. N. Y. Acad. Sci. 2006, 1088, 251–264. [Google Scholar] [CrossRef] [PubMed]
- Seymour, G.; Ford, P.; Cullinan, M.; Leishman, S.; Yamazaki, K. Relationship between periodontal infections and systemic disease. Clin. Microbiol. Infect. 2007, 13, 3–10. [Google Scholar] [CrossRef]
- Weng, Y.-M.; Ng, C.-J.; Seak, C.-J.; Chien, C.-Y.; Chen, K.-F.; Lin, J.-R.; Chang, C.-J. One-year survival rate and healthcare costs after cardiac arrest in Taiwan, 2006–2012. PLoS ONE 2018, 13, e0196687. [Google Scholar] [CrossRef] [PubMed]
- Suchard, J.R.; Fenton, F.R.; Powers, R.D. Medicare expenditures on unsuccessful out-of-hospital resuscitations. J. Emerg. Med. 1999, 17, 801–805. [Google Scholar] [CrossRef]
- Bishu, K.G.; Lekoubou, A.; Kirkland, E.; Schumann, S.O.; Schreiner, A.; Heincelman, M.; Moran, W.P.; Mauldin, P.D. Estimating the Economic Burden of Acute Myocardial Infarction in the US: 12 Year National Data. Am. J. Med Sci. 2020, 359, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Zhang, M.; Zhang, Y.; Su, X.; Chen, J.; Xu, B.; Tao, J.; Wang, Z.; Ma, A.; Li, H. Economic Burden of Myocardial Infarction Combined with Dyslipidemia. Front. Public Heal. 2021, 9, 648172. [Google Scholar] [CrossRef] [PubMed]
- Shiyovich, A.; Gilutz, H.; Arbelle, J.E.; Greenberg, D.; Plakht, Y. Temporal trends in healthcare resource utilization and costs following acute myocardial infarction. Isr. J. Heal. Policy Res. 2020, 9, 1–10. [Google Scholar] [CrossRef]
- Chu, D.; Lee, Y.-L.; Hu, H.-Y.; Chou, P. Dental prophylaxis decreases the risk of acute myocardial infarction: A nationwide population-based study in Taiwan. Clin. Interv. Aging 2015, 10, 175–182. [Google Scholar] [CrossRef][Green Version]
- Wu, T.-Y.; Majeed, A.; Kuo, K.N. An overview of the healthcare system in Taiwan. Lond. J. Prim. Care 2010, 3, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Council, N.D. Taiwan White Paper: American Chamber of Commerce in Taipei. Available online: https://ws.ndc.gov.tw/Download.ashx?u=LzAwMS9hZG1pbmlzdHJhdG9yLzEwL3JlbGZpbGUvNzEwOC8zNDIxOC85OWJhMWJjOC02NmQ4LTQzMGYtOTlmOC1kMmNlZWRmODJkYjMucGRm&n=576O5ZyL5ZWG5pyD44CMMjAxOeWPsOeBo%2beZveearuabuOOAjeS4reiLseaWh%2beJiC5wZGY%3d&icon=.pdf%20 (accessed on 13 January 2021).
- Chen, S.-J.; Liu, C.-J.; Chao, T.-F.; Wang, K.-L.; Chen, T.-J.; Chou, P.; Wang, F.-D.; Lin, S.-J.; Chiang, C.-E. Dental scaling and atrial fibrillation: A nationwide cohort study. Int. J. Cardiol. 2013, 168, 2300–2303. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.-C.; Tung, Y.-C.; Wu, P.; Wu, L.-S.; Lin, Y.-S.; Chang, C.J.; Kung, S.; Chu, P.-H. Dental Procedures and the Risk of Infective Endocarditis. Medicine 2015, 94, e1826. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.-L.; Chen, W.-K.; Lin, C.-L.; Lai, C.-Y.; Kao, C.-H.; Chiang, H.-H.; Yang, T.-Y.; Shih, H.-M. Association between intensive periodontal treatment and spontaneous intracerebral hemorrhage—A nationwide, population-based cohort study. Medicine 2019, 98, e14814. [Google Scholar] [CrossRef]
| Tooth Scaling Group | Comparison Group | p-Value | |
|---|---|---|---|
| n | 7164 | 7164 | |
| Gender = male (%) | 3307 (46.2) | 3307 (46.2) | 1.000 |
| Age (mean (SD)) | 56.10 (4.34) | 56.09 (4.35) | 0.820 |
| Hypertension = Yes (%) | 1545 (21.6) | 1468 (20.5) | 0.119 |
| Diabetes mellitus = Yes (%) | 741 (10.3) | 734 (10.2) | 0.869 |
| Hyperlipidemia = Yes (%) | 751 (10.5) | 749 (10.5) | 0.978 |
| Coronary artery disease = Yes (%) | 514 (7.2) | 512 (7.1) | 0.974 |
| Chronic renal disease = Yes (%) | 201 (2.8) | 185 (2.6) | 0.439 |
| Tooth Scaling Group | Comparison Group | |
|---|---|---|
| n | 7164 | 7164 |
| Acute myocardial infarction = Yes (%) | 136 ( 1.9) | 250 (3.5) |
| Hazard Ratio(95%CI) | 0.543 (0.441, 0.670) 1 | 1.000 (reference) |
| All tooth scaling expenditure | 2,916,823 | 0 |
| Total exp. in dental (exclude tooth scaling) | 10,098,446 | 1,273,043 |
| All acute myocardial infarction (AMI) expenditure | 32,419,393 | 58,543,492 |
| All acute myocardial infarction (AMI) expenditure/per person share | 4525.32 | 8171.90 |
| Ratio of AMI expenditure/All of expenditure | 1.25% | 1.55% |
| Sum of expenditure Total expenditure | 45,434,66 23,625,412,192 | 59,816,535 3,851,848,824 |
| Avg. Number Per Year | Group A | Group B | |
|---|---|---|---|
| <1 Tooth Scaling | 1–2 Tooth Scaling | p-Value | |
| n | 5453 | 1711 | |
| Gender = male (%) | 2532 (46.4) | 775 (45.3) | 0.426 |
| Age (mean (SD)) | 56.21 (4.35) | 55.76 (4.30) | <0.001 |
| Hypertension = Yes (%) | 1227 (22.5) | 318 (18.6) | 0.001 |
| Diabetes mellitus = Yes (%) | 579 (10.6) | 162 (9.5) | 0.188 |
| Hyperlipidemia = Yes (%) | 550 (10.1) | 201 (11.7) | 0.056 |
| Coronary artery disease = Yes (%) | 402 (7.4) | 112 (6.5) | 0.271 |
| Chronic renal disease = Yes (%) | 154 (2.8) | 47 (2.7) | 0.932 |
| Charlson comorbidity index (%) | 0.345 | ||
| 0 | 4353 (79.8) | 1364 (79.7) | |
| 1~2 | 840 (15.4) | 278 (16.2) | |
| 3+ | 260 (4.8) | 69 (4.0) |
| Group A | Group B | p-Value | |
|---|---|---|---|
| Avg. number per year | <1 tooth scaling | 1–2 tooth scaling | |
| N | 5453 | 1711 | |
| Acute myocardial infarction = Yes (%) | 108 (2.0) | 28 (1.6) | 0.419 |
| Adjusted Hazard Ratio(95%CI) | 0.557(0.444, 0.698) | 0.497(0.336, 0.734) | <0.001 |
| average exp. in dental (mean (SD)) | 1405.05 (1627.22) | 3128.87 (1441.73) | <0.001 |
| number of visits to the dentist (mean (SD)) | 1.22 (0.86) | 2.84 (1.16) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kao, Y.-W.; Shia, B.-C.; Chiang, H.-C.; Chen, M.; Wu, S.-Y. Association of Tooth Scaling with Acute Myocardial Infarction and Analysis of the Corresponding Medical Expenditure: A Nationwide Population-Based Study. Int. J. Environ. Res. Public Health 2021, 18, 7613. https://doi.org/10.3390/ijerph18147613
Kao Y-W, Shia B-C, Chiang H-C, Chen M, Wu S-Y. Association of Tooth Scaling with Acute Myocardial Infarction and Analysis of the Corresponding Medical Expenditure: A Nationwide Population-Based Study. International Journal of Environmental Research and Public Health. 2021; 18(14):7613. https://doi.org/10.3390/ijerph18147613
Chicago/Turabian StyleKao, Yi-Wei, Ben-Chang Shia, Huei-Chen Chiang, Mingchih Chen, and Szu-Yuan Wu. 2021. "Association of Tooth Scaling with Acute Myocardial Infarction and Analysis of the Corresponding Medical Expenditure: A Nationwide Population-Based Study" International Journal of Environmental Research and Public Health 18, no. 14: 7613. https://doi.org/10.3390/ijerph18147613
APA StyleKao, Y.-W., Shia, B.-C., Chiang, H.-C., Chen, M., & Wu, S.-Y. (2021). Association of Tooth Scaling with Acute Myocardial Infarction and Analysis of the Corresponding Medical Expenditure: A Nationwide Population-Based Study. International Journal of Environmental Research and Public Health, 18(14), 7613. https://doi.org/10.3390/ijerph18147613







