Understanding the Factors Related to Trauma-Induced Stress in Cancer Patients: A National Study of 17 Cancer Centers
Abstract
:1. Introduction
2. Methods
2.1. Data and Sample
2.2. Measures
2.2.1. Distress Thermometer (DT)
2.2.2. Posttraumatic Stress Symptoms (PTSS)
2.2.3. Physical Symptoms
2.2.4. Age and Sex
2.2.5. Social Support
2.3. Data Analysis
3. Results
4. Discussion
- Both older age and increased levels of social support were shown to decrease intrusive cognitive symptoms of PTSS. This suggests that those individuals who were older and those with higher social support had less intrusive cognitive symptoms.
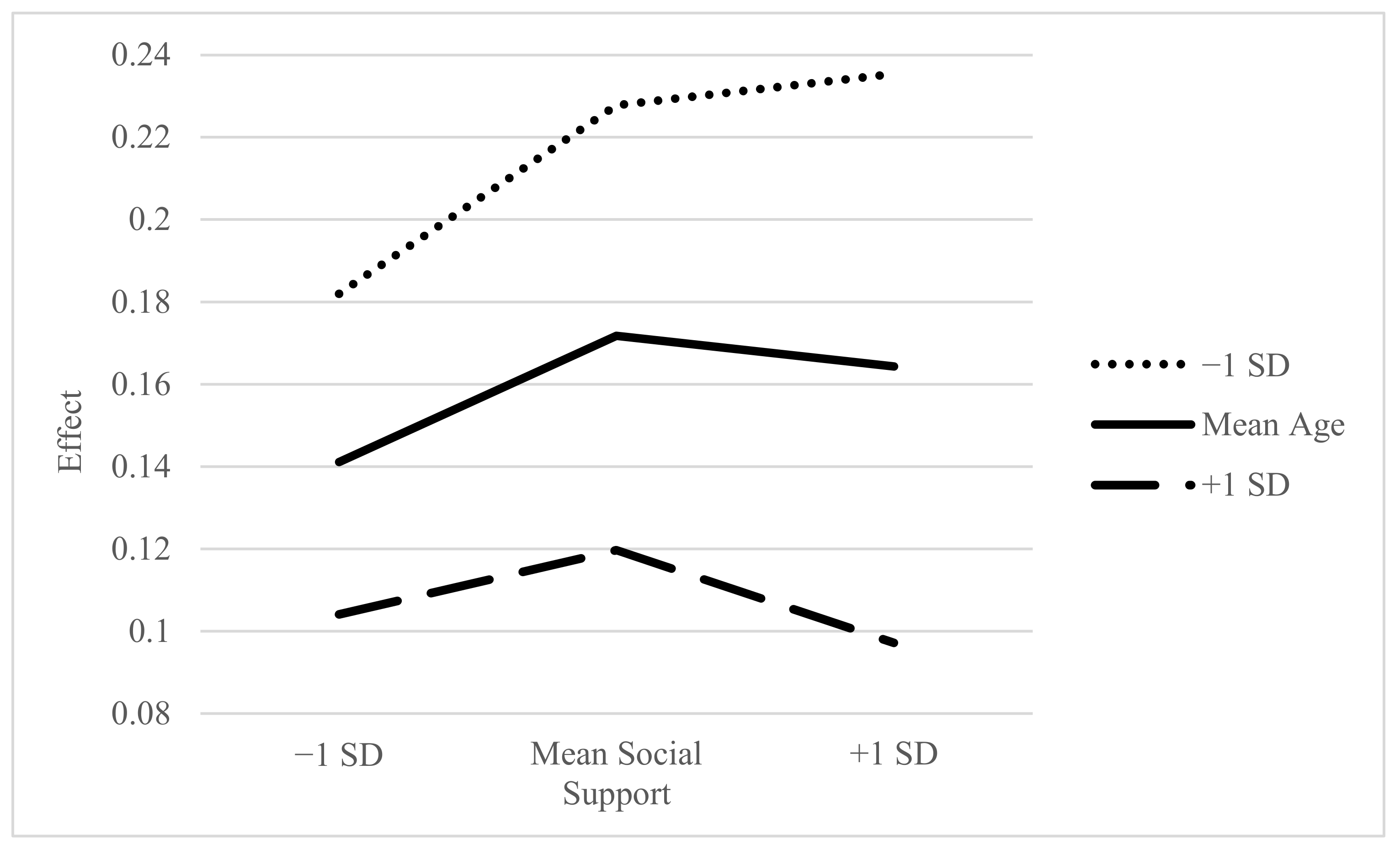
- The combined moderation effect of age and social support on the relationship between distress and intrusive cognitive symptoms of PTSS achieved an increase in intrusive cognitive symptoms of PTSS for older adults with higher levels of social support. This suggests the combination of older age and higher social support increased the intrusive cognitive symptoms.
- Social support also functioned as a moderating influence on the distress to symptom score path. Evidence indicated that social support may have served to attenuate the relationship between distress and PTSS symptoms.
- The hypothesized moderation of age was not supported. While previous literature has indicated that age may influence PTSS, it was not shown to have an independent effect in this study. This moderation was reflective of higher intrusive cognitive symptoms of PTSS in younger patients with moderate to high levels of social support. When combined with physical symptom mediation, younger age and higher levels of social support had an increasing effect on this mediating relationship.
- There was a direct relationship between distress and intrusive cognitive symptoms of PTSS, but the study also found that physical symptoms mediated the relationship. This suggests that while distress and PTSS may be related, the mechanism by which this relationship functions may be more complicated than it appears. Specifically, the pathway by which distress is related to intrusive cognitive symptoms of PTSS can occur by way of the physical symptoms associated with cancer treatment. The observed mediating effect of physical symptoms was conditional upon levels of age and social support. This suggests variability in the relationship between physical symptoms and PTSS, based upon an individual’s age and level of social support.
4.1. Study Limitations
4.2. Research Implications
4.3. Clinical Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leano, A.; Korman, M.B.; Goldberg, L.; Ellis, J. Are we missing PTSD in our patients with cancer? Part I. Can. Oncol. Nurs. J. 2019, 29, 141–146. [Google Scholar]
- Shand, L.K.; Cowlishaw, S.; Brooker, J.E.; Burney, S.; Ricciardelli, L. Correlates of post-traumatic stress symptoms and growth in cancer patients: A systematic review and meta-analysis. Psycho Oncol. 2015, 24, 624–634. [Google Scholar] [CrossRef] [PubMed]
- Abbey, G.; Thompson, S.B.; Hickish, T.; Heathcote, D. A meta-analysis of prevalence rates and moderating factors for cancer-related post-traumatic stress disorder. Psycho Oncol. 2015, 24, 371–381. [Google Scholar] [CrossRef]
- Sahar, J.; Fadhillah, H.; Pratiwi, A. Post-Traumatic Stress Syndrome (PTSS) in Nurses Post-Earthquake Disaster in Indonesia. Int. J. Indones. Natl. Nurses Assoc. (IJINNA) 2018, 1, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Fadhillah, H.; Pratiwi, A.; Setiana, R. Disaster nursing model: An approach to reduce post-traumatic stress syndrome prevalence in nurses. Syst. Rev. Pharmacy 2020, 11, 265–269. [Google Scholar]
- American Cancer Society. Cancer Facts and Figures. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-treatment-and-survivorship-facts-and-figures/cancer-treatment-and-survivorship-facts-and-figures-2019-2021.pdf (accessed on 2 May 2021).
- Fradgley, E.A.; Bultz, B.D.; Kelly, B.J.; Loscalzo, M.J.; Grassi, L.; Sitaram, B. Progress toward integrating Distress as the Sixth Vital Sign: A global snapshot of triumphs and tribulations in precision supportive care. J. Psychosoc. Oncol. Res. Pract. 2019, 1, e2. [Google Scholar] [CrossRef]
- Fitch, M.I.; Ashbury, F.; Nicoll, I. Reflections on the implementation of screening for distress (sixth vital sign) in Canada: Key lessons learned. Support. Care Cancer 2018, 26, 4011–4020. [Google Scholar] [CrossRef]
- Carlson, L.E.; Zelinski, E.L.; Toivonen, K.I.; Sundstrom, L.; Jobin, C.T.; Damaskos, P.; Zebrack, B. Prevalence of psychosocial distress in cancer patients across 55 North American cancer centers. J. Psychosoc. Oncol. 2019, 37, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Swartzman, S.; Booth, J.N.; Munro, A.; Sani, F. Posttraumatic stress disorder after cancer diagnosis in adults: A meta-analysis. Depress. Anxiety 2017, 34, 327–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pujol, J.-L.; Plassot, C.; Mérel, J.-P.; Arnaud, E.; Launay, M.; Daurès, J.-P.; Boulze, I. Post-Traumatic Stress Disorder and Health-Related Quality of Life in Patients and Their Significant Others Facing Lung Cancer Diagnosis: Intrusive Thoughts as Key Factors. Psychology 2013, 04, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Kangas, M.; Henry, J.L.; Bryant, R.A. Posttraumatic stress disorder following cancer: A conceptual and empirical review. Clin. Psychol. Rev. 2002, 22, 499–524. [Google Scholar] [CrossRef]
- Cordova, M.J.; Riba, M.B.; Spiegel, D. Post-traumatic stress disorder and cancer. Lancet Psychiatry 2017, 4, 330–338. [Google Scholar] [CrossRef] [Green Version]
- Curran, L.; Sharpe, L.; Butow, P. Anxiety in the context of cancer: A systematic review and development of an integrated model. Clin. Psychol. Rev. 2017, 56, 40–54. [Google Scholar] [CrossRef] [PubMed]
- Seiler, A.; Jenewein, J. Resilience in Cancer Patients. Front. Psychiatry 2019, 10, 208. [Google Scholar] [CrossRef] [Green Version]
- Faller, H.; Schuler, M.; Richard, M.; Heckl, U.; Weis, J.; Küffner, R. Effects of Psycho-Oncologic Interventions on Emotional Distress and Quality of Life in Adult Patients With Cancer: Systematic Review and Meta-Analysis. J. Clin. Oncol. 2013, 31, 782–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tung, H.-Y.; Lin, Y.-H.; Kao, C.-C.; Wu, S.-F. The Relationships Among Symptom Distress, Posttraumatic Stress Symptoms, and Depression in Patients With Female-specific Cancers. Cancer Nurs. 2018, 41, 181–188. [Google Scholar] [CrossRef]
- Lin, Y.; Kao, C.; Pan, I.; Liu, Y. Lower urinary symptoms, resilience, and post-traumatic stress symptoms among rectal cancer patients after surgery. Jpn. J. Nurs. Sci. 2020, 17, e12320. [Google Scholar] [CrossRef] [PubMed]
- Carlson, L.E.; Waller, A.; Groff, S.L.; Bultz, B.D. Screening for distress, the sixth vital sign, in lung cancer patients: Effects on pain, fatigue, and common problems-secondary outcomes of a randomized controlled trial. Psycho Oncol. 2013, 22, 1880–1888. [Google Scholar] [CrossRef]
- Sultan, S.M.; LeClair, T.L.; Rondeau, E.; Burns, W.; Abate, C. A systematic review on factors and consequences of parental distress as related to childhood cancer. Eur. J. Cancer Care 2016, 25, 616–637. [Google Scholar] [CrossRef] [Green Version]
- Tackett, A.P.; Cushing, C.C.; Suorsa, K.I.; Mullins, A.J.; Gamwell, K.L.; Mayes, S.; McNall-Knapp, R.; Chaney, J.M.; Mullins, L.L. Illness Uncertainty, Global Psychological Distress, and Posttraumatic Stress in Pediatric Cancer: A Preliminary Examination Using a Path Analysis Approach. J. Pediatr. Psychol. 2016, 41, 309–318. [Google Scholar] [CrossRef] [Green Version]
- Andreu, Y.; Galdón-Garrido, M.J.; Durà, E.; Martinez, P.; Perez, S.; Murgui, S. A longitudinal study of psychosocial distress in breast cancer: Prevalence and risk factors. Psychol. Health 2012, 27, 72–87. [Google Scholar] [CrossRef]
- Swartzman, S.; Sani, F.; Munro, A.J. The role of social support, family identification, and family constraints in predicting posttraumatic stress after cancer. Psycho Oncol. 2017, 26, 1330–1335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tridiuum Inc. Polaris Oncology Distress Management System Data. 2017; unpublished raw data. [Google Scholar]
- Akizuki, N.; Yamawaki, S.; Akechi, T.; Nakano, T.; Uchitomi, Y. Development of an Impact Thermometer for use in combination with the Distress Thermometer as a brief screening tool for adjustment disorders and/or major depression in cancer patients. J. Pain Symptom Manag. 2005, 29, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Vodermaier, A.; Linden, W.; Siu, C. Screening for Emotional Distress in Cancer Patients: A Systematic Review of Assessment Instruments. J. Natl. Cancer Inst. 2009, 101, 1464–1488. [Google Scholar] [CrossRef] [PubMed]
- Matsuoka, Y.; Nakano, T.; Inagaki, M.; Sugawara, Y.; Akechi, T.; Imoto, S.; Murakami, K.; Yamawaki, S.; Uchitomi, Y. Cancer-related intrusive thoughts as an indicator of poor psychological adjustment at 3 or more years after breast surgery: A preliminary study. Breast Cancer Res. Treat. 2002, 76, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Mehnert, A.; Berg, P.; Henrich, G.; Herschbach, P. Fear of cancer progression and cancer-related intrusive cognitions in breast cancer survivors. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2009, 18, 1273–1280. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.; Yeung, N.; Man, J.; Gallagher, M.W.; Chu, Q.; Deen, S.H. Ambivalence over emotional expression, intrusive thoughts, and posttraumatic stress symptoms among Chinese American breast cancer survivors. Support. Care Cancer 2017, 25, 3281–3287. [Google Scholar] [CrossRef]
- US Department of Veterans Affairs. PTSD: National Center for PTSD. Available online: https://www.ptsd.va.gov/professional/assessment/list_measures.asp (accessed on 3 May 2021).
- Norris, F.H.; Hamblen, J.L. Standardized self-report measures of civilian trauma and posttraumatic stress disorder. In Assessing Psychological Trauma and PTSD; Wilson, J.P., Keane, T.M., Martin, T., Eds.; Guilford Press: New York, NY, USA, 2004; pp. 63–102. [Google Scholar]
- Haber, M.G.; Cohen, J.L.; Lucas, T.; Baltes, B. The relationship between self-reported received and perceived social support: A meta-analytic review. Am. J. Commun. Psychol. 2007, 39, 133–144. [Google Scholar] [CrossRef]
- Fritz, M.S.; MacKinnon, D.P. Required Sample Size to Detect the Mediated Effect. Psychol. Sci. 2007, 18, 233–239. [Google Scholar] [CrossRef] [Green Version]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A regression-Based Approach; Guilford Press: New York, NY, USA, 2013; p. 507. [Google Scholar]
- Graves, K.D.; Arnold, S.M.; Love, C.L.; Kirsh, K.L.; Moore, P.G.; Passik, S.D. Distress screening in a multidisciplinary lung cancer clinic: Prevalence and predictors of clinically significant distress. Lung Cancer 2007, 55, 215–224. [Google Scholar] [CrossRef] [Green Version]
- Hegel, M.T.; Moore, C.P.; Collins, E.D.; Kearing, S.; Gillock, K.L.; Riggs, R.L.; Clay, K.F.; Ahles, T.A. Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer. Cancer 2006, 107, 2924–2931. [Google Scholar] [CrossRef]
- Hollingworth, W.; Metcalfe, C.; Mancero, S.; Harris, S.; Campbell, R.; Biddle, L.; McKell-Redwood, D.; Brennan, J. Are Needs Assessments Cost Effective in Reducing Distress Among Patients With Cancer? A Randomized Controlled Trial Using the Distress Thermometer and Problem List. J. Clin. Oncol. 2013, 31, 3631–3638. [Google Scholar] [CrossRef]
- Clark, P.G.; Rochon, E.; Brethwaite, D.; Edmiston, K.K. Screening for psychological and physical distress in a cancer inpatient treatment setting: A pilot study. Psycho Oncol. 2011, 20, 664-648. [Google Scholar] [CrossRef]
- Thekdi, S.M.; Milbury, K.; Spelman, A.; Wei, Q.; Wood, C.; Matin, S.F.; Tannir, N.; Jonasch, E.; Pisters, L.; Cohen, L. Posttraumatic stress and depressive symptoms in renal cell carcinoma: Association with quality of life and utility of single-item distress screening. Psycho-Oncology 2015, 24, 1477–1484. [Google Scholar] [CrossRef]
- E Carlson, L.; Angen, M.; Cullum, J.; Goodey, E.; Koopmans, J.; Lamont, L.; Macrae, J.H.; Martin, M.; Pelletier, G.; Robinson, J.; et al. High levels of untreated distress and fatigue in cancer patients. Br. J. Cancer 2004, 90, 2297–2304. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Kim, S.; Zhang, H. Changes in Depressive Symptoms among Older Adults with Multiple Chronic Conditions: Role of Positive and Negative Social Support. Int. J. Environ. Res. Public Health 2017, 14, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cox, D.W.; Buhr, E.E.; Owen, J.J.; Davidson, E. Linking partner emotional support, partner negative interaction, and trauma with psychological distress: Direct and moderating effects. J. Soc. Pers. Relatsh. 2016, 33, 303–319. [Google Scholar] [CrossRef]
- Gessler, S.; Low, J.; Daniells, E.; Williams, R.; Brough, V.; Tookman, A.; Jones, L. Screening for distress in cancer patients: Is the distress thermometer a valid measure in the UK and does it measure change over time? A prospective validation study. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2008, 17, 538–547. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, A.J. Pooled Results From 38 Analyses of the Accuracy of Distress Thermometer and Other Ultra-Short Methods of Detecting Cancer-Related Mood Disorders. J. Clin. Oncol. 2007, 25, 4670–4681. [Google Scholar] [CrossRef]
- Hegel, M.T.; Collins, E.D.; Kearing, S.; Gillock, K.L.; Moore, C.P.; Ahles, T.A. Sensitivity and specificity of the Distress Thermometer for depression in newly diagnosed breast cancer patients. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2008, 17, 556–560. [Google Scholar] [CrossRef]
- Andersen, B.L.; Farrar, W.B.; Golden-Kreutz, D.; Emery, C.F.; Glaser, R.; Crespin, T.; Carson, I.W.E. Distress reduction from a psychological intervention contributes to improved health for cancer patients. Brain Behav. Immun. 2007, 21, 953–961. [Google Scholar] [CrossRef] [Green Version]
- Zabora, J.; BrintzenhofeSzoc, K.; Curbow, B.; Hooker, C.; Piantadosi, S. The prevalence of psychological distress by cancer site. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens Cancer 2001, 10, 19–28. [Google Scholar] [CrossRef]
- BrintzenhofeSzoc, K.; Davis, C.; Kayser, K.; Lee, H.Y.; Nedjat-Haiem, F.; Oktay, J.S.; Zabora, J.; Zebrack, B.J. Screening for Psychosocial Distress: A National Survey of Oncology Social Workers. J. Psychosoc. Oncol. 2015, 33, 34–47. [Google Scholar] [CrossRef] [PubMed]
- Rohan, E.A. Removing the Stress from Selecting Instruments: Arming Social Workers to Take Leadership in Routine Distress Screening Implementation. J. Psychosoc. Oncol. 2012, 30, 667–678. [Google Scholar] [CrossRef] [Green Version]
- Bultz, B.D.; Watson, L.; Loscalzo, M.; Kelly, B.; Zabora, J. From foundation to inspiration: Implementing screening for distress (6th Vital Sign) for optimal cancer care—international leadership perspectives on program development. J. Psychosoc. Oncol. Res. Pract. 2021, 3, e051. [Google Scholar] [CrossRef]


| Sex | Age | |||||
|---|---|---|---|---|---|---|
| Center (n = 17) | Setting (Non-Rural = 76%) (Rural = 24%) | n (1119) | Male (31.4%) | Female (68.6%) | M (60.58) | SD (12.84) |
| 1 | Non-rural | 210 | 31.90 | 68.10 | 61.14 | 11.62 |
| 2 | Rural | 58 | 36.20 | 63.80 | 63.57 | 13.94 |
| 3 | Non-rural | 10 | 40.00 | 60.00 | 55.00 | 13.00 |
| 4 | Non-rural | 17 | 0.00 | 100.00 | 53.18 | 12.84 |
| 5 | Non-rural | 15 | 40.00 | 60.00 | 54.27 | 13.44 |
| 6 | Non-rural | 5 | 80.00 | 20.00 | 67.60 | 10.78 |
| 7 | Non-rural | 9 | 11.10 | 88.90 | 47.00 | 20.12 |
| 8 | Non-rural | 39 | 30.80 | 69.20 | 62.13 | 14.36 |
| 9 | Non-rural | 24 | 29.20 | 70.80 | 50.58 | 12.00 |
| 10 | Non-rural | 21 | 0.00 | 100.00 | 56.71 | 15.06 |
| 11 | Rural | 236 | 33.10 | 66.90 | 59.14 | 12.47 |
| 12 | Rural | 107 | 23.40 | 76.60 | 61.29 | 12.34 |
| 13 | Non-rural | 90 | 47.80 | 52.20 | 58.79 | 11.01 |
| 14 | Non-rural | 22 | 22.70 | 77.30 | 55.95 | 14.10 |
| 15 | Non-rural | 30 | 40.00 | 60.00 | 62.23 | 12.52 |
| 16 | Rural | 35 | 22.90 | 77.10 | 62.71 | 11.55 |
| 17 | Non-rural | 191 | 30.40 | 69.60 | 64.4 | 12.74 |
| Bivariate Correlations and Descriptive Statistics (n = 1119) | ||||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | M | SD | |
| 1. Distress | - | 5.07 | 2.70 | |||||
| 2. PTSS | 0.377 *** | - | 4.32 | 1.63 | ||||
| 3. Symptoms | −0.669 *** | −0.523 *** | - | 3.71 | 0.70 | |||
| 4. Social Support | −0.350 *** | −0.077 ** | 0.299 *** | - | 17.54 | 13.39 | ||
| 5. Age | −0.091 ** | −0.125 *** | 0.153 ** | 0.017 | - | 60.58 | 12.84 | |
| 6. Sex | 0.036 | 0.008 | 0.006 | 0.006 | −0.195 *** | - | ||
| Conditional Indirect Effects of Distress on PTSS at Values of the Moderators (Mediated by Symptom Score) | |||||
|---|---|---|---|---|---|
| Social Support | Age | Effect | Boot SE | 95% Boot CI | |
| LL | UL | ||||
| 47.7334 | 0.1820 | 0.0317 | 0.1246 | 0.0855 | |
| −1 SD | 60.5773 | 0.1411 | 0.0261 | 0.0955 | 0.1178 |
| 73.4212 | 0.1041 | 0.0273 | 0.0588 | 0.1690 | |
| 47.7334 | 0.2278 | 0.0243 | 0.1812 | 0.2757 | |
| MEAN LEVELS | 60.5773 | 0.1718 | 0.0187 | 0.1357 | 0.2102 |
| 73.4212 | 0.1197 | 0.0258 | 0.0723 | 0.1748 | |
| 47.7334 | 0.2354 | 0.0352 | 0.1664 | 0.3053 | |
| +1 SD | 60.5773 | 0.1643 | 0.0286 | 0.1100 | 0.2197 |
| 73.4212 | 0.0972 | 0.0355 | 0.0326 | 0.1702 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moore, M.R.; Davis, C.; Cadet, T.; Harralson, T.; Dietzen, L. Understanding the Factors Related to Trauma-Induced Stress in Cancer Patients: A National Study of 17 Cancer Centers. Int. J. Environ. Res. Public Health 2021, 18, 7600. https://doi.org/10.3390/ijerph18147600
Moore MR, Davis C, Cadet T, Harralson T, Dietzen L. Understanding the Factors Related to Trauma-Induced Stress in Cancer Patients: A National Study of 17 Cancer Centers. International Journal of Environmental Research and Public Health. 2021; 18(14):7600. https://doi.org/10.3390/ijerph18147600
Chicago/Turabian StyleMoore, Matthew R., Cindy Davis, Tamara Cadet, Tina Harralson, and Laura Dietzen. 2021. "Understanding the Factors Related to Trauma-Induced Stress in Cancer Patients: A National Study of 17 Cancer Centers" International Journal of Environmental Research and Public Health 18, no. 14: 7600. https://doi.org/10.3390/ijerph18147600
APA StyleMoore, M. R., Davis, C., Cadet, T., Harralson, T., & Dietzen, L. (2021). Understanding the Factors Related to Trauma-Induced Stress in Cancer Patients: A National Study of 17 Cancer Centers. International Journal of Environmental Research and Public Health, 18(14), 7600. https://doi.org/10.3390/ijerph18147600






