Family Medicine Academic Workforce of Medical Schools in Taiwan: A Nationwide Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Database of Major Medical Schools in Taiwan
2.2. Definitions of Medical Specialties and Subspecialties in Taiwan
2.3. Defintion of Taiwan Geographical Distribution
2.4. Data Analysis of Family Medicine Academic Faculty in Taiwan Medical Schools
3. Results
4. Discussion
4.1. Main Findings and Possible Explanations
4.2. Study Limitations and Strengths
4.3. Future Recommendations
- Efforts should be made to establish family medicine departments in medical schools in Taiwan to implement principles and practices of family medicine within the Taiwanese healthcare system.
- Family medicine should be embedded within the medical education curriculum at an early stage, to inform medical school students about primary care and family medicine practice and to be able to implement a holistic and comprehensive approach for health problems.
- Quality mentorship leads to a successful academic career and is associated with increased career satisfaction, academic productivity, and a sense of community; thus, it should be established in academic family medicine departments in Taiwan,
- Family medicine educator fellowship should be established, as a framework for providing family medicine skills training, a family medicine course curriculum for teaching skills training, and mentorship programs for family medicine in the future.
- Government or education institutions should strive to improve gender, age, regional, and other diversity among faculty members by providing promotional opportunities for diverse faculty in academic family medicine and overall academic medicine departments.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sadowski, S.A. Family Medicine’s Role in COVID 19 Pandemic. Available online: https://deepblue.lib.umich.edu/bitstream/handle/2027.42/155572/Sandowski%20main%20file.pdf?sequence=1&isAllowed=y (accessed on 10 June 2020).
- Rivero-Canto, O.; Marty-Jiménez, I.; Morales-Rojas, M.; Salgado Fonseca, A.E.; Acosta-Alonso, N. Antecedentes históricos de la medicina familiar. Mediciego 2010, 16, 2. [Google Scholar]
- Kidd, M. The Contribution of Family Medicine to Improving Health Systems: A Guidebook from the World Organization of Family Doctors; Routledge: New York, NY, USA, 2013. [Google Scholar]
- Taylor, R.B. (Ed.) Family medicine: Now and future practice. In Family Medicine: Principles and Practice, 6th ed.; Springer: New York, NY, USA, 2006; pp. 3–9. [Google Scholar]
- Jan, C.-F.; Hwang, S.-J.; Chang, C.-J.; Huang, C.-K.; Yang, H.-Y.; Chiu, T.-Y. Family physician system in Taiwan. J. Chin. Med. Assoc. 2020, 83, 117–124. [Google Scholar] [CrossRef] [PubMed]
- de Sutter, A.; Carl, L.; Manfred, M.; Christian, M.; Athina, T.; Henk, V.W.; Adam, W.; Jelle, S. Family medicine in times of ‘COVID-19′: A generalists’ voice. Eur. J. Gen. Pract. 2020, 26, 58–60. [Google Scholar] [CrossRef] [PubMed]
- Redwood-Campwell, L.; Dyck, C.; Delleman, B.; McKee, R. What are the family medicine faculty development needs of partners in low-and middle-income countries? Educ. Prim. Care 2019, 30, 29–34. [Google Scholar] [CrossRef]
- Svab, I.; Petek, S.M. Long-term evaluation of undergraduate family medicine curriculum in Slovenia. Srp. Arh. Celok. Lek. 2008, 136, 274–279. [Google Scholar] [CrossRef]
- Eyyup, K.; Raziye, S.G.; Celal, K.; Adem, D. Knowledge, attitudes and behaviors of medical faculty students about family medicine. Ann. Med. Res. 2020, 27, 2053–2062. [Google Scholar]
- Senf, J.H.; Campos-Outcalt, D.; Kutob, R. Factors Related to the Choice of Family Medicine: A Reassessment and Literature Review. J. Am. Board Fam. Pract. 2003, 16, 502–512. [Google Scholar] [CrossRef]
- National Development Council of Taiwan. Available online: https://reurl.cc/R6R069 (accessed on 1 April 2021).
- Laws & Regulations Database of the Republic of China. Available online: https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=L0020028 (accessed on 1 April 2021).
- Laws & Regulations Database of The Republic of China Diplomate Specialization and Examination Regulations. Available online: https://reurl.cc/OXQ00r (accessed on 1 April 2021).
- Ng, C.J.; Teng, C.L.; Abdullah, A.; Wong, C.H.; Hanafi, N.S.; Phoa, S.S.Y.; Tong, W.T. The status of family medicine training programs in the Asia Pacific. Fam. Med. 2016, 48, 194–202. [Google Scholar]
- Mackay Medical College. Available online: https://www.mmc.edu.tw/EN/index.html (accessed on 1 April 2021).
- Cheng, B.R.; Chang, H.T.; Lin, M.H.; Chen, T.J.; Chou, L.F.; Hwang, S.J. Rural-urban disparities in family physician practice patterns: A nationwide survey in Taiwan. Int. J. Health Plan. Manag. 2019, 34, e464–e473. [Google Scholar] [CrossRef]
- Leu, H.-I.; Chang, W.-T.; Lin, M.-H.; Chen, T.-J.; Hwang, S.-J.; Chou, L.-F.; Jeng, M.-J. Urban-Rural Disparity in Geographical and Temporal Availability of Pediatric Clinics: A Nationwide Survey in Taiwan. Pediatr. Neonatol. 2017, 58, 344–349. [Google Scholar] [CrossRef]
- Advancing Rural Family Medicine: The Canadian Collaborative Taskforce; Soles, T.L.; Wilson, C.R.; Oandasan, I.F. Family medicine education in rural communities as a health service intervention supporting recruitment and retention of physicians. Can. J. Rural. Med. 2017, 22, 28–32. [Google Scholar]
- Hernandez, L.J.; Pieroway, A. Mentorship for early career family physicians: Is there a role for the First Five Years in Family Practice Committee and the CFPC? Can. Fam. Physician 2018, 64, 861–862. [Google Scholar]
- Riley, M.; Skye, E.; Reed, B.D. Mentorship in an academic department of family medicine. Fam. Med. 2014, 46, 792–796. [Google Scholar] [PubMed]
- Tseng, T.-C.; Chen, T.-Y.; Chu, S.-Y.; Wang, H.-C.; Chang, C.-Y. Survey of the triple-mentoring program for students at a religious medical school. BMC Med. Educ. 2021, 21, 159. [Google Scholar] [CrossRef]
- Buchanan, J.; Maagaard, R.; Sammut, M.R.; Windak, A. EURACT—A sustainable model for the development of teachers of General Practice/Family Medicine [GP/FM]. Educ. Prim. Care 2016, 27, 424. [Google Scholar] [CrossRef]
- Willard-Grace, R.; Chen, E.H.; Hessler, D.; DeVore, D.; Prado, C.; Bodenheimer, T.; Thom, D.H. Health coaching by medical assistants to improve control of diabetes, hypertension, and hyperlipidemia in low-income patients: A randomized controlled trial. Ann. Fam. Med. 2015, 13, 130–138. [Google Scholar] [CrossRef]
- Svab, I.; Allen, J.; Zebiene, E.; Petek Ster, M.; Windak, A. Training experts in family medicine teaching. Eur. J. Gen. Pract. 2016, 22, 58–63. [Google Scholar] [CrossRef]
- Rebecca, J. Retaining talent at academic medical centers. Int. J. Acad. Med. 2016, 2, 46–51. [Google Scholar]
- Martin, J.C.; Avant, R.F.; Bowman, M.A.; Bucholtz, J.R.; Dickinson, J.R.; Evans, K.L.; Green, L.A.; Henley, D.E.; Jones, W.A.; Matheny, S.C.; et al. The Future of Family Medicine: A collaborative project of the family medicine community. Ann. Fam. Med. 2004, 2, S3–S32. [Google Scholar]
- Lewis-Stevenson, S.; Hueston, W.J.; Mainous, A.G.; Bazell, P.C.; Ye, X. Female and underrepresented minority faculty in academic departments of family medicine: Are women and minorities better off in family medicine? Fam. Med. 2001, 33, 459–465. [Google Scholar] [PubMed]
- Chen, S.-Y.T.; Jalal, S.; Ahmadi, M.; Khurshid, K.; Bhulani, N.; Rehman, A.U.; Ahmad, A.; Ding, J.; Aldred, T.-L.R.; Khosa, F. Influences for Gender Disparity in Academic Family Medicine in North American Medical Schools. Cureus 2020, 12, e8368. [Google Scholar] [CrossRef]
- Research Institute of Asian Women. Available online: http://e-asianwomen.org/xml/01687/01687.pdf (accessed on 1 April 2021).
- Ahmadi, M.; Khurshid, K.; Sanelli, P.C.; Jalal, S.; Chahal, T.; Norbash, A.; Nicolaou, S.; Castillo, M.; Khosa, F. Influences for Gender Disparity in Academic Neuroradiology. Am. J. Neuroradiol. 2018, 39, 18–23. [Google Scholar] [CrossRef]
- Campbell, J.C.; Yoon, S.C.; Grimm, L.J. Authorship and Impact of Gender-Specific Research in Major Radiology Journals. J. Am. Coll. Radiol. 2018, 16, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Carr, P.L.; Gunn, C.M.; Kaplan, S.A.; Raj, A.; Freund, K.M. Inadequate progress for women in academic medicine: Findings from the National Faculty Study. J. Womens Health (Larchmt) 2015, 24, 190–199. [Google Scholar] [CrossRef]
- Wang, Y.J.; Chiang, S.C.; Chen, T.J.; Chou, L.F.; Hwang, S.J.; Liu, J.Y. Birth trends among female physicians in Taiwan: A nationwide survey from 1996 to 2013. Int. J. Environ. Res. Public Health 2017, 14, 746. [Google Scholar] [CrossRef]
- Alavi, M.; Ho, T.; Stisher, C.; Richardson, E.; Kelly, C.; McCrory, K.; Snellings, J.; Zurek, K.; Boltz, M.W. Factors that influence student choice in family medicine: A national focus group. Fam. Med. 2019, 51, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Lawrent, G. Teachers’ multiple roles and perceived loss of professionalism in Tanzanian secondary schools. Waikato J. Educ. 2019, 24, 11–19. [Google Scholar] [CrossRef]
- Mazerolle, S.M.; Barrett, J.L. Work-Life Balance in Higher Education for Women: Perspectives of Athletic Training Faculty. Athl. Train. Educ. J. 2018, 13, 248–258. [Google Scholar] [CrossRef]
- Association of American Medical Colleges. Available online: http://bit.ly/2NqhwNH (accessed on 1 April 2021).
- Silver, M.P. Physician retirement: Gender, geography, flexibility and pensions. CMAJ 2017, 189, E1507–E1508. [Google Scholar] [CrossRef]
- John, J.; Judith, B.B.; Grant, R. Choosing family medicine. What influences medical students? Can. Fam. Physician 2003, 49, 1131–1137. [Google Scholar]
- National Health Insurance Administration. Available online: https://reurl.cc/5oXrr6 (accessed on 1 April 2021).
- Beber, S.; Antao, V.; Telner, D.; Krueger, P.; Peranson, J.; Meaney, C.; Meindl, M.; Webster, F. Examining the teaching roles and experiences of non-physician health care providers in family medicine education: A qualitative study. BMC Med. Educ. 2015, 15, 15. [Google Scholar] [CrossRef] [PubMed]
- Kohrs, F.P.; Mainous, A.G., III; Fernandez, E.S.; Matheny, S.C. Family medicine faculty development fellowships and the medically underserved. Fam. Med. 2001, 33, 124–127. [Google Scholar] [PubMed]
| Medical School Characteristics | ||||
|---|---|---|---|---|
| Public | Private | |||
| n | % | n | % | |
| With family medicine department | ||||
| North | 3 | 23.1 | 1 | 7.7 |
| Central | 0 | 0 | 2 | 15.3 |
| South | 1 | 7.7 | 1 | 7.7 |
| East | 0 | 0 | 1 | 7.7 |
| Total | 4 | 30.8 | 5 | 38.4 |
| Without family medicine department | ||||
| North | 0 | 0 | 3 | 23.1 |
| Central | 0 | 0 | 0 | 0 |
| South | 0 | 0 | 1 | 7.7 |
| East | 0 | 0 | 0 | 0 |
| Total | 0 | 0 | 4 | 30.8 |
| Total Family Medicine Academic Physician in Taiwan (n = 116) | ||||
|---|---|---|---|---|
| Public (n = 63, 54.3%) | Private (n = 53, 45.7%) | |||
| n | % | n | % | |
| With a family medicine department (n = 99, 85.3%) | 63 | 100 | 36 | 67.9 |
| Without a family medicine department (n = 17, 14.7%) | 0 | 0 | 17 | 32.1 |
| North (n = 79, 68.1%) | 58 | 92 | 21 | 39.6 |
| Central (n = 14, 12.1%) | 0 | 0 | 14 | 26.4 |
| South (n = 13, 11.2%) | 5 | 8 | 8 | 15.1 |
| East (n = 10, 8.6%) | 0 | 0 | 10 | 18.9 |
| Characteristic | n | % | |
|---|---|---|---|
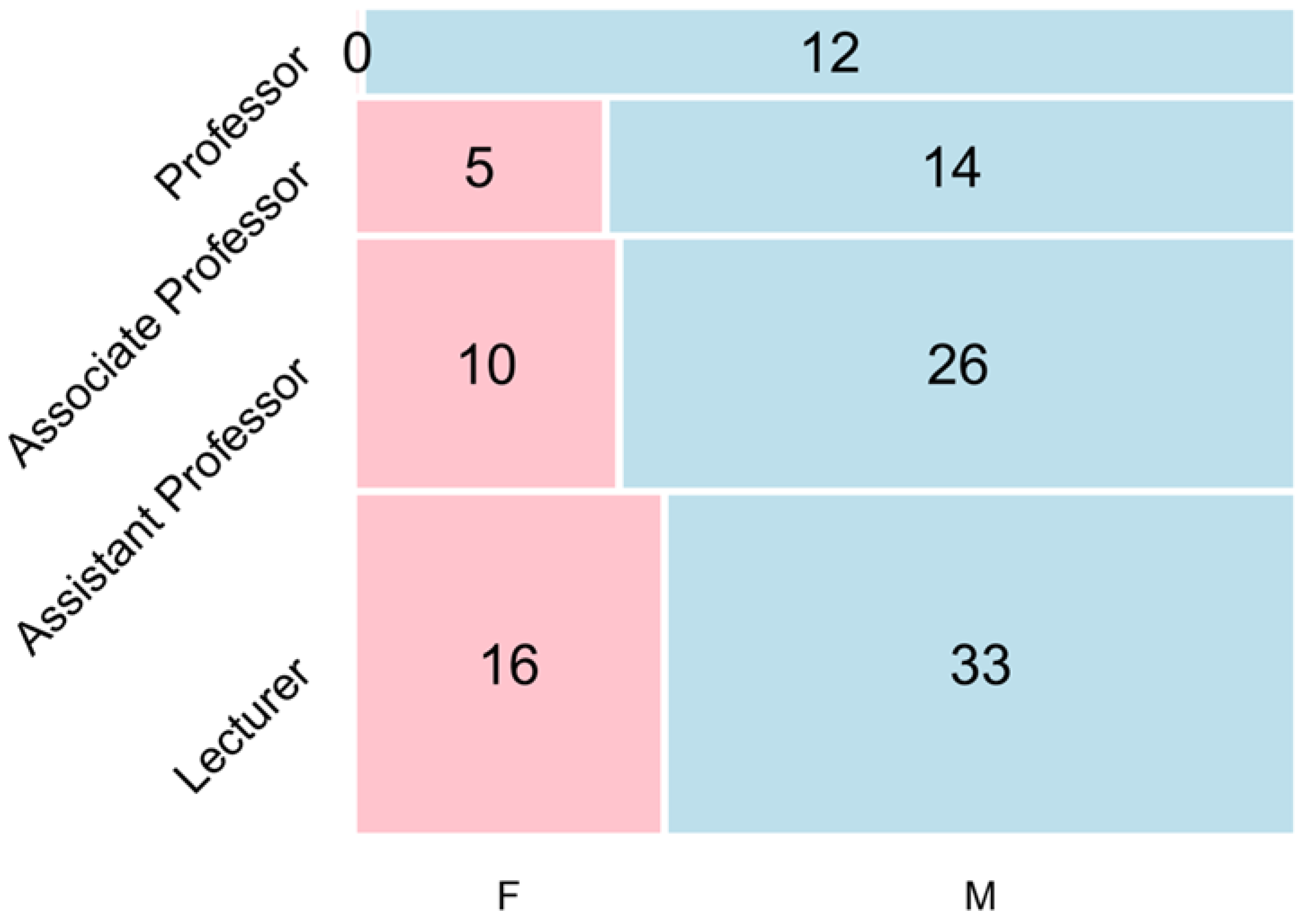
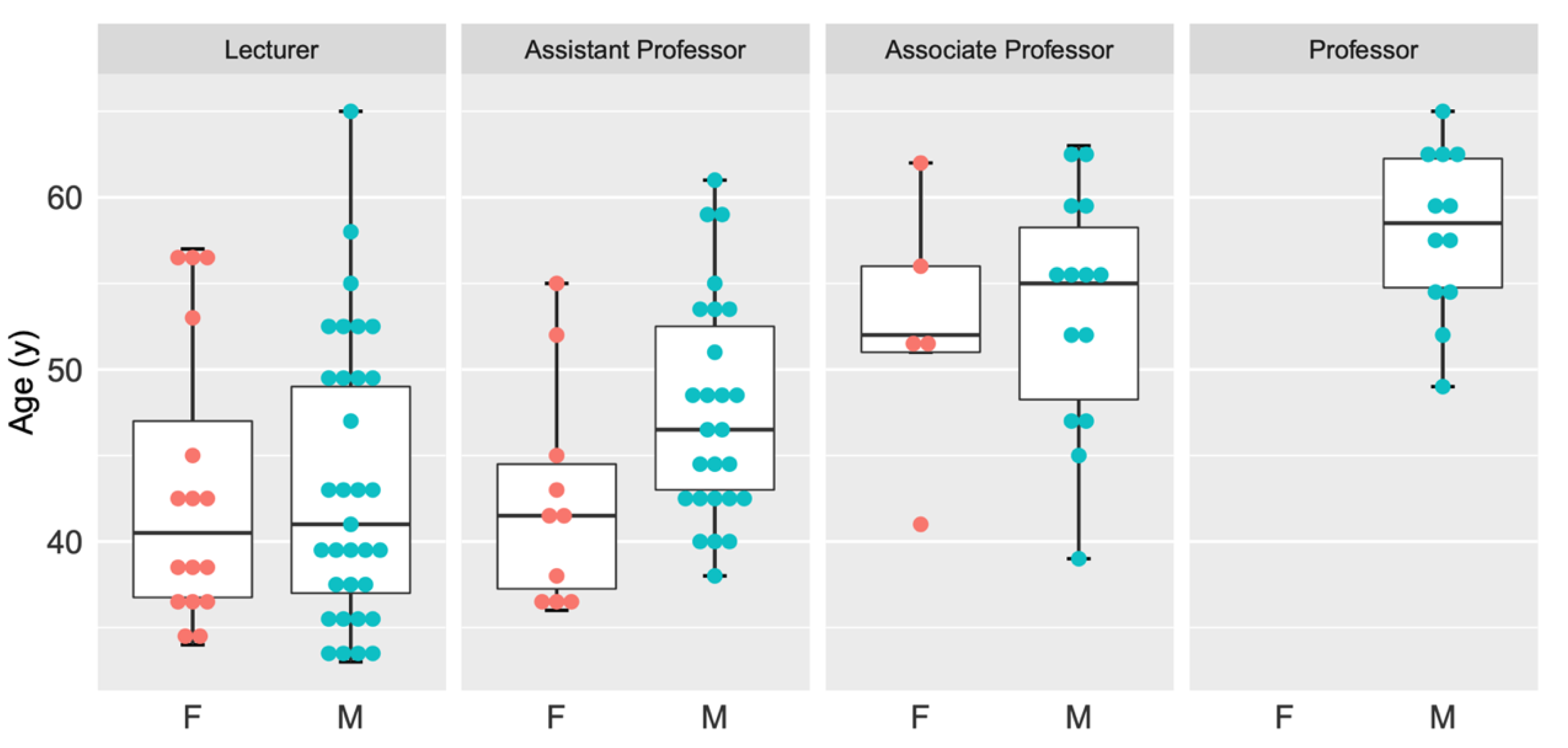
| Gender | |||
| Male | 85 | 73.3 | |
| Female | 31 | 26.7 | |
| Age (y) | |||
| 30–39 | 22 | 19.0 | |
| 40–49 | 40 | 34.5 | |
| 50–59 | 39 | 33.6 | |
| 60–69 | 15 | 12.9 | |
| Work status | |||
| Full-time | 26 | 22.4 | |
| Adjunct | 90 | 77.6 | |
| Academic position | |||
| Professor | 12 | 10.3 | |
| Associate Professor | 19 | 16.4 | |
| Assistant Professor | 36 | 31.0 | |
| Lecturer | 49 | 42.2 | |
| Faculty year | |||
| <10 years | 94 | 81.1% | |
| 10–20 years | 20 | 17.2% | |
| >20 years | 2 | 1.7% | |
| Faculty degree | |||
| PhD | 38 | 32.8 | |
| Master | 49 | 42.2 | |
| Bachelor | 29 | 0.25 | |
| Subspecialty | |||
| Gerontology and geriatrics medicine | 55 | 47.4 | |
| Hospice palliative medicine | 53 | 45.7 | |
| Environmental and occupational medicine | 13 | 11.2 | |
| Obesity medicine | 11 | 9.5 | |
| International travel medicine | 5 | 4.3 | |
| Adolescent medicine | 3 | 2.6 | |
| Osteoporosis medicine | 2 | 1.7 | |
| Rank | All Faculty | Male Faculty | Female Faculty | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Full-time faculty | ||||||
| Professor | 10 | 38. 5 | 10 | 50 | 0 | 0 |
| Associate Professor | 9 | 34.6 | 7 | 35 | 2 | 33.3 |
| Assistant Professor | 6 | 23.1 | 3 | 15 | 3 | 50 |
| Lecturer | 1 | 3.8 | 0 | 0 | 1 | 16.7 |
| Total | 26 | 100 | 20 | 100 | 6 | 100 |
| Adjunct time faculty | ||||||
| Professor | 2 | 2.2 | 2 | 3.0 | 0 | 0 |
| Associate Professor | 10 | 11.1 | 7 | 10.8 | 3 | 12 |
| Assistant Professor | 30 | 33.3 | 23 | 35.4 | 7 | 28 |
| Lecturer | 48 | 53.4 | 33 | 50.8 | 15 | 60 |
| Total | 90 | 100 | 65 | 100 | 25 | 100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.-H.; Chang, H.-T.; Lin, M.-H.; Chen, T.-J.; Hwang, S.-J.; Lin, M.-N. Family Medicine Academic Workforce of Medical Schools in Taiwan: A Nationwide Survey. Int. J. Environ. Res. Public Health 2021, 18, 7182. https://doi.org/10.3390/ijerph18137182
Chen S-H, Chang H-T, Lin M-H, Chen T-J, Hwang S-J, Lin M-N. Family Medicine Academic Workforce of Medical Schools in Taiwan: A Nationwide Survey. International Journal of Environmental Research and Public Health. 2021; 18(13):7182. https://doi.org/10.3390/ijerph18137182
Chicago/Turabian StyleChen, Shu-Han, Hsiao-Ting Chang, Ming-Hwai Lin, Tzeng-Ji Chen, Shinn-Jang Hwang, and Ming-Nan Lin. 2021. "Family Medicine Academic Workforce of Medical Schools in Taiwan: A Nationwide Survey" International Journal of Environmental Research and Public Health 18, no. 13: 7182. https://doi.org/10.3390/ijerph18137182
APA StyleChen, S.-H., Chang, H.-T., Lin, M.-H., Chen, T.-J., Hwang, S.-J., & Lin, M.-N. (2021). Family Medicine Academic Workforce of Medical Schools in Taiwan: A Nationwide Survey. International Journal of Environmental Research and Public Health, 18(13), 7182. https://doi.org/10.3390/ijerph18137182








