Gait Flexibility among Older Persons Significantly More Impaired in Fallers Than Non-Fallers—A Longitudinal Study
Abstract
1. Introduction
2. Materials and Methods
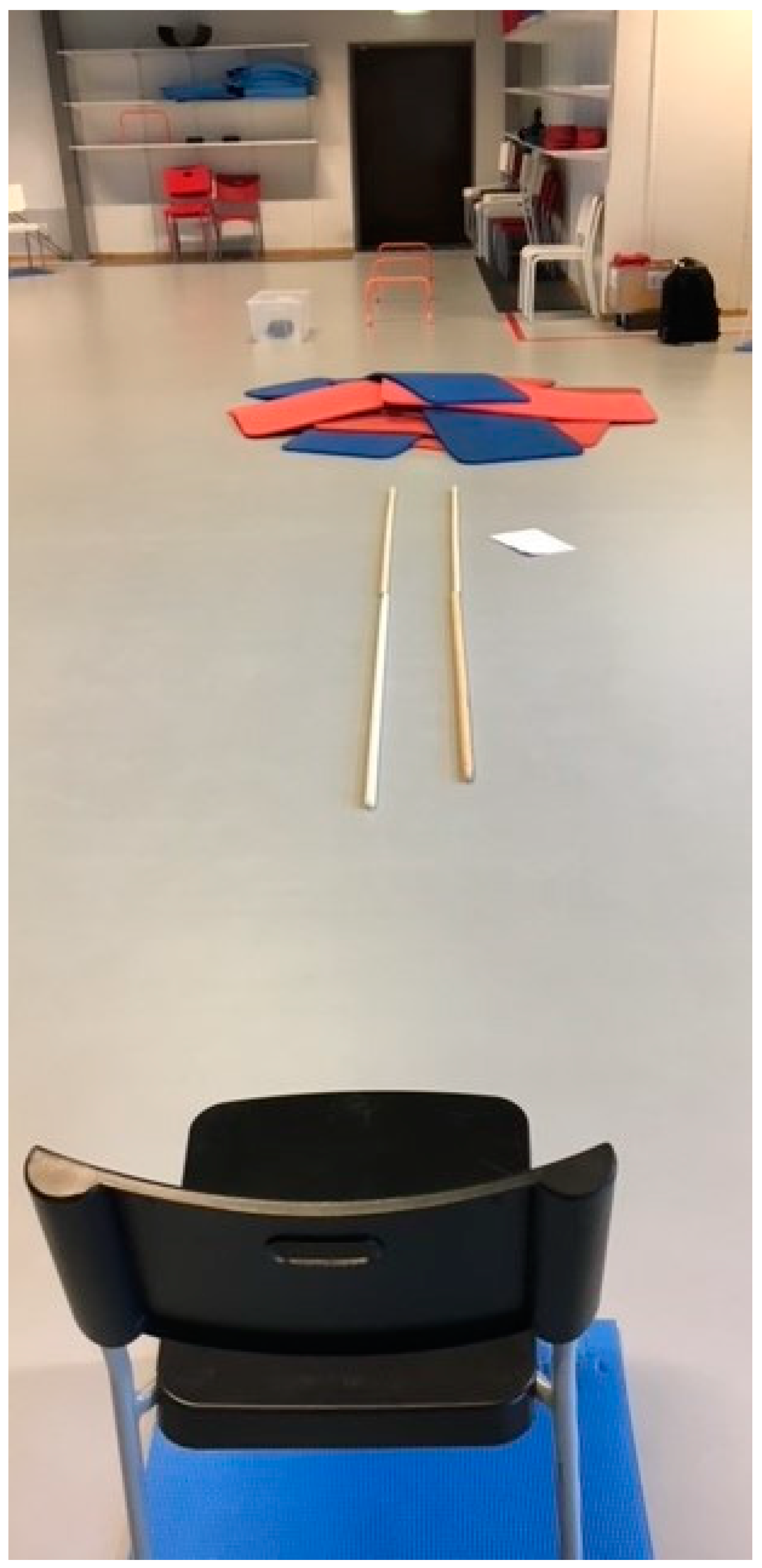
2.1. Settings
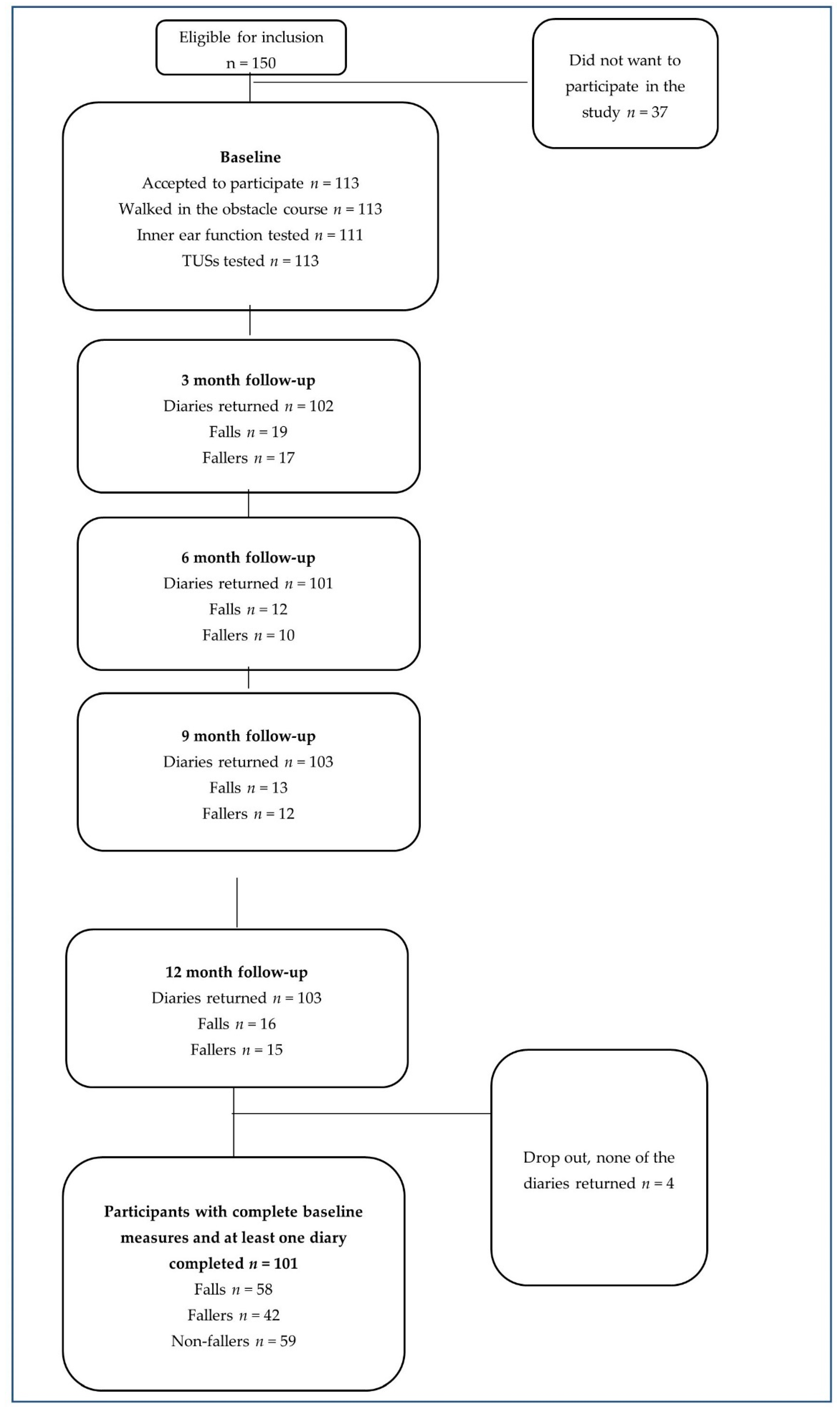
2.2. Participants
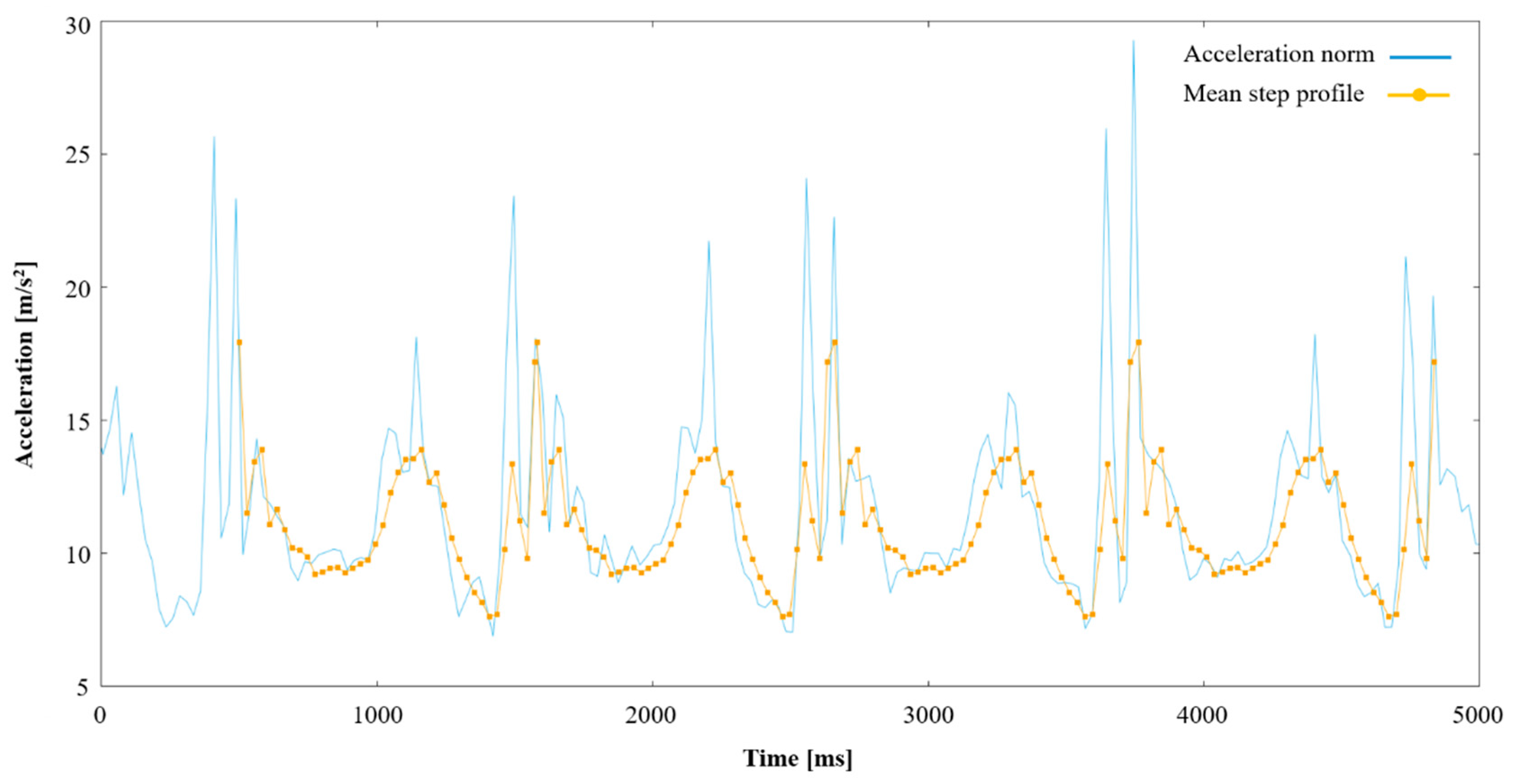
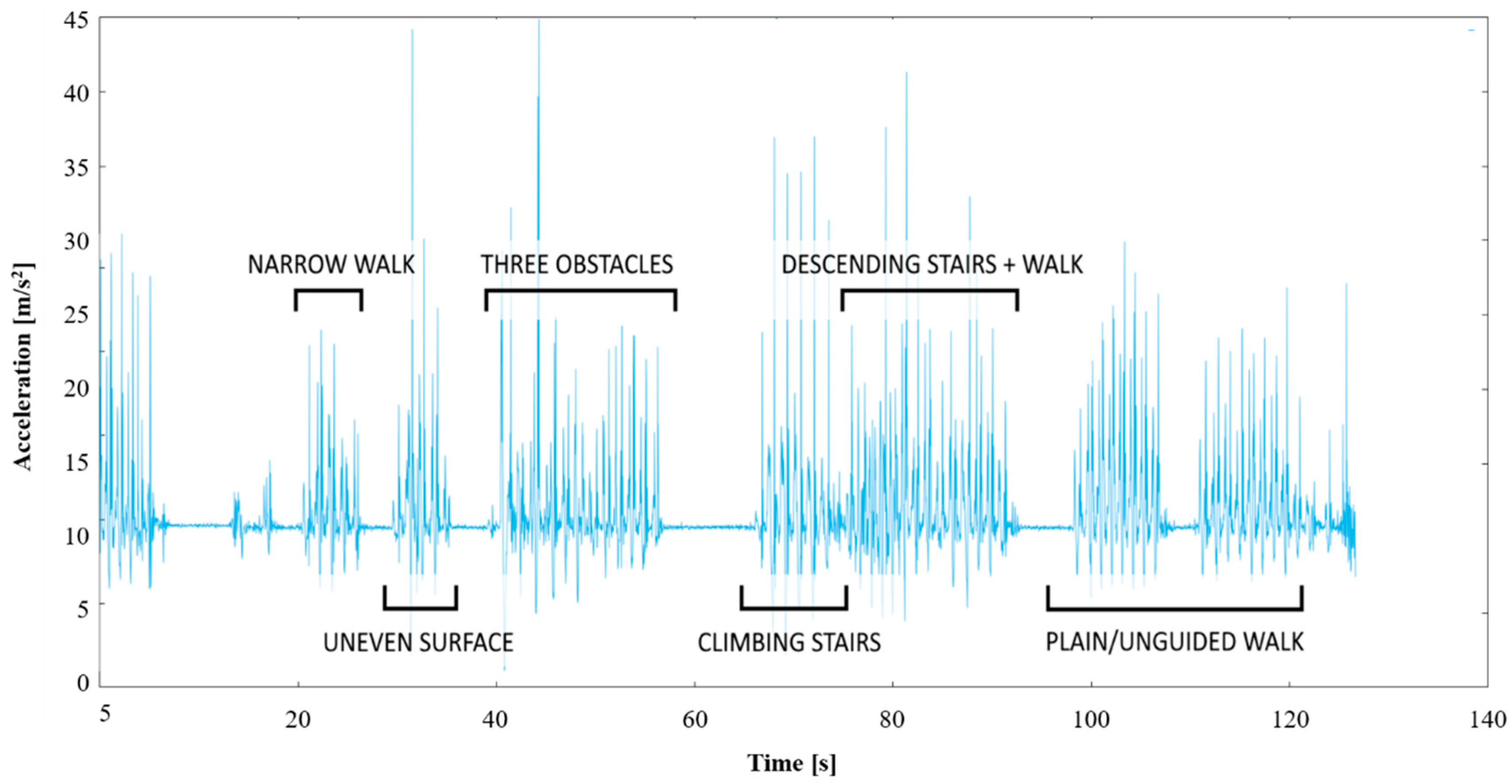
2.3. Baseline Measures
2.4. Falls
2.5. Statistics
2.6. Ethical Considerations
3. Results
3.1. Participants
3.2. Baseline Measures
3.3. 12-Month Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Report on Falls Prevention in Older Age; Ageing, & Life Course Unit, WHO: Geneva, Switzerland, 2007. [Google Scholar]
- World Health Organization. Global Health and Ageing; US National Institute of Aging, WHO: Geneva, Switzerland, 2011; p. 32.
- World Health Organization. Falls 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 28 June 2021).
- Cameron, I.D.; Dyer, S.M.; Panagoda, C.E.; Murray, G.R.; Hill, K.D.; Cumming, R.G.; Kerse, N. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst. Rev. 2018, 9, CD005465. [Google Scholar] [CrossRef] [PubMed]
- The National Board of Health and Welfare. Statistics about Causes of Death 2015. 2016. Available online: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2020-6-6798.pdf (accessed on 28 June 2021). (In Swedish).
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 9, CD007146. [Google Scholar]
- Ganz, D.A.; Bao, Y.; Shekelle, P.G.; Rubenstein, L.Z. Will my patient fall? JAMA 2007, 297, 77–86. [Google Scholar] [CrossRef]
- Pirker, W.; Katzenschlager, R. Gait disorders in adults and the elderly: A clinical guide. Wien. Klin. Wochenschr. 2017, 129, 81–95. [Google Scholar] [CrossRef]
- Kwon, M.S.; Kwon, Y.R.; Park, Y.S.; Kim, J.W. Comparison of gait patterns in elderly fallers and non-fallers. Technol. Health Care 2018, 26, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Hausdorff, J.M.; Rios, D.A.; Edelberg, H.K. Gait variability and fall risk in community-living older adults: A 1-year prospective study. Arch. Phys. Med. Rehabil. 2001, 82, 1050–1056. [Google Scholar] [CrossRef] [PubMed]
- Robinovitch, S.N.; Feldman, F.; Yang, Y.; Schonnop, R.; Leung, P.M.; Sarraf, T.; Sims-Gould, J.; Loughin, M. Video capture of the circumstances of falls in elderly people residing in long-term care: An observational study. Lancet 2013, 381, 47–54. [Google Scholar] [CrossRef]
- Muir-Hunter, S.W.; Wittwer, J.E. Dual-task testing to predict falls in community-dwelling older adults: A systematic review. Physiotherapy 2016, 102, 29–40. [Google Scholar] [CrossRef]
- Johansson, J.; Nordstrom, A.; Nordstrom, P. Greater Fall Risk in Elderly Women Than in Men Is Associated With Increased Gait Variability During Multitasking. J. Am. Med. Dir. Assoc. 2016, 17, 535–540. [Google Scholar] [CrossRef]
- Dros, J.; Maarsingh, O.R.; van der Horst, H.E.; Bindels, P.J.; Ter Riet, G.; van Weert, H.C. Tests used to evaluate dizziness in primary care. CMAJ 2010, 182, E621–E631. [Google Scholar] [CrossRef][Green Version]
- Sumner, A. The Dix-Hallpike Test. J. Physiother. 2012, 58, 131. [Google Scholar] [CrossRef]
- Edlow, J.A.; Newman-Toker, D.E.; Savitz, S.I. Diagnosis and initial management of cerebellar infarction. Lancet Neurol. 2008, 7, 951–964. [Google Scholar] [CrossRef]
- Barry, E.; Galvin, R.; Keogh, C.; Horgan, F.; Fahey, T. Is the Timed Up and Go test a useful predictor of risk of falls in community-dwelling older adults: A systematic review and meta-analysis. BMC Geriatr. 2014, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Tseng, H.Z.; Chao, W.Y. Head-shaking nystagmus: A sensitive indicator of vestibular dysfunction. Clin. Otolaryngol. Allied. Sci. 1997, 22, 549–552. [Google Scholar]
- Bhattacharyya, N.; Gubbels, S.P.; Schwartz, S.R.; Edlow, J.A.; El-Kashlan, H.; Fife, T.; Holmberg, J.M.; Mahoney, K.; Hollingsworth, D.B.; Roberts, R.; et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update). Otolaryngol. Head Neck Surg. 2017, 156 (Suppl. 3), S1–S47. [Google Scholar] [CrossRef] [PubMed]
- Hofheinz, M.; Mibs, M. The Prognostic Validity of the Timed Up and Go Test With a Dual-Task for Predicting the Risk of Falls in the Elderly. Gerontol. Geriatr. Med. 2016, 2. [Google Scholar] [CrossRef]
- Panel on Prevention of Falls in Older Persons; American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J. Am. Geriatr. Soc. 2011, 59, 148–157. [Google Scholar] [CrossRef]
- Lach, H.W.; Reed, A.T.; Arfken, C.L.; Miller, J.P.; Paige, G.D.; Birge, S.J.; Peck, W.A. Falls in the elderly: Reliability of a classification system. JAGS 1991, 39, 197–202. [Google Scholar] [CrossRef]
- Altman, D. Practical Statistics for Medical Research, 9th ed.; Chapman&Hall/CRC: New York, NY, USA, 1991; 611p. [Google Scholar]
- Ekvall Hansson, E.; Magnusson, M. Vestibular asymmetry predicts falls among elderly patients with multi-sensory dizziness. BMC Geriatr. 2013, 13, 77. [Google Scholar] [CrossRef]
- Larsson, J.; Ekvall Hansson, E.; Miller, M. Increased double support variability in elderly female fallers with vestibular asymmetry. Gait Posture 2015, 41, 820–824. [Google Scholar] [CrossRef]
- Kristinsdottir, E.K.; Jarnlo, G.-B.; Magnusson, M. Aberrations in postural control, vibration sensation and some vestibular findings in healthy 64-92-year-old subjects. Scand. J. Rehabil. Med. 1997, 29, 257–265. [Google Scholar]
- Ekvall Hansson, E.; Dahlberg, L.E.; Magnusson, M. Vestibular Rehabilitation Affects Vestibular Asymmetry among Patients with Fall-Related Wrist Fractures-A Randomized Controlled Trial. Gerontology 2015, 61, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Kristinsdottir, E.K.; Nordell, E.; Jarnlo, G.B.; Tjader, A.; Thorngren, K.G.; Magnusson, M. Observation of vestibular asymmetry in a majority of patients over 50 years with fall-related wrist fractures. Acta Otolaryngol. 2001, 121, 481–485. [Google Scholar] [CrossRef]
- Kang, L.; Han, P.; Wang, J.; Ma, Y.; Jia, L.; Fu, L.; Yu, H.; Chen, X.; Niu, K.; Guo, Q. Timed Up and Go Test can predict recurrent falls: A longitudinal study of the community-dwelling elderly in China. Clin. Interv. Aging 2017, 12, 2009–2016. [Google Scholar] [CrossRef] [PubMed]
- Schoene, D.; Wu, S.M.S.; Mikolaizak, A.S.; Menant, J.C.; Smith, S.T.; Delbaere, K.; Lord, S.R. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: Systematic review and meta-analysis. J. Am. Geriatr. Soc. 2013, 61, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Ekvall Hansson, E.; Månsson, N.-O.; Håkansson, A.; Ringsberg, K.A. Falls among dizzy patients in primary health care-An intervention study with control group. Int. J. Rehabil. Res. 2008, 31, 51–57. [Google Scholar] [CrossRef]
- Olsson Möller, U.; Kristensson, J.; Midlöv, P.; Ekdahl, C.; Jakobsson, U. Predictive Validity and Cut-Off Scores in Four Diagnostic Tests for Falls–A Study in Frail Older People at Home. Phys. Occup. Ther. Geriatr. 2012, 30, 189–201. [Google Scholar] [CrossRef]

| Evaluated Characteristics | n = 101 | Fallers n = 42 | Non-Fallers n = 59 | p-Value |
|---|---|---|---|---|
| Age in years (mean (SD)) | 75.0 (5.6) | 75.7 (6.2) | 74.6 (5.2) | 0.328 |
| Health status (healthy/reported illnesses) | 41/60 | 18/24 | 23/36 | 0.696 |
| Gender number: Male/Female | 10/91 | 5/37 | 5/54 | 0.404 |
| Vestibular function (healthy/pathological) | 16/85 | 6/36 | 10/49 | 0.788 |
| Headshake test | 24/77 | 11/31 | 13/46 | 0.629 |
| Dix–Hallpike test | 19/82 | 33/9 | 49/10 | 0.570 |
| Head impulse test a | 60/39 | 26/15 | 34/24 | 0.631 |
| Total number of falls | 58 | 58 | 0 | na |
| Gait parameters obstacle course (mean (SD)) | ||||
| Average stride time P1 b [ms] | 1318.5 (100.8) | 1319.0 (97.6) | 1318.1 (103.9) | 0.754 |
| Variation in average stride time P1 [ms] | 297.9 (72.9) | 282.1 (75.6) | 309.1 (69.4) | 0.081 |
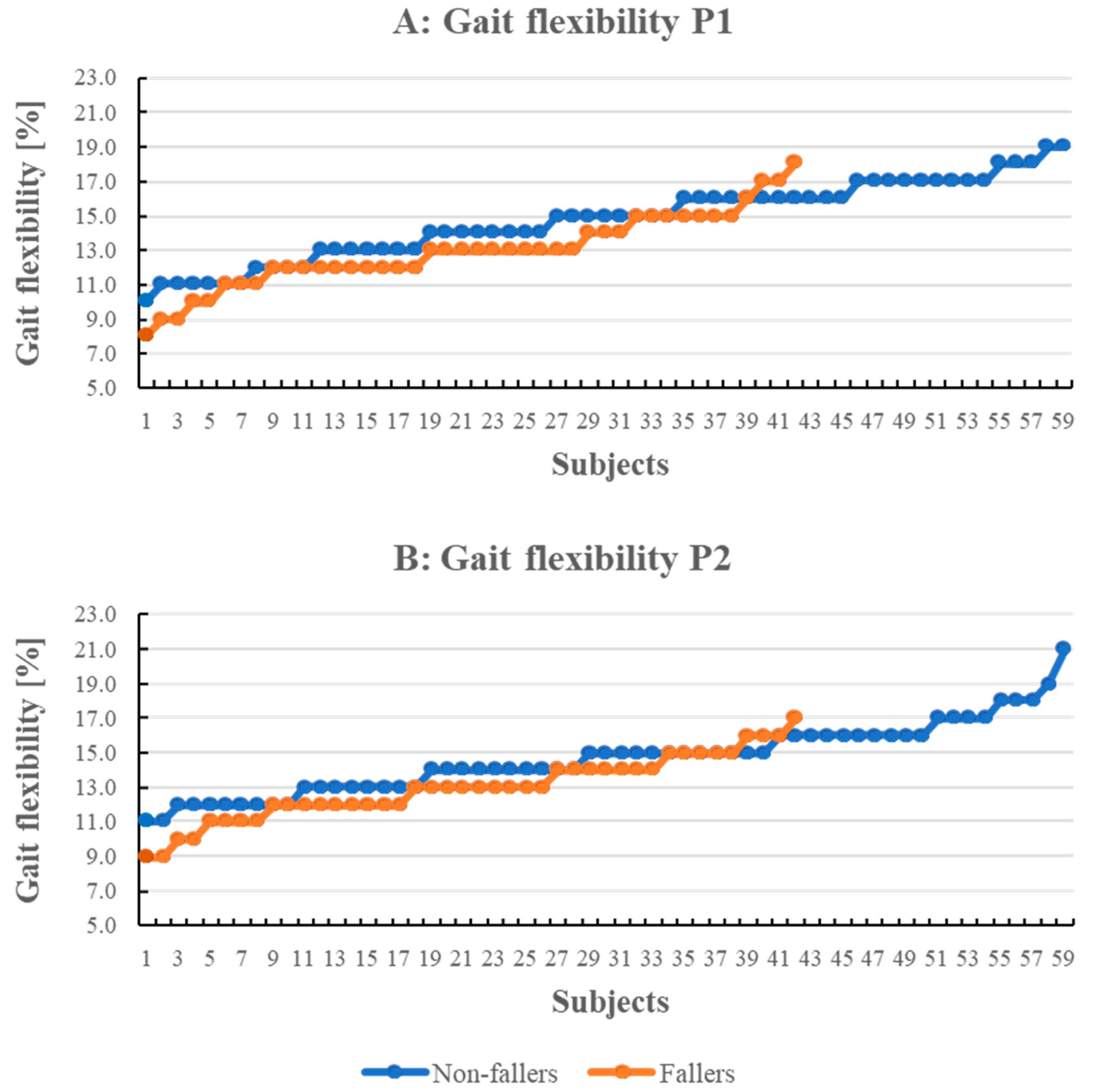
| Gait flexibility P1 [%] | 14.0 (2.4) | 13.0 (2.2) | 14.7 (2.3) | <0.001 |
| Average stride time P2 c [ms] | 1294.9 (88.1) | 1296.2 (86.8) | 1294.0 (89.8) | 0.918 |
| Variation in average stride time P2 [ms] | 301.1 (66.5) | 289.44 (65.8) | 309.3 (66.3) | 0.081 |
| Gait flexibility P2 [%] | 14.0 (2.1) | 13.0 (1.9) | 14.6 (2.0) | <0.001 |
| Gait parameters walking on an even surface (mean (SD)) | ||||
| Average stride time [ms] | 1151.1 (80.5) | 1168.2 (80.0) | 1139.0 (79.2)) | 0.104 |
| Variation in average stride time [ms] | 187.9 (90.0) | 190.6 (94.0) | 185.9 (87.9) | 0.793 |
| Gait flexibility [%] | 9.5 (2.5) | 9.0 (2.3) | 9.9 (2.5) | 0.058 |
| TUG tests (mean (SD)) | ||||
| TUG [s] | 8.4 (1.4) | 8.7 (1.5) | 8.3 (1.2) | 0.308 |
| TUGman d [s] | 9.4 (2.1) | 9.7 (2.2) | 9.2 (2.0) | 0.144 |
| TUGcogn e [s] | 10.2 (1.8) | 10.6 (2.1) | 10.0 (1.7) | 0.157 |
| diffTUGman f [s] | 1.0 (1.4) | 1.1 (1.3) | 0.9 (1.4) | 0.361 |
| diffTUGcogn g [s] | 1.8 (1.1) | 1.9 (1.3) | 1.7 (1.0) | 0.469 |
| Extrinsic Falls n = 46 | Intrinsic Falls n = 10 | Non-Classifiable Falls n = 2 | |
|---|---|---|---|
| May–July | 13 | 3 | 1 |
| August–October | 9 | 2 | 1 |
| November–January | 12 | 1 | 0 |
| February–April | 12 | 4 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ekvall Hansson, E.; Valkonen, E.; Olsson Möller, U.; Chen Lin, Y.; Magnusson, M.; Fransson, P.-A. Gait Flexibility among Older Persons Significantly More Impaired in Fallers Than Non-Fallers—A Longitudinal Study. Int. J. Environ. Res. Public Health 2021, 18, 7074. https://doi.org/10.3390/ijerph18137074
Ekvall Hansson E, Valkonen E, Olsson Möller U, Chen Lin Y, Magnusson M, Fransson P-A. Gait Flexibility among Older Persons Significantly More Impaired in Fallers Than Non-Fallers—A Longitudinal Study. International Journal of Environmental Research and Public Health. 2021; 18(13):7074. https://doi.org/10.3390/ijerph18137074
Chicago/Turabian StyleEkvall Hansson, Eva, Elina Valkonen, Ulrika Olsson Möller, Yi Chen Lin, Måns Magnusson, and Per-Anders Fransson. 2021. "Gait Flexibility among Older Persons Significantly More Impaired in Fallers Than Non-Fallers—A Longitudinal Study" International Journal of Environmental Research and Public Health 18, no. 13: 7074. https://doi.org/10.3390/ijerph18137074
APA StyleEkvall Hansson, E., Valkonen, E., Olsson Möller, U., Chen Lin, Y., Magnusson, M., & Fransson, P.-A. (2021). Gait Flexibility among Older Persons Significantly More Impaired in Fallers Than Non-Fallers—A Longitudinal Study. International Journal of Environmental Research and Public Health, 18(13), 7074. https://doi.org/10.3390/ijerph18137074







