LGB Tobacco Control: Do Health Belief Model Constructs Predict Tobacco Use Intentions Differently between LGB and Heterosexual Individuals?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Study 1 Measures
2.3.1. Perceived Health Threat of Smoking
2.3.2. Perceived Benefits of Smoking
2.3.3. Perceived Barriers to Smoking
2.3.4. Intentions to Continue Smoking
2.3.5. Covariates
2.4. Study 2 Measures
2.4.1. The Perceived Health Threat of Vaping
2.4.2. Perceived Benefits of Vaping
2.4.3. Perceived Barriers to Vaping
2.4.4. Intentions to Vape
2.4.5. Covariates
2.5. Data Analysis
3. Results
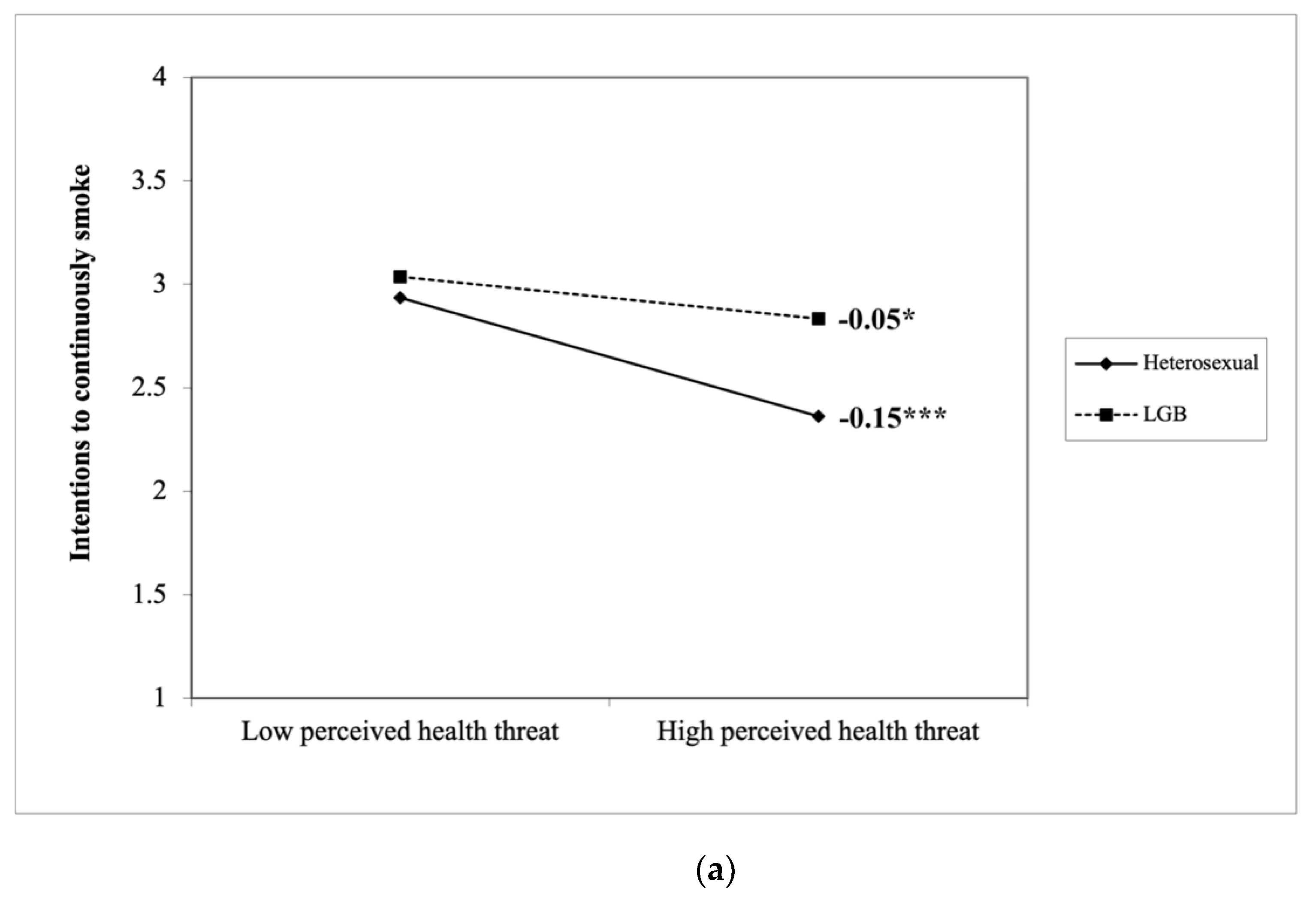
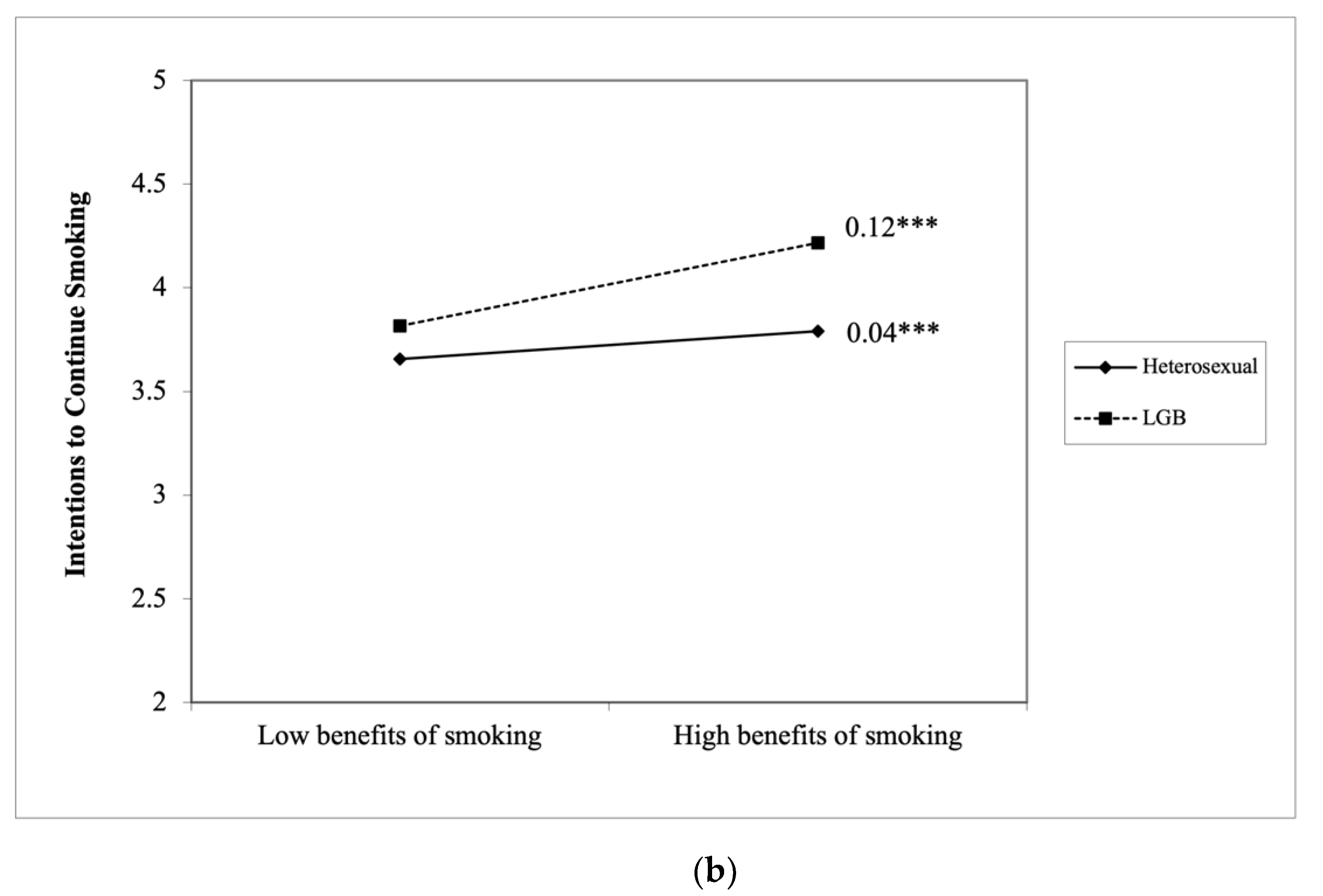
3.1. Study 1 Results
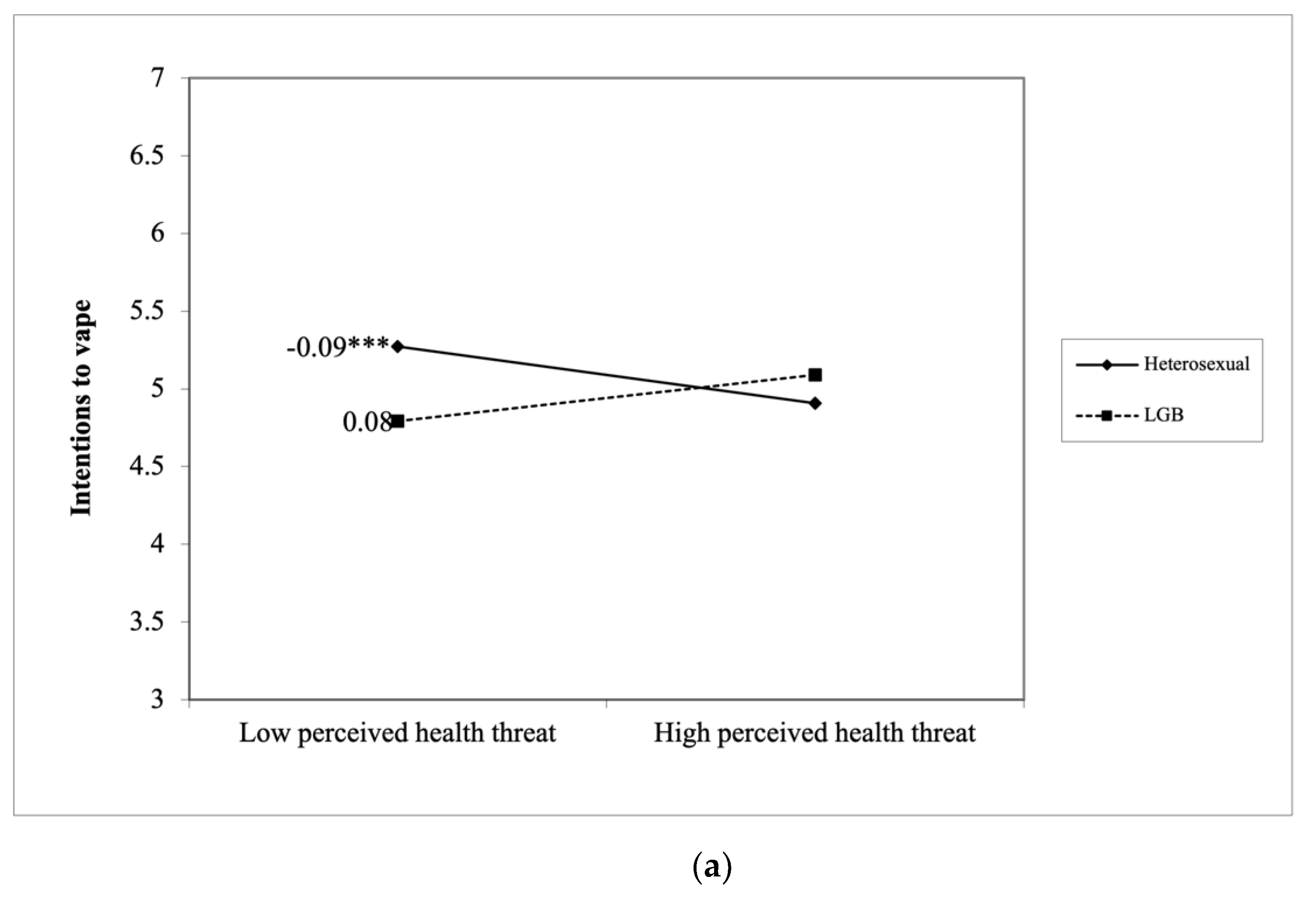
3.2. Study 2 Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jamal, A.; Phillips, E.; Gentzke, A.S.; Homa, D.M.; Babb, S.D.; King, B.A.; Neff, L.J. Current Cigarette Smoking Among Adults—United States, 2016. Morb. Mortal. Wkly. Rep. 2018, 67, 53. [Google Scholar] [CrossRef] [Green Version]
- IOM. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding; The National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Spears, C.A.; Jones, D.M.; Weaver, S.R.; Huang, J.; Yang, B.; Pechacek, T.F.; Eriksen, M.P. Sociodemographic Correlates of Electronic Nicotine Delivery Systems (ENDS) Use in the United States, 2016–2017. Am. J. Public Health 2019, 109, 1224–1232. [Google Scholar] [CrossRef]
- United States Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General; US Department of Health and Human Services, Center for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health: Atlanta, GA, USA, 2014. [Google Scholar]
- CDC. Outbreak of Lung Injury Associated with E-Cigarette Use, or Vaping. Available online: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html (accessed on 27 April 2021).
- King, B.A.; Dube, S.R.; Tynan, M.A. Current tobacco use among adults in the United States: Findings from the National Adult Tobacco Survey. Am. J. Public Health 2012, 102, e93–e100. [Google Scholar] [CrossRef]
- Caceres, B.A.; Brody, A.; Luscombe, R.E.; Primiano, J.E.; Marusca, P.; Sitts, E.M.; Chyun, D. A Systematic Review of Cardiovascular Disease in Sexual Minorities. Am. J. Public Health 2017, 107, e13–e21. [Google Scholar] [CrossRef]
- Washington, H.A. Burning Love: Big Tobacco Takes Aim at LGBT Youths. Am. J. Public Health 2002, 92, 1086–1095. [Google Scholar] [CrossRef]
- CDC. Burden of Cigarette Use in the U.S. Available online: https://www.cdc.gov/tobacco/campaign/tips/resources/data/cigarette-smoking-in-united-states.html (accessed on 27 April 2021).
- Guillory, J.; Crankshaw, E.; Farrelly, M.C.; Alam, I.; Fiacco, L.; Curry, L.; Hoffman, L.; Ganz, O.; Delahanty, J. LGBT young adults’ awareness of and receptivity to the This Free Life tobacco public education campaign. Tob. Control 2020, 30, 63–70. [Google Scholar] [CrossRef]
- Lee, J.G.; Matthews, A.K.; McCullen, C.A.; Melvin, C.L. Promotion of tobacco use cessation for lesbian, gay, bisexual, and transgender people: A systematic review. Am. J. Prev. Med. 2014, 47, 823–831. [Google Scholar] [CrossRef] [Green Version]
- Cruz, T.B.; Rose, S.W.; Lienemann, B.A.; Byron, M.J.; Meissner, H.I.; Baezconde-Garbanati, L.; Huang, L.L.; Carroll, D.M.; Soto, C.; Unger, J.B. Pro-tobacco marketing and anti-tobacco campaigns aimed at vulnerable populations: A review of the literature. Tob. Induc. Dis. 2019, 17, 68. [Google Scholar] [CrossRef]
- Glanz, K.; Rimer, B.K.; Viswanath, K. Health Behavior and Health Education: Theory, Research, and Practice, 5th ed.; Jossey-Bass: San Francisco, CA, USA, 2015. [Google Scholar]
- Janz, N.K.; Becker, M.H. The Health Belief Model: A Decade Later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef] [Green Version]
- Pribadi, E.T.; Devy, S.R. Application of the Health Belief Model on the intention to stop smoking behavior among young adult women. J. Public Health Res. 2020, 9, 1817. [Google Scholar] [CrossRef]
- Kathuria, H.; Seibert, R.G.; Cobb, V.; Herbst, N.; Weinstein, Z.M.; Gowarty, M.; Jhunjhunwala, R.; Helm, E.D.; Wiener, R.S. Perceived barriers to quitting cigarettes among hospitalized smokers with substance use disorders: A mixed methods study. Addict. Behav. 2019, 95, 41–48. [Google Scholar] [CrossRef]
- Cooper, M.; Loukas, A.; Case, K.R.; Marti, C.N.; Perry, C.L. A longitudinal study of risk perceptions and e-cigarette initiation among college students: Interactions with smoking status. Drug Alcohol. Depend. 2018, 186, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Roys, M.R.; Peltier, M.R.; Stewart, S.A.; Waters, A.F.; Waldo, K.M.; Copeland, A.L. The association between problematic alcohol use, risk perceptions, and e-cigarette use. Am. J. Drug Alcohol Abus. 2020, 46, 224–231. [Google Scholar] [CrossRef]
- Li, Y.; Samp, J.A. Navigating Remarkable Communication Experiences of Sexual Minorities; Lexington Books: Lanham, MA, USA, 2020. [Google Scholar]
- Navarro, M.A.; Hoffman, L.; Crankshaw, E.C.; Guillory, J.; Jacobs, S. LGBT Identity and Its Influence on Perceived Effectiveness of Advertisements from a LGBT Tobacco Public Education Campaign. J. Health Commun. 2019, 24, 469–481. [Google Scholar] [CrossRef]
- Burns, E.K.; Deaton, E.A.; Levinson, A.H. Rates and Reasons: Disparities in Low Intentions to Use a State Smoking Cessation Quitline. Am. J. Health Promot. 2011, 25, S59–S65. [Google Scholar] [CrossRef] [Green Version]
- Yang, B.; Owusu, D.; Popova, L. Effects of a Nicotine Fact Sheet on Perceived Risk of Nicotine and E-Cigarettes and Intentions to Seek Information About and Use E-Cigarettes. Int. J. Environ. Health Res. 2020, 17, 131. [Google Scholar] [CrossRef] [Green Version]
- Yang, B.; Popova, L. Communicating risk differences between electronic and combusted cigarettes: The role of the FDA-mandated addiction warning and a nicotine fact sheet. Tob. Control. 2020, 29, 663. [Google Scholar] [CrossRef] [PubMed]
- Owusu, D.; Massey, Z.; Popova, L. An experimental study of messages communicating potential harms of electronic cigarettes. PLoS ONE 2020, 15, e0240611. [Google Scholar] [CrossRef]
- El-Toukhy, S. Parsing Susceptibility and Severity Dimensions of Health Risk Perceptions. J. Health Commun. 2015, 20, 499–511. [Google Scholar] [CrossRef] [PubMed]
- Chaffee, B.W.; Gansky, S.A.; Halpern-Felsher, B.; Couch, E.T.; Essex, G.; Walsh, M.M. Conditional risk assessment of adolescents’ electronic cigarette perceptions. Am. J. Health Behav. 2015, 39, 421–432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Fagerström, K.O. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. Br. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, M.J.; Hughes, J.R.; Solomon, L.J.; Callas, P.W. Both smoking reduction with nicotine replacement therapy and motivational advice increase future cessation among smokers unmotivated to quit. J. Consult. Clin. Psychol. 2004, 72, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Popova, L.; Ling, P.M. Nonsmokers’ responses to new warning labels on smokeless tobacco and electronic cigarettes: An experimental study. BMC Public Health 2014, 14, 997. [Google Scholar] [CrossRef] [Green Version]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 2nd ed.; The Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Smith, E.A.; Malone, R.E. The outing of Philip Morris: Advertising tobacco to gay men. Am. J. Public Health 2003, 93, 988–993. [Google Scholar] [CrossRef] [PubMed]
- Dilley, J.A.; Spigner, C.; Boysun, M.J.; Dent, C.W.; Pizacani, B.A. Does tobacco industry marketing excessively impact lesbian, gay and bisexual communities? Tob. Control. 2008, 17, 385. [Google Scholar] [CrossRef]
- Stevens, P.; Carlson, L.M.; Hinman, J.M. An Analysis of Tobacco Industry Marketing to Lesbian, Gay, Bisexual, and Transgender (LGBT) Populations: Strategies for Mainstream Tobacco Control and Prevention. Health Promot. Pract. 2004, 5, 129S–134S. [Google Scholar] [CrossRef]
- Lee, S.J.; Sanders-Jackson, A.; Fallin-Bennett, A.; Tan, A.S.L. Comparing the effects of organic, natural, and no additives labels on tobacco packaging between Lesbian, Gay, Bisexual (LGB) and heterosexual smokers. Addict. Behav. 2019, 91, 175–179. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Study 1 (n = 1808, %) | Study 2 (n = 2801, %) |
|---|---|---|
| Age (years) | ||
| 18–29 | 23.00 | 19.35 |
| 30–44 | 33.10 | 24.21 |
| 45–59 | 23.90 | 25.35 |
| 60+ | 20.00 | 31.10 |
| Gender | ||
| Woman | 54.32 | 50.07 |
| Man | 44.97 | 48.98 |
| Transgender | 0.72 | 0.32 |
| Sexual orientation | ||
| Heterosexual | 88.99 | 90.54 |
| Lesbian or gay | 4.04 | 3.53 |
| Bisexual | 6.08 | 4.82 |
| Queer or other | 0.88 | 1.11 |
| Race/Ethnicity | ||
| White | 72.84 | 78.89 |
| People of color | 27.16 | 21.11 |
| Education | ||
| College or above | 37.44 | 34.99 |
| Some college or below | 62.56 | 65.01 |
| Current e-cigarette use | ||
| Yes | 53.76 | 76.12 |
| No | 46.24 | 23.88 |
| Current cigarette use | ||
| Yes | 100.00 | 41.31 |
| No | 0.00 | 48.69 |
| Variable | Heterosexual | LGB | Full Sample | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Median | SD | Mean | Median | SD | Mean | Median | SD | |
| Study 1 (n = 1808) | |||||||||
| Perceived health threat of smoking | 6.46 | 6.50 | 1.86 | 6.31 | 6.50 | 1.94 | 6.44 | 6.50 | 1.87 |
| Benefits of smoking | 2.81 | 2.75 | 1.66 | 3.12 | 3.00 | 1.73 | 2.85 | 2.75 | 1.67 |
| Barriers to smoking | 4.75 | 5.20 | 1.36 | 4.69 | 5.00 | 1.39 | 4.74 | 5.20 | 1.37 |
| Intentions to continue smoking | 2.43 | 2.33 | 0.82 | 2.66 | 2.67 | 0.82 | 2.45 | 2.33 | 0.81 |
| Study 2 (n = 2801) | |||||||||
| Perceived health threat of vaping | 3.87 | 3.67 | 2.10 | 4.13 | 4.00 | 2.25 | 3.90 | 3.67 | 2.12 |
| Benefits of vaping | 2.43 | 2.00 | 2.26 | 3.07 | 2.75 | 2.28 | 2.49 | 2.25 | 2.27 |
| Barriers to vaping | 4.85 | 5.00 | 1.76 | 4.51 | 4.80 | 1.97 | 4.82 | 5.00 | 1.78 |
| Intentions to vape | 3.17 | 1.00 | 2.78 | 3.58 | 2.00 | 2.93 | 3.21 | 1.00 | 2.80 |
| Variable | B | SE | p | 95% CI for B | |||
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Block 1: Controls | 0.091 *** | ||||||
| Block 2: | 0.154 *** | ||||||
| LGB | 0.28 | 0.05 | 0.11 | <0.001 | 0.17 | 0.38 | |
| Perceived health threat | −0.14 | 0.01 | −0.33 | <0.001 | −0.16 | −0.12 | |
| Benefits of smoking | 0.03 | 0.01 | 0.06 | 0.004 | 0.01 | 0.05 | |
| Barriers to smoking | −0.05 | 0.01 | −0.09 | <0.001 | −0.08 | −0.03 | |
| Block 3: | |||||||
| 3A. LGB Threat | 0.10 | 0.03 | 0.25 | <0.001 | 0.04 | 0.15 | 0.005 *** |
| 3B. LGB Benefits | 0.08 | 0.03 | 0.10 | 0.013 | 0.02 | 0.14 | 0.003 * |
| 3C. LGB Barriers | 0.03 | 0.04 | 0.06 | 0.407 | −0.04 | 0.11 | 0.000 |
| Variable | B | SE | p | 95% CI for B | |||
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Block 1: Controls | 0.396 *** | ||||||
| Block 2: | 0.107 *** | ||||||
| LGB | −0.20 | 0.13 | −0.02 | 0.114 | −0.46 | 0.05 | |
| Perceived health threat | −0.02 | 0.02 | −0.01 | 0.337 | −0.06 | 0.02 | |
| Benefits of vaping | 0.33 | 0.02 | 0.27 | <0.001 | 0.30 | 0.37 | |
| Barriers to vaping | −0.44 | 0.02 | −0.28 | <0.001 | −0.48 | −0.39 | |
| Block 3: | |||||||
| 3A. LGB Threat | 0.16 | 0.07 | 0.08 | 0.021 | 0.02 | 0.29 | 0.001 * |
| 3B. LGB Benefits | −0.06 | 0.06 | −0.02 | 0.314 | −0.17 | 0.05 | 0.000 |
| 3C. LGB Barriers | −0.18 | 0.07 | −0.10 | 0.005 | −0.31 | −0.05 | 0.001 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Yang, B.; Chen, B. LGB Tobacco Control: Do Health Belief Model Constructs Predict Tobacco Use Intentions Differently between LGB and Heterosexual Individuals? Int. J. Environ. Res. Public Health 2021, 18, 7008. https://doi.org/10.3390/ijerph18137008
Li Y, Yang B, Chen B. LGB Tobacco Control: Do Health Belief Model Constructs Predict Tobacco Use Intentions Differently between LGB and Heterosexual Individuals? International Journal of Environmental Research and Public Health. 2021; 18(13):7008. https://doi.org/10.3390/ijerph18137008
Chicago/Turabian StyleLi, Yachao, Bo Yang, and Bryan Chen. 2021. "LGB Tobacco Control: Do Health Belief Model Constructs Predict Tobacco Use Intentions Differently between LGB and Heterosexual Individuals?" International Journal of Environmental Research and Public Health 18, no. 13: 7008. https://doi.org/10.3390/ijerph18137008
APA StyleLi, Y., Yang, B., & Chen, B. (2021). LGB Tobacco Control: Do Health Belief Model Constructs Predict Tobacco Use Intentions Differently between LGB and Heterosexual Individuals? International Journal of Environmental Research and Public Health, 18(13), 7008. https://doi.org/10.3390/ijerph18137008







