The Effect of Work Safety on Organizational Social Sustainability Improvement in the Healthcare Sector: The Case of a Public Sector Hospital in Pakistan
Abstract
:1. Introduction
2. Literature Review
3. Theoretical Framework and Hypotheses
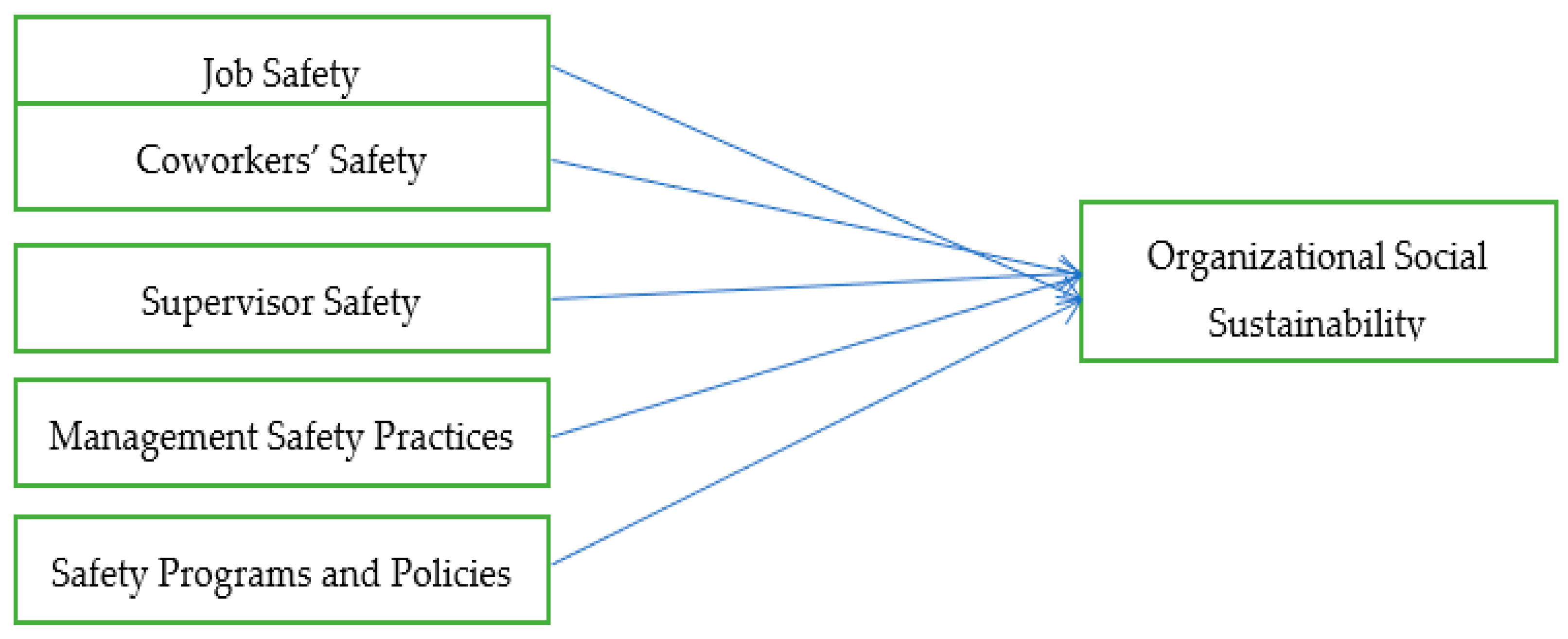
3.1. Definition of Variables
3.1.1. Organizational Social Sustainability (OSS)
3.1.2. Work Safety (WS)
- i.
- Job Safety: Job safety indicates the integration of all the measures considered necessary to free the work environment of physical, psychological, and social ills. Job safety is ensured when it is not dangerous, hazardous, unsafe, unhealthy, scary, and risky, and there is no fear and chance of death.
- ii.
- Coworker Safety: Coworker safety refers to the safety orientation of the workforce. It is the seriousness and concern of the workforce about the safety of other employees working in the same workplace. It is employees’ overall obedience to safety rules, caring about others’ safety, encouraging others to be safe, and making efforts to keep the work environment free of hazards.
- iii.
- Supervisor Safety: This is the behavior of the immediate supervisor towards safety measures. It is the extent to which a supervisor is serious and concerned regarding making the work environment safe. Safety-conscious supervisors encourage employees’ safe behavior, implement safety rules, explain safety rules and processes, reward safety behaviors, and involve employees in planning and implementing safety measures.
- iv.
- Management Safety Practices: This is about management intervention to ensure work safety and provision of a hazards-free work environment to its workers. It is assessed through the provision of safety training, safety inspections, provision of safety equipment, quick response to safety problems, rewarding safe workers, and provision of safety information.
- v.
- Safety Programs and Policies: This explains the relevance and effectiveness of safety programs and policies. To ensure safety at work, policies should be clear, useful, worthwhile, applicable, valid, and reliable.
3.2. Operationalization of Variables
3.3. Hypotheses
4. Methods
Measures
5. Results
5.1. Reliability
5.2. Validity
5.3. Correlations
5.4. Hypotheses Testing
6. Discussion
Recommendations
- (a)
- Employees are very concerned about job safety. Hospital administration must do job safety analysis and job redesign, which are presently lacking, in order to ensure job safety under changing conditions.
- (b)
- Implementation of safety programs and standards is left to ward/department supervisors alone and no involvement of hospital management was noticed as such. Participation of higher management in department-level safety affairs seems necessary to make it more effective and purposeful.
- (c)
- The careless behaviors of employees add to the safety issues in hospitals. Training of employees to make them realize the sensitivity of safety issues and their role in aggravating or mitigating the safety issues is necessary. Apart from training, employees should be held responsible for violations of safety standards.
- (d)
- Supervisors’ training on safety issues is of great importance. Enhancing supervisors’ understanding of safety issues and of different ways to manage them will make a big difference.
- (e)
- Review of safety policies and programs and evaluation of their relevance and effectiveness is of utmost importance. Purging outdated and irrelevant policies, procedures, and standards and introducing appropriate ones is the need of the hour.
- (f)
- A great improvement can be brought in social sustainability in hospitals through managing work safety issues, which will ultimately improve the quality of healthcare services provided to the patients.
7. Conclusions
7.1. General Conclusion
7.2. Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stoddard, J.E.; Pollard, C.E.; Evans, M.R. The triple bottom line: A framework for sustainable tourism development. Int. J. Hosp. Tour. Adm. 2012, 13, 233–258. [Google Scholar] [CrossRef]
- Comber, A.J.; Brunsdon, C.; Radburn, R. A spatial analysis of variations in health access: Linking geography, socio-economic status and access perceptions. Int. J. Health Geogr. 2011, 10, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Ullah, Z.; Khan, M.Z.; Khan, M.A. Towards service quality measurement mechanism of teaching hospitals. Int. J. Healthc. Manag. 2020, 1–6. [Google Scholar] [CrossRef]
- Amin, M.; Nasharuddin, S.Z. Hospital service quality and its effects on patient satisfaction and behavioural intention. Clin. Gov. Int. J. 2013. [Google Scholar] [CrossRef] [Green Version]
- Swain, S.; Kar, N.C. Hospital service quality as antecedent of patient satisfaction–a conceptual framework. Int. J. Pharm. Healthc. Mark. 2018, 18. [Google Scholar] [CrossRef]
- Kruk, M.E.; Freedman, L.P. Assessing health system performance in developing countries: A review of the literature. Health Policy 2008, 85, 263–276. [Google Scholar] [CrossRef] [PubMed]
- Ullah, Z.; Khan, M.Z.; Siddique, M. Analysis of employees’ perception of workplace support and level of motivation in public sector healthcare organization. Bus. Econ. Rev. 2017, 9, 240–257. [Google Scholar] [CrossRef]
- Ullah, Z.; Khan, M.Z. The impact of transactional and transformational leadership on job related outcomes in the nursing profession. Sarhad J. Manag. Sci. 2020, 6, 143–160. [Google Scholar]
- Evans, D.B.; Edejer, T.T.; Lauer, J.; Frenk, J.; Murray, C.J.L. Measuring quality: From the system to the provider. Int. J. Qual. Health Care 2001, 13, 439–446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ullah, Z.; Ahmad, N. Study of dynamics of quality of healthcare services: The patient perspective. J. Xi’an Univ. Archit. Technol. 2020, XII, 3103. [Google Scholar]
- Sugiono, N.; Ali, J.; Miranda, S. The effect of employee, management, working environment, and safety culture on occupational healthy and safety performance: A case study in an oil and gas company in Indonesia. Int. J. Integr. Eng. 2020, 12, 268–279. [Google Scholar]
- Morhason-Bello, I.O.; Odedina, F.; Rebbeck, T.R.; Harford, J.; Dangou, J.-M.; Denny, L.; Adewole, I.F. Challenges and opportunities in cancer control in Africa: A perspective from the African Organisation for Research and Training in Cancer. Lancet Oncol. 2013, 14, e142–e151. [Google Scholar] [CrossRef]
- Rasmussen, L.V.; Bierbaum, R.; Oldekop, J.; Agrawal, A. Bridging the practitioner-researcher divide: Indicators to track environmental, economic, and sociocultural sustainability of agricultural commodity production. Glob. Environ. Chang. 2017, 42, 33–46. [Google Scholar] [CrossRef]
- Pfeffer, J. Building sustainable organizations: The human factor. Acad. Manag. Perspect. 2010, 24, 34–45. [Google Scholar]
- Hovlid, E.; Bukve, O.; Haug, K.; Aslaksen, A.B.; Von Plessen, C. Sustainability of healthcare improvement: What can we learn from learning theory? BMC Health Serv. Res. 2012, 12, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Hussain, M.; Khan, M.; Ajmal, M.; Sheikh, K.S.; Ahamat, A. A multi-stakeholders view of the barriers of social sustainability in healthcare supply chains. Sustain. Account. Manag. Policy J. 2019, 10, 290–313. [Google Scholar] [CrossRef]
- Brugha, R.; Zwi, A. Improving the quality of private sector delivery of public health services: Challenges and strategies. Health Policy Plan. 1998, 13, 107–120. [Google Scholar] [CrossRef] [Green Version]
- Ullah, Z.; Khan, M.Z.; Rehman, W.U. Assessing quality of service through customer satisfaction: The case of public sector healthcare organization in pakistan. Ucp Manag. Rev. (UCPMR) 2017, 1, 97–116. [Google Scholar] [CrossRef]
- Kortum, E.; Leka, S.; Cox, T. Psychosocial risks and work-related stress in developing countries: Health impact, priorities, barriers and solutions. Int. J. Occup. Med. Environ. Health 2010, 23, 225–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pirzadeh, P.; Lingard, H. Understanding the dynamics of construction decision making and the impact on work health and safety. J. Manag. Eng. 2017, 33, 05017003. [Google Scholar] [CrossRef]
- Hammer, L.B.; Truxillo, D.M.; Bodner, T.; Pytlovany, A.C.; Richman, A. Exploration of the impact of organisational context on a workplace safety and health intervention. Work Stress 2019, 33, 192–210. [Google Scholar] [CrossRef]
- Che Huei, L.; Ya-Wen, L.; Ming, Y.C.; Chen, H.L.; Yi, W.J.; Hung, L.M. Occupational health and safety hazards faced by healthcare professionals in Taiwan: A systematic review of risk factors and control strategies. SAGE Open Med. 2020, 8, 2050312120918999. [Google Scholar] [CrossRef] [PubMed]
- Mohd Fahmi, M.R. Using Work Scale Safety (WSS) to Determine Factors Influencing Safety Behavior among Auxiliary Police. Ph.D. Thesis, Universiti Utara Malaysia, Utara, Malaysia, 2017. [Google Scholar]
- Ng, L.-P.; Choong, Y.-O.; Kuar, L.-S.; Tan, C.-E.; Teoh, S.-Y. Job satisfaction and organizational citizenship behaviour amongst health professionals: The mediating role of work engagement. Int. J. Healthc. Manag. 2019, 1–8. [Google Scholar] [CrossRef]
- Azeem, M.U.; Bajwa, S.U.; Shahzad, K.; Aslam, H. Psychological contract violation and turnover intention: The role of job dissatisfaction and work disengagement. Empl. Relat. Int. J. 2020, 42, 1291–1308. [Google Scholar] [CrossRef]
- Seilonen, J. What is Sustainability? A Discourse Analysis of Oil Companies’ Sustainability Reports; Hankens: Helsinki, Finland, 2021. [Google Scholar]
- Bibri, S.E.; Krogstie, J. Smart sustainable cities of the future: An extensive interdisciplinary literature review. Sustain. Cities Soc. 2017, 31, 183–212. [Google Scholar] [CrossRef]
- Crespo-Gonzalez, C.; Benrimoj, S.I.; Scerri, M.; Garcia-Cardenas, V. Sustainability of innovations in healthcare: A systematic review and conceptual framework for professional pharmacy services. Res. Soc. Adm. Pharm. 2020, 16, 1331–1343. [Google Scholar] [CrossRef] [PubMed]
- Dzhengiz, T. A literature review of inter-organizational sustainability learning. Sustainability 2020, 12, 4876. [Google Scholar] [CrossRef]
- Ajmal, M.M.; Khan, M.; Hussain, M.; Helo, P. Conceptualizing and incorporating social sustainability in the business world. Int. J. Sustain. Dev. World Ecol. 2018, 25, 327–339. [Google Scholar] [CrossRef]
- Moore, J.E.; Mascarenhas, A.; Bain, J.; Straus, S.E. Developing a comprehensive definition of sustainability. Implement. Sci. 2017, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Schaltegger, S.; Burritt, R. Corporate sustainability. In The International Yearbook of Environmental and Resource Economics 2005/2006; Edward Elgar Publishing: Cheltenham, UK, 2005; pp. 185–222. [Google Scholar]
- Sodhi, M.S.; Tang, C.S. Corporate social sustainability in supply chains: A thematic analysis of the literature. Int. J. Prod. Res. 2018, 56, 882–901. [Google Scholar] [CrossRef]
- Paulraj, A. Understanding the relationships between internal resources and capabilities, sustainable supply management and organizational sustainability. J. Supply Chain Manag. 2011, 47, 19–37. [Google Scholar] [CrossRef]
- Smith, P.A.; Sharicz, C. The shift needed for sustainability. Learn. Organ. 2011, 18, 73–86. [Google Scholar] [CrossRef]
- Milán-García, J.; Uribe-Toril, J.; Ruiz-Real, J.L.; Valenciano, J.D.P. Sustainable local development: An overview of the state of knowledge. Resources 2019, 8, 31. [Google Scholar] [CrossRef] [Green Version]
- Smith, P.A.; Wals, A.E.; Schwarzin, L. Fostering organizational sustainability through dialogic interaction. Learn. Organ. 2012, 18, 73–86. [Google Scholar] [CrossRef]
- Coblentz, J.B. Organizational Sustainability: The Three Aspects that Matter; Academy for Educational Development: Washington, DC, USA, 2002. [Google Scholar]
- Agyeman, J.; Warner, K. Putting’just sustainability’into place: From paradigm to practice. Policy Manag. Rev. 2002, 2, 8. [Google Scholar]
- Fiorino, D.J. Sustainability as a conceptual focus for public administration. Public Adm. Rev. 2010, 70, s78–s88. [Google Scholar] [CrossRef]
- Hasna, A. Dimensions of Sustainability. J. Eng. Sustain. Dev. Energy Environ. Health 2007, 2, 47–57. [Google Scholar] [CrossRef]
- Opp, S.M.; Saunders, K.L. Pillar talk: Local sustainability initiatives and policies in the United States—Finding evidence of the “three E’s”: Economic development, environmental protection, and social equity. Urban Aff. Rev. 2013, 49, 678–717. [Google Scholar] [CrossRef]
- Stazyk, E.C.; Moldavanova, A.; Frederickson, H.G. Sustainability, intergenerational social equity, and the socially responsible organization. Adm. Soc. 2016, 48, 655–682. [Google Scholar] [CrossRef]
- Portney, K.E.; Cuttler, Z. The local nonprofit sector and the pursuit of sustainability in American cities: A preliminary exploration. Local Environ. 2010, 15, 323–339. [Google Scholar] [CrossRef]
- Schaltegger, S.; Burritt, R. Measuring and managing sustainability performance of supply chains. Supply Chain. Manag. Int. J. 2014, 19. [Google Scholar] [CrossRef]
- Dempsey, N.; Bramley, G.; Power, S.; Brown, C. The social dimension of sustainable development: Defining urban social sustainability. Sustain. Dev. 2011, 19, 289–300. [Google Scholar] [CrossRef]
- Koppenjan, J.F.; Enserink, B. Public–private partnerships in urban infrastructures: Reconciling private sector participation and sustainability. Public Adm. Rev. 2009, 69, 284–296. [Google Scholar] [CrossRef]
- Vallance, S.; Perkins, H.C.; Dixon, J.E. What is social sustainability? A clarification of concepts. Geoforum 2011, 42, 342–348. [Google Scholar] [CrossRef]
- Lee, C.M.J.; Che-Ha, N.; Alwi, S.F.S. Service customer orientation and social sustainability: The case of small medium enterprises. J. Bus. Res. 2021, 122, 751–760. [Google Scholar] [CrossRef]
- Sajjad, A.; Shahbaz, W. Mindfulness and social sustainability: An integrative review. Soc. Indic. Res. 2020, 150, 73–94. [Google Scholar] [CrossRef]
- Gálvez, A.; Tirado, F.; Martínez, M.J. Work–life balance, organizations and social sustainability: Analyzing female telework in Spain. Sustainability 2020, 12, 3567. [Google Scholar] [CrossRef]
- Pasaribu, S.I.; Vanclay, F.; Zhao, Y. Challenges to implementing socially-sustainable community development in oil palm and forestry operations in Indonesia. Land 2020, 9, 61. [Google Scholar] [CrossRef] [Green Version]
- Polèse, M.; Stren, R. The social sustainability of cities. Chapter 2000, 1, 3–38. [Google Scholar]
- Nakawuki, H. Job Satisfaction, Occupational Hazards, and Stress and Among Health Workers of Butabika National Referral Mental Hospital. Ph.D. Thesis, Makerere University, Kampala, Uganda, 2019. [Google Scholar]
- Macik-Frey, M.; Quick, J.C.; Nelson, D.L. Advances in occupational health: From a stressful beginning to a positive future. J. Manag. 2007, 33, 809–840. [Google Scholar] [CrossRef]
- Wilburn, S.Q.; Eijkemans, G. Preventing needlestick injuries among healthcare workers: A WHO-ICN collaboration. Int. J. Occup. Environ. Health 2004, 10, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Chirico, F. New and Emerging Risk Factors in Occupational Health. Appl. Sci. 2020, 10, 8906. [Google Scholar] [CrossRef]
- Wijnen, B.F.; Lokkerbol, J.; Boot, C.; Havermans, B.M.; Van Der Beek, A.J.; Smit, F. Implementing interventions to reduce work-related stress among health-care workers: An investment appraisal from the employer’s perspective. Int. Arch. Occup. Environ. Health 2020, 93, 123–132. [Google Scholar] [CrossRef] [Green Version]
- Kwasnicka, D.; Dombrowski, S.U.; White, M.; Sniehotta, F.F. Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychol. Rev. 2016, 10, 277–296. [Google Scholar] [CrossRef]
- Bogard, W.C. Bringing social theory to hazards research: Conditions and consequences of the mitigation of environmental hazards. Sociol. Perspect. 1988, 31, 147–168. [Google Scholar] [CrossRef]
- Reddy, V.; Bennadi, D. Occupational hazards among dentists: A descriptive study. J. Oral Hyg. Health 2015. [Google Scholar] [CrossRef] [Green Version]
- Haleblian, J.; Finkelstein, S. The influence of organizational acquisition experience on acquisition performance: A behavioral learning perspective. Adm. Sci. Q. 1999, 44, 29–56. [Google Scholar] [CrossRef]
- Cox, T.; Griffiths, A.; Rial-González, E. Research on Work-Related Stress; European Communities: Luxembourg, 2000. [Google Scholar]
- Sauter, S.L.; Murphy, L.R.; Hurrell, J.J. Prevention of work-related psychological disorders: A national strategy proposed by the National Institute for Occupational Safety and Health (NIOSH). Am. Psychol. 1990, 45, 1146. [Google Scholar] [CrossRef]
- Whatley, M.A.; Webster, J.M.; Smith, R.H.; Rhodes, A. The effect of a favor on public and private compliance: How internalized is the norm of reciprocity? Basic Appl. Soc. Psychol. 1999, 21, 251–259. [Google Scholar] [CrossRef]
- Widok, A.H. Social sustainability: Theories, concepts, practicability. In Environmental Informatics and Industrial Environmental Protection: Concepts, Methods and Tools (2); Industrial Environmental Informatics Unit: Berlin, Germany, 2009. [Google Scholar]
- Braccini, A.M.; Margherita, E.G. Exploring organizational sustainability of industry 4.0 under the triple bottom line: The case of a manufacturing company. Sustainability 2019, 11, 36. [Google Scholar] [CrossRef] [Green Version]
- Böhringer, C.; Jochem, P.E. Measuring the immeasurable—A survey of sustainability indices. Ecol. Econ. 2007, 63, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Dillard, J.; Dujon, V.; King, M.C. Understanding the Social Dimension of Sustainability; Routledge: New York, NY, USA, 2008. [Google Scholar]
- Littig, B.; Griessler, E. Social sustainability: A catchword between political pragmatism and social theory. Int. J. Sustain. Dev. 2005, 8, 65–79. [Google Scholar] [CrossRef] [Green Version]
- Eizenberg, E.; Jabareen, Y. Social sustainability: A new conceptual framework. Sustainability 2017, 9, 68. [Google Scholar] [CrossRef] [Green Version]
- Wilson, M.G.; DeJoy, D.M.; Vandenberg, R.J.; Richardson, H.A.; McGrath, A.L. Work characteristics and employee health and well-being: Test of a model of healthy work organization. J. Occup. Organ. Psychol. 2004, 77, 565–588. [Google Scholar] [CrossRef]
- Nahrgang, J.D.; Morgeson, F.P.; Hofmann, D.A. Safety at work: A meta-analytic investigation of the link between job demands, job resources, burnout, engagement, and safety outcomes. J. Appl. Psychol. 2011, 96, 71. [Google Scholar] [CrossRef]
- Dollard, M.F.; Bakker, A.B. Psychosocial safety climate as a precursor to conducive work environments, psychological health problems, and employee engagement. J. Occup. Organ. Psychol. 2010, 83, 579–599. [Google Scholar] [CrossRef] [Green Version]
- Hayes, B.E.; Perander, J.; Smecko, T.; Trask, J. Measuring perceptions of workplace safety: Development and validation of the work safety scale. J. Saf. Res. 1998, 29, 145–161. [Google Scholar] [CrossRef]
- Stromquist, N.P. Education in a Globalized World: The Connectivity of Economic Power, Technology, and Knowledge; Rowman & Littlefield: Lanham, MD, USA, 2002. [Google Scholar]
- Storper, M. The limits to globalization: Technology districts and international trade. Econ. Geogr. 1992, 68, 60–93. [Google Scholar] [CrossRef]
- Jaumotte, F.; Lall, S.; Papageorgiou, C. Rising income inequality: Technology, or trade and financial globalization? IMF Econ. Rev. 2013, 61, 271–309. [Google Scholar] [CrossRef] [Green Version]
- Pfeffer, J. Producing sustainable competitive advantage through the effective management of people. Acad. Manag. Perspect. 1995, 9, 55–69. [Google Scholar] [CrossRef]
- Bartlett, C.A.; Ghoshal, S. Building competitive advantage through people. MIT Sloan Manag. Rev. 2002, 43, 34. [Google Scholar]
- Boxall, P. Achieving competitive advantage through human resource strategy: Towards a theory of industry dynamics. Hum. Resour. Manag. Rev. 1998, 8, 265–288. [Google Scholar] [CrossRef]
- Brown, K.A.; Willis, P.G.; Prussia, G.E. Predicting safe employee behavior in the steel industry: Development and test of a sociotechnical model. J. Oper. Manag. 2000, 18, 445–465. [Google Scholar] [CrossRef]
- Cella-De-Oliveira, F.A. Indicators of organizational sustainability: A proposition from organizational competences. Int. Rev. Manag. Bus. Res. 2013, 2, 962. [Google Scholar]
- Jansen, E.; Mallan, K.M.; Daniels, L.A. Extending the validity of the feeding practices and structure questionnaire. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Hoyle, R.H. The structural equation modeling approach: Basic concepts and fundamental issues. In Structural Equation Modeling: Concepts, Issues, and Applications; Hoyle, R.H., Ed.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef] [Green Version]
- Wong, K.K.-K. Partial least squares structural equation modeling (PLS-SEM) techniques using SmartPLS. Mark. Bull. 2013, 24, 1–32. [Google Scholar]
- Henseler, J. Bridging design and behavioral research with variance-based structural equation modeling. J. Advert. 2017, 46, 178–192. [Google Scholar] [CrossRef]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation coefficients: Appropriate use and interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef]
- Kozak, A. Effects of multicollinearity and autocorrelation on the variable-exponent taper functions. Can. J. For. Res. 1997, 27, 619–629. [Google Scholar] [CrossRef]
- Ornell, F.; Halpern, S.C.; Kessler, F.H.P.; Narvaez, J.C.D.M. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. Cad. Saude Publica 2020, 36, e00063520. [Google Scholar] [CrossRef] [PubMed]
- Gavin, B.; Hayden, J.; Adamis, D.; McNicholas, F. Caring for the psychological well-being of healthcare professionals in the Covid-19 pandemic crisis. Ir. Med. J. 2020, 113, 51. [Google Scholar]
- Danet, A.D. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med. Clínica (Engl. Ed.) 2021, 156, 449–458. [Google Scholar] [CrossRef]
- Jalili, M.; Niroomand, M.; Hadavand, F.; Zeinali, K.; Fotouhi, A. Burnout among healthcare professionals during COVID-19 pandemic: A cross-sectional study. Int. Arch. Occup. Environ. Health 2021, 1–8. [Google Scholar] [CrossRef]
- Braquehais, M.D.; Vargas-Cáceres, S.; Gómez-Durán, E.; Nieva, G.; Valero, S.; Casas, M.; Bruguera, E. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. QJM Int. J. Med. 2020, 113, 613–617. [Google Scholar] [CrossRef] [PubMed]
- Najjar, M.; Small, M.H.; Yasin, M.M. Social sustainability strategy across the supply chain: A conceptual approach from the organisational perspective. Sustainability 2020, 12, 10438. [Google Scholar] [CrossRef]
- Abid, G.; Ahmed, S.; Elahi, N.S.; Ilyas, S. Antecedents and mechanism of employee well-being for social sustainability: A sequential mediation. Sustain. Prod. Consum. 2020, 24, 79–89. [Google Scholar] [CrossRef]
- Epstein, M.J.; Elkington, J.; Herman, B. Making Sustainability Work: Best Practices in Managing and Measuring Corporate Social, Environmental and Economic Impacts; Routledge: Sheffield, UK, 2018. [Google Scholar]
- Nwachukwu, N.C.; Orji, F.A.; Ugbogu, O.C. Health care waste management–public health benefits, and the need for effective environmental regulatory surveillance in federal Republic of Nigeria. Curr. Top. Public Health 2013, 2, 149–178. [Google Scholar]
- Gershon, R.R.; Karkashian, C.D.; Grosch, J.W.; Murphy, L.R.; Escamilla-Cejudo, A.; Flanagan, P.A.; Bernacki, E.; Kasting, C.; Martin, L. Hospital safety climate and its relationship with safe work practices and workplace exposure incidents. Am. J. Infect. Control 2000, 28, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Clarke, S. Safety leadership: A meta-analytic review of transformational and transactional leadership styles as antecedents of safety behaviours. J. Occup. Organ. Psychol. 2013, 86, 22–49. [Google Scholar] [CrossRef]
- Michael, J.H.; Guo, Z.G.; Wiedenbeck, J.K.; Ray, C.D. Production supervisor impacts on subordinates’ safety outcomes: An investigation of leader-member exchange and safety communication. J. Saf. Res. 2006, 37, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Harris, T.C. Predicting Workplace Safety Outcomes through Subordinate and Supervisor Involvement in Safety Issues; University of Connecticut: Tolland, CT, USA, 1997. [Google Scholar]
- Yanar, B.; Lay, M.; Smith, P.M. The interplay between supervisor safety support and occupational health and safety vulnerability on work injury. Saf. Health Work 2019, 10, 172–179. [Google Scholar] [CrossRef]
- Thompson, R.C.; Hilton, T.F.; Witt, L.A. Where the safety rubber meets the shop floor: A confirmatory model of management influence on workplace safety. J. Saf. Res. 1998, 29, 15–24. [Google Scholar] [CrossRef]
- Colligan, M.J.; Cohen, A. The role of training in promoting workplace safety and health. In The Psychology of Workplace Safety; Barling, J., Frone, M.R., Eds.; American Psychological Association: Washington, DC, USA, 2004. [Google Scholar]
- Ayim Gyekye, S. Workers’ perceptions of workplace safety and job satisfaction. Int. J. Occup. Saf. Ergon. 2005, 11, 291–302. [Google Scholar] [CrossRef] [Green Version]
- Khattak, F.H. Hospital waste management in Pakistan. Pak. J. Med. Res. 2009, 48, 19–23. [Google Scholar]
- Abdullah, M.T.; Shaw, J. A review of the experience of hospital autonomy in Pakistan. Int. J. Health Plan. Manag. 2007, 22, 45–62. [Google Scholar] [CrossRef] [Green Version]
- Misbah, S.; Mahboob, U. Strengths, weaknesses, opportunities, and threats analysis of integrating the World Health Organization patient safety curriculum into undergraduate medical education in Pakistan: A qualitative case study. J. Educ. Eval. Health Prof. 2017, 14, 35. [Google Scholar] [CrossRef] [PubMed]
| Variables | Items (Measurement) | Variables | Items (Measurement) |
|---|---|---|---|
| Job Safety Do you agree or disagree that each of the following words or phrases describes your job? | Dangerous | Management Safety (Practices) Do you agree or disagree that each of the following words or phrases describes your management? | Provides enough safety training |
| Hazardous | Conducts frequent safety inspections | ||
| Unhealthy | Investigates safety problems quickly | ||
| Fear of death | Provides safe equipment | ||
| Chance of death | Provides safe working conditions | ||
| Safe | Helps maintain a clear work area | ||
| Scary | Keeps workers informed of hazards | ||
| Coworker Safety Do you agree or disagree that each of the following words or phrases describes these people? | Ignore safety rules | Safety Programs (Policies) Do you agree or disagree that each of the following words or phrases describes this safety program? | Helps prevent accidents |
| Do not care about others’ safety | Unclear | ||
| Pay attention to safety rules | Effective in reducing injuries | ||
| Encourage others to be safe | Does not apply to my workplace | ||
| Keep work area clean | Important | ||
| Safety-oriented | Does not work | ||
| Supervisor Safety Do you agree or disagree that each of the following words or phrases describes these people? | Praises safe work behaviors | Organizational Social Sustainability Do you agree or disagree that each of the following words or phrases describes your relation with the organization? | Sense of belonging |
| Keeps workers informed of safety rules | Social capital | ||
| Perceived environment | |||
| Trains workers to be safe | Social interactions/security | ||
| Acts on safety suggestions | Interaction with space | ||
| Updates safety rules | Satisfaction from space | ||
| Enforces safety rules | Voice and influence |
| Demographics | Frequency | Percentage |
|---|---|---|
| Gender | ||
| 260 | 60 |
| 171 | 40 |
| Age (in years) | ||
| 92 | 21 |
| 102 | 24 |
| 112 | 26 |
| 73 | 17 |
| 52 | 12 |
| Experience (in years) | ||
| 90 | 20 |
| 108 | 25 |
| 119 | 28 |
| 81 | 19 |
| 33 | 08 |
| Healthcare Professional | ||
| 186 | 43 |
| 190 | 44 |
| 55 | 13 |
| Variables * | Cronbach’s Alpha | rho_A | Composite Reliability | (AVE) |
|---|---|---|---|---|
| Cowrker | 0.791 | 0.833 | 0.863 | 0.617 |
| Job | 0.870 | 0.877 | 0.906 | 0.659 |
| MgtP | 0.739 | 0.742 | 0.852 | 0.658 |
| OSS | 0.818 | 0.819 | 0.892 | 0.733 |
| Prgrms | 0.779 | 0.788 | 0.849 | 0.531 |
| Supervsr | 0.884 | 0.894 | 0.915 | 0.683 |
| Cowrker | Job | MgtP | OSS | Prgrms | Supervsr | |
|---|---|---|---|---|---|---|
| Cowrker | 0.786 | |||||
| Job | 0.594 | 0.812 | ||||
| MgtP | 0.576 | 0.607 | 0.811 | |||
| OSS | 0.579 | 0.628 | 0.544 | 0.856 | ||
| Prgrms | 0.675 | 0.758 | 0.696 | 0.645 | 0.759 | |
| Supervsr | 0.605 | 0.588 | 0.749 | 0.6 | 0.722 | 0.827 |
| Cowrker | Job | MgtP | OSS | Prgrms | Supervsr | |
|---|---|---|---|---|---|---|
| Cowrker | ||||||
| Job | 0.698 | |||||
| MgtP | 0.752 | 0.753 | ||||
| OSS | 0.696 | 0.734 | 0.697 | |||
| Prgrms | 0.848 | 0.870 | 0.816 | 0.779 | ||
| Supervsr | 0.702 | 0.667 | 0.819 | 0.699 | 0.814 |
| OSS | |
|---|---|
| Cowrker | 1.987 |
| Job | 2.479 |
| MgtP | 2.614 |
| OSS | |
| Prgrms | 3.876 |
| Supervsr | 3.036 |
| Cowrker | Job | MgtP | OSS | Prgrms | Supervsr | |
|---|---|---|---|---|---|---|
| Cowrker | 1 | |||||
| Job | 0.694 | 1 | ||||
| MgtP | 0.676 | 0.607 | 1 | |||
| OSS | 0.679 | 0.628 | 0.644 | 1 | ||
| Prgrms | 0.675 | 0.758 | 0.696 | 0.645 | 1 | |
| Supervsr | 0.605 | 0.688 | 0.749 | 0.650 | 0.752 | 1 |
| R Square | R Square Adjusted | |
|---|---|---|
| OSS | 0.506 | 0.498 |
| Original Sample (O) | Sample Mean (M) | Standard Deviation (STDEV) | T Statistics (|O/STDEV|) | p Values | |
|---|---|---|---|---|---|
| Cowrker -> OSS | 0.181 | 0.184 | 0.066 | 2.721 | 0.007 |
| Job -> OSS | 0.279 | 0.280 | 0.071 | 3.955 | 0.000 |
| MgtP -> OSS | 0.014 | 0.014 | 0.073 | 0.195 | 0.845 |
| Prgrms -> OSS | 0.148 | 0.150 | 0.082 | 1.794 | 0.043 |
| Supervsr -> OSS | 0.205 | 0.203 | 0.072 | 2.858 | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ullah, Z.; Sulaiman, M.A.B.A.; Ali, S.B.; Ahmad, N.; Scholz, M.; Han, H. The Effect of Work Safety on Organizational Social Sustainability Improvement in the Healthcare Sector: The Case of a Public Sector Hospital in Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 6672. https://doi.org/10.3390/ijerph18126672
Ullah Z, Sulaiman MABA, Ali SB, Ahmad N, Scholz M, Han H. The Effect of Work Safety on Organizational Social Sustainability Improvement in the Healthcare Sector: The Case of a Public Sector Hospital in Pakistan. International Journal of Environmental Research and Public Health. 2021; 18(12):6672. https://doi.org/10.3390/ijerph18126672
Chicago/Turabian StyleUllah, Zia, Mohammed Ali Bait Ali Sulaiman, Syed Babar Ali, Naveed Ahmad, Miklas Scholz, and Heesup Han. 2021. "The Effect of Work Safety on Organizational Social Sustainability Improvement in the Healthcare Sector: The Case of a Public Sector Hospital in Pakistan" International Journal of Environmental Research and Public Health 18, no. 12: 6672. https://doi.org/10.3390/ijerph18126672
APA StyleUllah, Z., Sulaiman, M. A. B. A., Ali, S. B., Ahmad, N., Scholz, M., & Han, H. (2021). The Effect of Work Safety on Organizational Social Sustainability Improvement in the Healthcare Sector: The Case of a Public Sector Hospital in Pakistan. International Journal of Environmental Research and Public Health, 18(12), 6672. https://doi.org/10.3390/ijerph18126672










